Abstract
Objectives
To develop and evaluate a classroom-based curriculum designed to promote interprofessional competencies by having undergraduate students from various health professions work together on system-based problems using quality improvement (QI) methods and tools to improve patient-centered care.
Design
Students from 4 health care programs (nursing, nutrition, pharmacy, and physical therapy) participated in an interprofessional QI activity. In groups of 6 or 7, students completed pre-intervention and post-intervention reflection tools on attitudes relating to interprofessio nal teams, and a tool designed to evaluate group process.
Assessment
One hundred thirty-four students (76.6%) completed both self-reflection instruments, and 132 (74.2%) completed the post-course group evaluation instrument. Although already high prior to the activity, students' mean post-intervention reflection scores increased for 12 of 16 items. Post-intervention group evaluation scores reflected a high level of satisfaction with the experience.
Conclusion
Use of a quality-based case study and QI methodology were an effective approach to enhancing interprofessional experiences among students.
Keywords: interprofessional education, quality improvement
INTRODUCTION
Quality improvement (QI) knowledge and skills are core competencies for health care providers.1 As early as 1991, the Pew Health Professions Commission asserted health education must not only prepare students to provide quality care, but also help improve the system.2 To be competent at entry-to-practice, health care students require knowledge on how systems work, how to benchmark and measure against that benchmark, how to identify normal variation, and how to initiate change.2 This knowledge should be acquired during their formative educational years.3
A number of educational outcomes or QI competencies have been identified, with specific competencies associated with particular teaching methods.4 QI competencies associated with lectures and seminar formats include the ability of the student to develop an aim, linking data to change, describing the Plan-Do-Study-Act (PDSA) cycle, eliciting interprofessional input, and incorporating an interprofessional perspective.5 Being able to define the problem; identify stakeholders; carry out root cause analysis; and identify, implement, and evaluate an intervention have been suggested as well, but are more often associated with graduate-level students preparing independent-study QI proposals and projects in real-life practice settings.4
Interprofessional collaboration is critical for the success of any QI initiative.3 Not surprisingly, the ability to work together as members of an interprofessional team to continuously improve the system is considered a core competency of health care professionals.6 Interprofessional competencies include being knowledgeable of the roles of other professions, understanding the constraints of one's own role, having good communication and negotiation skills, and having the ability to work with others effectively.7 As faculties move to integrate more QI content into health care curricula, it is important to acknowledge interprofessional education (IPE) as critical for students to develop their QI competencies.8
Despite the need, there continues to be a lack of integration of QI theory and methods into the core curricula of most health professions programs; in part, due to a failure to see quality improvement as an educational priority of undergraduate health care programs, and because of a lack of expertise within health faculties.3 Health care educators have also struggled to integrate interprofessional competencies into their curricula. In addition to attitudinal, cultural, and economic barriers, attempts to increase student awareness and experience with interprofessional competencies often represent a significant increase in faculty workload, with little recognition by administration of that workload.9
To meet these challenges, educators must consider approaches beyond traditional didactic lectures to secure for their students the ability to improve and evaluate the quality of care.10 Educators must adopt pedagogical models that will effectively prepare their students to work in teams, to engage in data-driven decision making and improve patient care processes.6 Indeed, through the process of identifying and investigating a problem, such as that seen with QI, students come to understand and value one another.3 Furthermore, by using an interprofessional approach as the method by which QI knowledge and skills are acquired, both QI and interprofessional teaching objectives may be met while minimizing the overall increase in faculty and student workloads.
Over the past 3 decades, a variety of methods have been used to teach quality improvement principles and practices, including didactic lectures, observation of quality improvement activities, personal improvement projects, and participation in peer-review activities.11-19 In addition to these approaches, the combination of lectures and small group exercises is viewed as an effective approach to transfer competencies associated with improved quality care.20
The purpose of this paper is to report on the development and evaluation of a classroom-based curriculum designed to promote interprofessional competencies by allowing undergraduate students from various health professions to work together on system-based problems using quality improvement methods and tools to improve patient-centred care.
