Abstract
This study examined the association between fathers’ alcoholism and other risk factors such as parental depression, family conflict, infant temperament, and parent–infant attachment. The quality of parent–infant interactions was hypothesized to be a proximal mediator of the associations among alcoholism and other risk factors and attachment. The participants were 223 families (104 nonalcoholic families and 119 alcoholic families) with 12-month-old infants recruited through birth records. Infants in families with two parents with alcohol problem had significantly higher rates of insecure attachment with both parents. Structural Equations Modeling indicated that the fathers’ alcohol problem was associated with lower paternal sensitivity (higher negative affect, lower positive engagement, and lower sensitive responding) during father–infant play interactions, and this in turn was associated with higher risk for infant attachment insecurity with fathers. The association between the fathers’ alcohol problem and infant attachment security with the mother was mediated by maternal depression, and maternal alcohol problems and family conflict were associated with maternal sensitivity during play interactions. These results indicate that the fathers’ alcoholism is associated with higher family risk including the quality of the parent–infant relationship; infant attachment develops in a family context; and this context has a significant association with attachment security.
Numerous studies on children of alcoholic fathers have suggested that they are at higher risk for negative outcomes, such as behavior problems, conduct disorders, and later delinquency including substance use (Chassin, Rogosch, & Barrera, 1991; Johnson, Leonard, & Jacob, 1989; Steinglass, 1987; West & Prinz, 1987). Although the bulk of this literature has been focused on adolescent and adult children of alcoholics, increasing evidence suggests that indices of risk may be present in the early years (Jansen, Fitzgerald, Ham, & Zucker, 1995; Noll, Zucker, & Greenberg, 1990; Zucker & Fitzgerald, 1991). Indeed, results from ongoing studies of infants of alcoholic fathers have demonstrated that fathers’ alcoholism is associated with the quality of father–infant interactions and fathers’ aggravation with the infant, and this statistical effect is mediated by fathers’ depression (Eiden, Chavez, & Leonard, 1999; Eiden & Leonard, 2000).
Recent studies with preschool children of alcoholics have demonstrated that there are variations in the nature of risk structure within families and that parents’ negative affect expression is a mediator of risk for later externalizing problems among children of alcoholics (Wong, Zucker, Puttler, & Fitzgerald, 1999). In addition to direct associations between alcoholism and negative child outcomes, indirect associations via parental psychopathology (e.g., depression and antisocial behavior), as well as a cumulative impact of co-occurring risk factors of alcoholism and other psychopathology, have been demonstrated (Eiden et al., 1999; Loukas, Fitzgerald, Zucker, & von Eye, 2001; Mun, Fitzgerald, von Eye, Puttler, & Zucker, 2001; Wong et al., 1999). Parental alcoholism is also associated with family conflict and violence (Leonard & Quigley, 1999; Murphy & O’Farrell, 1996; Quigley & Leonard, 2000; Spaccarelli, Sandler, & Roosa, 1994), which in turn has a negative impact on parenting and child outcomes (Cummings & Davies, 1994; Fergusson & Horwood, 1998). Thus, fathers’ alcoholism serves as a marker variable for increased family risk and negative parenting behavior. These aspects of family functioning are known to be significant predictors of the quality of infant attachment. The purpose of this study was to examine the association between fathers’ alcoholism and associated risk factors with infant attachment to mother and father.
The development of a secure attachment relationship with a caring adult is one crucial aspect of social–emotional development during infancy. Indeed, research conducted with mother–infant dyads suggests that secure infants tend to resolve subsequent developmental issues more adaptively compared to insecurely attached infants. In contrast, infants who are insecurely attached are more likely to have difficulties negotiating salient developmental issues in later years, including development of independence and ego resilience, social competence, and emotional health (e.g., Easterbrooks, Biesecker, & Lyons–Ruth, 2000; Shaw, Owens, Vondra, & Keenan, 1996; Sroufe, Carlson, & Schulman, 1993; Urban, Carlson, Egeland, & Sroufe, 1991). Thus, insecure attachment may be viewed as an early indicator of risk for later maladaptation. Attachment theory argues that infants form attachment relationships on the basis of repeated interactions with caregivers. Although the exact nature of parent–infant interactions predictive of attachment security has been under debate in recent years (see Belsky, 1997; Cowan, 1997; De Wolff & van Ijzendoorn, 1997; Thompson, 1997; van Ijzendoorn & De Wolff, 1997), the theoretical link between parent–infant interactions and attachment security has been well validated (De Wolff & van Ijzendoorn, 1997; van Ijzendoorn & De Wolff, 1997). Research has demonstrated that this association is more complex than originally understood and that the strength of this association is context dependent (De Wolff & van Ijzendoorn, 1997; van Ijzendoorn & De Wolff, 1997).
