SUMMARY
In Ethopia, like many developing countries, autopsy is rare unless conducted in the medico-legal arena, making vital statistics that include sparse pathological diagnoses. To determine the most common factors contributing to death among individuals who died from natural or injury-related events in Ethiopia in 2006, 200 consecutive autopsies were conducted at the Forensic Medico-legal Pathology Department, Menelik II Hospital, Addis Ababa, Ethiopia. The results describe significant pathological observations, putative cause of death, age distribution, and gender ratios. Eighty-one percent of the cases were male, and the mean age was 38.9 (±15.5 years). Fifty-two percent of the individuals died from natural causes, including infections, and 48% died from injury-related events. In the natural deaths group, pulmonary complications were the most commonly reported cause of death by gross examination at autopsy, with suspected tuberculosis accounting for 12%. Tuberculosis (21, 8%) and liver disease (14, 5%) were the most common histopathological findings in the natural and injury-related causes groups, respectively. In the injury-related group, automobile accident was the most common cause of accidental death (80%), and homicide by beating was the most common cause of death in the intentional injury group (31%). These data provide valuable unbiased analyses of causes of death among individuals in Addis Ababa, Ethiopia.
Keywords: autopsy, cause death, pathology
INTRODUCTION
Numerous studies describe the use of verbal autopsy to ascertain the cause of death in resource-limited settings where more precise means such as clinical autopsy and vital registration are scarce [1–3]. A verbal autopsy is an indirect method of finding out the cause of a death, based on an interview with next of kin or other caregivers regarding symptoms, signs, and circumstances preceding death [4]. However, misclassification of cause of death presents a significant problem, and a high degree of variability for classification exists among sites [5]. Moreover, when cause of death statistics are collected strictly from hospital settings, the results tend to be biased since hospitals populations are not representative [6]. Studies addressing the validity of verbal autopsy point out the need for models that consider populations with variable patterns of cause-specific mortality. In systems where community-based verbal autopsy interviews are utilized, vital registration is not maintained [1, 2, 5, 7]. Thus, in these communities, there exists a need to improve the specificity and sensitivity of classification systems for cause of death.
In 1984, in one of the few and perhaps one of the best documented reports of autopsy findings in Addis Ababa, Gebre-Selassie analyzed 256 autopsies conducted at Addis Ababa Faculty of Medicine in Black Lion Hospital [8]. Results from these studies indicated that in 66.4% of the cases, clinical diagnoses were confirmed by autopsy, 31.2% revealed a different diagnosis, and 2.4% were inconclusive. These results clearly demonstrate the value of autopsy in developing regions to support clinical observations and advance epidemiological studies.
METHODS
Data in this report are based on information collected from a study to determine the most common causes of natural and injury-related deaths from consecutive 200 adult autopsy cases received during a 2-month period by the Forensic Medico-legal Pathology Department at Menelik II Hospital in Addis Ababa, Ethiopia. Exclusion criteria were a post-mortem time exceeding 24h, individuals under the age of 18, and incomplete information from police reports or clinical sources. Subjects included individuals that died in the hospital or health clinic while receiving treatment and those that died outside of the hospital. A police report, clinical information, or both accompanied each case. Cases were categorized as either natural or injury-related deaths. Deaths from natural causes were classified as those resulting from documented pre-existing illnesses or an acute event (eg., myocardial infarction) as determined by gross observations at autopsy. Injury-related deaths included accidental (automobile, falls), intentional (suicide, homicide), or those from an undetermined source of trauma, as previously described [9].
Histopathological analyses were conducted at Addis Ababa University Faculty of Medicine, Department of Pathology. For these studies, tissue blocks (approximately 2.5 cm2) from the spleen, liver, lung (lower right lobe), peri-bronchial lymph nodes, adrenals, and brain (frontal cortex/white matter, basal ganglia/lenticular nucleus, hippocampus and spinal cord) were obtained from each case. Blocks were fixed in 10% formalin and processed for histological analyses. Paraffin blocks were serially sectioned and stained with hematoxylin and eosin for pathological examination. Histological diagnosis of Tuberculosis was verified by acid-fast staining as described by Bibbo and Day [10]. The Federal Democratic Republic of Ethiopia, Ethiopian Science and Technology Commission, and the Universities of California and Temple Human Subjects Research Protection Program approved all studies.
