Growth is influenced by factors such as gestational age, birth weight, type of feeding (breast or formula), parental stature, environment, nutrition, chronic illness or special health care needs. When evaluating growth that does not follow a normal pattern, each of these factors should be considered.
This guide describes ways to use and interpret the 2000 Centers for Disease Control and Prevention (CDC) Growth Charts (1) to assess physical growth in infants, children and adolescents. During routine screening, physical growth is assessed using a child’s weight, length/stature, and head circumference (infants and toddlers). One-time measurements, taken and plotted accurately on a growth chart, may be used to screen children for nutritional risk. However, they do not provide adequate information to determine a child’s growth pattern. A series of weight and length/stature measurements are more informative.
The 2000 CDC charts (1) offer improvements to the 1977 National Center for Health Statistics charts, including the addition of 3rd and 97th outer percentile curves and body mass index (BMI) for age charts to evaluate weight as a function of height, a feature previously missing on growth charts for older children and adolescents. The collaborative Canadian growth statement recommends usage of the 2000 CDC growth charts containing the 3rd and 97th percentiles to reduce the chance of error in identifying too many children as having potential growth problems when it is not warranted (2).
SELECTING THE APPROPRIATE GROWTH CHARTS
See the CDC Web site to download growth charts (1) <www.cdc.gov/nchs/about/major/nhanes/growthcharts/clinical_charts.htm#Clin%202>.
The clinical growth chart set 2 (with outer limits of the curves at 3rd and 97th percentiles) of the 2000 CDC charts are recommended. They contain both the weight-for-age and stature-for-age curves on one page, have grids scaled in metric units with English units in a secondary scale, and include a table for recording the anthropometric measurements.
Birth to 36 months: Length-for-age, weight-for-age, head circumference-for-age and weight-for-length.
Two to 20 years: Stature-for-age, weight-for-age, BMI-for-age. Plus optional weight-for-stature chart for younger children from about two to five years old.
Preterm infants (< 37 weeks)
Plot measurements using gestation-adjusted age (until 24 to 36 months) on either the regular CDC charts or use charts for very low birth weight and low birth weight infants from the Infant Health and Development Program (3,4).
Breastfed infants
Because growth rates may differ, misinterpretation of the growth rate of an exclusively breastfed infant plotted on charts that include formula fed infants might lead to inappropriate counselling to discontinue breastfeeding (5).
Children with special health needs
The CDC growth charts should be used in this population, with consideration of the potential influence of specific conditions on growth. Disease-specific growth charts (ie, Down syndrome) may be used in conjunction with the CDC charts.
BMI-for-age (Weight [kg]/Height [m2]) is a tool used to screen children two to 20 years old to help identify individuals who are potentially overweight; however, it is not a diagnostic tool. Additional investigations such as skinfold measurements are needed to determine whether a child who has a high BMI-for-age has excess fat. Careful consideration of the differing body compositions of males and females, and the individual child’s stage of pubertal maturity is important (1,2).
INTERPRETING MEASUREMENTS ON THE GROWTH CHARTS
The curves on the growth chart represent selected percentiles of the reference population and can be used to identify the child’s rank relative to other children of the same sex and similar age. For example, when a plotted weight is on the 90th percentile for weight-for-age, it means that only 10 of 100 children (10%) of the same age and sex in the reference population have a higher weight-for-age.
Single plotted measurements can be interpreted using the cut-off values and corresponding nutrition indicators shown in Table 1. In most children, serial height and weight measurements follow consistently along a ‘channel’ on or between the same percentile(s). It is normal for children to change one to two percentile lines during the first two to three years, usually moving toward the 50th percentile line. With the exception of the first two to three years of life and puberty, crossing percentile lines is potentially a sign of growth disturbance. Serial measurements showing unexpected crossing of two or more percentile lines downwards is considered to be reflective of failure to thrive or growth failure.
TABLE 1.