DESIGN
The Participants
During the academic year 2007-2008, 223 students from 4 health care programs (nursing, nutrition, pharmacy, and physical therapy) participated in an interprofessional QI activity at the University of Saskatchewan. Our project involved more senior students with prior exposure to interprofessional initiatives than junior students. Students were assigned to work in groups of 6 or 7, either in term 1 (fall 2007) or term 2 (winter 2008). Participants in term 1 included 45 third-year pharmacy students, 46 fourth-year nursing students, and 30 third-year physical therapy students. Participants in term 2 consisted of 37 pharmacy students not assigned to term 1 groups, along with 39 second-year nursing students and 26 second-year nutrition students. Scheduling and resource constraints precluded the use of workplace-based experiences; thus, an intermediate lecture and paper-based approach involving multiple health disciplines was deemed most appropriate to build on students' existing knowledge and skills.21
The Curriculum
The pedagogical focus of this project was a QI exercise evaluating a case about elderly patients in transition from acute care to community care that was developed specifically for this project. The case was designed to address the key steps associated with initiating, improving, evaluating, and sustaining a quality improvement program.22 For the students, the emphasis was on developing strategies to produce improvement and how to determine whether a change occurred. Students were provided the opportunity to collaborate and contribute to the team, and the use of real data provided a level of authenticity to the exercise. The skills they employed were relevant and practical for entry-level health care professionals.23
Course content relating to QI was delivered to the students in the form of a uniprofessional session (1.5-3 hours, depending on program-based scheduling constraints) and 2 interprofessional group sessions (3 hours in total). Students were required to complete 3 assignments (2 individual and 1 group). These were designed to assess QI core competencies in terms of understanding and application of the PDSA.
During the uniprofessional sessions, students received an introductory lecture on QI theory and methods. Specific components included defining the elements of an aim statement (what is the group specifically trying to accomplish?), the types of measurement (outcome, process, balancing) used in QI, the PDSA Cycle and its application in QI, and how to define the problem using approaches such as Ishikawa (Fishbone) Diagrams or brainstorming. Students were also familiarized with the use of time-series data charts, and how these might be used to assess performance, and to measure the effect of a quality improvement initiative. In preparation for group work, students also received actual health-system data (Appendix 1), and a written description of the role they were to assume during the group sessions.
Following the lecture and prior to the first group session, students completed and submitted the first take-home assignment. The assignment consisted of multiple-choice questions and short-answer items designed to assess the student's ability to synthesize and apply QI theory.
In the first group session, the interprofessional student teams reviewed key QI concepts, analyzed actual health-system data (relating to patient satisfaction with hospital discharge), and chose priorities for improvement. Next, the teams created a quality improvement team charter in which they defined an improvement aim and selected a family of measures to monitor progress toward their goal.
For the second assignment, students individually researched and identified 3 evidence-based change ideas for their teams to consider testing (available by request from the author). Students were encouraged to use and were assessed on their ability to use traditional and nontraditional sources for determining potential ideas for change given their case study, with assessment heavily weighted toward rationale (ie, “tell me why we should try this idea and not another”).
In the second group session, each team reviewed all their change ideas, consensually selected 1 change idea, developed a PDSA cycle plan (available by request from the author), reviewed the characteristics of effective teams, and completed and submitted the team charter (available by request from the author) for which the team received a pass or fail grade.
Course instructors from the participating programs served as facilitators during the group sessions. The uniprofessional lectures were provided by a senior QI consultant and the group sessions were led by staff members from the Health Quality Council of Saskatchewan. Evaluation and grading of the assignments were carried out by a senior QI consultant from the Council with more than 4 years experience working with individuals and teams in applying QI methodology in practice.
Interprofessional Education Evaluation
In addition to the QI component, students were invited to complete both a pre-intervention and post-intervention self-reflection tool on knowledge, attitudes, and beliefs relating to interprofessional teams originally developed by Clark.24 The questionnaire consisted of 16 items, each using a 7-point Likert scale anchored by diametrically opposing statements relating to teamwork.
At the end of the second group session, students also were given the opportunity to complete a questionnaire developed by McMaster University that was designed to evaluate group process.25 The questionnaire included 9 items, each using a 7-point Likert scale anchored by diametrically opposing statements about the functioning of their team during the QI group sessions. Students were also invited to provide written comments about the exercise.
Students willing to participate in the research component of the class provided written consent prior to their participation in the study, and each received a copy of the consent form. Consent was requested and forms were collected during a scheduled lecture. To avoid any real or perceived coercion of nonparticipants by other students or the instructors, all students were provided with copies of the IPE evaluation instruments and invited to complete them whether or not they indicated a wish to participate in the research study. Completed survey instruments from nonparticipants were subsequently destroyed by the graduate student administering the questionnaires and were never seen by the course instructors or the other members of the research team. The graduate student also ensured that all research materials were de-identified and given anonymous identifiers to protect the identity of participants and nonparticipants. The master list was sealed to make it unavailable to the research team. The research protocol was approved by the Research Ethics Board of the University of Saskatchewan.
Descriptive and comparative statistics were carried out using SPSS 16.0. The Wilcoxon signed-rank test was used to compare pre- and post-IPE and group process survey data. Kruskal-Wallis and Bonferonni's tests were used to compare changes in these responses across the 5 participating student groups.
