Abstract
Co-occurring posttraumatic stress disorder (PTSD) is prevalent in addiction treatment programs and a risk factor for negative outcomes. Although interventions have been developed to address substance use and PTSD, treatment options are needed that are effective, well tolerated by patients, and potentially integrated with existing program services. This paper describes a cognitive behavioral therapy (CBT) for PTSD that was adapted from a treatment for persons with severe mental illnesses and PTSD in community mental health settings. The new adaptation is for patients in community addiction treatment with co-occurring PTSD and substance use disorders. In this study, 5 community therapists delivered the CBT for PTSD. Outcome data are available on 11 patients who were assessed at baseline, post-CBT treatment, and at a 3-month follow-up post-treatment. Primary outcomes were substance use, PTSD severity, and retention, of which all were favorable for patients receiving the CBT for PTSD.
Keywords: Co-occurring disorders, PTSD, CBT, addiction treatment
1. Introduction
Approximately 35% to 50% of people in addiction treatment programs have a lifetime diagnosis of posttraumatic stress disorder (PTSD), and 25% to 42% have a current diagnosis (Back et al., 2000; Brady, Back, & Coffey, 2004; P. J. Brown, Recupero, & Stout, 1995; Cacciola, Alterman, McKay, & Rutherford, 2001; Dansky et al., 1996; Jacobsen, Southwick, & Kosten, 2001; Mills, Lynskey, Teesson, Ross, & Darke, 2005; Ouimette, Ahrens, Moos, & Finney, 1997).
Co-occurring PTSD and substance use disorders add to greater problem severity in psychiatric, medical, social and employment functioning (Back et al., 2000; Brady, Killeen, Saladin, & Dansky, 1994; Najavits, Weiss, Shaw, & Muenz, 1998; Ouimette, Moos, & Finney, 2003; Trafton, Minkel, & Humphreys, 2006). These compounding severities have negative addiction treatment implications. Persons with PTSD respond less favorably to routine treatments, use more treatment services, are more likely to drop out of treatment, and are less likely to remain in continuing care. Further, although outcomes in substance use vary, psychiatric symptoms, health and psychosocial functioning are consistently worse (Brady et al., 1994; S. Brown et al., 1995; P. J. Brown, Stout, & Mueller, 1999; Hien, Nunes, Levin, & Fraser, 2000; Cacciola, Koppenhaver, Alterman, & McKay, 2009; McGovern, Drake, & Weiss, 2005; Mills, Teesson, Ross, Darke, & Shanahan, 2005; Ouimette, Finney, & Moos, 1999; Ouimette et al., 1997; Trafton et al., 2006).
Historically, addiction treatment programs did not address PTSD for fear of stimulating or exacerbating re-experiencing symptoms (nightmares, flashbacks, re-living traumatic events), and risk jeopardizing early and unstable periods of abstinence (S. Brown, 1985; Killeen et al., 2008).
Recently, four standardized behavioral interventions have been developed to address co-occurring PTSD and substance use disorders: Substance Dependence PTSD Therapy (SDPT) (Triffleman, Carroll, & Kellogg, 1999), Concurrent Treatment of PTSD and Cocaine Dependence (CTPCD) (Back, Dansky, Carroll, Foa, & Brady, 2001; Brady, Dansky, Back, Foa, & Carroll, 2001), Transcend (Donovan, Padin-Rivera, & Kowaliw, 2001) and Seeking Safety (SS) (Najavits et al., 1998; Najavits, 2002). The four interventions vary by approach, format, duration, setting, integration with addiction treatment (vs. stand alone), gender composition, retention rate, degree of research support for efficacy, and whether there is an active research program continuing to test and refine the therapy.
Only Transcend was developed as an integrated treatment and offered to patients with co-occurring PTSD and substance use disorders during addiction treatment-as-usual (Donovan et al., 2001). SDPT, CTPCD and SS were developed as stand alone therapies and recruited subjects via newspaper advertisements and postings. Therapists delivering the interventions in all for studies were experienced and carefully selected research clinicians with at least masters’ level degrees and most with doctorates.
Neither SDPT nor Transcend reported retention outcomes. CTPCD reported a retention rate of 39% (Brady et al., 2001). In two studies, SS was found to have retention rates of 63% (Najavits et al., 1998) and 61% (Hien, Cohen, Miele, Litt, & Capstick, 2004).
