Abstract
The purpose of this study was to compare substance involvement among psychiatrically hospitalized adolescent smokers who had received motivational interviewing (MI) versus a brief advice (BA) for smoking cessation. One hundred and ninety-one (191) adolescent smokers (62.3% female; 15.4 years of age) were randomly assigned to MI (n=116) or BA (n=75). All patients were assessed at baseline, immediately after hospitalization, and at 1-, 3-, 6-, 9-, and 12-month follow-ups. Rates of substance use in the MI condition during follow-up increased from a low of 8.2% (SD = 18.5) to a high of 15.4% (SD = 30.0) substance use days. Whereas in BA, substance use days increased from a low of 8.4% (SD = 20.8) to a high of 21.4% (SD = 35.2). The results of this study suggest that MI, relative to BA, for smoking cessation was associated with better substance use outcomes during the first six months following psychiatric hospitalization among adolescents. This finding is consistent with previous studies that have shown that smoking cessation does not have a detrimental effect on substance abuse treatment outcomes among youth.
Keywords: Adolescents, substance use outcomes, motivational interviewing, smoking cessation, inpatient treatment, psychiatric comorbidity
1. Introduction
1.1. Comorbid smoking and alcohol and drug involvement among adolescents
Smoking and other substance involvement among adolescents continue to be a significant public health problem in the United States. Twenty-two percent of high school seniors report using an illicit drug, while even a greater number of teens have used alcohol (44%) in the last month (Johnston, O’Malley, Bachman, & Schulenberg, December 11, 2007). In the same survey, 22% of high school seniors reported using tobacco in the last month (Johnston et al., December 11, 2007). Significant impairments are associated with adolescent substance involvement, such as poor academic functioning (e.g., (Brook, Stimmel, Zhang, & Brook, 2008), family dysfunction (e.g., (Dakof, 2000), health problems (Mertens, Flisher, Fleming, & Weisner, 2007) and psychiatric comorbidity (e.g., (Deas & Brown, 2006).
In addition, there exists high comorbidity between smoking and other alcohol and drug involvement in both adult and adolescent populations. For example, among adolescents in substance abuse treatment, the majority of youth (66–85%) report currently smoking (Chun, Guydish, & Chan, 2007; Myers & Brown, 1994). Similarly, among smoking adolescents in an inpatient psychiatric treatment program, 74% also met criteria for an alcohol and/or drug use disorder (Ramsey et al., 2003). Prospective studies have demonstrated that smoking increases the risk for the onset of a substance use disorder among adolescents (Brook, Brook, Zhang, Cohen, & Whiteman, 2002; Mathers, Toumbourou, Catalano, Williams, & Patton, 2006). In addition, the reverse relationship also appears to exist with the progression of alcohol and drug involvement in youth leading to initiation and increases in cigarette use (Ellickson, McGuigan, & Klein, 2001).
1.2. Substance use outcomes after smoking cessation treatment
Traditionally, the treatment of individuals with comorbid nicotine and other substance dependence has been focused on addressing what has often been considered the more serious of the two, the alcohol and/or drug use problem (Battjes, 1988). In fact, most clinicians hesitated to address smoking behavior for fear it would hinder substance use treatment efforts (Bobo, 1989). However, there is evidence to suggest that continued smoking is associated with poorer substance abuse treatment outcomes among drug dependent adults (e.g., (Frosch, Shoptaw, Nahom, & Jarvik, 2000). In addition, making a smoking quit attempt has also been associated with greater days abstinent for alcohol and illicit drugs among individuals seeking substance abuse treatment (Kohn, Tsoh, & Weisner, 2003). Among adolescents treated for substance abuse, initial evidence also indicates that receiving a smoking cessation intervention may be associated with better short-term outcomes (Myers & Prochaska, 2008). Therefore, the notion that smoking treatment would negatively interfere with rates of substance involvement has not received empirical support (Myers, 1999; Myers & Prochaska, 2008).
