Abstract
The introduction of biological agents targeting tumor necrosis factor-alpha (TNF-α) has brought about a paradigm shift in the treatment of rheumatoid arthritis (RA). Although these anti-TNF agents have excellent efficacy against RA, a substantial number of patients still show inadequate responses. In Western countries, such patients are already being treated with new classes of antirheumatic drugs such as abatacept and rituximab. Tocilizumab (TCZ) is a humanized monoclonal antibody developed in Japan against the human interleukin-6 (IL-6) receptor. TCZ does not only alleviate the signs and symptoms of RA but also seems to prevent progressive bone and joint destruction. However, there is a concern that TCZ might increase the risk of adverse events such as infections since IL-6 plays a pivotal role in the immune system. Calculating the relative risks of specific adverse outcomes with TCZ use remains difficult, due to insufficient patient numbers enrolled in clinical trials to date. This review presents tentative guidelines for the use of TCZ for RA patients prepared by the Japan College of Rheumatology and based on results of clinical trials in Japan and Western countries. The guidelines are intended as a guide for postmarketing surveillance and clinical practice, and will be revised periodically based on the surveillance.
Keywords: Rheumatoid arthritis, Tocilizumab, Anti-TNF, IL-6, Antirheumatics
Introduction
The introduction of biological agents has significantly altered the natural course of rheumatoid arthritis (RA) and associated joint destruction. Anti-tumor necrosis factor-alpha (TNF-α) agents, infliximab and etanercept, show excellent efficacy in Japanese RA patients. However, the use of these anti-TNFs has been linked to potentially serious adverse effects, particularly infections and malignancies. The Japan College of Rheumatology (JCR) therefore released specific guidelines developed specifically for the proper use of these agents [1].
Tocilizumab (TCZ) is a humanized anti-human interleukin-6 receptor (IL-6R) monoclonal antibody developed recently in Japan. TCZ binds to the alpha chain of both membrane-bound and soluble IL-6R, thus blocking IL-6/IL-6R signaling [2, 3]. In the recent Japanese clinical trial of TCZ monotherapy, 80.3% of patients on 8 mg/kg TCZ achieved the American College of Rheumatology improvement criteria 20% (ACR20) response [4]. TCZ does not only suppress the signs and symptoms of RA but also inhibits bone and joint destruction in RA patients [5]. In the European phase III clinical trial, 50.0% of patients on 8 mg/kg TCZ achieved ACR20 at 24 weeks [6]. It is reported that TCZ is effective even in RA patients refractory to anti-TNF biologics [6]. TCZ is also effective against multicentric Castleman disease [7] and juvenile inflammatory arthritis (JIA) [8], and as of January 2009, TCZ has been approved for clinical use against RA as well as these two conditions, but only in Japan.
Since TCZ is a drug with a new mode of action, unexpected adverse effects may be encountered when used in a variety of RA patients in daily practice. Although both efficacy and safety profiles of TCZ for RA have been substantiated in clinical trials, the relatively small patient numbers to date preclude accurate detection and risk assessment of adverse events associated with this drug, particularly rare occurrences. Furthermore, patients enrolled in clinical trials are carefully selected based on both inclusion and exclusion criteria and thus differ from those in daily practice in terms of risk analysis.
The Ministry of Health, Labor, and Welfare (MHLW) commissioned Chugai Pharmaceutical Company to undertake a postmarketing surveillance of the initial 3,000 cases for adverse events. Based on this, and data of clinical trials conducted in Japan and Western countries, the JCR formulated official guidelines for the use of TCZ in Japan [9] (Table 1). The guidelines are equivalent to a “clinical guide to use” and subject to change periodically based on the pharmacovigilance activities in Japan. The JCR also organized a committee for the medical treatment of rheumatic disease. The committee designed a proposal for the initial guidelines on the safe use of TCZ, which were then discussed and approved by the JCR board of directors. The guidelines were subject to the standard journal review process.