RESULTS
Of 200 autopsies conducted, 12 were excluded due to age, >24h post-mortem interval, or lack of information regarding either circumstances of death or in the final autopsy report. Age of subjects included in the study ranged from 18 to 82, with a mean of 38.9 years and a median of 35 years (Table 1). Of the 188 cases included in this report, 152 were male (81%). Death in 98 cases (52%) was reported to have resulted from natural causes and in 90 cases from injury (48%) (Table 1). The mean age in the natural causes group was 42.6 ±15.2 years (median 40 years) (Table 2). The mean age for intentional injury-related deaths was 34 ±9.6 (median 32.5 years), and 35 ±13.5 years (median 30 years) for accidental injury-related deaths (Table 3).
Table 1.
Demographics and Pathological findings from all cases.
| Case Demographics (n = 188) | |
| Mean Age (years) | 38.9 ± 15.5a |
| % Male | 152 (81%)b |
| Natural Cause | 98 (52%) |
| Injury Related (accidental and intentional) | 90 (48%) |
| Pathological Observations Reported at Autopsy By Gross Examination (n = 188) | |
| Suspected Chronic Illness | 112 (60%) |
| Suspected CNS Infection | 37 (20%) |
| Suspected pulmonary TBc with pneumonia | 84 (45%) |
| Cachexia | 8 (4%) |
| Cardiac Disease | 14 (7%) |
±, standard deviation years;
percent of total cases
Tuberculosis, TB.
Table 2.
Causes of Naturally Occurring Deaths
| Natural Deaths n=98 | Mean Age (years) | |
|---|---|---|
| Reported Causes of Death at Autopsy | n | 42.6 ±15.2a |
| Cerebral hemorrhage/stroke | 9 | 39±12.6 |
| Pneumonia | 30 | 40±18.0 |
| Liver Disease | 5 | 48±12.4 |
| Cardiac Failure | 14 | 50±17.3 |
| Sepsis | 6 | 43±16.0 |
| Pulmonary TB | 12 | 50±17.4 |
| Wasting | 4 | 29±2.1 |
| Otherb | 18 | 37±13.1 |
±, standard deviation years;
complications of pregnancy, gastric or enteric hemorrhage, gastritis, hepatitis, undefined tumors, meningitis, acute pancreatitis, splenomegaly, malaria or multiple chronic infections.
Table 3.
Causes of Injury-related Deaths
| Causes of Injury-Related Deaths n=90 | Mean Age (years) | |
|---|---|---|
| Intentional n=47 | na | 34 ±9.6b |
| Asphyxiation/Strangulation | 4 | 39±9 |
| Gun Shot Wound | 10 | 30±7.4 |
| Trauma from Beating | 28 | 36±10.2 |
| Stab Wounds | 5 | 31±4.5 |
| Accidental n=43 | 35 ±13.5 | |
| Auto Accident | 34 | 35±14.1 |
| Drowning | 3 | 31±10 |
| Electric Shock | 2 | 20, 30 |
| Head Trauma (fall) | 3 | 38±12.2 |
| Poisoning (CO2) | 1 | 23 |
the 90 cases of injury related deaths are separated by cause, number of cases for each cause category (n), classification ratio;
±, standard deviation.
Sixty percent of all cases were reported as having signs of chronic illness, 20% of which were suspected of having some type of CNS infection, 45% suspected of Tuberculosis infection with pneumonia, and 4 % and 7% with cachexia and cardiac disease, respectively (Table 1). Findings from the brains of two representative cases are shown in Figures 1 and 2. The brain from a 35-year-old patient who died with severe cachexia, pulmonary Tuberculosis, and suspected HIV encephalitis is illustrated in Figure 1. Gross examination revealed a purulent exudate over the entire brain and atrophy. In contrast to normal histological findings in the brain of a 37-year-old man who died from a gun shot wound (GSW) (Figs. 2A, D, G), histopathological analyses of the case (shown in Fig. 1) indicated white matter vacuolarization, microglial nodules (Fig. 2B, arrowhead), reactive gliosis (Fig. 2E), and positive immunoreactivity for HIV p24 (Fig. 2H). Likewise, a second representative case with pneumonia, hepatomegaly, and suspected HIV showed white matter vacuolarization, lymphocytic infiltration (Fig. 2C), reactive gliosis (Fig. 2F), and was also positive for HIV p24 (Fig. 2I). Given the reported links between tuberculosis and HIV in the Ethiopian population, experiments to assess HIV status are currently underway. Likewise, more detailed neuropathological studies are being conducted in the suspected tuberculosis cases to address potential interactions with HIV.
