Abstract
Objective
To present and describe interprofessional education (IPE) in 6 US colleges of pharmacy including benefits, barriers, and strategies for implementation.
Methods
A focus group with campus faculty IPE leaders and administrators was conducted at each of the 6 colleges. External facilitators used a structured script with open-ended questions to guide each session. A qualitative approach was used and content analysis of transcripts was conducted.
Results
On a 10-point scale, mean participant interest in IPE was 8.8 ± 1.7. Incentives included enhanced student education, instructional economies of scale, improved communication among disciplines, and promotion of teamwork to improve quality of care. Curricular logistics, limited resources, lack of conceptual support, and cultural issues were the major barriers to IPE. Institutions were at various stages of IPE implementation. Participants emphasized that full institutional support was critical in maintaining IPE programs.
Conclusion
Interest in IPE was high and opportunities were numerous as described by faculty members at the institutions; however, numerous challenges to implementation were identified.
Keywords: interprofessional education, focus group, pharmacy
INTRODUCTION
One of the 10 primary tenets set forth by the Institute of Medicine (IOM) for reforming healthcare education to improve quality and better meet patient needs is teaching students to work in interprofessional practice, reflective of the importance of teamwork in effective, comprehensive healthcare.1 The corollary to interprofessional practice is to be educated in such a manner. Yet, the long-held educational paradigm at most healthcare institutions, including schools and colleges of pharmacy, is to deliver instruction within professions. At many institutions, healthcare professional students have been trained in “silos,” as separate disciplines are not exposed to one another until clinical experiences late in their educational training. An instructional realignment through efforts across the healthcare disciplines has the potential to create many challenges, as well as previously unexplored opportunities, within professional education.
The approach to interprofessional education (IPE), particularly within healthcare professions, is still a developing concept, with the bulk of the literature reflecting models outside the United States. Focus group interviews of patients, students, and academic staff members in England indicated all groups realized the importance of IPE in influencing professional identity.2 There was also broad agreement across professions that the implementation of IPE can create organizational challenges, and there was a lack of consensus regarding the optimal sequencing of such instruction within the curricular spectrum (ie, early vs. late in course of study). The attitudes of faculty members towards IPE, and factors influencing those opinions, were recently assessed in a Canadian academic health center.3 Although collective (ie, medicine, nursing, pharmacy, social work) scores were positive, medicine faculty members had significantly lower attitude scores, while female faculty members and those with experience in IPE reported significantly higher scores.
Since faculty attitudes are an important factor driving the implementation of IPE initiatives, awareness of these attitudes and influencing attributes is important. The contemporary issues that US pharmacy faculty members face in considering the approach to IPE, and how these issues compare to their professional colleagues, are still unclear, as is the approach US healthcare professions have taken to respond to the IOM's call to arms about IPE. Thus, using a qualitative approach, we set out to identify the nature of IPE implementation, specific organizational challenges to implementation, and opportunities for integration that remain among US schools and colleges of pharmacy and their campus colleagues.
METHODS
Focus groups of faculty members from 6 US colleges of pharmacy and affiliated health professions colleges were conducted. Only 1 focus group session was conducted on the campus of each participating institution, with groups ranging in size from 5 to 8 participants.
Campus faculty leaders in educational delivery, administration, and IPE were invited to participate in the 2-hour sessions, following their consent to participate in the institutional review board-approved investigation. These leaders were identified by virtue of their administrative position (eg, dean of academic affairs), engagement in formalized campus IPE endeavors, involvement in existing IPE committees, or related activities. Students or trainees engaged in interprofessional education were not eligible for study participation. No participants were excluded upon the basis of gender, racial/ethnic group, or other characteristics.