As a result, researchers have recently begun to make the argument that smoking treatment could actually have a positive effect on substance use outcomes. For example, Burling and colleagues (Burling, Burling, & Latini, 2001) stated that smoking cessation treatment, through the encouragement of making lifestyle changes, promoting a sense of mastery and self-efficacy, and practicing relapse prevention skills, could generalize to substance use. In a recent meta-analysis, Prochaska and colleagues (Prochaska, Delucchi, & Hall, 2004) examined outcomes of smoking cessation interventions from 19 randomized controlled trials with individuals in addictions treatment or recovery. The results of the meta-analysis pointed toward the positive effect of smoking cessation treatment which increased the likelihood of long-term abstinence from alcohol and drugs by an average of 25%. Similarly, among adolescent populations, studies have demonstrated that smoking interventions do not detrimentally influence substance use outcomes (Myers & Brown, 2005; Myers, Brown, & Kelly, 2000) and may actually be beneficial (Myers & Prochaska, 2008).
1.3. The present study
This line of research, especially with adolescent populations, is relatively new. Most of the previous studies have been conducted by presenting a smoking intervention to substance abusing adult populations in treatment for alcohol and drug use problems. Much less is known about the influence of smoking cessation programs on substance abusing adolescents who are not specifically receiving treatment for alcohol and drug problems. The purpose of this study was to compare substance involvement among adolescent smokers in a psychiatric inpatient facility who had received either a motivational interviewing intervention or brief advice for smoking cessation. Based on studies of smoking cessation for adults and youth in substance abuse treatment, it was hypothesized that participants receiving the active (motivational enhancement) smoking cessation intervention would evidence improved substance use outcomes compared with those in the brief advice condition.
2. Method
2.1. Procedure
The study will be described only briefly as details of the study including recruitment, inclusion/exclusion criteria, and follow-up rates are available in Brown, et al, (Brown et al., 2003). Adolescent smokers ages 13–17 who were admitted to the inpatient psychiatric program were recruited for participation in a smoking cessation study. All participants provided written assent for study participation, and written consent was obtained from a parent or legal guardian. Participants were assigned, by cohort, to treatment condition: Brief Advice (BA) or Motivational Intervention (MI). Assignment to treatment condition was done in cohorts to avoid potential intervention contamination during hospitalization. Between cohorts, no recruitment occurred until study participants from the previous cohort had been discharged from the hospital. The assignment of cohorts to treatment condition was determined randomly before the initiation of the study. However, due to slower than anticipated participant flow, recruitment was ended before all cohorts were completed, resulting in an imbalance in participants in the two conditions. Twelve cohorts of 16 participants were completed. However, one participant withdrew from the study during a period of non-recruitment between cohorts, resulting in a total sample size of 191. Of these, 116 participants were assigned to motivational intervention and 75 to brief advice.
All patients were assessed at baseline, immediately after hospitalization, and at 1-, 3-, 6-, 9-, and 12-month follow-ups. The 3- and 9-month follow-ups were limited to the administration, by telephone, of a 3-month timeline follow-back interview regarding smoking. All assessments were completed by bachelors level research assistants who were unaware of participants’ treatment condition. We completed follow-ups with 94%, 95%, 92%, 93% and 91% of participants at the 1-, 3-, 6-, 9-, and 12-month follow-ups respectively. Rates of missing data were not significantly different across MI and BA conditions.
2.2. Participants
A total of 1099 patients were screened for possible recruitment into a randomized clinical trial for smoking cessation from February 1998 to April 2001. Of these 1099 patients, 533 were either non-smokers or did not smoke weekly and therefore did not meet the study’s smoking inclusion criterion. Additional patients were excluded because of recent violent behavior (n =46), current psychotic disorders (n = 58), current participation in another study (n = 28), uncertain guardianship status (n = 21), language incompatibility (n = 16), having a sibling in the study (n = 11), significant cognitive impairment (n = 7), residing too far away to complete follow up assessments (n = 6), or for hearing impairment (n = 4). Of the 369 patients who appeared to meet all of the eligibility criteria (pending confirmation with interview for psychiatric diagnosis), 147 refused study participation. The parents of 11 patients refused to allow their children to participate, and an additional 20 patients withdrew from the study before completing the baseline assessment battery.