Figure 1.
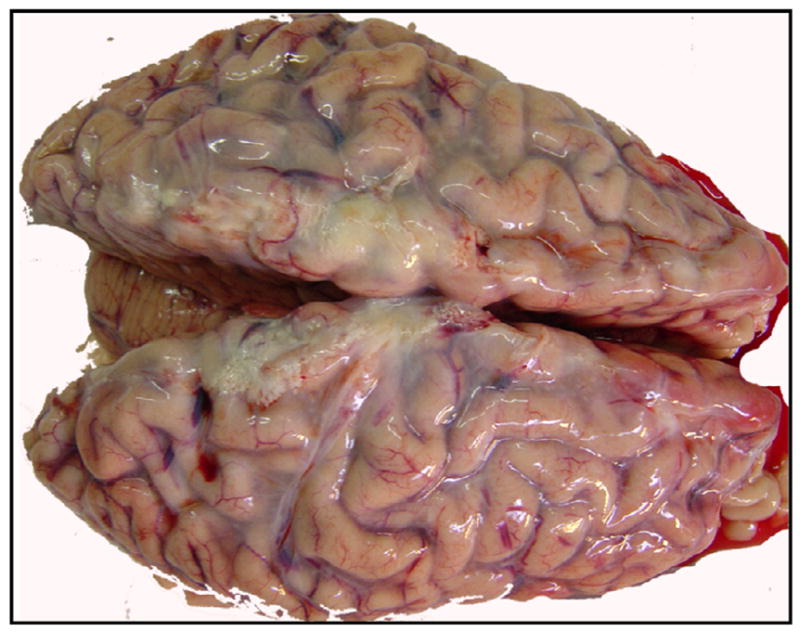
Whole brain from a 35-year-old patient who died from PTB with severe wasting syndrome, splenomegaly, and suspected HIV/AIDS. The brain atrophied, and a purulent exudate was observed over the entire brain.
Figure 2.
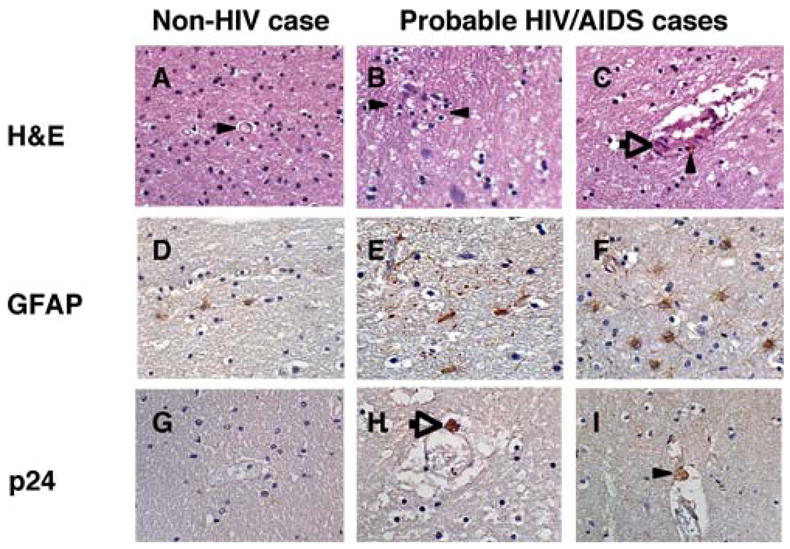
Neuropathological findings in sections from white matter tracts underlying frontal cortex stained with H&E (Panels A–C); anti-GFAP antibody (Panels D–F); or anti-HIV p24 antibody from a subset of autopsy cases from Addis Ababa. Panels A, D, G are sections from a 37-year-old individual who died from a gunshot wound to the abdomen, with no evidence of chronic illness or brain trauma; Panels B, E, H are sections from the case shown in Figure 1. Panels C, F, I are sections from a 55-year-old patient with PTB who died from pneumonia with hepatomegaly and suspected HIV/AIDS. A) H&E stain showing well-preserved white matter and vascular architecture (arrowhead), with no evidence of lymphocytic infiltration; B) H&E stain showing extensive vacuolarization of white matter and microglial nodular formation (arrow); C) H&E stain showing disruption of vascular architecture with white matter vacuolarization, lymphocytic and macrophage infiltration (arrowhead); D) GFAP immunoreactivity observed in a normal control; E) GFAP immunoreactive astrocytes surrounding an area suggestive of a migroglial nodule; F) GFAP immunoreactivity indicating reactive gliosis in a case with accompanying white matter damage; G) Absence of HIV-p24 immunoreactivty in the non-HIV case; H) HIV-p24 immunoreactive macrophage closely abutting capillary (arrow) with accompanying white matter vacuolarization; I) HIV-p24 immunoreactivity in a macrophage closely abutting capillary (arrowhead). H&E: hematoxylin and eosin; GFAP: glial fibrillary acidic protein; p24: HIV p24 protein.