Table 1.
Guidelines for the use of tocilizumab (TCZ) for treatment of rheumatoid arthritis
| Eligibility and inclusion criteria |
| 1. Patients fulfilling the American College of Rheumatology 1987 Classification criteria for the diagnosis of rheumatoid arthritis (RA) and showing inadequate response to conventional treatment. Inadequate response of RA to previous treatment is defined as the presence of the following three clinical findings: Tender joints ≥6 Swollen joints ≥6 ESR ≥28 mm/h or CRP ≥2.0 mg/dl |
| 2. Patients showing inadequate control despite treatment for at least 3 months with standard doses of conventional biological or nonbiological disease-modifying antirheumatic drugs (DMARDs) [e.g., methotrexate (MTX), bucillamine, leflunomide, tacrolimus, sulfasalazine, biological DMARD infliximab, etanercept, and adalimumab] |
| 3. It is recommended that patients should have the following laboratory test results in order to avoid potential opportunistic infections: WBC ≥4,000/mm3 Peripheral blood lymphocytes ≥1,000/mm3 Serum or plasma (1 to >3)-β-d-glucan: negative |
| Exclusion criteria |
| 1. Active infection Bacterial infection Mycobacterial infection including latent tuberculosis defined by history, purified protein derivative (PPD) skin test, radiography, or interferon-γ releasing assay Chronic active Epstein–Barr virus (CAEBV) infection defined by detection of EBV genome in peripheral blood Active hepatitis B virus (HBV) infection |
| 2. History of serious hypersensitivity reaction against TCZ |
| Dosage of TCZ |
| Administer 8 mg/kg diluted in 100–250 ml saline by drip infusion every 4 weeks. |
| When starting infusion, observe the patient carefully. In the absence of abnormal symptoms, drip infusion should be completed in about 1 h. |
| Cautions |
| There are several issues related to safety of TCZ. When starting or continuing TCZ therapy, it is necessary to notify and be prepared for the following complications, medical interventions, and/or conditions: |
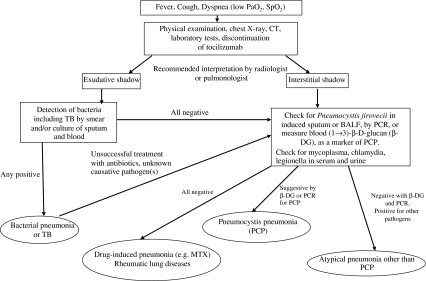
| 1. Infection. Infectious disease, especially respiratory infection, is the most important based on its frequency and severity. When symptoms, such as fever, cough, and dyspnea, occur under TCZ therapy, it is necessary to notify the condition and consult the diagnostic flow chart shown in Fig. 1 Bacterial pneumonia Tuberculosis and nontuberculous mycobacterial infection Pneumocystis pneumonia |
| 2. Bowel perforation and secondary peritonitis. Several cases with bowel perforation followed by peritonitis have been reported. |
| 3. Hyperlipidemia. TCZ therapy is reported to increase serum levels of lipids, cholesterol, and/or triglycerides. |
| 4. Transient neutropenia. Neutropenia is reported in patients on TCZ therapy although the majority of cases are transient and often mild in nature. |
| 5. Use with other DMARDs. TCZ has been approved for use without concomitant DMARDs in Japan. When considering combining TCZ with other DMARDs, it is necessary to evaluate the indications and to monitor the adverse events with utmost care. |
| 6. Serious infusion reactions. Severe infusion reactions may require airway maintenance, oxygen inhalation, subcutaneous epinephrine, and intravenous corticosteroid. |
| 7. Surgery under TCZ therapy. Because TCZ might delay wound healing and mask surgical-site infection, surgery should be postponed until clearance of drug from the bloodstream, i.e., for at least 14 days after the last infusion of the drug. |
| 8. Use during pregnancy and lactation. Avoid use of TCZ in pregnant and lactating women due to concerns regarding safety for embryos and neonates. |
| 9. Use in patients with malignancies. Consider carefully prescription of TCZ for patients with precancerous lesions or recent history of neoplasm because it remains unclear whether TCZ affects carcinogenesis or not. |
Eligibility and inclusion criteria for TCZ