The final study sample (n = 191) consisted of 62.3% female and 37.7% male participants. The mean age of participants was 15.4 years, of whom 94.8% were white, 1.6% Hispanic/Latino, 0% African American, and 3.6% of other ethnicities. Participants on average reported that they first smoked a cigarette before age 11 [Mean (SD) 10.85 (2.20)]. During the three months before hospitalization, participants smoked on an average of 91.19 (18.63)% of the days and smoked an average of 14.48 (9.37) cigarettes on smoking days. About 64% (63.9%) of the sample (n = 122) were daily smokers. Participants had a mean (SD) score of 4.9 (1.82) on the Fagerström tolerance questionnaire, modified for use with adolescents, and 68.6% (n = 131) met DSM-IV criteria for nicotine dependence. The mean (SD) length of participants’ inpatient hospital stay was 9.11 (7.11) days. Demographic, diagnostic, smoking, and substance use characteristics are presented by treatment group in Table 1.
Table 1.
Baseline demographic, diagnostic, smoking, and substance use characteristics for teens randomized to Motivational Interviewing and Brief Advice treatment condition.
| Motivational Interviewing | Brief Advice | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Statistic, p value | |
| Age | 15.36 | 1.27 | 15.41 | 1.29 | t=0.26, p=0.79 |
| Female | 48.3% | 48.9% | X2=0.09, p=0.76 | ||
| Affective | 45.5% | 42.3% | X2=0.19, p=0.66 | ||
| Anxiety | 54.5% | 56.4% | X2=0.07, p=0.79 | ||
| Substance | 70.5% | 73.1% | X2=0.14, p=0.70 | ||
| Disruptive | 77.7% | 80.8% | X2=0.26, p=0.61 | ||
| Cigarettes per day | 13.55 | 10.12 | 14.43 | 8.88 | t=0.64, p=0.52 |
| Fagerstrom | 4.92 | 1.82 | 4.87 | 1.85 | t=−0.18, p=0.86 |
| Percentage of Days With Substance use | 26.18 | 30.91 | 28.18 | 31.27 | t=0.44, p=0.66 |
2.3. Treatment Conditions
Motivational Interviewing Condition (MI)
The MI treatment consisted of two 45-minute individual sessions that occurred while the patient was hospitalized, in addition to comprehensive self-help materials, and up to 6 brief telephone sessions for the patient during the 6 months following discharge from the hospital. The MI intervention also involved a parent intervention component, which consisted of up to 4 brief telephone counseling sessions over the same time period.
Brief Advice (BA)
Consistent with AHCPR guidelines (Fiore et al., 1996), participants in the BA condition received 5–10 minutes of advice to quit smoking, delivered by one of the study therapists and received limited self-help materials. The therapist firmly and clearly advised the patient to quit smoking, discussed some of the health effects of smoking, and provided information to assist in a quit attempt.
Interventions were delivered by doctoral level clinical psychologists and post-doctoral psychology fellows, according to written therapist manuals under the supervision of the senior author. Therapists were crossed with treatment conditions, such that they provided intervention in both conditions.
2.4. Measures
Timeline Followback (TLFB)
TLFB procedures (Sobell & Sobell, 1996) were used to assess number of cigarettes smoked, number of standard alcoholic drinks consumed, and classes of illicit substances used for each of the 90 days preceding hospitalization and at each follow-up going back to the point of last study interview. The TLFB has strong reliability and validity in adult substance users (Sobell & Sobell, 1996), adult smokers (Brown et al., 1998), and adolescent smokers (Lewis-Esquerre et al., 2005). The TLFB at baseline covered the 3 months prior to hospitalization; TLFB at follow-ups assessed substance use since the previous assessment. Monthly averages for substance use were computed only using days when participants were not in an environment that restricted them from smoking or using substances.