With respect to efficacy testing, although Transcend, SDPT and CTPCD had positive impact on PTSD symptoms, only SS was studied within a randomized controlled group design and found effective with PTSD symptoms. One study found that SS resulted in greater improvement than treatment as usual (Najavits et al., 1998), whereas a second study found SS had similar improvements in PTSD compared to a relapse prevention program (Hien et al., 2004). A third study of 12 session version of SS likewise found similar improvements in SS to a women’s health education program (Cohen & Hien, 2006; Hien, 2006). But, SS remains the only one of the four interventions (SS) with an active research program.
There is presently no actively researched behavioral treatment for PTSD specifically designed to be integrated within the context of existing addiction treatment services, for delivery to eligible patients receiving care and by typical community clinicians.
To this end, we selected and adapted a cognitive behavioral therapy (CBT) for PTSD program based upon the methods of cognitive restructuring, and with a proven track record with another at-risk comorbid population—persons with severe mental illnesses, including psychosis (Rosenberg, Mueser, Jankowski, Salyers, & Acker, 2004). In a randomized controlled trial, Mueser et al. (2008) found significant PTSD symptom reduction and excellent retention (81%).
Furthermore, typical community mental health clinicians were trained and supervised to deliver the CBT for PTSD, and did so with adequate competence and adherence. This suggests the potential for ease of translation to other community settings and typical clinicians who work within them.
Research has shown that exposure-based treatments for PTSD although effective, are undermined by high attrition rates. Treatment retention has been found to be better in cognitive restructuring vs. exposure-based approaches to PTSD (Marks, Lovell, Noshirvani, Livanou, & Thrasher, 1998; Tarrier et al., 1999). With respect to integrated treatments for PTSD and substance use disorders, CPTCD and SDPT are exposure-based approaches and though only CPTCD reported attrition (61%), it was high.
Given the need for continued development of behavioral treatments for co-occurring substance use and PTSD, particularly designed for delivery by typical addiction counselors in community addiction treatment programs, the rationale for testing a modification of the CBT for PTSD among patients with severe mental illnesses in community mental health settings seemed clear.
The present study aims to test the feasibility of the CBT for PTSD adapted for persons with co-occurring PTSD and substance use disorders in addiction treatment settings. This study intends to address three primary research questions:
Does CBT for PTSD in addiction treatment programs significantly reduce PTSD symptoms?
Does CBT for PTSD in addiction treatment programs significantly reduce substance use?
How does the retention rate of CBT for PTSD compare with other reported interventions for co-occurring PTSD and substance use disorders?
2. Methods
2.1 Design
This was a one-group, pre-test/post-test design with repeated measures at baseline, post-treatment and at 3-months post-treatment.
2.2 Setting
Subjects were recruited from three adult addiction treatment agencies’ intensive outpatient program level of care. Intensive outpatient programs (IOP) are 9-12 hours per week, 3-4 days or evenings, and are primarily rendered via group counseling formats. The focus is on patient and family education about addiction, developing coping skills to manage relapse, and arranging for continuing care. The planned duration of the intensive phase of treatment is 4-6 weeks, followed by weekly continuing care groups for an additional 2-3 months. The three settings were comparable in organization, staffing and clinical protocols. These sites were: Farnum Rehabiliation Center (Manchester, New Hampshire), FreshStart at Concord Hospital (Concord, New Hampshire) and Quitting Time at the Clara Martin Center (Wilder, Vermont). The CBT for PTSD was delivered during the course IOP and continuing care and delivered on site.
2.3 Intervention
CBT for PTSD in addiction treatment programs is a manual-guided individual therapy. CBT for PTSD imparts 3 learning and skill components to patients in order to improve PTSD symptoms and substance use: 1) Patient education about PTSD and its relation to substance use and treatment; 2) Breathing retraining: A behavioral anxiety reduction skill; and 3) Cognitive restructuring: A cognitive approach and functional analysis of the link among emotions, cognitions and situations. Although cognitive restructuring forces neither in vivo or imaginal exposure per se, it does address avoidance symptoms by teaching cognitive processing of trauma-related thoughts, affects and experiences. Thus, patient education, anxiety reduction skill development, reduced avoidance and cognitive processing are all ingredients of the CBT for PTSD. These ingredients are core to all effective PTSD therapies (Keene, 2009). The CBT for PTSD manual has 8 modules: 1) Introduction to the treatment; 2) Crisis and Relapse Prevention Plan; 3) Breathing Retraining; 4) PTSD: Primary Symptoms; 5) PTSD: Associated Symptoms; 6) Cognitive Restructuring: The first 3 steps; 7) Cognitive Restructuring: The 5-step program; and 8) Generalization Training and Termination. Eight to twelve sessions are necessary to cover all 8 modules (some sessions cover more than one module; some modules take more than one session to cover). A client workbook is used in conjunction with the therapist manual, and, as with most cognitive behavioral therapies, the approach includes homework between sessions, patient education and self-monitoring, skill acquisition, implementation and practice, and developing self-efficacy about more adaptive and alternative cognitions and behaviors.