External facilitators used a singular, structured group script to guide each session. The definition of IPE according to Steinert, “occasions when 2 or more professions learn with, from and about each other to improve collaborations and the quality of care,” was used in this investigation.4 Open-ended questions were used to determine the campus climate towards IPE and identify any previous instructional methods attempted, current campus IPE endeavors, implementation barriers encountered in the past or expected, potential approaches to overcoming challenges and sustaining progress, and perceived IPE benefits. Because each participant's verbal comments were audiotaped, each member was assigned a code number for grouping and categorization of data. Two questions were posed to the group to initially guide the discussion:
According to Steinert, interprofessional education (IPE) is defined as “occasions when 2 or more professions learn with, from, and about each other to improve collaborations and the quality of care.” What is your program's interest (1-10, 10 being highest) in implementation, and why?
List the top 3 challenges to IPE at this university. Place them in rank order of importance.
Participants' written responses to the questions were assigned a corresponding code number. All materials, including additional observational notes, were then transcribed to a comprehensive written document capturing each site's focus group session. In this qualitative investigation, a content analysis of transcripts was conducted in the manner of Miles and Huberman to discover categories or themes consistent with the study's aims.5
A review of each institution's current IPE endeavors and planned activities was also conducted to characterize progress towards implementation. Prochaska's transtheoretical model of change was the basis for characterization.6 First developed to describe the process of smoking cessation, the transtheoretical model delineates stages that most individuals experience when changing a behavior. While commonly used in the setting of public health (eg, substance abuse and addiction) and disease management (eg, adherence to antiretroviral regimens), the model of change has not been commonly used to describe shifts in educational paradigms.7 In this investigation, institutions that had yet to programmatically consider IPE implementation were characterized as pre-contemplative; those that had begun investigations into IPE but had yet to undertake any formal preparation or planning were noted to be contemplative. The preparation phase was ascribed to campuses that were engaged in developing policies, enlisting interested faculty members (whether internally or through external recruitment efforts), and fulfilling other planning roles. Activities connected to the action phase included pilot projects, as well as the development and installation of approaches intended to become a permanent part of the curriculum. The maintenance category was connected to the routine role IPE techniques served in the healthcare professions' curricula, while organizations in which IPE had ceased were noted to be in relapse.
RESULTS
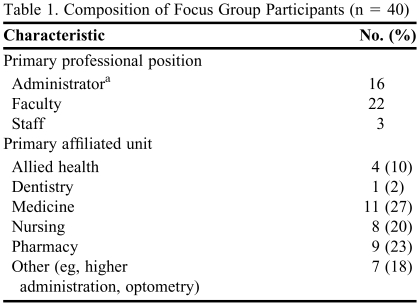
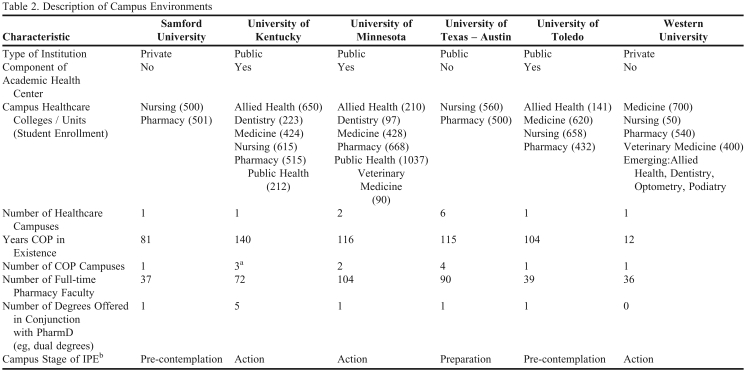
Forty individuals attended the focus group session held on their campus; 7 invited subjects were unable to participate due to scheduling conflicts. Medicine (11, 27%) and pharmacy (9, 23%) were the programs of study with which participants were most commonly affiliated (Table 1). At 4 of the 6 institutions, the college of pharmacy was a component of an academic health center (Table 2). One college of pharmacy had been in existence for fewer than 15 years. Two of the institutions were composed of only 1 healthcare college or school in addition to pharmacy. Participants were asked to indicate their respective unit's interest in IPE, with values ranging from 1 (no interest) to 10 (highest degree of interest). Most participants noted a value of 10 (mean 8.8 ± 1.7), indicating a high degree of interest in IPE.