Recommended cut-off values and nutritional indicators for Canadian children
| Anthropometric index | Cut-off values (2) | Nutritional indicator |
|---|---|---|
| Length/stature-for-age | < 3rd percentile | Stunting/shortness: the infant or child may be short because parents are short or he/she may be stunted because of long-term malnutrition, delayed maturation, chronic illness or a genetic disorder. |
| Weight-for-length/stature (available for use up to about 5 years of age), % IBW*, or BMI-for-age (> 2 years old) | < 3rd percentile
< 89% IBW* < 5th percentile |
Underweight or wasting: may be indicative of recent malnutrition, dehydration or a genetic disorder. Traditional measures of underweight (weight for length/stature and % IBW*) continue to be recommended until validity of using BMI-for-age to assess underweight is established. Alternatively, BMI-for-age may be used to screen for underweight (> 2 years old), with awareness of the limited experience of its role in underweight. |
| BMI-for-age | 85th and < 95th percentile | Overweight: further evaluation necessary, looking for comorbidities and possible causes. |
| Weight-for-length (< 2 years old) or BMI-for-age (≤ 2 years old) | ≤ 97th percentile
≤ 95th percentile |
Obesity: should undergo evaluation for possible underlying genetic or endocrine causes. |
| Head circumference-for-age | < 3rd or > 97th percentile | Head circumference reflects brain size and it is used for screening for potential health, nutrition or developmental problems among infants from birth to 36 months old. |
To calculate percent ideal body weight (% IBW), plot length or height on growth chart to identify length/height-for-age percentile. Locate ideal body weight as the weight at the same percentile as the height, for the same age and sex. % IBW=actual weight ideal body weight × 100. BMI Body mass index
ACCURATE MEASUREMENT EQUIPMENT AND TECHNIQUES
Accuracy in equipment and measurement technique are essential because these measurements will be used to make fundamental decisions about the child (see Maternal and Child Health Bureau training modules [6]).
Weighing infants
The infant should be weighed nude on a calibrated beam or electronic scale.
The scale should be accurate and reliable with a maximum weight of 20 kg in 10 g increments and easily “zeroed” and recently calibrated.
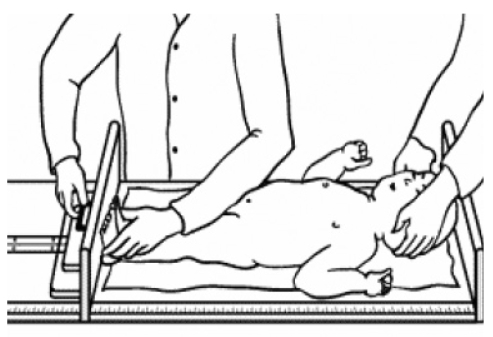
Measuring infant length (Figure 1)
Figure 1).
Measuring infant length. Reproduced with permission from reference 8
Use a calibrated length board with fixed headpiece and movable footpiece which is perpendicular to the surface of the table.
Two trained people are needed to get an accurate measurement.
Measure the infant without shoes and wearing light underclothing or diaper.
The infant should be placed on its back in the centre of the board, lying flat against the surface. Eyes should be looking up. Both legs should be fully extended and toes should be pointing upward with feet flat against the foot piece.
Measure length to the nearest 0.1 cm.
Measuring head circumference (Figure 2)
Figure 2).
Measuring head circumference. Reproduced with permission from reference 8
Position the tape just above the eyebrow, above the ears and around the biggest part on the back of the head.
Use a flexible, nonstretchable tape.
Measure to the nearest 0.1 cm.
Weighing children and adolescents
A child older than 24 to 36 months is weighed standing on a beam-balance or digital scale, provided they can stand on their own. The child is weighed wearing light undergarments or lightweight outer clothing.
Weight is recorded to the nearest 0.1 kg.
Note: Children unable to stand unsupported may need to be held by someone when weighed, with the weight of the person holding the child subtracted from their combined weight. A larger child with special needs may need to be weighed on sit-down or wheelchair scales.
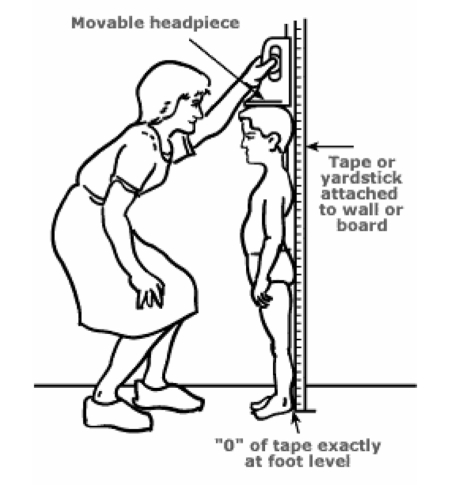
Measuring stature in children and adolescents (Figure 3)
Figure 3).