Natural Deaths
In the natural deaths group, in 30 cases out of 98 (31%), death was attributed to pneumonia, and 12 (12%) were suspected of pulmonary M. Tuberculosis (PTB) (Table 2). Histopathological analyses of tissue sections from brain, lymph nodes, spleen, lung, liver, and adrenals confirmed tuberculosis in 21% of the natural deaths cases and in 8% of the injury-related deaths (see section below) (Table 4).
Table 4.
Histopathological Findings
| N: Ia related deaths n=185 | |
| NSFb | 39:59 |
| Tuberculosis | 21:7 |
| Pneumonia | 4:1 |
| Encephalitisc | 5:3 |
| Liver Disease | 14:5 |
| Brain hemorrhage | 6:0 |
| Solid organ hemorrhage | 3:3 |
| Other CNS findings | 7:9 |
Natural Deaths; N, Injury-related Deaths; I
no significant findings; NSF
Encephalitis group includes herpes simplex virus, cytomegalovirus or undefined cause. Other includes gliosis, thickened dura with thrombosis, abscess, papilloma virus, and hypoxic changes/neuronal loss.
Of the 98 natural deaths, 14 (14.3%) were classified as likely resulting from cardiac failure, 11 with gross pathological signs adequate to result in sudden death, as described previously [11, 12], and 3 without pathologies in the heart to explain sudden death. In these 3 cases, accompanying severe bilateral pulmonary congestion with brain edema was noted. Of the 14 cardiac cases, 1 was a female, age 35 with accompanying gastritis. The remaining 13 cases were male, ranging in ages from 18 to 78 years. Six of the 14 cases of heart failure (43%) were under the age of 50, and 8 were ≥ 50 years of age. Pathological findings from gross examination of the heart failure cases included obesity, chronic heart disease, atherosclerosis, pericarditis, enlarged heart and liver, lung and liver congestion, arachnoiditis, brain edema, ventricular hypertrophy, and gastritis. Our results that ~79% of the cases diagnosed with heart failure showed classic signs adequate to explain sudden death parallel those reported previously in an Ethiopian cohort [12].
Findings from histopathological examination of brain, lungs, lymph node, spleen, liver, and adrenal tissues from the natural causes group are reported in Table 4. Briefly, no significant histopathological observations were reported in 39 (40%) of these cases. Pneumonia was confirmed in 4, encephalitis in 5, liver disease in 14, brain hemorrhage in 6, and other solid organ hemorrhage in 3. In the natural deaths group, liver disease was present in 14 cases (Tables 2 and 4). Of these 14 cases, liver disease was determined to be the cause of death in 5 (36%). Each of these 5 patients suffered from cirrhosis. Of the remaining 9 cases where liver disease was found, 7 died from PTB, 1 from heart failure, and 1 from brain hemorrhage. Liver disease in these 9 cases was described as fatty liver. It is unknown whether alcohol abuse, high triglycerides, or diabetes contributed. Obesity was not present in any of these cases.