Table 1.
Composition of Focus Group Participants (n = 40)
a14 (86%) also held faculty appointments
Table 2.
Description of Campus Environments
Abbreviations: COP = colleges/schools of pharmacy; IPE = interprofessional education
aIncludes 2 experiential education hubs
bInterprofessional education; based upon transtheoretical model6
Benefits of IPE
Six primary benefits of IPE emerged from the focus group sessions, 3 of which were linked directly to common missions of academic institutions.
Enhance student education and training. Participants noted that interprofessional approaches to education more effectively prepare students for clinical practice, from functioning in an interprofessional manner, to understanding the roles each discipline fulfills in the provision of patient care.
Capitalize upon instructional economies of scale. The potential for IPE models to minimize resources necessary to provide and administer multiple degree and professional programs was identified.
Expand opportunities for research and scholarship. In addition to potential resource benefits, IPE was linked to enhanced research and scholarly endeavors.
Improve communication among healthcare professionals. The potential for IPE to eliminate barriers to a greater understanding of other professions' roles and cultures was commonly identified.
Promote teamwork. Learning with and from each other supports team-based approaches to care delivery.
Improve quality of care and patient outcomes. A number of methods in which interprofessional approaches to education may lead to improved patient care were discussed including: promoting patient and provider safety; identifying and preventing errors; improving efficiency; and enhancing patient communication.
Barriers to IPE Implementation
Focus group members delineated a number of hurdles to IPE implementation which were later connected to the primary themes of curricular concerns, limited resources, lack of conceptual support, and cultural challenges connected to each profession. Scheduling common courses and activities across multiple degree programs, insufficient classroom space to accommodate interprofessional learners, and the lock-step characteristic of most professional degree curricula were commonly elicited. The time and resources needed to develop IPE instructional approaches, subsequent course and content ownership battles that may arise, and the need to identify a primary group to evaluate student performance and assess the curricular changes also appeared. The lack of consistency with which students are prepared to enter professional degree programs, and the corresponding baseline knowledge and abilities, may also hamper the development of educational methods that cross disciplines. Unique pedagogical approaches to educating entry-level practitioners among each profession were thought to also hinder IPE success.
Concern about insufficient resources was a common thread in all focus group sessions. Specific concerns included the time and human resources needed to develop and sustain IPE approaches, which were thought to vary considerably from current instructional designs. Financial constraints that permeate all higher academic institutions, as well as individual academic units, and the connections between tuition dollars and unit funding, were noted to be of particular concern. As 1 participant explained, “…why should I send my students to your class, if they're in my class [we] get 100% [of the tuition] ; if they're in your class, [we] only get 25%…” The relative dearth of faculty experienced in IPE delivery approaches was thought to be a significant hindrance, particularly in light of the overall faculty shortage that pharmacy is experiencing.
The defining nature of disciplines, and their innate differences, were noted as potential roadblocks to IPE. The traditional roles that each profession plays in the healthcare environment, and how those carry over to educational endeavors, promote fragmentation and inconsistent priorities. Realigning approaches to team-based education requires basic tenets of IPE, including trust, communication, and parallel priorities. These features were noted to be lacking on some campuses. A practical barrier was the lack of infrastructure to reward faculty members for engaging in IPE approaches, particularly given the nature of the contemporary promotion and tenure system (eg, focus on individual achievement). From a broader perspective, support of the premise of interprofessional education was considered vital to success. Thus, a lack of such support was thought to be a death knell to successful implementation. Such concerns were noted to emanate at the institutional level, with a trickle-down effect to unit administrators, faculty and students. As one participant suggested: “We do not to my knowledge have a mechanism at the institutional level to reward it [IPE]. I think to go even further, what we need to do is expect it of our faculty.” A lack of consistent focus on IPE among accrediting bodies in the academic healthcare sector was also noted to be a hurdle.