ASSESSMENT
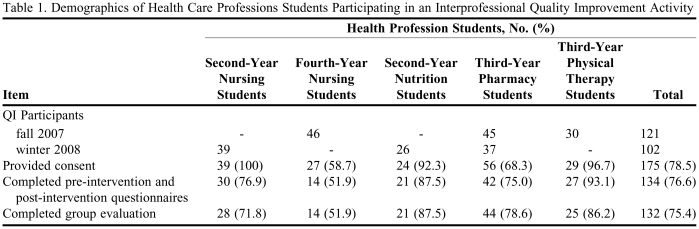
Of the 223 students participating in the QI exercise, 175 (78.5%) provided signed consent to participate (Table 1). Of these, 134 students (76.6%) completed both the pre-intervention and post-intervention self-reflection instruments, and 132 (75.4%) completed the post-intervention group evaluation instrument. The highest completion rates were among nutrition and physical therapy students, while the lowest rates of participation and instrument completion were among fourth-year nursing students.
Table 1.
Demographics of Health Care Professions Students Participating in an Interprofessional Quality Improvement Activity
Abbreviations: QI = quality improvement
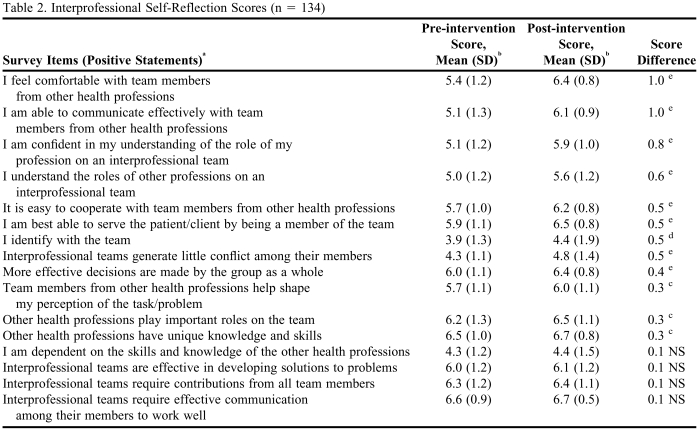
Pre-intervention reflection scores (Table 2) were generally high (more than 5 on a 7-point scale). Items scored lower on the pre-intervention evaluation included: I identify with the team (3.9); Interprofessional teams generate little conflict among their members (4.3); and I am dependent on the skills and knowledge of the other health professions (4.3).
Table 2.
Interprofessional Self-Reflection Scores (n = 134)
aItems presented in descending order based on difference between pre-intervention and post-intervention test scores.
bEach survey item was anchored by a negative and positive statement and students were asked to indicate where they saw themselves on a 7-point continuum between the 2 statements. Due to space limitations, only the positive statements are presented in the table.
c p < 0.05
d p < 0.01
e p < 0.001
Significant increases were found between pre-intervention and post-intervention reflection scores for 12 of 16 items (p < 0.05). Of these, the post-intervention scores for 7 items were substantially higher (more than 0.5) than the pre-intervention. These items dealt with the student's ability to communicate and cooperate with others and their comfort with and ability to identify with their team. The other 5 items with significant higher post-intervention scores but with a score increase of less than 0.5, dealt with team conflict, group decision making, and the role of other professions. Few significant differences were seen based on professional designation.
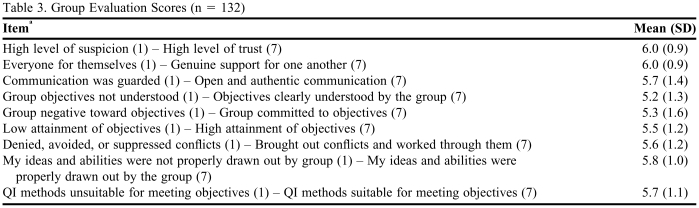
Post-intervention group evaluation scores reflected a high level of satisfaction with the experience (Table 3). All 9 items in the questionnaire were scored above 5 (maximum 7). The mean for the 9 items was 5.6, and mean scores ranged from a low of 5.2 (objectives understood by group) to a high of 6.0 (group members genuinely support each other). There were no significant differences in the group evaluation scores based on professional designation.
Table 3.
Group Evaluation Scores (n = 132)
aEach item was anchored by a negative and positive statements and students were asked to indicate where they saw themselves on a 7-point continuum between the 2 statements.