Columbia-Diagnostic Interview Schedule for Children (C-DISC)
The C-DISC (Costello, Edelbrock, Duncan, Kalas, & Klaric, 1984) was used to determine the diagnostic status of study participants. The C-DISC is a reliable and valid structured interview (Costello et al., 1984; Weinstein, Noam, Grimes, Stone, & Schwab-Stone, 1990) that assesses DSM-IV (Association, 1994) diagnoses of psychopathology for children and adolescents. Using results from the C-DISC, we collapsed diagnoses into four groups: mood disorders (n = 84), anxiety disorders (n = 105), disruptive behavioral disorders including attention deficit hyperactivity disorder (n = 150), and substance related disorders (n = 136).
Problem Involvement with Chemicals (PIC)
The PIC is a 29-item measure included as part of the Personal Experience Screening Questionnaire (Winters, 1992). Items are rated on a 4-point Likert scale and summed for a total score. The PIC has demonstrated reliability, test-retest stability, and good predictive validity (Winters, 1992). In the current sample, the PIC was highly internally consistent (alpha=.93) with a mean of 64.75 (SD = 24.43).
2.5. Statistical Analyses
We first examined treatment group differences in the frequency of substance use during 12 months after discharge from Butler Hospital. We then conducted generalized linear mixed modeling (GLMM) to test group differences in the frequency of post-hospital substance use. In these analyses, we examined demographic variables (age and gender), diagnostic categories, and substance use problems as potential covariates. The addition of relevant covariates that have an association with substance use outcomes would increase statistical power even if they were not significantly related to treatment condition.
3. Results
Participants did not differ significantly by treatment condition on age, gender, substance use problems, percentage of days using substances, or hospital length of stay (p’s > .10). Rates of diagnostic categories also did not differ across MI and BA treatment conditions, p’s > .60.
3.1. Substance Use Outcomes
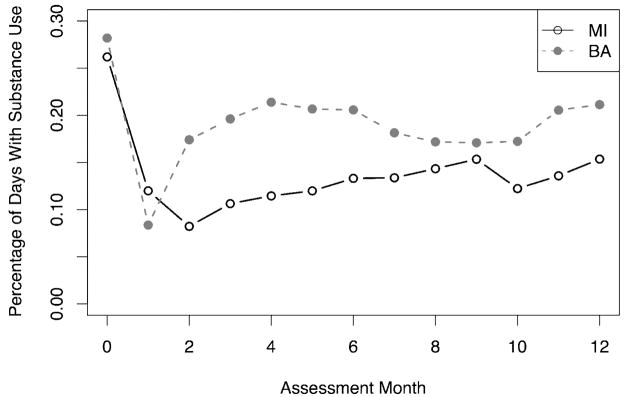
Figure 1 demonstrates the significant reduction in substance use from the baseline assessment (assessment 0) to the period following hospital discharge in both MI and BA conditions. The frequency of days with substance use in the MI condition during follow-up increased from a low of 8.2% (SD = 18.5) of possible substance use days in month 2 to a high of 15.4% (SD = 30.0) in month 12. In BA, substance use days increased rapidly from a low of 8.4% (SD = 20.8) in month 1 to a high of 21.4% (SD = 35.2) in month 4 before stabilizing between 17 and 21% in months 5 to 12. (See Figure 1). For data analysis, an arcsine transformation was used to correct skewness with these data.
Figure 1.
Frequency of substance use days for teens in Motivational Interviewing (MI) and Brief Advice (BA) treatment conditions at baseline (assessment 0) and at each month following psychiatric hospitalization.