Injury-related Deaths
Results from our study indicate a greater percentage for intentional injury-related deaths (52%) than for unintentional (48%). Forty-six of these were homicides, and 1 of the asphyxiation/strangulation cases was reported as a suicide (Table 3). Sixty percent of the homicides resulted from trauma sustained from being beaten, and 21% were from gun shot wounds (GSW) (Table 3). The mean age in the intentional deaths group was 34±9.6 years. The GSW group was the youngest (30±7.4), and the asphyxiation/strangulation group was the oldest (39±9 years). Of the intentional injuries reported by the Ethiopian Ministry of Health in 1998–1999, 85% were listed as interpersonal in nature (including homicide). The information available for the present study did not include specifics of the homicide (e.g., interpersonal or others), thus no comment can be made regarding the nature of the crime. Statistics from two previous reports conducted over a 15 year period (1982–1996) indicated that suicide and attempted suicide accounted for 7% of injury cases reported, with 70.2 % of the suicides from hanging [13, 14]. The only suicide in our data set was by hanging (Table 3). In agreement with several other studies from developing countries [15], intentional injury victims in our study were predominantly male (89%). Thus, although limited to 47 cases, our study provides valuable indicators for age ranges, gender, and the most common causes of death from intentional injury among individuals in Addis Ababa.
Our data support previous reports that Ethiopia has the one of the worst fatality rates due to automobile accidents per 10,000 licensed drivers world-wide [16, 17]. Eighty percent of the accidental injury-related deaths described in this study resulted from automobile accidents; the mean age of victims was 35±14.1 years, and 22% of the victims were female (Table 3). Drowning, electrical shock, trauma from falling, and poisoning accounted for the remaining 20 % (Table 3).
Histopathological findings for the injury-related group are reported in Table 4. In some cases, more than one medical illness was confirmed. Briefly, no significant histopathological findings were reported in 59 (66%) of the injury-related deaths, and tuberculosis was confirmed in 7 (8%) cases of this group. Likewise, 3 cases showed evidence of encephalitis, 5 had liver disease, and 3 had solid organ hemorrhage. Of the 5 patients in the injury-related group with liver disease (Tables 4 and 5), 2 had hepatitis and 3 had cirrhosis. Of these 5 patients, 2 died in automobile accidents, 1 from carbon monoxide poisoning, and 1 from a fall. Nine cases of the 90 (10%) showed other significant CNS histopathological findings, including hypoxic changes with neuronal loss, papilloma virus infection of the spinal cord, and reactive gliosis (Table 4). Slides from 3 cases in the injury-related group were unavailable for examination at the time of analyses (Tables 4 and 5, n =185). Suspected illnesses observed by histopathological examination are grouped according to cause of injury-related death in Table 5. No cases of brain edema, brain hemorrhage, or hepato-splenomegaly were reported by histopathological analyses, and only one case of pneumonia was confirmed (data not shown).
Table 5.
Medical Illness by Histopathological Examination of Injury-related Deaths, n= 185.
| NSFa | TBb | Encephc | Liver disd | Solid organ heme | Other CNSf | No slidesg | |
|---|---|---|---|---|---|---|---|
| Asphyxiation/ Strangulation |
4 | 0 | 0 | 0 | 0 | 0 | 0 |
| Gun Shot Wound | 8 | 0 | 0 | 0 | 0 | 2 | 0 |
| Trauma from Beating | 16 | 3 | 2 | 1 | 1 | 3 | 1 |
| Stab Wounds | 5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Auto Accident | 21 | 4 | 1 | 2 | 2 | 4 | 2 |
| Drowning | 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Electric Shock | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Head Trauma (fall) | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Poisoning (CO2) | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
NSF, no significant findings;
TB, Tuberculosis;
Enceph, encephalitis;
Liver dis, liver disease;
Solid organ hem, solid organ hemorrhage;
Other CNS, other CNS findings including gliosis, thickened dura with thrombosis, abscess, papilloma virus, CMV, and hypoxic changes/neuronal loss;
No slides, no slides available at time of examination.
DISCUSSION
Fifty-two percent of autopsies conducted at the Forensic Medico-legal Pathology Department at Menelik II Hospital in Addis Ababa, Ethiopia, resulted from natural causes and 48 % from injury-related events. In agreement with studies conducted over two decades ago [8], a significant percentage of cases (21%) in the natural causes group in our study exhibited gross pathology consistent with pulmonary involvement according to observations at autopsy. Although cases included in the 1984 study resulted from either natural or injury-related events but were not medico-legal in nature, trends in cause were similar to those observed in our study.