Theoretical models of parenting (Belsky, Rovine, & Taylor, 1984; Snyder & Huntley, 1991) have suggested that there are multiple sources of influence on parenting quality and on the development of parent–infant attachment. These sources can be divided into three broad domains: parent domain, child domain, and the sociocontextual factors. Among children of alcoholics, potential influences from the parent domain include alcohol problems, parental depression, and antisocial behavior. Fathers with alcohol problems have higher mean levels of depression (Eiden et al., 1999; Jacob, Krahn, & Leonard, 1991). Partners of alcoholics also report higher levels of depression on average compared to partners of nonalcoholics (Eiden & Leonard, 1996). Numerous studies of families with depressed mothers from clinical as well as community samples have reported associations between maternal depression and less optimal mother–infant interactions in the first year of life (see Campbell & Cohn, 1997; Cohn & Campbell, 1992; Murray & Cooper, 1997). Mothers with higher levels of depression exhibit lower positive affect and higher negative affect and show lower levels of consistency and contingent responsiveness (Cohn & Campbell, 1992; Field et al., 1985; Fleming, Ruble, Flett, & Shaul, 1988). This association between maternal depression and mother–infant interactions is especially pronounced when maternal depression occurs with other risk factors (Campbell & Cohn, 1997; Carter, Garrity–Rokous, Chazan–Cohen, Little, & Briggs–Gowan, 2001; Murray & Cooper, 1997). Although much is known about the association between maternal depression for mother–infant interactions, little research is currently available on the impact of fathers’ psychopathology, including depression on the quality of father–infant interactions. In one of the few studies on father–infant interactions among alcoholic families, Eiden et al. (1999) demonstrated that fathers’ alcoholism was associated with negative father–infant interactions, and this association was mediated by fathers’ depression.
Several studies have demonstrated that maternal depression is directly associated with an increased risk for insecure attachment with mother, especially when depression is chronic or occurring in the context of family dysfunction (Carter et al., 2001; DeMulder & Radke–Yarrow, 1991; Martins & Gaffan, 2000; Radke–Yarrow, Cummings, Kuczynski, & Chapman, 1985; Teti, Gelfand, Messinger, & Isabella, 1995). Few studies have examined the association between fathers’ alcoholism or depression with infant–father attachment. The majority of studies on father–infant attachment conducted to date consist of middle-class, low risk families. These studies indicate that the distribution of attachment classifications in father–infant dyads is similar to that in mother–infant dyads and that fathers’ attachment representation is associated with infant attachment to father (see van Ijzendoorn & De Wolff, 1997).
Although the link between maternal depression and infant outcome has been well established, less is known about the impact of parents’ antisocial behavior on family functioning during infancy. Antisocial behavior is of importance, not only because of the link with alcoholism and potential to influence parenting (see Zucker, Ellis, Bingham, & Fitzgerald, 1996), but also because of possible genetic linkages to infant temperament (see Jansen et al., 1995; Tarter, Alterman, & Edwards, 1985; Windle, 1991). One of the few studies focusing on these aspects of parental functioning among alcoholic families found both maternal and paternal antisocial behaviors to be significant predictors of behavior problems among preschool aged children (Jansen et al., 1995).
The second domain of influence on the quality of interactions and attachment is the child domain. This domain may be especially critical among children of alcoholics given the theory that one pathway to later maladaptation among children of alcoholics is through negative temperament (Blackson, 1994; Chassin, Collins, Ritter, & Shirley, 2001; Colder & Chassin, 1997; Neighbors, Clark, Duncan, Donovan, & Brody, 2000; Wong et al., 1999). Theoretical links have also been proposed between infant temperament and quality of parent–infant interactions. Indeed, studies have demonstrated that aspects of infant temperament have a significant impact on the quality of interactions, and the association between temperament and attachment security is mediated or moderated by maternal sensitivity during interactions (Mangelsdorf, Gunnar, Kestenbaum, & Lang, 1991; Susman–Stillman, Kalkose, Egeland, & Waldman, 1996; van den Bloom & Hoeksma, 1994). Fewer studies have investigated the role of infant temperament in predicting father–infant interactions or attachment.