Current IPE Environments
The action stage reflected current IPE endeavors in 3 of the institutions assessed, 2 of which were characterized as components of an academic health center (Table 2). A number of pilot projects, as well as more established activities, were noted in the action stage institutions. Interdisciplinary cases (ie, participants from 6 differing disciplines), joint OSCEs (objective, structured clinical examinations), and pilot IPE approaches to experiential education in the rural setting were pedagogic techniques being employed or pursued. One campus commemorated its 3-year history with the delivery of a joint best practices institute for health professions faculty members. Another institution supported a student organization which united students from across the health professions, while students in a third setting were engaged in a national IPE case-based competition.
Student engagement in public health activities was commonly associated with new or established IPE practices. Connections to practice included student health screenings, student-run clinics, and campus or community bus tours. A participant explained, “… although it's not in the professional setting, it is getting people together, getting them to know each other, who are from different professions…it's kind of a preliminary step to getting them to talk in a professional setting.”
The engagement of a few individuals in IPE activities was noted in the sole institution in the preparation stage. A lack of a cohesive or organized approach to IPE development (“happenstance”) was described, amid pockets in which interprofessional care was inculcated (ie, pediatrics). Precontemplation reflected environments in which a handful of individuals were struggling to experiment with IPE approaches, with no institutional support or consistency across disciplines. One focus group participant pondered if the campus efforts were “too little, too late.”
Strategies for IPE Implementation and Maintenance
Global.
Regardless of the IPE stage in which participants worked, a number of common approaches to educational innovation were identified. An underlying theme was the recognition that widespread change in the educational paradigm is difficult to achieve, but persistence, consistent buy-in throughout the educational hierarchy, and willingness to accept some setbacks would yield an improved product (eg, a more well-rounded/qualified/better-prepared practitioner). At a global level, participants agreed that change to an IPE focus must be consistently supported and stimulated by the accreditation standards for all healthcare professions. Because curricular and pedagogical alterations are commonly driven by accrediting agencies, and successful IPE requires the support of all disciplines, program accreditation is a necessary incentive to promote and sustain change. Support must then follow throughout the hierarchy of higher education, beginning with administration. A strategic institutional statement should convey the importance of IPE, as individual colleges, thought leaders, and faculty members move forward in implementation. One participant felt the issue may have moved beyond the purview of individual academic institutions: “It seems like we need to be working with the accrediting agencies to make sure they are talking together so they understand the issue.” A common discussion point was the need to identify champions for IPE implementation from each academic unit, with an IPE steering committee playing a critical role in orchestrating projects across disciplines. Participants speculated that empowering an interprofessional steering group may lessen political jockeying among the institution's colleges and schools. To be most effective, individuals felt the committee should consider developing an IPE curriculum, with elements focused on instruction, service, and research. Such a cross-cutting approach would be consistent with an institutional IPE strategic statement, and would intercalate with major missions of both academic units and individual faculty members. Academic incentives for units, as well as individual faculty members, to pursue IPE initiatives were also key success factors identified. Budgetary support was often listed as the primary incentive, along with funding of pilot projects, and sustained funding for successful endeavors. Funding streams may arise from federal or state funds, or through donors, grants, and foundations. In addressing the importance of IPE funding, one participant commented: “I believe the only way it [IPE] is going to rise to the top is if someone at the top says ‘thou shalt do it or thou shalt not have a budget.’”
Operational.
A suggested initial approach to developing an IPE curriculum was an examination of each discipline's curricula to identify: core knowledge and skills required for successful graduates; corresponding common content areas or courses of study; and academic scheduling details (eg, credit hours, course meeting frequency, course sequencing, class size). The desired outcome of such an examination would be to inform the IPE steering committee of groups of students, rather than overall degree programs, that are most likely to benefit from IPE activities, and for whom courses of study are most amenable to IPE implementation.