The World Health Organization (WHO) estimated the life expectancy at birth for individuals in Ethiopia at 33.5 years in 1999 and 50 years in 2005 [18]. Results from our study indicated lower actual life spans by 7–16 years. However, our study included only 188 cases from a defined population and did not reflect the same population considered by WHO. Rather, our study describes information gathered from deaths of questionable cause where autopsy was deemed necessary by either the police and/or by the attending physician.
Tuberculosis was confirmed in 21% of the natural deaths cases and in 8% of the injury-related deaths from this study. According to WHO, the incidence of tuberculosis in Ethiopia in 2005 was estimated to be 341/100,000 pop/yr, and the prevalence was 546/100,000 pop [19]. Coinciding with the Ethiopian HIV epidemic, a tuberculosis epidemic also emerged, ranking Ethiopia 8th among countries with the highest tuberculosis burden [19]. HIV has played a key role in Tuberculosis by modifying the incidence and clinical presentation, and there is an estimated 57% prevalence of HIV among tuberculosis patients in Ethiopia [20, 21]. In response to the increasing severity of the HIV-tuberculosis problem, a direct-observation tuberculosis control (DOTS) program was instituted by Ethiopia at the recommendation of the WHO. Increased burden of dual infection is expected [22], with primary resistance to anti-tuberculosis drugs occurring significantly more often in dually infected patients [23].
With a population of over 3 million, HIV infection in the capital city of Addis Ababa was projected to be approximately 15.6%, while the prevalence in rural areas was only 3.7% [24]. Because the cases in this study were from Addis Ababa, the results do not take into account the populations outside of the city. Voluntary HIV testing is not widely accepted among individuals in Ethiopia [25, 26]. It is estimated that in many regions of Sub-Saharan Africa, less than 10% of people know their HIV status [26]. Factors such as stigma associated with a positive HIV status, lack of confidentiality, length of time waiting for results and logistics for obtaining a test contribute to the low numbers of individuals willing to receive tests. In some instances, people in Ethiopia have avoided visiting public clinics that offer, among their many services, HIV testing and treatment, for fear of being perceived by peers as having HIV. At a tuberculosis clinic in southern Ethiopia, the acceptability of HIV testing was assessed in 190 patients with tuberculosis [25]. Although all agreed initially, only 35% actually allowed the testing and of those tested, 21% were HIV positive [25]. Although the HIV status of persons included in this study is currently not known, data from other studies suggest that some of the patients in our study with tuberculosis likely are HIV-positive as well. Considering the low acceptance of HIV testing, it will be informative to confirm the number of HIV-positive individuals in the natural deaths group, as well as the injury-related group, since many of these individuals likely were unaware of their HIV status.
With regard to heart failure, a recent study conducted by Schneider and Bezabih reported that of 92 sudden deaths in Addis Ababa without an injury component, ~69% showed adequate morphological changes to explain sudden death of a cardiac nature, while ~22% showed some structural changes, inadequate though to explain sudden death, and ~8 % showed no cardiac abnormalities [12]. Our results that ~79% of the cases diagnosed with heart failure showed classic signs adequate to explain sudden death parallel those of Schneider and Bezahib.
Liver disease was present in 14 and 5% of the natural and injury-related groups, respectively. It is unknown if any of the patients that died from liver disease were chronic alcohol abusers or if alcohol played a role in their deaths. Likewise, of the cases included in this study that died from accidental or intentional injuries, it is unknown if alcohol was a contributor. In this regard, it is also unknown if alcohol use by drivers who survived the auto accidents was a contributor. Few studies have been conducted that address specifically alcohol abuse in Ethiopia. One study reported that among 10,468 persons 15 years of age and above, 16% met the criterion for problem drinking according to the CAGE questionnaire [27]. This study was conducted in Butajira, a small town outside of Addis Ababa with a population of around 40,000. Most studies involving drugs of abuse conducted in Ethiopia address Khat (Catha Edulis Frosk), a plant with amphetamine-like effects. It is unknown if Khat played a role in any of the deaths in these studies. Further studies are required to address these potential contributors to deaths in Addis Ababa.