Generalized linear mixed modeling (Pinheiro & Bates, 2000) was used to examine group difference in rate of substance use over the 12 months of follow-up. We included randomized participants who provided valid timeline data for follow-up months (n = 186). Differences in the rates of substance use over time are apparent in Figure 1. In fitting models, we first evaluated the significance of individual differences in rates of substance use over time using a likelihood ratio test (LRT) of nested models fit with maximum likelihood methods with and without a random effect for time. The LRT suggested including (X2 =246.7, df=1, p < 0.001) a random effect to allow individuals to vary in their levels of substance use over time. In these models, we examined the set of potential covariates including age, gender, diagnostic comorbidity, and level of substance use problems. Initial models did not support a relationship between the presence of an affective disorder (p > 0.10) and substance use outcomes. Further, when considered together with the continuous measure of substance use problems, substance use diagnosis was not related to substance use outcomes (B = 0.06, SE = 0.6, p > 0.29) and was not considered further. The final set of model terms included the frequency of substance use at baseline, age, gender, anxiety and disruptive behavioral disorder diagnoses, and substance use problems as covariates along with the linear effect of time and the main effect of treatment condition. Examination of Figure 1 suggested that in the BA condition, substance use rates rapidly increased and then stabilized over the 12-months after hospitalization while rates of substance use only slightly increased in the MI condition. Therefore, we included model terms that reflected both the linear (B =0.02, SE =0.01, p <0.02) and quadratic (B =−0.001, SE =0.001, p <0.05) effects of time. Results indicated that more frequent substance use (B = .10, SE = .03, p < .002) and more substance use problems (B = .07, SE = .03, p < .03) at baseline as well as having a disruptive behavioral disorder (B = 0.15, SE = 0.06, p < .01) were significantly related to more frequent substance use during follow-up. Girls (B =0.09, SE =0.05, p <0.07) and teens with an anxiety disorder (B =−0.10, SE =0.05, p <0.08) both had trend-level associations with substance use outcomes. Averaged across the 12 months of follow-up, there was no overall difference in the frequency of substance use between individuals in MI and BA conditions (B = −.04, SE = .05, p > .25). When added to the model in a final step, the quadratic effect of time did not suggest a significant interaction with condition across the full 12-months of follow (B = .001, SE = .001, p > .30).
Although no overall main effect for MI was supported for the full 12-months of follow-up, in post-hoc analyses, we explored whether the effect of MI in potentially preventing the escalation of substance use that was observed during the initial months after discharge was statistically significant. Follow-up analyses of the first six-months proceeded by adding the standard set of covariates as above along with treatment condition and the linear and quadratic effects of time. Results indicated there was no overall main effect of condition, (B = .07, SE = .07, p > .05). As a next step we entered the 2-way interactions of treatment with time. Significant interactions of condition and the linear (B = 0.07, SE = 0.04, p < .05) and quadratic effect of time (B = 0.02, SE = .006, p < .01) was observed suggesting a significant effect of MI in preventing an increase in substance use during the first six-months following hospitalization.
4. Discussion
The results of this study suggest that receiving an MI intervention, relative to BA, for smoking cessation was associated with better substance use outcomes during the first six months following psychiatric inpatient treatment among adolescents. Specifically, receiving MI for smoking cessation rather than BA served to prevent an increase in substance abuse among adolescents during this early time period following hospital discharge. This finding is consistent with previous studies that have shown that encouraging attempts at smoking cessation does not have a detrimental effect on substance abuse treatment outcomes among youth,
Unexpectedly, the MI smoking cessation intervention, compared to BA, in this study was not related to improved smoking outcomes or deceased smoking levels. Overall, nearly one-half of participants (49%) made quit attempts of at least 24 hours in both conditions (Brown et al., 2003). Our results were similar to other trials demonstrating small and statistically non-significant effects of MI on smoking behavior. However, pooled evaluation of clinical trials among adolescents has provided some evidence that MI for teen smoking may be effective at increasing quit attempts and reducing smoking levels (Colby et al., 1998; Woodruff, Edwards, Conway, & Elliott, 2001). Because smoking and substance use are highly correlated, the expectation would be that any decreases in smoking attributable to MI in this study would be associated with decreases in substance involvement. Therefore, the limited effect of the intervention for smoking outcomes in this sample, coupled with the improvements in substance involvement, is somewhat surprising.
There may exist several explanations for why a MI intervention for smoking would be associated with better outcomes for substance use but not smoking among adolescents. Substance use was quite high in this population and was frequently cited as an initial impediment to successful smoking cessation. Often teens selected to focus on change plans during the MI intervention that included behavior related to sustaining changes in substance use behavior. These initial changes could explain the differential effects of MI and BA as no opportunity to discuss substance use was provided in the BA intervention. We did not anticipate this possibility and were unable to evaluate this possibility in the current study. An ongoing trial is evaluating the effectiveness of a MI intervention focusing on facilitating changes in substance use among psychiatric inpatient adolescents.