A commonly recommended tenet to implementing IPE was to view it as a continuum, with small forays at the onset. Participants felt that expecting wholesale change in a short time was unrealistic, and might lead to confusion, frustration, and lack of acceptance by faculty members and students. Group members recommended that activities should first focus on a small area (eg, practice approaches, ethics in practice, professionalism, core foundational science). Some observed that an initial approach outside the classroom is wise and pointed to service learning as a particular method for early integration. IPE could also be conceived as more of an event, rather than an entire course, with longitudinal experiences frequently described. One group suggested wide-sweeping change to the IPE educational paradigm rather than having discipline-specific instruction with carve-outs for IPE, implement an educational delivery model with IPE as the primary instructional approach, with carve-outs for discipline-specific needs. One participant suggested, “It's not the amount of credit hours that they spend together, it's that they have a … thread of interprofessional experience throughout whatever their program is.”
Regardless of the instructional methods used, participants uniformly embraced an understanding of the roles each profession plays in healthcare delivery as a foundational aspect of successful IPE. Tactics to build such understanding included engaging instructors from other units or degree programs in educational delivery. A particular approach to prepare all disciplines for the practice setting was thought to be the integration of simulation or standardized patients that are cared for by the team. Gaining faculty support and enthusiasm for implementation was also a critical element. In addition to developing requisite award structures, some participants noted that perhaps not all faculty members need to or should be involved in IPE (eg, basic sciences). Yet another noted that, while widespread institutional support is critical, faculty members must individually embrace IPE.
DISCUSSION
The challenges US healthcare professions face in responding to national recommendations for interprofessional education are much like those experienced by their colleagues elsewhere. The approach to IPE is still in development, or has yet to become a significant focus, and the progress in implementing IPE is varied among institutions. Organizational approaches, logistics (eg, scheduling), curricular ownership, sequencing, and other practical elements continue to be identified as challenges. Yet, despite these challenges, faculty members and administrators are generally supportive of interprofessional approaches to healthcare professions education, regardless of progress that may be occurring at their respective institutions. However, many of the focus group participants were already actively engaged in IPE planning or development at their own campuses, but not all professions were equally represented in the investigation. Thus, these findings cannot be considered as fully representative of their faculty colleagues. Nevertheless, a variety of institutions were assessed as represented by the range of participant characteristics, including pharmacy program duration, presence of multiple healthcare degree-granting units, institutional focus on research, and campus stage of IPE development.
Wholesale change in educational approach is not a realistic expectation for contemporary health professions education. Rather, each institution should pursue IPE implementation in an intentional, mission-driven manner, with the realization that progress is to be measured in small increments. As newer faculty members join schools and colleges of pharmacy, the likelihood that they will be products of IPE training environments is expected to increase. This new generation of faculty members may be instrumental in sustaining any progress made in IPE implementation.
This inquiry was not inclusive of all stakeholders, particularly students and patients. While there is a paucity of literature assessing the patient perspective, data are available from the student cohort. Understanding roles and responsibilities of other team members, development of trust in others, and minimizing professional barriers are student-perceived benefits of IPE.8 However, some students perceived IPE as a source of tension when combined with their individual discipline's learning expectations.9 Students who participated in a 2-year Canadian interprofessional education intervention in the mental health services setting found merit in evaluating their profession's value and their attitudes toward patients, and reported increased confidence in their jobs; however, there was no statistical change in team performance.
Because of the dearth of existing literature directly reflecting pharmacy IPE initiatives, one should examine perceptions from a health educator perspective with special attention to those studies that include pharmacy educators.11 Attitudes of Canadian senior academic administrators of health professional education programs, which included pharmacy, were generally positive and lacked any discipline-specific differences.12 Primary barriers identified by these administrators in implementing and maintaining IPE were scheduling, curriculum ownership issues, and lack of perceived benefit. In a similar US study, Gardner et al also found overall positive attitudes toward IPE among senior health professional academic administrators.13
The focus group sessions were beneficial in uncovering contemporary issues surrounding IPE at colleges of pharmacy and the higher institutions in which they were located. However, such discovery was not limited to informing the development of this manuscript, as individual participating sites garnered local benefits. At one campus, an initial foray into multidisciplinary student case conferences with a corresponding day-long showcase of planned IPE instruction was stimulated by the local focus group session. Participants in yet another session were inspired to develop an interprofessional case activity. In a third setting, results of the local focus group have been reviewed by the IPE steering committee to inform future IPE planning.