TCZ is recommended for patients who are diagnosed by the American College of Rheumatology 1987 classification criteria for the diagnosis of RA [10], and who show inadequate response despite treatment for at least 3 months with the maximum permissible dose of one of the nonbiologic disease-modifying antirheumatic drugs (DMARDs) [methotrexate (MTX), bucillamine, sulfasalazine, leflunomide, or tacrolimus] rated as “recommendation A level” in the diagnostic manual and evidence-based treatment guidelines [11] developed by the study group of the MHLW, or tacrolimus approved as DMARD only in Japan with some efficacy data [12, 13]. Patients showing inadequate response to the biologic DMARDs approved in Japan (infliximab, etanercept, and adalimumab) are also included. Inadequate response to previous treatment is defined by the presence of at least six tender joints and swollen joints, and either C-reactive protein (CRP) levels of at least 2.0 mg/dl or an erythrocyte sedimentation rate (ESR) of at least 28 mm/h.
To avoid potential opportunistic infections, patients should have a peripheral leukocyte count of 4,000/mm3 or more, a peripheral lymphocyte count of 1,000/mm3 or more, and a negative test for blood β-d-glucan. These criteria are similar to those set for the use of anti-TNF agents in RA patients [1] and are based on the important role played by cellular immunity against opportunistic infections caused by Mycobacterium tuberculosis or fungi such as Pneumocystis jiroveci, and that these infections are likely to occur in patients with low peripheral lymphocyte counts [14]. A test for blood β-d-glucan, a component of fungi, has been included in the diagnosis of fungal infections, especially those with Pneumocystis jiroveci.
Exclusion criteria for TCZ
Active infection
TCZ is contraindicated in patients with ongoing infections, as is the case for other biologics. IL-6 is the major inducer of inflammatory responses against infection [15], thus TCZ could mask signs of infection such as fever, general malaise, and elevation of surrogate markers including CRP and ESR, and consequently make early diagnosis of infections more difficult. However, symptoms such as cough, sputum, and dyspnea are not masked with TCZ. Leukocytosis and a left shift in neutrophil count are also not suppressed by TCZ. Furthermore, radiographic analysis can be used to detect early-stage respiratory infections.
As a precaution against tuberculosis, candidate patients for treatment with TCZ must also undergo a thorough review of family and past history of tuberculosis, chest radiography, and a purified protein derivative (PPD) skin test. Suspected abnormalities on chest radiography should be further investigated by computed tomography of the chest. TCZ is contraindicated in patients with abnormalities on chest radiography such as linear opacities, calcification larger than 5 mm, and pleural thickening suggestive of old tuberculosis, and in individuals with pulmonary or extrapulmonary tuberculosis. However, treatment with TCZ may be considered together with antituberculosis agents only if the potential benefits outweigh the potential risks. In patients with a strongly positive PPD skin test (presence of induration) or radiographic opacities suggestive of old pulmonary tuberculosis, treatment with isoniazid (0.3 g/day or 5 mg/kg for low-body-weight patients) should be initiated at least 3 weeks prior to administration of TCZ and continued for the subsequent 6–9 months. It is advisable that patients with active nontuberculous mycobacterial infection are excluded from TCZ treatment because it is often difficult to control these infections.
It remains unclear whether blocking the IL-6/IL-6R pathway directly induces the proliferation or activation of herpes group viruses such as Epstein–Barr virus (EBV). However, it would be better for patients with active EBV infection, defined by detection of EBV genes in peripheral blood, to avoid treatment with TCZ. One case died from hemophagocytosis associated with reactivation of EBV following a single infusion of TCZ [16].