Limited information exists regarding injury-related deaths in Ethiopia, and the accuracy of such reports is affected by under-reporting, misclassification, and the functional status of the reporting healthcare institution [16]. For example, the Ethiopian Ministry of Health statistics for 1998–1999 report that 18.6% of injuries were unintentional, 27.8% were intentional, and 53.6% were listed as “other” [16]. However, the percentage of injuries resulting in death was not reported [16]. Thus, the contribution that these injuries made to the death rate is unknown. Our data show that death from GSW was the most common means of homicide in younger adults. In the injury-related deaths group, a significant proportion of individuals showed signs of chronic illness, including tuberculosis, encephalitis, hepatic, or CNS disease.
Results from these data provide unbiased analyses of cause of death among the general population of Addis Ababa from both outside and within the hospital setting. Since cases meeting inclusion criteria were collected consecutively, our data represent a more accurate account of the most common causes of death among individuals for which autopsy was deemed necessary by medical or police officials. Data from autopsy studies provide valuable information regarding not only the cause of death but also the status of general health among individuals who died from injury-related events in Addis Ababa, Ethiopia.
Acknowledgments
National Institutes of Neurological Disease and Stroke (R21NS055639 to T.D.L), Minorities Health and Health Disparities Research Programs, National Institutes of Health (T3700067 to M.C.), National Institutes of Mental Health (the Center for AIDS Research at UCSD (Developmental award to T.D.L. from the HNRC Center Award P30 MH62512 to Igor Grant).
The authors wish to acknowledge Tenagne Alemu for his tireless efforts to make this project possible, Eliezer Masliah for significant efforts in data collection and neuropathological analyses, and the contributions of the HIV Neurobehavioral Research Center Group, whose multidisciplinary efforts have contributed to many of the insights contained in this paper. The HIV Neurobehavioral Research Center (HNRC) is supported by Center award MH 62512 from NIMH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lulu K, Berhane Y. The use of simplified verbal autopsy in identifying causes of adult death in a predominantly rural population in Ethiopia. BMC Public Health. 2005;5:58. doi: 10.1186/1471-2458-5-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Araya T, Reniers G, Schaap A, Kebede D, Kumie A, Nagelkerke N, Coutinho R, Sanders E. Lay diagnosis of causes of death for monitoring AIDS mortality in Addis Ababa, Ethiopia. Trop Med Int Health. 2004;9:178–86. doi: 10.1046/j.1365-3156.2003.01172.x. [DOI] [PubMed] [Google Scholar]
- 3.Reniers G, Araya T, Schaap A, Kumie A, Kebede D, Nagelkerke N, Coutinho R, Sanders EJ. Monitoring cause-specific adult mortality in developing countries: a comparison of data sources for Addis Ababa and its implications for policy and research. Soc Sci Med. 2005;61:1952–7. doi: 10.1016/j.socscimed.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 4.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandramohan D, Setel P, Quigley M. Effect of misclassification of causes of death in verbal autopsy: can it be adjusted? Int J Epidemiol. 2001;30:509–14. doi: 10.1093/ije/30.3.509. [DOI] [PubMed] [Google Scholar]
- 6.Cooper RS, Osotimehin B, Kaufman JS, Forrester T. Disease burden in sub-Saharan Africa: what should we conclude in the absence of data? Lancet. 1998;351:208–10. doi: 10.1016/S0140-6736(97)06512-4. [DOI] [PubMed] [Google Scholar]
- 7.Fantahun M, Fottrell E, Berhane Y, Wall S, Hogberg U, Byass P. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84:204–10. doi: 10.2471/blt.05.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gebre-Selassie L. Analysis of 256 autopsies at the Department of Pathology, Addis Ababa University. Ethiop Med J. 1984;22:29–33. [PubMed] [Google Scholar]