Despite the findings of this investigation, which echoed those of previous inquiries from other countries, there is much more to be learned about IPE. Because this undertaking was qualitative in nature, it must be viewed and interpreted in the context in which it was sought (eg, driven primarily by individual perceptions). Additionally, the true impact of interprofessional educational techniques on student learning and retention, particularly as measured by the quality of patient care they subsequently deliver, has yet to be measured. While challenges colleges of pharmacy may face in IPE implementation appear to mirror those of other professions, pharmacy may face the greatest pressure to implement IPE as it relates to accreditation standards. Thus, colleges of pharmacy are encouraged to provide the needed campus-wide stimulus to evoke a shift in the educational paradigm.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the guidance of R. Lee Evans, PharmD, in this endeavor.
REFERENCES
- 1.Greiner AC, Knevel E, editors. Health Professions Education: A Bridge to Quality. A report of the Committee on the Health Professions Education Summit, Institute of Medicine. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Carlisle C, Cooper H, Watkins C. Do none of you talk to each other? The challenges facing the implementation of interprofessional education. Med Teach. 2004;26(6):546–52. doi: 10.1080/61421590410001711616. [DOI] [PubMed] [Google Scholar]
- 3.Curran VR, Sharpe D, Forristall J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Med Educ. 2007;41(9):892–6. doi: 10.1111/j.1365-2923.2007.02823.x. [DOI] [PubMed] [Google Scholar]
- 4.Steinert Y. Learning together to teach together: interprofessional education and faculty development. J Interprof Care. 2005;1(Suppl):60–75. doi: 10.1080/13561820500081778. [DOI] [PubMed] [Google Scholar]
- 5.Miles MB, Huberman AM. Qualitative Data Analysis. Thousand Oaks, Calif: Sage; 1994. [Google Scholar]
- 6.Prochaska JO, DiClemente CC. Stages and processes of self-change in smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 7.Wagner G, Iguchi M, Schneider S, Scott J, Anderson D. Placebo practice trials; a tool to assess and improve adherence readiness. HIV Clin Trials. 2002;3(6):475–81. doi: 10.1310/WQRY-FNUL-VNE1-56XA. [DOI] [PubMed] [Google Scholar]
- 8.O'Neill BJ, Wyness MA. Student voices on an interprofessional course. Med Teach. 2005;27(5):433–8. doi: 10.1080/01421590500086680. [DOI] [PubMed] [Google Scholar]
- 9.Johnson R. Exploring student views of interprofessional education. Int J Therapy Rehab. 2003;10(7):314–20. [Google Scholar]
- 10.Carpenter J, Barnes D, Dickinson C, Wooff D. Outcomes of interprofessional education for community mental health services in England: The longitudinal evaluation of a postgraduate programme. J Interprof Care. 2006;20(2):145–61. doi: 10.1080/13561820600655653. [DOI] [PubMed] [Google Scholar]
- 11.Remington TL, Foulk MA, Williams BC. Evaluation of evidence for interprofessional education. Am J Pharm Educ. 2006;(3):70. doi: 10.5688/aj700366. Article 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curran VR, Deacon DR, Fleet L. Academic administrators' attitudes towards interprofessional education in Canadian schools of health professional education. J Interprof Care. 2005;1(Suppl):76–86. doi: 10.1080/13561820500081802. [DOI] [PubMed] [Google Scholar]
- 13.Gardner SF, Chamberlin GD, Heestand DE, Stowe CD. Interdisciplinary didactic instruction at academic health centers in the United States: Attitudes and barriers. Adv Health Sci Educ Theory Pract. 2002;7(3):179–90. doi: 10.1023/a:1021144215376. [DOI] [PubMed] [Google Scholar]