Finally, the third domain of influence on parent–infant interactions and attachment is the context in which development occurs. Among various contextual factors influencing families, one of critical importance for families with alcoholic fathers is family conflict. Although there is some debate over the role of alcohol in causing family conflict, the literature linking alcoholism to marital conflict clearly demonstrates that alcoholism is associated with increased interparental conflict and violence (Leonard, 1993; Leonard & Quigley, 1999; Murphy & O’Farrell, 1996; Quigley & Leonard, 2000; Spaccarelli et al., 1994; West & Prinz, 1987). Marital conflict and violence have been associated with increased risk for distress and maladjustment among children of all ages (see Cummings & Davies, 1994; Handal, Tschannen, & Searight, 1998; Jouriles, Norwood, McDonald, Vincent, & Mahoney, 1996; McNeal & Amato, 1998). Increased levels of marital conflict have also been associated with negative parenting behavior (Donovan, Leavitt, & Walsh, 1998; Eiden & Leonard, 1996) and may be one pathway explaining the association between marital conflict and child adjustment.
Taken together, models of parenting suggest that parenting and child outcomes are influenced by three domains: parent domain, child domain, and the family context. Among the myriad aspects reflected within each domain, four that are of particular relevance to alcoholic families apart from alcoholism per se are parental depression, antisocial behavior, infant temperament, and family conflict. These sources of influence may have direct associations with the quality of infant–parent attachment or may have indirect associations through their influences on parenting behavior. Thus, any association between paternal alcoholism and infant attachment may be explained by several mediational pathways: through the association between fathers’ alcoholism and parental depression, fathers’ alcoholism and antisocial behavior, fathers’ alcoholism and infant temperament, and fathers’ alcoholism and family conflict and through associations between these variables and parenting behavior.
Recent studies and theoretical discussions on the impact of risk and protective factors on a number of developmental outcomes have noted that multiple risk conditions from different domains of functioning often co-occur (Pungello, Kupersmidt, Burchinal, & Patterson, 1996; Rutter, 1987; Sameroff, Seifer, Baldwin, & Baldwin, 1993; Seifer, 1995; Zeanah, Boris, & Larrieu, 1997). In other words, risk conditions such as parental alcoholism or depression seldom occur in isolation. Given this situation, researchers have argued that the total number of risk factors may be more predictive of child outcomes than exposure to any specific risk condition (Seifer, 1995; Zeanah et al., 1997). Indeed, in a study examining the association between chronic family adversity and infant attachment security, Shaw and Vondra (1993) demonstrated the connection between cumulative adversity and security of mother– infant attachment among 12-month-olds.
The major goal of this study was to examine the association between fathers’ alcoholism and parent–infant attachment. We first tested the direct association between fathers’ alcohol problem and father–infant and mother–infant attachment (direct effects model). Next, we examined whether the addition of other risk factors associated with alcoholism improved the fit of the model. Next, we tested the hypothesis that fathers’ alcohol problem would be associated with father–infant attachment through associations with fathers’ parenting behavior (indirect effects model). Similarly, fathers’ alcohol problem would be associated with mother–infant attachment through associations with mothers’ parenting behavior. Next, we tested a model that included associations between fathers’ alcohol problem and other risk factors (depression, temperament, and family conflict) and paths from these predictors to fathers’ parenting behavior and infant attachment. We included mothers’ alcohol problems in the model testing the associations with infant–mother attachment, although the nature of our design precludes examination of the impact of maternal alcohol problems independent of fathers’ alcohol problems. Finally, we examined the association between cumulative family risk scores and parent–infant attachment.