2.4 Therapist selection, training and supervision
Therapist training and supervision in CBT for PTSD in this study consisted of an initial 90-minute didactic overview and then twice monthly individual telephone supervision, and twice per month face-to-face individual supervision. All sessions were audio taped and rated by independent raters for CBT for PTSD in addiction treatment using the Adherence and Competence Index (ACI). In exchange for training and supervision, five community therapists volunteered for participation in this study: A licensed psychiatric nurse practitioner; a licensed doctoral level clinical psychologist; a licensed masters’ level clinical social worker; an intern in masters’ degree mental health counseling program; and, a masters’ level rehabilitation counselor.
Therapy session audiotapes were rated by independent raters and overall, found to be at a satisfactory level of adherence and good level of competence. All therapists received a score of at least a 4 on the 7-point adherence and competence scales, which was considered a priori to be adequate. No therapy courses or therapists were disqualified on the basis of poor adherence or lack of competence.
2.5 Subjects
Subjects were recruited from the three addiction treatment programs. Within the first week of admission, patients were administered the PTSD Checklist (PCL). The PCL is a diagnostic screening measure and includes a list of traumatic life events (DSM-IV PTSD diagnosis criterion A) and is followed by 17 symptom related items pertaining to DSM-IV PTSD diagnosis criteria B (re-experiencing), C (avoidance) and D (hyper-arousal). Symptoms are rated on a 5-point scale in terms of “how much bothered by” from 1-Not at all to 5-Extremely. Scores of 44 or more have been found to be diagnostic of PTSD (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996)
Patients screening positive for PTSD on PCL were approached for research participation consent. This research study was reviewed and approved by the Trustees of Dartmouth College Committee for the Protection of Human Subjects, the State of New Hampshire Department of Health and Human Services Committee for the Protection of Human Subjects, and the Human Investigation Committee at Concord Hospital.
Twenty-three patients were assessed as eligible for study participation. Eleven patients started the therapy (i.e., attended at least two sessions of CBT) and received at least one follow-up assessment. In the results section, baseline differences between completers vs. non-completers and those for whom follow-up data were available are presented.
2.6 Measures
The primary outcome measure for PTSD was the Clinician Administered PSTD Scale (CAPS) (Blake et al., 1998). The CAPS is a structured diagnostic interview conducted by a trained interviewer. The CAPS derives an overall severity score (44 or more is considered a positive PTSD diagnosis), subscale scores on the B (re-experiencing), C (avoidance) and D (hyper-arousal) criteria, and a PTSD diagnosis (present/absent). CAPS ratings can be made for lifetime or current symptoms. For this research, ratings were based on current symptoms (past 30 days).
The primary outcome measures for substance use were: Time-Line Follow-Back Calendar (TLFB) (Sobell, Maisto, Sobell, & Cooper, 1979), urine toxicology and breathalyzer data, and the Addiction Severity Index drug and alcohol composite scores (ASI) (McLellan, Luborsky, Woody, & O’Brien, 1980). The measure of retention was set a priori, with a designation of completion at 8 or more sessions attended, i.e. 75% of planned dose.
2.7 Data Analyses
SAS 9.2 and SPSS 15.0 were used to conduct all data analyses (SAS Institute Inc., 2008; SPSS, 2006). Univariate statistics were used to describe the demographic (age, gender, ethnicity) and baseline clinical characteristics of the sample (PTSD severity, substance use) (SPSS, 2006).
Generalized Estimating Equations (GEE) modeling an appropriate technique for correlated and incomplete data, were used to measure average change in PTSD severity (CAPS scores) and substance use (TLFB, positive toxicology data, and ASI Alcohol and Drug Severity Composite scores) across the 3 assessment periods (baseline, post-treatment, 3-month post-treatment).
Specific difference between baseline to post-treatment, baseline to 3-month post-treatment, and between post-treatment to 3-month post-treatment means were also assessed (SAS Institute Inc., 2008). Survival analysis curve was used to track retention in the CBT over number of sessions attended.