It remains controversial whether TCZ also affects viral loads of hepatitis B virus (HBV) and hepatitis C virus (HCV). However, patients with active HBV infection should be excluded because hepatitis B infection is often exacerbated by various immunosuppressants [17].
Past history of serious infusion reaction
Although severe or life-threatening infusion reactions following TCZ administration are rare, a few cases with acute reaction have been reported [4–6, 21]. History of serious infusion reaction against TCZ is a contraindication, in line with the manufacturer’s recommendation.
Use of TCZ
The recommended dosage and administration route of TCZ in Japan is 8 mg/kg given once monthly as an intravenous infusion over 1 h. Drug-related infusion reactions were reported in clinical trials, although most were mild [4–6, 21]. Simultaneous administration of MTX is not mandatory, since clinical trials conducted in Japan were performed with monotherapy.
Because TCZ can suppress elevation of CRP and ESR, it is inadequate to evaluate its effectiveness by clinical scores. Rather, it is recommended that any such evaluation should be based on tender joint and swollen joint counts, or on calculated scores that do not rely on CRP or ESR, e.g., the clinical disease activity index (CDAI) [18]. In addition, the efficacy of TCZ should be evaluated after at least 3 months of treatment because stable responses to TCZ were only accomplished after such period in the published clinical trials [4, 5].
Cautions for the safe use of TCZ
Infections
Infections are the most common adverse events during TCZ therapy, although serious outcomes are rare [4–6, 19–22]. In addition, all infections improve by appropriate treatment, and no prolongation of treatment due to infection has been documented. Since pneumonia is a particularly common and serious infection in RA patients [23], the JCR has developed a specific algorithm for the differential diagnosis of pneumonia (Fig. 1).
Fig. 1.
Diagnostic algorithm of pneumonia during tocilizumab therapy
No specific pathogens were detected in patients with pneumonia or other infections related to TCZ treatment [4–6, 19–22]. No increase in tuberculosis was observed with TCZ treatment [4, 5, 20–22], compared with the anti-TNF agents [24]. However, TCZ therapy may significantly alter the onset or clinical course of pneumonia. There are anecdotal reports that patients presenting with minimal clinical symptoms develop severe pneumonia with shock within 1 day of the start of TCZ therapy [25]. Sufficient evidence indicates that TCZ can suppress the elevation of CRP and fever even in infections. CRP and fever are not suitable markers of early stages of infection. Suppression of inflammatory responses might delay the early diagnosis of infections, especially pneumonia, and both patients and physicians should be aware of this effect during TCZ therapy.
Epidemiological studies have identified the risk factors for infection in RA patients. These include advanced age [23, 26], pulmonary comorbidities [23, 26], corticosteroid use [23, 26], and impaired daily activity [21]. Patients with these risk factors should be considered more susceptible to infections during TCZ therapy, and tapering or ceasing corticosteroid use is strongly recommended. Patients should also be vaccinated prior to or even during TCZ treatment against influenza and pneumococcus if over 65 years old. TCZ does not alter the response to vaccination against influenza or pneumococcus [27, 28].
Bowel perforation
Several cases of bowel perforation followed by peritonitis were reported in the clinical trials of TCZ [29]. Although this adverse event is extremely rare, it is more infrequent with other biologics including anti-TNF agents [30, 31]. Postmarketing surveillance should explore whether this adverse event is specific to TCZ. In this regard, serum IL-6 level was elevated specifically prior to intestinal perforation [32, 33], and it is possible that TCZ could mask the early symptoms of diverticulitis and hamper healing by its inhibitory effect on IL-6/IL-6R signaling.