Method
Participants
The participants were 223 families with 12-month-old infants (107 girls and 116 boys) who were recruited for an ongoing longitudinal study of parenting and infant development. Families were classified as being in one of two major groups: the nonalcoholic group, consisting of parents with no or few current alcohol problems (n = 104), and the father alcoholic group (n = 119). Within the father alcoholic group, 99 mothers were light drinking or abstaining and 20 mothers were heavy drinking or had current alcohol problems. Because of videotaping error, the observational data for one father–infant dyad in the nonalcoholic group could not be coded, and two others had missing attachment data because they did not keep their 12-month appointments. The majority of the mothers in the study were Caucasian (94%), about 5% were African American, and 1% were Hispanic or Native American. Similarly, the majority of fathers were Caucasian (89%), a few were African American (7%), and the rest were Hispanic or Native American (4%). Although parental education ranged from less than high school degree to Master’s Degree, about half the mothers (57%) and fathers (55%) had received some post-high school education or had a college degree. Annual family income ranged from $4,000 to $95,000 (M = $41,824, SD = $19,423). All of the mothers were residing with the father of the infant in the study at the time of recruitment. Most of the parents were married to each other (88%), about 11% were unmarried, and 1% were divorced or separated from a previous partner. Mothers’ age ranged from 19 to 40 years (M = 30.43, SD = 4.58) and fathers’ age ranged from 21 to 58 years (M = 32.94, SD = 6.06). About 61% of the mothers and 91% of the fathers were working outside the home. Mothers’ work hours ranged from 5 to 72 hr/week (M = 16.63, SD = 16.38 hr) and fathers’ work hours ranged from 4 to 84 hr/week (M = 40.71, SD = 16.65 hr). A few of the families were on welfare (Aid to Families with Dependent Children, 6%) and about 4% of the fathers were receiving unemployment compensation. Parity ranged from one to five with the majority of families having one to two children, including the target child (68%). About 18% of the infants in the study were only children. Thus, the majority of the families were middle-income, Caucasian families with one to two children in the household.
Procedure
The names and addresses of these families were obtained from the New York State birth records for Erie County. These birth records were preselected to exclude families with premature (gestational age of 35 weeks or lower), or low birth weight infants (birth weight of less than 2500 g), maternal age of less than 18 and greater than 40 years at the time of the infant’s birth, plural births (e.g., twins), and infants with congenital anomalies, palsies, or drug withdrawal symptoms. Introductory letters were sent to a large number of families (n = 9457) who met the above-mentioned basic eligibility criteria. Each letter included a form that all families were asked to complete and return (average response rate = 25%). Of these, about 2,285 replies (96%) indicated an interest in the study. Only a handful of the replies (n = 97 or 4%) indicated lack of interest. Respondents were compared to the overall population with respect to information collected on the birth records. These analyses indicated a slight tendency for infants of responders to have higher Apgar scores (M = 8.94 vs. 8.97), higher birth weight (M = 3460 vs. 3516 g), and higher number of prenatal visits (M = 10.31 vs. 10.50). Responders were also more likely to be Caucasian (88% of total births vs. 91% of responders), have higher educational levels, and have a female infant. These differences were significant given the very large sample size, even though the size of the differences was minimal.
Parents who indicated an interest in the study were screened by telephone with regard to sociodemographics and further eligibility criteria. Initial inclusion criteria consisted of both parents cohabiting since the infants’ birth, infant being the youngest child in the family, mother not pregnant at recruitment, no mother–infant separations for over a week, parents as the primary caregivers, and no infant major medical problems. These criteria were important to control because each has the potential to markedly alter parent–infant interactions. Additional inclusion criteria were utilized to minimize the possibility that any observed infant behaviors could be the result of prenatal exposure to drugs or heavy alcohol use. These additional criteria were that there could be no maternal drug use during pregnancy or the past year except for mild marijuana use (no more than twice during pregnancy), average daily ethanol consumption was .50 ounces or less (one drink/day), and she did not engage in binge drinking (five or more drinks per occasion) during pregnancy. During the phone screen, mothers were administered the Family History Research Diagnostic Criteria for alcoholism (RDC) with regard to their partners’ drinking (Andreason, Rice, Endicott, Reich, & Coryell, 1986), and fathers were screened with regard to their alcohol use, problems, and treatment.