The beneficial effects on substance use may also derive from the type of intervention employed (i.e., MI). As described by Baer and Peterson (Baer & Peterson, 2002), motivational interviewing may be particularly well-suited for use with teens. Adolescence is a developmental period characterized by the need to develop autonomy and individuation, as well as the tendency to question and resist authority figures. It is also a time characterized by ambivalence, in terms of risk behaviors, identity and roles. Adolescents are most likely to respond well to a style that respects their autonomy, provides choices and not only acknowledges ambivalence, but actually capitalizes upon it to decrease resistance and develop motivation for change. Therefore, the therapeutic process of motivational techniques in general may be sufficient to result in increased motivation for change, irrespective of target behavior.
Although there have only been a few MI studies with adolescent populations, there is increasing evidence that MI interventions may be effective for substance abusing youth. For example, the efficacy of brief MI was evaluated to reduce alcohol-related consequences among adolescents (N=94) treated in a hospital emergency room (ER) following an alcohol-related event (Monti et al., 1999). At 6-month follow-up, adolescents who received MI showed a 32% reduction in drinking and driving and had half the occurrence of alcohol-related injuries as compared to adolescents receiving standard care. In a pilot study of the Adolescent Cannabis Check-up utilizing a motivational interviewing style, reductions in the quantity and frequency of marijuana were maintained 6 months later (Martin, Copeland, & Swift, 2005). Further, recent reviews of the literature (Grenard, Ames, Pentz, & Sussman, 2006; Tevyaw & Monti, 2004) have each concluded that motivational interviewing may be an effective intervention strategy for reducing alcohol and drug use.
Lastly, the results of this study may not be entirely unique. Bobo and colleagues (Bobo, McIlvain, Lando, Walker, & Leed-Kelly, 1998) conducted a randomized community intervention trial examining the effect of smoking cessation counseling on recovery from alcoholism. Their smoking intervention consisted of four 10–15 minute sessions of individualized counseling based on the readiness to change model. They compared the intervention administered to adults in several residential substance abuse treatment programs to usual care in matched control sites. While they found both moderate and heavy drinking rates were reduced in the intervention group, they did not find a treatment effect for tobacco quit rates. The investigators explained the finding by stating that they may not have been powered to detect an effect of the intervention on smoking and that low-intensity tobacco interventions may not be sufficient to demonstrate high quit rates. While this explanation may be true, several of our above-proposed hypotheses (e.g. perceived harmfulness of smoking relative to alcohol and drug use) may have also contributed to their finding.
Study limitations include the lack of a no treatment control, without which we cannot state with certainty that MI for smoking cessation was preferable to no treatment at all. Also, the same therapists delivered both the MI and BA interventions. Despite the interventions being carefully scripted per written therapist manuals and therapists receiving weekly supervision, we cannot rule out the possibility that therapist bias may have favored the MI over the BA condition. Nonetheless we expect this possibility to be remote as we did not observe significant differences in tobacco use outcomes across the two conditions (Brown et al., 2003) and it is not clear that substance use outcomes would have been impacted. Finally, we cannot assume causality or rule out other possible explanations for study findings. Other therapeutic encounters experienced during hospitalization were aimed at substance use reduction and likely had an impact in the noted reduction in substance use relative to pre-hospitalization, although this presumably would have been comparable across treatment groups.
In conclusion, while we have proposed several explanations for finding an effect of a smoking intervention on substance use but not smoking outcomes among adolescents, further research is needed to explore the validity of these hypotheses. More specifically, studies on the relationship between smoking and substance use and on the therapeutic processes of MI are necessary. However, the results of this study do contribute to the growing body of literature that supports the value of smoking cessation efforts among substance abusing populations.