Elevation of serum lipid concentrations
In clinical trials, serum lipid levels are often elevated during TCZ therapy [4–6, 19–22]. Serum total cholesterol increased in 38% of patients on TCZ monotherapy in one Japanese study [5] and in 23% of the patients given a combination of TCZ and nonbiologic DMARDs in a European study [22]. However, total cholesterol levels stabilized in the upper normal range in most cases. Furthermore, the atherogenic index was not altered in these cases due to accompanying increases in high-density lipoprotein [5, 22].
Cardiovascular complications were rarely reported during TCZ clinical trials, although the observation periods were relatively short [5, 22]. Statin therapy is recommended when lipid levels increase above normal range. These phenomena are probably due to suppression of inflammation, which can also be observed under anti-TNF treatment. Nevertheless, elevated serum lipids during TCZ treatment should be monitored during postmarketing surveillance since IL-6 signaling might also directly affect lipid metabolism.
Transient neutropenia
Neutropenia has been reported with TCZ treatment [6, 19–22]. Neutrophil counts below 1,000/mm3 were recorded, although not associated with infection. The transient nature of these changes indicates that margination of neutrophils from the circulation in the bone marrow might be responsible [19].
Combination with other DMARDs
Since the clinical trials of TCZ in Japan were designed as monotherapy treatment [5], this drug has been approved only for use without concomitant DMARDs. Clinical trials in Western countries have shown the efficacy of TCZ treatment when combined with conventional DMARDs, particularly MTX. Elevated levels of hepatic transaminases were detected more frequently in the TCZ groups in these trials [19, 21], although their levels were less than threefold the upper limits of normal in the majority of patients and returned to normal with repeated treatment. No such findings were reported in Japanese trials [4, 19, 22]. Monitoring of serum liver enzymes is recommended during TCZ treatment, especially when the latter is combined with MTX.
Infusion reactions
Similar to other biologic agents, TCZ can induce infusion reactions during or after the treatment day, although most reactions are mild and transient [4–6, 19–22]. Infusion reactions were observed in 11 out of 157 patients in the SAMURAI trial [5]. Sleepiness, headache, and increased blood pressure were observed but they were transient in nature. However, preparation for severe infusion reactions is recommended in case of emergencies; airway maintenance, oxygen inhalation, subcutaneous epinephrine, and intravenous corticosteroids should be available at bedside.
Surgery
The effect of IL-6 on wound healing remains to be clarified [34], although it is possible that wound healing might be delayed under TCZ therapy. Moreover, the signs and symptoms of surgical-site infection might be masked in patients treated with TCZ, as discussed above. CRP levels were completely normalized in patients with stable serum TCZ levels [35]. At present, it is advisable that surgery is postponed in patients on TCZ treatment until reduction of drug level in peripheral blood, i.e., deferment of surgery to at least 14 days after the last infusion of the drug.
Pregnancy and lactation
There are no data available on the safety of TCZ in pregnancy and lactation. IL-6 was reported to reduce recurrent abortion in an animal model [36], however the effect of TCZ on embryonic and fetal development is unknown. Therefore, it is currently not recommended to administer TCZ to pregnant women.
Malignancy
It remains unclear whether blocking of IL-6 signaling affects the progression of malignancy [37]. IL-6 induces cachexia in cancer patients, but might also inhibit proliferation of certain types of cancer cells [38]. Administration of TCZ to patients with present or recent history of malignancy or precancerous lesions should be avoided at present, in line with recommendations for anti-TNF agents.
Summary
TCZ is a novel therapeutic option for RA patients who exhibit inadequate response to nonbiologic or biologic DMARDs. Treatment with this drug prevented structural joint damage in Japanese clinical trials. However, the safety profile of TCZ is not yet defined since the numbers of patients involved in the clinical trials are insufficient to detect infrequent but potentially serious adverse effects. Therefore, the JCR has developed tentative guidelines for the proper use of TCZ, and postmarketing surveillance is underway according to these preliminary guidelines.