Measuring stature in children and adolescents. Reproduced with permission from reference 8
Young children from 24 to 36 months may have either length or stature measured. The appropriate chart (length- or stature-for-age) should be used for plotting the results. Children with physical disabilities (unable to stand) may require the use of a recumbent board or the usage of other segment length measurements (2,6,7).
Measure stature for children over 24 months who can stand unassisted.
- A stadiometer for stature measurements requires:
- ○ a wall mounted vertical board with an attached metric rule; and
- ○ a horizontal headpiece that can be brought into contact with the superior part of the head.
The child or adolescent stands against the stadiometer without shoes, with heels together, legs straight, arms at sides and shoulders relaxed.
Ensure that the child is looking straight ahead.
Bring the perpendicular headpiece down to touch the crown of the head.
The measurer’s eyes should be parallel with the headpiece.
Measure to the nearest 0.1 cm.
Note: Alternative measurements like segmental lengths, girths and skinfolds require special skills and equipment. They are performed at some paediatric centres for monitoring growth in children with special health needs (2,7).
Acknowledgments
This fact sheet was developed by Dietitians of Canada and is endorsed by the Canadian Paediatric Society, The College of Family Physicians of Canada and Community Health Nurses Association of Canada. The content of this fact sheet is based on “Assessing and Monitoring Growth in Canadian Infants and Children: Which Growth Charts to Use? A Collaborative Statement from Dietitians of Canada, Canadian Paediatric Society, The College of Family Physicians of Canada and Community Health Nurses Association of Canada, 2003”. To access the complete position paper go to <www.dietitians.ca/news/highlights_positions.html>.
Dietitians of Canada gratefully acknowledges authors Janet Schlenker RDN (DCPNN) and Shefali Raja RDN (DCPNN) for the development of this fact sheet and the DC Paediatric Nutrition Network (DCPNN) for financial support.
Footnotes
NOTE: The PARENT FACT SHEET Is My Child Growing Well should be used in addition to the HEALTH PROFESSIONAL FACT SHEET. Both are available by searching the key words “growth charts” at <www.dietitians.ca/resources/resourcesearch.asp>
Dietitians of Canada and Canadian Paediatric Society. All rights reserved. Permission to reprint in its entirety for noncommercial use only.
REFERENCES AND RESOURCES
- 1.Centers for Disease Control and Prevention, National Center for Health Statistics CDC growth charts: United States. < www.cdc.gov/growthcharts/> (Version current at February 10, 2004).
- 2.A Collaborative Statement from the Dietitians of Canada. Canadian Paediatric Society. The College of Family Physicians of Canada and Community Health Nurses Association of Canada Which Growth Charts to Use for Assessing and Monitoring Growth in Canadian Infants and Children. 2003 doi: 10.3148/65.1.2004.22. < www.dietitians.ca/news/highlights_positions.html> (Version current at February 10, 2004). [DOI] [PubMed]
- 3.The Infant Health and Development Program. Enhancing the outcomes of low-birth-weight, premature infants. A multisite randomized trial. JAMA. 1990;263:3035–42. doi: 10.1001/jama.1990.03440220059030. [DOI] [PubMed] [Google Scholar]
- 4.Sherry B, Mei Z, Grummer-Strawn L, Dietz WH. Evaluation of and recommendations for growth references for very low birth weight (1500 grams) infants in the United States. Pediatrics. 2003;111:750–8. doi: 10.1542/peds.111.4.750. [DOI] [PubMed] [Google Scholar]
- 5.Dewey KG. Nutrition, growth and complementary feeding of the breastfed infant. Pediatr Clin North Am. 2001;48:87–104. doi: 10.1016/s0031-3955(05)70287-x. [DOI] [PubMed] [Google Scholar]
- 6.Maternal and Child Health Bureau Training Modules. < http://depts.washington.edu/growth> (Version current February 10, 2004).
- 7.See SHAPES (Canadian Growth Charts for alternative measurements like segment lengths, girths and skinfolds), 2000. Can J Diet Pract Res. 1999;60:1, 20–26. < www.sunny-hill.bc.ca/sunnyhill/shhcc/publications.asp> (Version current at February 10, 2004). [Google Scholar]
- 8.Nardella M, Campo L, Ogata B, editors. Olympia, Washington: State Department of Health; 2001. Nutrition Interventions for Children with Special Health Care Needs. Developed by Cristine M Trahms, MS,RD, FADA, University of Washington, Seattle, Washington, 2002. [Google Scholar]