Marks for QI assignments 1 and 2 were both relatively high (85.6% and 80.8%, respectively) with a mean of 34.2 (SD 3.3) for the first assignment (maximum score of 40), and a mean of 9.7 (SD 0.95) for the second assignment (maximum score of 12). The distribution of marks was narrow for both assignments with most marks ranging from 23 to 40 for assignment 1 and 4 to 12 for assignment 2. All groups submitted and received a passing grade for the third assignment (the team charter).
DISCUSSION
The purpose of this paper is to report on the development and evaluation of a classroom-based curriculum designed to promote interprofessional competencies by allowing undergraduate students from various health professions to work together on system-based problems using quality improvement (QI) methods and tools to improve patient-centred care. At the beginning of the QI module, students generally held positive views about interprofessional teams and their role within these teams. While it was encouraging that students already supported interprofessional approaches to care, it raised the possibility that there would be “little room to grow” in terms of measuring a positive change in attitudes toward interprofessional teams as the result of participating in the QI workshop. However, the study was able to demonstrate a number of positive changes in student perceptions of the interprofessional team. These changes along with positive evaluations of the group processes suggest the use of a QI framework is an appropriate and feasible educational model, both to promote interprofessional concepts and to support interprofessional approaches to learning.
The high scores achieved by the students for the QI assignments suggest the students did acquire the core knowledge presented in the QI module (lecture and group work). However, the contribution of an interprofessional format is not known. Indeed, the first assignment followed a uniprofessional lecture and the second assignment was carried out individually following group interaction. Students completed assignment 3 (team charter) together, but it was assessed only as a pass or fail and all teams received a passing grade. As well, there were no comparator groups such as uniprofessional teams. Future research might be carried out to better demonstrate the benefits of an interprofessional approach but was beyond the scope of this project.
Limitations
The limitations of the study included rates of participation in the study by some groups of students and the generalizability of the findings. Lower percentages of fourth-year nursing students and pharmacy students agreed to participate in the study. Nonparticipants may have represented those students with views less favorable toward interprofessional practice. However, these lower consent rates may reflect the timing of when this consent was sought from these 2 groups of students: on a Friday afternoon for the fourth-year nursing students, and at the start of an early morning class for the pharmacy students. There was also a lower rate of participation in the research component of the project among fourth-year nursing students who had given consent and the reason for this was unclear.
The study took place in a University containing multiple professional colleges and at a time when many interprofessional training initiatives were underway across the province of Saskatchewan as part of a 3-year nationally funded project. Institutions with more limited representation across the health professions or where interprofessional education has a lower or greater profile within the curriculum might experience different results. Finally, the contribution of the HQC staff members was critical to the delivery of the QI module. The presence and availability of this type of community partner and/or faculty members who specialize in QI methodology may greatly affect the student experience and the educational outcomes achieved with regard to interprofessional competencies.
CONCLUSIONS
Use of a quality-based case study and a quality improvement methodology appear to be an effective approach to supporting and enhancing interprofessional experiences among health professional students. The partnership between the Health Quality Council staff members and the University of Saskatchewan and the Saskatchewan Institute for Applied Science and Technology faculty members helped to strengthen the link between theory and practice.
ACKNOWLEDGEMENTS
Funding for this project was provided by a grant from the Patient Centered Interprofessional Team Experiences (P-CITE) Program, Interprofessional Education for Collaborative Patient-Centred Practice (IECPCP), Health Canada Project.
Appendix 1. Example of Patient Experience Data
REFERENCES
- 1. Health Professionals Education: A Bridge to Quality. Institute of Medicine, Washington, DC: National Academy Press; 2003.