Acknowledgments
The authors R.K. and M.H. received research grants for the pharmacovigilance of biologics from Abbott Japan, Eisai Company, Wyeth K.K. Japan, Takeda Pharmaceutical Company, Mitsubishi Tanabe Pharma, and Chugai Pharmaceutical Company. M.H. also received consulting fees from Chugai Pharmaceutical Company. T.A. received a research grant from Takeda Pharmaceutical Company. S.K. received research grants from Eisai Company, Wyeth K.K. Japan, Takeda Pharmaceutical Company, Mitsubishi Tanabe Pharma, and Chugai Pharmaceutical Company. T.S. received consulting fees from Eisai Company, Takeda Pharmaceutical Company, Banyu Pharmaceutical Company, Daiichi-Sankyo Company, and Astellas Pharmaceutical Company. M.Y. received consulting fees from Abbott Japan, Takeda Pharmaceutical Company and Mitsubishi Tanabe Pharma. N.M. received consulting fees from Abbott Japan, Eisai Company, Wyeth K.K. Japan, Takeda Pharmaceutical Company, Mitsubishi Tanabe Pharma, and Chugai Pharmaceutical Company. The other authors have no competing interests.
References
- 1.Koike R, Takeuchi T, Eguchi K, Miyasaka N. Update on the Japanese guidelines for the use of infliximab and etanercept in rheumatoid arthritis. Mod Rheumatol. 2007;17:451–8. [DOI] [PubMed]
- 2.Choy EHS, Isenberg DA, Garrood T, Farrow S, Ioannou Y, Bird H, et al. Therapeutic benefit of blocking interleukin-6 activity with an anti-interleukin-6 receptor monoclonal antibody in rheumatoid arthritis. Arthritis Rheum. 2002;46:3143–50. [DOI] [PubMed]
- 3.Nishimoto N, Yoshizaki K, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, et al. Treatment of rheumatoid arthritis with humanized anti-interleukin-6 receptor antibody. A multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2004;50:1761–9. [DOI] [PubMed]
- 4.Nishimoto N, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, Azuma J, et al. Study of active controlled tocilizumab monotherapy for rheumatoid arthritis patients with an inadequate response to methotrexate (SATORI): significant reduction in disease activity and serum vascular endothelial growth factor by IL-6 receptor inhibition therapy. Mod Rheumatol. 2009;19:12–9. [DOI] [PMC free article] [PubMed]
- 5.Nishimoto N, Hashimoto J, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, et al. Study of active controlled monotherapy used for rheumatoid arthritis, an IL-6 inhibitor (SAMURAI): evidence of clinical and radiographic benefit from an x ray reader-blinded randomized controlled trial of tocilizumab. Ann Rheum Dis. 2007;66:1162–7. [DOI] [PMC free article] [PubMed]
- 6.Emery P, Keystone E, Tony HP, Cantagrel A, van Vollenhoven R, Sanchez A, et al. IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to anti-tumour necrosis factor biologicals: results from a 24-week multicentre randomized placebo-controlled trial. Ann Rheum Dis. 2008;67:1516–23. [DOI] [PMC free article] [PubMed]
- 7.Nishimoto N, Kanakura Y, Aozasa K, Johkoh T, Nakamura M, Nakano S, et al. Humanised anti-interleukin-6 receptor antibody treatment of multicentric Castleman disease. Blood. 2005;106:2627–32. [DOI] [PubMed]
- 8.Yokota S, Imagawa T, Mori M, Miyamae T, Aihara Y, Takei S, et al. Efficacy and safety of tocilizumab in patients with systemic-onset juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled, withdrawal phase III trial. Lancet. 2008;371:998–1006. [DOI] [PubMed]
- 9.Guideline for the use of tocilizumab in rheumatoid arthritis, Japan College of Rheumatology home page (in Japanese). http://www.ryumachi-jp.com/info/080724_TCZ.html.