Acknowledgments
This research was supported by Grant CA 77082 from the National Cancer Institute to Richard A. Brown, Ph.D.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amercian Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association.; 1994. [Google Scholar]
- Baer JS, Peterson PL. Motivational interviewing for adolescents and young adults. In: Miller IW, Rollnick S, editors. Motivational Interviewing: Preparing people for change. 2. New York: The Guilford Press; 2002. [Google Scholar]
- Battjes RJ. Smoking as an issue in alcohol and drug abuse treatment. Addict Behav. 1988;13(3):225–230. doi: 10.1016/0306-4603(88)90049-4. [DOI] [PubMed] [Google Scholar]
- Bobo JK. Nicotine dependence and alcoholism epidemiology and treatment. J Psychoactive Drugs. 1989;21(3):323–329. doi: 10.1080/02791072.1989.10472174. [DOI] [PubMed] [Google Scholar]
- Bobo JK, McIlvain HE, Lando HA, Walker RD, Leed-Kelly A. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction. 1998;93(6):877–887. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Arch Gen Psychiatry. 2002;59(11):1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Brook JS, Stimmel MA, Zhang C, Brook DW. The association between earlier marijuana use and subsequent academic achievement and health problems: a longitudinal study. Am J Addict. 2008;17(2):155–160. doi: 10.1080/10550490701860930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychology of Addictive Behaviors. 1998;12(2):101–112. [Google Scholar]
- Brown RA, Ramsey SE, Strong DR, Myers MG, Kahler CW, Lejuez CW, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tob Control. 2003;12(Suppl 4):IV3–10. doi: 10.1136/tc.12.suppl_4.iv3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burling TA, Burling AS, Latini D. A controlled smoking cessation trial for substance-dependent inpatients. J Consult Clin Psychol. 2001;69(2):295–304. doi: 10.1037//0022-006x.69.2.295. [DOI] [PubMed] [Google Scholar]
- Chun J, Guydish J, Chan YF. Smoking among adolescents in substance abuse treatment: a study of programs, policy, and prevalence. J Psychoactive Drugs. 2007;39(4):443–449. doi: 10.1080/02791072.2007.10399883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby SM, Monti PM, Barnett NP, Rohsenow DJ, Weissman K, Spirito A, et al. Brief motivational interviewing in a hospital setting for adolescent smoking: A preliminary study. Journal of Consulting and Clinical Psychology. 1998;66(3):574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- Costello AJ, Edelbrock C, Duncan MK, Kalas R, Klaric S. Development and testing of the NIMH Diagnostic Interview Schedule for Children on a clinical population: Final report. Rockville, MD: Center for Epidemiologic Studies, National Institute for Mental Health; 1984. (No. Contract #RFP-DB-81-0027) [Google Scholar]
- Dakof GA. Understanding gender differences in adolescent drug abuse: issues of comorbidity and family functioning. J Psychoactive Drugs. 2000;32(1):25–32. doi: 10.1080/02791072.2000.10400209. [DOI] [PubMed] [Google Scholar]
- Deas D, Brown ES. Adolescent substance abuse and psychiatric comorbidities. J Clin Psychiatry. 2006;67(7):e02. doi: 10.4088/jcp.0706e02. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, McGuigan KA, Klein DJ. Predictors of late-onset smoking and cessation over 10 years. J Adolesc Health. 2001;29(2):101–108. doi: 10.1016/s1054-139x(00)00199-3. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Smoking Cessation: Clinical Practice Guideline - Number 18. U.S. Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, Centers for Disease Control and Prevention; 1996 . (No. AHCPR Publication No. 96–0692) [Google Scholar]
- Frosch DL, Shoptaw S, Nahom D, Jarvik ME. Associations between tobacco smoking and illicit drug use among methadone-maintained opiate-dependent individuals. Exp Clin Psychopharmacol. 2000;8(1):97–103. doi: 10.1037//1064-1297.8.1.97. [DOI] [PubMed] [Google Scholar]
- Grenard JL, Ames SL, Pentz MA, Sussman S. Motivational interviewing with adolescents and young adults for drug-related problems. Int J Adolesc Med Health. 2006;18(1):53–67. doi: 10.1515/ijamh.2006.18.1.53. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Overall, illicit drug use by American teens continues a gradual decline in 2007. [accessed 10/17/08.];University of Michigan News Service: Ann Arbor, MI [Online] 2007 December 11; Available www.monitoringthefuture.org.