3. Results
3.1 Patient demographic and baseline clinical characteristics
The mean age of the sample was 34.4 (sd=8.8). The patients were all Caucasian and predominately female (91%). All patients were positive for PTSD at baseline assessment with an average CAPS Total Score of 73.9 (sd=13.9). Patients scored an average of 21.1 (sd=5.4) on the CAPS B criteria score (re-experiencing), 29.6 (sd=6.8) on the CAPS C criteria score (avoidance), and 23.1 (sd=6.1) on the CAPS D criteria score (hyper-arousal). These scores are indicative of a severe level of PTSD symptom severity. The majority of patients experienced a childhood sexual assault (81.8%). The second most common trauma was being involved in an accident (45.5%). (See Table 1).
Table 1.
Patient demographics and baseline clinical characteristics (n=11)
| Demographics | |
|---|---|
| Age Mean(sd) | 34 (8.8) |
| Gender (Male) | 9% |
| Race (Caucasian/White) | 100% |
| Baseline: PTSD severity | |
| PTSD Diagnosis: Positive | 100% |
| CAP Score Total | 73.9 (13.9) |
| CAPS B Criteria (Re-experiencing) | 21.2 (5.4) |
| CAPS C Criteria (Avoidance) | 29.6 (6.8) |
| CAPS D Criteria (Increased Arousal) | 23.1 (6.3) |
| Trauma Types | |
| Childhood Sexual Assault | 81.8% |
| Childhood Physical Assault | 36.4% |
| Adult Sexual Assault | 9.1% |
| Adult Physical Assault | 36.4% |
| Accident | 45.5% |
| Disaster | 0.0% |
| Tragic Death | 9.1% |
| Hazardous Duty | 9.1% |
| Chronological sequence of trauma and substance use | |
| Trauma > Substance use | 27.3% |
| Trauma > Substance use > Trauma > Substance use | 63.6% |
| Substance use > Trauma | 9.1% |
| Baseline: Substance Severity | |
| Objective measures | |
| Urine Toxicology Negative | 81.8% |
| Alcohol positive breathalyzer | 0.0% |
| 3-month Timeline Follow Back | |
| Mean number of days drinking | 24.7 (25.7) |
| Mean number of days using drugs | 15.6 (26.9) |
| ASI Composite Scores | |
| Alcohol | .41 (.12) |
| Drug | .19 (.14) |
More than half of the patients began using substances after they experienced either one or multiple traumatic life events (63.6%).
At baseline, eighty-two percent (82%) of the patients tested negative on a urine toxicology screen and none had a positive alcohol breathalyzer test. Using the TLFB, in the past 90 days, patients spent approximately 25 days using alcohol and 16 days using drugs (See Table 1).
3.2 PTSD severity
As shown in Figure 1, there was a substantial decrease in current PTSD diagnosis (meeting diagnostic criteria over past 30 days) from baseline (100% PTSD positive) to post-treatment (27% PTSD positive) to 3-month post-treatment (20% PTSD positive). As shown in Table 2, there was a significant change over time on the current (past 30 days) CAPS Total Score, as well as the CAPS B, C and D criterion score (χ2=79.21, 2 df, p<.0001; χ2=51.85, 2 df, p<.0001; χ2=45.59, 2 df, p<.0001, χ2=29.81, 2 df, p<.0001). The CAPS Total and CAPS C criteria score at post-treatment and 3-month post-treatment were significantly different from baseline levels (χ2=343.02, 1 df, p<.0001; χ2=46.05, 1 df, p<.0001; χ2=226.82, 1 df, p<.0001; χ2=18.71, 1 df, p<.0001). There was also a significant change between the post-treatment and the 3-month post-treatment (χ2=29.85, 1 df, p<.0001; χ2=11.81, 1 df, p=.001) (See Table 2). For the CAPS B criteria and CAPS D criteria scores, there was a significant change between baseline and post-treatment, baseline and 3-month post-treatment (χ2=24.79, 1 df, p<.0001; χ2=51.31, 1 df, p<.0001; χ2=20.70, 1 df, p<.0001; χ2=29.15, 1 df, p<.0001), but no significant change between post-treatment and 3-month post-treatment (χ2=1.03, 1 df, p=.31; χ2=1.99, 1 df, p=.16).
Figure 1.