- 10.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. [DOI] [PubMed]
- 11.Study Group of the Ministry of Health, Labour and Welfare. Diagnostic and therapeutic manual of rheumatoid arthritis. Diagnostic manual and evidence-based treatment guidelines (in Japanese). Tokyo: Japan Rheumatism Foundation; 2004.
- 12.Kawai S, Yamamoto K. Safety of tacrolimus, an immunosuppressive agent, in the treatment of rheumatoid arthritis in elderly patients. Rheumatology. 2006;45:441–4. [DOI] [PubMed]
- 13.Kawai S, Tanaka K, Ohno I, Utsunomiya K, Seino Y. Safety of long-term tacrolimus therapy for rheumatoid arthritis: an open-label, uncontrolled study in non-elderly patients. Mod Rheumatol. 2008;18:345–53. [DOI] [PubMed]
- 14.Ogawa J, Harigai M, Nagasaka K, Nakamura T, Miyasaka N. Prediction of and prophylaxis against Pneumocystis pneumonia in patients with connective tissue diseases undergoing medium- or high-dose corticosteroid therapy. Mod Rheumatol. 2005;15:91–6. [DOI] [PubMed]
- 15.Kishimoto T. Interleukin-6: discovery of apleiotropic cytokine. Arthritis Res Ther. 2006;8(Suppl 2):S2. [DOI] [PMC free article] [PubMed]
- 16.Ogawa J, Harigai M, Akashi T, Nagasaka K, Suzuki F, Tominaga S, et al. Exacerbation of chronic active Epstein–Barr virus infection in a patient with rheumatoid arthritis receiving humanized anti-interleukin-6 receptor monoclonal antibody. Ann Rheum Dis. 2006;65:1667–9. [DOI] [PMC free article] [PubMed]
- 17.Calabrese LH, Zein NN, Vassilopoulos D. Hepatitis B virus (HBV) reactivation with immunosuppressive therapy in rheumatic diseases: assessment and preventive strategies. Ann Rheum Dis. 2006;65:983–9. [DOI] [PMC free article] [PubMed]
- 18.Aletaha D, Nell VPK, Stamm T, Uffmann M, Pflunbeil S, Machold K, et al. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7:R796–806. [DOI] [PMC free article] [PubMed]
- 19.Maini RN, Taylor PC, Szechinski J, Pavelka K, Broll J, Balint G, et al. Double-blind randomized controlled clinical trial of the interleukin-6 receptor antagonist, tocilizumab, in European patients with rheumatoid arthritis who had an incomplete response to methotrexate. Arthritis Rheum. 2006;54:2817–29. [DOI] [PubMed]
- 20.Smolen JS, Beaulieu A, Rubbert-Roth A, Romos-Remus C, Rovensky J, Alecock E, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomized trial. Lancet. 2008;371:987–97. [DOI] [PubMed]
- 21.Genovese MC, Mckay JD, Nasonov EL, Mysler EF, da Silva NA, Alecock E, et al. Interleukin-6 receptor inhibition with tocilizumab reduces disease activity in rheumatoid arthritis with inadequate response to disease-modifying antirheumatic drugs. The tocilizumab in combination with traditional disease-modifying antirheumatic drug therapy study. Arthritis Rheum. 2008;58:2968–80. [DOI] [PubMed]
- 22.Nishimoto N, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, Azuma J. Long-term safety and efficacy of tocilizumab, an anti-interleukin-6 receptor monoclonal antibody, in monotherapy, in patients with rheumatoid arthritis (the STREAM study): evidence of safety and efficacy in a 5-year extension study. Ann Rheum Dis. 2008; (Epub ahead of print). [DOI] [PMC free article] [PubMed]
- 23.Wolfe F, Caplan L, Michaud K. Treatment for rheumatoid arthritis and the risk of hospitalization for pneumonia. Associations with prednisone, disease-modifying antirheumatic drugs, and anti-tumor necrosis factor therapy. Arthritis Rheum. 2006;54:628–34. [DOI] [PubMed]
- 24.Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD, et al. Tuberculosis associated with infliximab, a tumor necrosis factor a-neutralizing agent. N Engl J Med. 2001;345:1098–104. [DOI] [PubMed]
- 25.Fujiwara H, Nishimoto N, Hamano Y, Asanuma N, Miki S, Kasayama S, et al. Masked early symptoms of pneumonia in patients with rheumatoid arthritis during tocilizumab treatment: a report of two cases. Mod Rheumatol. 2009;19:64–8. [DOI] [PubMed]
- 26.Doran MF, Crowson CS, Pond GR, O’Fallon WM, Gabriel SE. Predictors of infection in rheumatoid arthritis. Arthritis Rheum. 2002;46:2294–300. [DOI] [PubMed]
- 27.Tsuru T, Terao K, Suzaki M, Nakashima H, Amamoto T, Akiyama A, et al. Immune response to influenza vaccine in patients with rheumatoid arthritis under IL-6 signal blockade therapy with tocilizumab. Ann Rheum Dis. 2007;66(Suppl II):439.