- Kohn CS, Tsoh JY, Weisner CM. Changes in smoking status among substance abusers: baseline characteristics and abstinence from alcohol and drugs at 12-month follow-up. Drug Alcohol Depend. 2003;69(1):61–71. doi: 10.1016/s0376-8716(02)00256-9. [DOI] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, Tevyaw TO, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug Alcohol Depend. 2005;79(1):33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Martin G, Copeland J, Swift W. The Adolescent Cannabis Check-Up: Feasibility of a brief intervention for young cannabis users. Journal of Substance Abuse and Treatment. 2005;29(3):207–213. doi: 10.1016/j.jsat.2005.06.005. [DOI] [PubMed] [Google Scholar]
- Mathers M, Toumbourou JW, Catalano RF, Williams J, Patton GC. Consequences of youth tobacco use: a review of prospective behavioural studies. Addiction. 2006;101(7):948–958. doi: 10.1111/j.1360-0443.2006.01438.x. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Flisher AJ, Fleming MF, Weisner CM. Medical conditions of adolescents in alcohol and drug treatment: comparison with matched controls. J Adolesc Health. 2007;40(2):173–179. doi: 10.1016/j.jadohealth.2006.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67(6):989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Myers MG. Smoking intervention with adolescent substance abusers. Initial recommendations. J Subst Abuse Treat. 1999;16(4):289–298. doi: 10.1016/s0740-5472(98)00038-5. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. Smoking and health in substance-abusing adolescents: a two-year follow-up. Pediatrics. 1994;93(4):561–566. [PubMed] [Google Scholar]
- Myers MG, Brown SA. A controlled study of a cigarette smoking cessation intervention for adolescents in substance abuse treatment. Psychol Addict Behav. 2005;19(2):230–233. doi: 10.1037/0893-164X.19.2.230. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA, Kelly JF. A smoking intervention for substance abusing adolescents: outcomes, predictors of cessation attempts, and post-treatment substance use. Journal of Child and Adolescent Substance Abuse. 2000;9:77–91. [Google Scholar]
- Myers MG, Prochaska JJ. Does smoking intervention influence adolescent substance use disorder treatment outcomes? Substance Abuse. 2008;29(2):81–88. doi: 10.1080/08897070802093361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro JC, Bates DM. Mixed Effects Models in S and S-Plus. New York: Springer-Verlag; 2000. [Google Scholar]
- Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. J Consult Clin Psychol. 2004;72(6):1144–1156. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- Ramsey SE, Strong DR, Stuart GL, Weinstock MC, Williams LA, Tarnoff G, et al. Substance use and diagnostic characteristics that differentiate smoking and nonsmoking adolescents in a psychiatric setting. J Nerv Ment Dis. 2003;191(11):759–762. doi: 10.1097/01.nmd.0000095130.33301.f9. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation.; 1996. [Google Scholar]
- Tevyaw TO, Monti PM. Motivational enhancement and other brief interventions for adolescent substance abuse: foundations, applications and evaluations. Addiction, 99 Suppl. 2004;2:63–75. doi: 10.1111/j.1360-0443.2004.00855.x. [DOI] [PubMed] [Google Scholar]
- Weinstein SR, Noam GG, Grimes K, Stone K, Schwab-Stone M. Convergence of DSM-III diagnoses and self-reported symptoms in child and adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:627–634. doi: 10.1097/00004583-199007000-00018. [DOI] [PubMed] [Google Scholar]
- Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addict Behav. 1992;17(5):479–490. doi: 10.1016/0306-4603(92)90008-j. [DOI] [PubMed] [Google Scholar]
- Woodruff SI, Edwards CC, Conway TL, Elliott SP. Pilot test of an Internet virtual world chat room for rural teen smokers. J Adolesc Health. 2001;29(4):239–243. doi: 10.1016/s1054-139x(01)00262-2. [DOI] [PubMed] [Google Scholar]