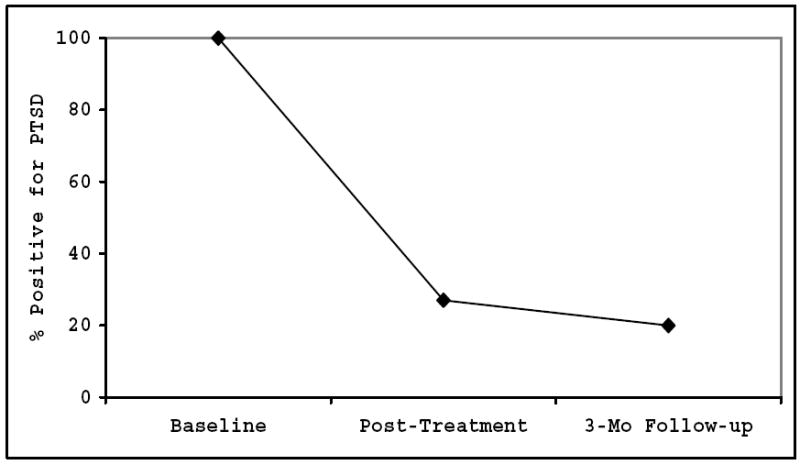
CAPS Diagnosis
Table 2.
PTSD Severity
| Baseline n=11 | Post-Tx n=11 | 3-Mo Post-Tx n=10 | χ2 | |
|---|---|---|---|---|
| Mean | Mean | Mean | ||
| CAPS Score Total | 74a | 37b | 28b,c | 79.21*** |
| CAPS B Criteria (Re-experiencing) | 21a | 9b | 8b | 51.85*** |
| CAPS C Criteria (Avoidance) | 30a | 14b | 9b,c | 45.59*** |
| CAPS D Criteria (Increased Arousal) | 23a | 14b | 12b | 29.81*** |
Items with the superscript b are significantly different from baseline;
Items with the superscript c are significantly different from Post-Tx;
p<.05;
p<.01;
p<.001
3.3 Substance use
There were no significance changes over time in urine toxicological outcomes from baseline (82% negative), post-treatment (80% negative), and 3-mo post-treatment (80% negative). Also, the breathalyzer test remained negative over time. Although there was a reduction in the days of alcohol use between baseline and post-treatment, it was not at a significant level. There were no significant changes in the number of days drinking or using drugs over time. There were significant decreases among several of the ASI alcohol and drug severity composite scores (χ2=8.36, 2 df, p=.02; χ2=6.76, 2 df, p=.03). There was a significant decrease in the ASI alcohol severity composite score between baseline & post-treatment and baseline & 3-month post-treatment (χ2=5.64, 1 df, p=.02; χ2=5.68, 1 df, p=.02). There were no significant changes between post-treatment and 3-month post treatment (χ2=0.08, 1 df, p=.77). Similarly, we found a significant reduction in the ASI drug severity composite score from baseline to post-treatment and baseline to 3-month post-treatment, but no significant decrease from post-treatment to 3-month post-treatment (χ2=4.18, 1 df, p.04; χ2=6.54, 1 df, p=.01; χ2=0.06, 1 df, p=.81).
3.4 Retention
Examining the a priori definition of retention (75% of total planned, fifteen of the twenty-three patients (65%) completed at least 8 sessions of CBT. This rate is comparable to SS (61-63%) and better than CTPCD (39%), the latter being an exposure-based approach. On average, completers attended 10.5 CBT sessions over the course of treatment (See Figure 1).
Using intent to treat analyses, we compared the 15 study subjects (completers) to the 8 subjects who did not complete treatment. We found no significant t-test differences on baseline demographic or clinical characteristics (PTSD and substance use severity) between the two groups. Although not statistically significant, non-completers tended reporting less childhood sexual or physical assault, and scored lower on the CAPS total score. There were no differences on substance use severity measures.
In addition, we compared baseline characteristics of those patients for whom follow-up data were available (n=11) with those for whom we were unable to obtain follow-up information (n=12). The groups did not differ (t-tests) on demographic characteristics (age, gender), PTSD symptom severity (CAPS total score), or substance use severity (ASI composite scores).
Finally, we compared the baseline characteristics of treatment completers with follow-up information (n=11) with non-completers without follow-up data (n=8). The t-test comparisons yielded no significant differences.
4. Discussion
4.1 Summary of findings
The present findings provide support for the feasibility of CBT for PTSD for patients with these co-occurring disorders in community addiction treatment settings.
CBT for PTSD had significant impact on current CAPS PTSD diagnosis: Only 27% were positive for PTSD post-treatment, and even fewer (20%) were PTSD positive at 3-month follow-up. This suggests that changes made during treatment can be sustained over a short period of time outside of treatment.