- 28.Tsuru T, Terao K, Suzaki M, Nakashima H, Amamoto T, Akiyama A, et al. Immune response to Pneumococcal vaccine in patients with rheumatoid arthritis under IL-6 receptor inhibition with tocilizumab. Arthritis Rheum. 2007;56:S1026.
- 29.Chugai Pharmaceuticals Ltd. Safety Report of Actemra. November 2008 (in Japanese).
- 30.Takeuchi T, Tatsuki Y, Nogami Y, Ishiguro N, Tanaka Y, Yamanaka H, et al. Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis. 2007;67:189–94. [DOI] [PubMed]
- 31.Koike T, Harigai M, Inokuma S, Inoue K, Ishiguro N, Ryu J, et al. Safety outcomes from a large Japanese post-marketing surveillance for etanercept. Arthritis Rheum. 2007;56:S182. [DOI]
- 32.Yoon DY, Chu J, Chandler C, Hiyama S, Thompson JE, Hines OJ. Human cytokine levels in nonperforated versus perforated appendicitis: molecular serum markers for extent of disease? Am Surg. 2002;68:1033–7. [PubMed]
- 33.Endo S, Inada K, Inoue Y, Otsu T, Kasai T, Kuwata Y, et al. Endotoxin and cytokines in patients with gastrointestinal tract perforation. Mediators Inflamm. 1992;1:45–8. [DOI] [PMC free article] [PubMed]
- 34.Biffl WL, Moore EE, Moore FA, Peterson VM. Interleukin-6 in the injured patient. Marker of injury or mediator of inflammation? Ann Surg. 1996;224:647–64. [DOI] [PMC free article] [PubMed]
- 35.Nishimoto N, Terao K, Mima T, Nakahara H, Takagi N, Kakehi T. Mechanisms and pathologic significances in increase in serum interleukin-6 (IL-6) and soluble IL-6 receptor after administration of an anti-IL-6 receptor antibody, tocilizumab, in patients with rheumatoid arthritis and Catsleman disease. Blood. 2008;112:3959–64. [DOI] [PubMed]
- 36.Dubinsky V, Junovich G, Gentile T, Gutierrez G. IL-6 as a regulatory factor of the humoral response during pregnancy. Am J Reprod Immunol. 2008;60:197–203. [DOI] [PubMed]
- 37.Yamanaka H, Nishimoto N, Inoue E, Hara M, Tomatsu T, Kamatani N. Incidence of malignancies in Japanese rheumatoid arthritis patients treated with tocilizumab in comparison to those in an observational cohort Japanese patients and a Japanese population database. Ann Rheum Dis. 2007;66(Suppl II):122.
- 38.Hong DS, Angelo LS, Kurzrock R. Interleukin-6 and its receptor in cancer. Implications for translational therapeutics. Cancer. 2007;110:1911–28. [DOI] [PubMed]