- 2.Batalden PB, Stoltz PK. A framework for the continual improvement of health care: building and applying professional and improvement knowledge to test changes in daily work. Joint Commission J Quality Improvement. 1993;19(10):424–52. doi: 10.1016/s1070-3241(16)30025-6. [DOI] [PubMed] [Google Scholar]
- 3.Ladden MD, Bednash G, Stevens DP, Moore GT. Educating interprofessional learner for quality, safety and systems improvement. J Interprofessional Care. 2006;20(5):497–505. doi: 10.1080/13561820600935543. [DOI] [PubMed] [Google Scholar]
- 4.Leenstra JL, Beckman TJ, Reed DA, et al. Validation of a method for assessing resident physicians' quality improvement proposals. J Gen Intern Med. 2007;22(9):1330–4. doi: 10.1007/s11606-007-0260-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogrinc G, Headrick LA, Morrison IJ, Foster T. Teaching and assessing resident competence in practice-based learning and improvement. J Gen Intern Med. 2004;19(5):496–500. doi: 10.1111/j.1525-1497.2004.30102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore SM, Novotny J, Quinn D, Norman L, Harper DC. Taking aim at interdisciplinary education for continuous improvement in health care. Nurs Health Care Perspect. 1997;18(6):308–15. [PubMed] [Google Scholar]
- 7.Oandasan I, Reeves S. Key elements for interprofessional education. Part 1: The learner, the educator and the learning context. J Interprofessional Care. 2005;19(S1):21–38. doi: 10.1080/13561820500083550. [DOI] [PubMed] [Google Scholar]
- 8.Barr H. Interprofessional education: the fourth focus. J Interprofessional Care. 2007;21(S2):40–50. doi: 10.1080/13561820701515335. [DOI] [PubMed] [Google Scholar]
- 9.Gilbert JH. Interprofessional learning and higher education structural barriers. J Interprofessional Care. 2005;19(Supp 1):87–106. doi: 10.1080/13561820500067132. [DOI] [PubMed] [Google Scholar]
- 10.Holmboe ES, Prince L, Green M. Teaching and improving quality of care in a primary care internal medicine residency clinic. Acad Med. 2005;80(6):571–7. doi: 10.1097/00001888-200506000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Barbaccia JC. Introducing quality assurance and medical audit into the UCSF Medical Center curriculum. J Med Educ. 1976;51(5):386–91. doi: 10.1097/00001888-197605000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Weeks W, Robinson M, Brooks W, Batalden P. Using early clinical experiences to integrate quality-improvement learning into medical education. Acad Med. 2000;75(1):81–4. doi: 10.1097/00001888-200001000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Mulligan J, Garg M, Skipper J, McNamara M. Quality assurance in undergraduate medical education at the Medical College of Ohio. J Med Educ. 1976;51(5):378–85. doi: 10.1097/00001888-197605000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Barr D, Wollstadt L, Goodrich L, Pittman J, Booker C, Evans R. The Rockford School of Medicine undergraduate quality assurance program. J Med Educ. 1976;51(5):370–7. doi: 10.1097/00001888-197605000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Headrick L, Nueuharuser D, Schwab P, Stevens D. Continuous quality improvement and the education of the generalist physician. Acad Med. 1995;7(1):S104–S9. doi: 10.1097/00001888-199501000-00033. [DOI] [PubMed] [Google Scholar]
- 16.Weingart S. A house officer-sponsored quality improvement initiative: leadership lessons and liabilities. Joint Commission J Quality Improvement. 1998;24(7):371–8. doi: 10.1016/s1070-3241(16)30388-1. [DOI] [PubMed] [Google Scholar]
- 17.Gordon P, Carlson L, Chessman A, Kundrat M, Morahan P, Headrick L. A multi-site collaborative for the development of interdisciplinary education in continuous improvement for health professional students. Acad Med. 1996;71(9):973–8. doi: 10.1097/00001888-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Headrick L, Richardson A, Priebe G. Continuous improvement learning for residents. Pediatrics. 1998;101(4 Pt 2):768–73. [PubMed] [Google Scholar]
- 19.Kyrkjebo J. Beyond the classroom: integrating improvement learning into health professions education in Norway. Joint Commission J Quality Improvement. 1999;25(11):588–97. doi: 10.1016/s1070-3241(16)30472-2. [DOI] [PubMed] [Google Scholar]
- 20.Singh R, Naughton B, Taylor J, et al. A comprehensive collaborative patient safety residency curriculum to address the ACGME core competencies. Med Educ. 2005;39(12):1195–204. doi: 10.1111/j.1365-2929.2005.02333.x. [DOI] [PubMed] [Google Scholar]
- 21.D'Eon M. A blueprint for interprofessional learning. J Interprofessional Care. 2005;(Supplement 1):49–59. doi: 10.1080/13561820512331350227. [DOI] [PubMed] [Google Scholar]
- 22.Curtis JR, Cook DJ, Wall RJ, et al. Intensive care unit quality improvement: A “how to” guide for the interdisciplinary team. Crit Care Med. 2006;34(1):211–8. doi: 10.1097/01.ccm.0000190617.76104.ac. [DOI] [PubMed] [Google Scholar]
- 23.Headrick LA. Washington, DC: HRSA/Bureau of Health Professions; 2000. Learning to improve complex systems of care. Collaborative Education to Ensure Patient Safety; pp. 75–88. [Google Scholar]
- 24.Clark P. Learning on interdisciplinary gerontological teams: instructional concepts and methods. Educ Gerontol. 1994;20(4):349–64. [Google Scholar]
- 25.Jaques D. Learning in Groups. 3rd ed. London: Kogan Page Limited; 2000. p. 246. [Google Scholar]