Patients who received CBT for PTSD also experienced significant reductions in substance use and in substance use severity. But, since patients were also receiving intensive outpatient program addiction treatment services it is unclear how much these changes may be associated with this treatment as usual vs. the specific mechanisms of CBT. Finally, using a conservative estimate of retention (75% of planned sessions) as criteria, 65% of patients completed the therapy.
Although the retention rate compares favorably to other treatments for co-occurring PTSD and substance use, treatment engagement and completion remains a challenge for these patients. The present study could not identify significant differences in baseline characteristics (predictors of attrition) though less severe PTSD and trauma type were notable trends.
4.2 Limitations
Since this study lacks the experimental rigor associated with a randomized controlled trial, there are many threats to internal and external validity. First, at this juncture we cannot, with absolute scientific confidence, attribute the changes in PTSD symptoms and substance use to the CBT for PTSD. Since there is no comparison condition, these changes may have occurred naturalistically, or by participation in the intensive outpatient addiction treatment alone. Second, we have no specific measure of the potential for volunteer bias. This study may have an unusual sample of persons in addiction treatment with PTSD. Perhaps the patients who did not provide informed consent are more severe and at greater risk for negative treatment outcomes. Third, although the therapists in this study were volunteers from the community vs. elite research therapists, they were nonetheless not community addiction counselors. It remains unclear how simple and easy to implement the CBT for PTSD in addiction treatment may be until community-based addiction counselors are trained and supervised in the approach, and their adherence and competence measured over time.
The finding that CBT for PTSD compares favorably in primary outcomes (PTSD and substance use) to one established treatment (SS) and has better retention (vs. SS and CTPCD) lends support to its promise, but cannot, at the present stage of research development, argue for its efficacy.
4.3 Future research
The limitations noted also chart the course for the next phase of behavioral therapy development (Onken, Blaine, & Battjest, 1997; Rounsaville, Weiss, & Carroll, 1999; Rounsaville, Carroll, & Onken, 2001). This next stage would compare the CBT for PTSD plus addiction treatment as usual versus addiction treatment as usual plus a matched attention control or an intervention targeting something other than PTSD. The findings from this more rigorous study will shed more light on the potential efficacy and change mechanisms of CBT for PTSD. The challenges of treatment engagement and retention must also be considered in research design and the CBT for PTSD intervention refinement. Adding upfront motivational enhancement strategies to enlist patient “buy-in” to address PTSD within the context of addiction treatment seem warranted.
Further, understanding the types of addiction treatment programs for patients who are likely to benefit from a specialized PTSD interventions, and the longer term cost-benefits of providing or not providing integrated care remains unknown (Flynn & Brown, 2008; Schneider, Cronkite, & Timko, 2008).
Figure 2.
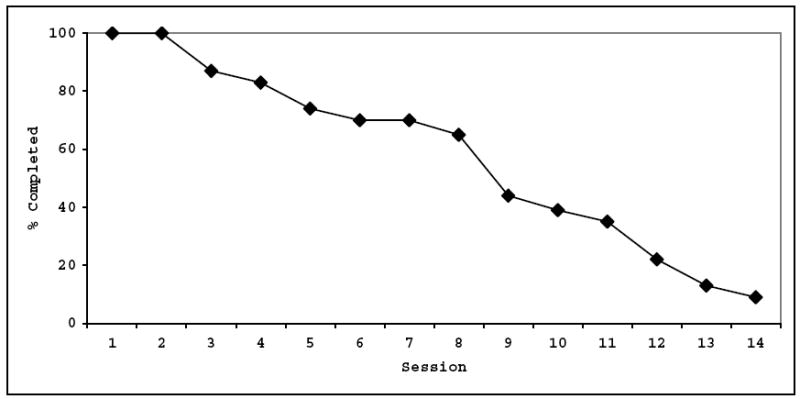
CBT for PTSD treatment retention
Table 3.