- 9.Sorenson SB, Shen H, Kraus JF. Undetermined manner of death. A comparison with unintentional injury, suicide, and homicide death. Eval Rev. 1997;21:43–57. doi: 10.1177/0193841X9702100103. [DOI] [PubMed] [Google Scholar]
- 10.Ma D, Bibbo L. Comprehensive Cytopathology. 2. Harcourt; 1997. Comprehensive Cytopathology; p. 707. [Google Scholar]
- 11.Davies MJ. The investigation of sudden cardiac death. Histopathology. 1999;34:93–8. doi: 10.1046/j.1365-2559.1999.00648.x. [DOI] [PubMed] [Google Scholar]
- 12.Schneider BKJ. Causes of sudden death in Addis Ababa, Ethiopia. Ethiop Med J. 2001;39:323–340. [PubMed] [Google Scholar]
- 13.Bekry A. Trends in suicide, parasuicide and accidental poisoning in children in Addis Ababa, Ethiopia. Ethiopian Journal of Health and Development. 1999;13:247–262. [Google Scholar]
- 14.Kebede D, Ketsela T. Suicide attempts in Ethiopian adolescents in Addis Abeba high schools. Ethiop Med J. 1993;31:83–90. [PubMed] [Google Scholar]
- 15.Smith GS, Barss P. Unintentional injuries in developing countries: the epidemiology of a neglected problem. Epidemiol Rev. 1991;13:228–66. doi: 10.1093/oxfordjournals.epirev.a036070. [DOI] [PubMed] [Google Scholar]
- 16.Taye M, Larson CP, Lindtjorn B. Unintentional and Intentional Injuries. In: Kloos H Berhane., editor. The Epidemiology and Ecology of Health and Disease in Ethiopia. Sharma Books; Addis Ababa: 2006. pp. 794–806. [Google Scholar]
- 17.Dessie T, Larson CP. The occurrence and driver characteristics associated with motor vehicle injuries in Addis Ababa, Ethiopia. J Trop Med Hyg. 1991;94:395–400. [PubMed] [Google Scholar]
- 18.WHO. Issues New Healthy Life Expectancy ratings. WHO press; 2006. [Google Scholar]
- 19.WHO. Global Tuberculosis Report WHO/CDS/TB/2001.287. WHO press; 2001. [Google Scholar]
- 20.Yassin MA, Takele L, Gebresenbet S, Girma E, Lera M, Lendebo E, Cuevas LE. HIV and tuberculosis coinfection in the southern region of Ethiopia: a prospective epidemiological study. Scand J Infect Dis. 2004;36:670–3. doi: 10.1080/00365540410020848. [DOI] [PubMed] [Google Scholar]
- 21.Bruchfeld J, Aderaye G, Palme IB, Bjorvatn B, Britton S, Feleke Y, Kallenius G, Lindquist L. Evaluation of outpatients with suspected pulmonary tuberculosis in a high HIV prevalence setting in Ethiopia: clinical, diagnostic and epidemiological characteristics. Scand J Infect Dis. 2002;34:331–7. doi: 10.1080/00365540110080025. [DOI] [PubMed] [Google Scholar]
- 22.Berggren Palme I, Gudetta B, Degefu H, Muhe L, Bruchfeld J, Giesecke J. A controlled estimate of the risk of HIV infection in Ethiopian children with tuberculosis. Epidemiol Infect. 2001;127:517–25. doi: 10.1017/s0950268801006215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demissie M, Lemma E, Gebeyehu M, Lindtjorn B. Sensitivity to anti-tuberculosis drugs in HIV-positive and -negative patients in Addis Ababa. Scand J Infect Dis. 2001;33:914–9. doi: 10.1080/00365540110076822. [DOI] [PubMed] [Google Scholar]
- 24.E. Ministry of Health. AIDS In Ethiopia. D. P. a. C. Department; MOH, Ethiopia: 2002. pp. 1–36. [Google Scholar]
- 25.Jerene D, Endale A, Lindtjorn B. Acceptability of HIV counselling and testing among tuberculosis patients in south Ethiopia. BMC Int Health Hum Rights. 2007;7:4. doi: 10.1186/1472-698X-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matovu JK, Makumbi FE. Expanding access to voluntary HIV counselling and testing in sub-Saharan Africa: alternative approaches for improving uptake, 2001–2007. Trop Med Int Health. 2007;12:1315–22. doi: 10.1111/j.1365-3156.2007.01923.x. [DOI] [PubMed] [Google Scholar]
- 27.Alem A, Kebede D, Kullgren G. The epidemiology of problem drinking in Butajira, Ethiopia. Acta Psychiatr Scand Suppl. 1999;397:77–83. doi: 10.1111/j.1600-0447.1999.tb10698.x. [DOI] [PubMed] [Google Scholar]