Substance Use Severity
| Baseline n=11 | Post-Tx n=11 | 3-Mo Post-Tx n=10 | χ2 | |
|---|---|---|---|---|
| Mean | Mean | Mean | ||
| 3-Month Timeline Follow Back | ||||
| Number of days drinking | 24.7 | 4.9 | 6.5 | 4.40 |
| Number of days using drugs | 15.6 | 2.2 | 1.6 | 1.73 |
| ASI Composite Scores | ||||
| Alcohol | .41a | .29b | .27b | 8.36* |
| Drug | .19a | .13b | .12b | 6.76* |
p<.05,
p<.01,
p<.001;
Items with the superscript b are significantly different from baseline in the GEE model;
Items with the superscript c are significantly different from Post-Tx
Acknowledgments
This research was supported by NIDA grant K23 DA 16574-01A (McGovern) and NIDA grant K24DA022288 (Weiss). The authors thank the patients and staff of the Farnum Rehabilitation Center (Manchester, New Hampshire), FreshStart at Concord Hospital (Concord, New Hampshire) and Quitting Time at the Clara Martin Center (Wilder, Vermont). We also want to acknowledge the contributions of Stephen Higgins, Kim Mueser, Lois Hollow, Karen Gillock, Ellen Eberhart, Jim Gamache, Melissa Edney, and Aurora Matzkin.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Mark P. McGovern, Dartmouth Medical School
Chantal Lambert-Harris, Dartmouth Medical School.
Stephanie Acquilano, Dartmouth Medical School.
Haiyi Xie, Dartmouth Medical School.
Arthur I. Alterman, University of Pennsylvania
Roger D. Weiss, McLean Hospital, Harvard Medical School
References
- Back SE, Dansky BS, Carroll KM, Foa EB, Brady KT. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Description of procedures. Journal of Substance Abuse Treatment. 2001;21(1):35–45. doi: 10.1016/s0740-5472(01)00181-7. [DOI] [PubMed] [Google Scholar]
- Back SE, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without post-traumatic stress disorder: A comparison of substance use, trauma history and psychiatric comorbidity. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2000;9(1):51–62. doi: 10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM. Clinician administered PTSD scale for DSM-IV. White River VT: National Center for PTSD; 1998. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. Journal of Substance Abuse Treatment. 2001;21(1):47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- Brady KT, Killeen T, Saladin ME, Dansky B. Comorbid substance abuse and posttraumatic stress disorder: Characteristics of women in treatment. The American Journal on Addictions. 1994;3(2):160–164. [Google Scholar]
- Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addictive Behaviors. 1995;20(2):251–254. doi: 10.1016/0306-4603(94)00060-3. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors. 1999;13(2):115–122. [Google Scholar]
- Brown S. Treating the alcoholic. New York, NY: Wiley; 1985. [Google Scholar]
- Cacciola JS, Alterman AI, McKay JR, Rutherford MJ. Psychiatric comorbidity in patients with substance use disorders: Do not forget axis II disorders. Psychiatric Annals. 2001;31:321–331. [Google Scholar]
- Cacciola JS, Koppenhaver J, Alterman AI, McKay JR. Posttraumatic stress disorder and other psychopathology in substance abusing patients. Drug and Alcohol Dependence. 2009;101(12):27–33. doi: 10.1016/j.drugalcdep.2008.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen LR, Hien DA. Treatment outcomes for women with substance abuse and PTSD who have experienced complex trauma. Psychiatric Services (Washington, D.C.) 2006;57(1):100–106. doi: 10.1176/appi.ps.57.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dansky BS, Brady KT, Saladin ME, Killeen T, Becker S, Roitzsch JC. Victimization and PTSD in individuals with substance use disorders: Gender and racial differences. The American Journal of Drug and Alcohol Abuse. 1996;22(1):75–93. doi: 10.3109/00952999609001646. [DOI] [PubMed] [Google Scholar]
- Donovan B, Padin-Rivera E, Kowaliw S. “Transcend”: Initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress. 2001;14(4):757–772. doi: 10.1023/A:1013094206154. [DOI] [PubMed] [Google Scholar]
- Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: Issues and prospects. Journal of Substance Abuse Treatment. 2008;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA. Preliminary findings from the “women and trauma” study. Presented at the annual meeting of the NIDA Clinical Trials Network; St. Petersburg, Florida. December 7.2006. [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. The American Journal of Psychiatry. 2004;161(8):1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hien DA, Nunes E, Levin FR, Fraser D. Posttraumatic stress disorder and short-term outcome in early methadone maintenance treatment. Journal of Substance Abuse Treatment. 2000;19(1):31–37. doi: 10.1016/s0740-5472(99)00088-4. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: A review of the literature. American Journal of Psychiatry. 2001;158(8):1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Keene T. State of the art treatment for PTSD. Paper presented at the NIDA meeting on Addressing Substance Abuse and Comorbidities Among Military Personnel, Veterans, and Their Families: A Research Agenda; Bethesda, Maryland. January 6.2009. [Google Scholar]
- Killeen T, Hien D, Campbell A, Brown C, Hansen C, Jiang H, et al. Adverse events in an integrated trauma-focused intervention for women in community substance abuse treatment. Journal of Substance Abuse Treatment. 2008;35:304–311. doi: 10.1016/j.jsat.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks I, Lovell K, Noshirvani H, Livanou M, Thrasher S. Treatment of posttraumatic stress disorder by exposure and/or cognitive restructuring: A controlled study. Archives of General Psychiatry. 1998;55(4):317–325. doi: 10.1001/archpsyc.55.4.317. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Drake KM, Weiss RD. Co-occurring PTSD and substance use disorders in community addiction treatment: Prevalence, retention and treatment outcomes. Paper presented at the annual meeting of the College on Problems of Drug Dependence, Orlando; Florida. June 22.2005. [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. The Journal of Nervous and Mental Disease; the Journal of Nervous and Mental Disease. 1980;168(1):26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Mills KL, Lynskey M, Teesson M, Ross J, Darke S. Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): Prevalence and correlates. Drug and Alcohol Dependence. 2005;77(3):243–249. doi: 10.1016/j.drugalcdep.2004.08.016. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Darke S, Shanahan M. The costs and outcomes of treatment for opioid dependence associated with posttraumatic stress disorder. Psychiatric Services. 2005;56(8):940–945. doi: 10.1176/appi.ps.56.8.940. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, et al. A randomized controlled trial of cognitive-behavioral treatment for post-traumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology. 2008;76(2):259–271. doi: 10.1037/0022-006X.76.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM. Clinicians’ views on treating posttraumatic stress disorder and substance use disorder. Journal of Substance Abuse Treatment. 2002;22:79–85. doi: 10.1016/s0740-5472(02)00219-2. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. Journal of Traumatic Stress. 1998;11(3):437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Onken LS, Blaine JD, Battjest R. Behavioral therapy research: A conceptualization of a process. In: Henngler SW, Amentos R, editors. Innovative approaches for difficult to treat populations. Washington, DC: American Psychiatric Press; 1997. pp. 477–485. [Google Scholar]
- Ouimette PC, Ahrens C, Moos RH, Finney JW. Posttraumatic stress disorder in substance abuse patients: Relationship to 1-year posttreatment outcomes. Psychology of Addictive Behaviors. 1997;11(1):34–37. [Google Scholar]
- Ouimette PC, Finney JW, Moos RH. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13(2):105–114. [Google Scholar]
- Ouimette PC, Moos RH, Finney JW. PTSD treatment and 5-year remission among patients with substance abuse and posttraumatic stress disorders. Journal of Consulting and Clinical Psychology. 2003;71(2):410–414. doi: 10.1037/0022-006x.71.2.410. [DOI] [PubMed] [Google Scholar]
- Rosenberg SD, Mueser KT, Jankowski MK, Salyers MP, Acker K. Cognitive-behavioral treatment of PTSD in severe mental illness: Results of a pilot study. American Journal of Psychiatric Rehabilitation. 2004;7(2):171–186. [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science & Practice. 2001;8:133–142. [Google Scholar]
- Rounsaville BJ, Weiss RD, Carroll KM. Options for managing psychotropic medications in drug-abusing patients participating in behavioral therapies clinical trials. American Journal on Addictions. 1999;8:178–189. doi: 10.1080/105504999305794. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. SAS/STAT user’s guide. Cary, NC: SAS Institute Inc; 2008. [Google Scholar]
- Schneider R, Cronkite R, Timko C. Lifetime physical and sexual abuse and substance use treatment outcomes in men. Journal of Substance Abuse Treatment. 2008;35:353–361. doi: 10.1016/j.jsat.2008.01.001. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behavioral Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- SPSS, Inc. SPSS 15.0 for windows. Chicago, IL: SPSS, Inc; 2006. [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, et al. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 1999;67(1):13–18. doi: 10.1037//0022-006x.67.1.13. [DOI] [PubMed] [Google Scholar]
- Trafton JA, Minkel J, Humphreys K. Opioid substitution treatment reduces substance use equivalently in patients with and without posttraumatic stress disorder. Journal of Studies on Alcohol. 2006;67(2):228–235. doi: 10.15288/jsa.2006.67.228. [DOI] [PubMed] [Google Scholar]
- Triffleman E, Carroll K, Kellogg S. Substance dependence posttraumatic stress disorder therapy: An integrated cognitive-behavioral approach. Journal of Substance Abuse Treatment. 1999;17(12):3–14. doi: 10.1016/s0740-5472(98)00067-1. [DOI] [PubMed] [Google Scholar]