Families meeting the basic inclusion criteria were provisionally assigned to one of two groups on the basis of parental screens (nonalcoholic, father alcoholic), with final group status assigned on the basis of both the phone screen and questionnaires administered at the first visit. Mothers in the nonalcoholic group scored below 3 on an alcohol screening measure (TWEAK, Chan, Welte, & Russell, 1993), were not heavy drinkers (average daily ethanol consumption <1.00 ounce), did not acknowledge binge drinking, and did not meet DSM-IV criteria for abuse or dependence. Fathers in the nonalcoholic group did not meet RDC criteria for alcoholism according to maternal report, did not acknowledge having a problem with alcohol, had never been in treatment, and had alcohol related problems in fewer than two areas in the past year and three areas in his lifetime (according to responses on a screening interview based on the University of Michigan Composite Diagnostic Index [UM-CIDI]; Anthony, Warner, & Kessler, 1994). The father alcoholic group consisted of two subgroups: one with partners who had low alcohol problems and the other with partners who had high alcohol problems. A family could be classified in the father alcoholic group by meeting any one of the following three criteria: (a) the father met RDC criteria for alcoholism according to maternal report; (b) he acknowledged having a problem with alcohol or having been in treatment for alcoholism, was currently drinking, and had at least one alcohol-related problem in the past year; or (c) he indicated having alcohol-related problems in three or more areas in the past year or met DSM-IV criteria for abuse or dependence in the past year. The subgroup of alcoholic fathers with light drinking partners consisted of women who did not have alcohol related problems; that is, they met nonalcoholic group criteria. The subgroup of alcoholic fathers with heavy-drinking partners consisted of women who acknowledged alcohol-related problems (TWEAK score of three or higher, or met DSM-IV diagnosis for abuse or dependence) or were heavy drinkers (average daily ethanol consumption of 1.00 ounce or higher, and/or binge drinking). All of the women in this group met DSM-IV criteria for abuse or dependence.
It should be noted that women who reported drinking moderate to heavy amounts of alcohol during pregnancy (see criteria above) were excluded from the study in order to control for potential fetal alcohol effects. Because we had a large pool of families potentially eligible for the nonalcoholic group, alcoholic and nonalcoholic families were matched on race/ethnicity, maternal education, child gender, parity, and marital status.
Families were asked to visit the Institute at five different infant ages (12, 18, 24, and 36 months and on entry into kindergarten), with three visits at each age. Extensive observational assessments with both parents were conducted at each age. Coding of observational data from subsequent visits are ongoing as are assessments at 5–6 years of child age. This paper focuses on the 12-month questionnaire and observational assessments that have been completed and coded for the entire sample. At 12 months, mother–infant observations were conducted at the first visit followed by a developmental assessment at the second visit. Father–infant observations were conducted at the third visit. There was a 4–6 week lag between the mother–infant and father–infant visits. At the two parent–infant visits, the Strange Situation paradigm was conducted first, followed by a 5-min free-play, a 10-min clean-up, and an 8-min structured play situation.
Measures
Parental alcohol use
Although parental alcohol abuse and dependence problems were partially assessed from the screening interview, self-report versions with more detailed questions were used to enhance the alcohol data and check for consistent reporting. A self-report instrument based on the UM-CIDI interview (Anthony et al., 1994; Kessler et al., 1994) was used to assess alcohol abuse and dependence. Several questions of the instrument were reworded to inquire as to “how many times” a problem had been experienced, as opposed to whether it happened “very often.” DSM-IV criteria for alcohol abuse and dependence diagnoses for current alcohol problems (in the past year) were used to assign final diagnostic group status. For abuse criteria, recurrent alcohol problems were described as those occurring at least three to five times in the past year or one or two times in three or more problem areas. This instrument was also used to derive continuous measures of the number of alcohol-related abuse and dependence symptoms in the past year. A quantity–frequency measure (QFI) of alcohol use adapted from Cahalan, Cisin, and Crossley (1969) was used to obtain a measure of average daily ethanol intake for both parents. Finally, a measure indicating severity of heavy drinking was computed. This five-item measure assessed the frequency of drinking six or more drinks, getting drunk, blacking out, passing out, and getting sick. Because of different variances, these items were standardized before summing. The internal reliability of this measure was excellent (α = .85).
All of the alcohol measures were highly skewed and were transformed using square root transformations. The resulting alcohol variables for each parent were strongly correlated with each other. Confirmatory factor analyses revealed that fathers’ QFI, last year dependence symptoms, and severity of heavy drinking (SVHD) loaded on the same factor, reflecting fathers’ current alcohol problems. Confirmatory factor analyses on mothers’ QFI, last year dependence symptoms, and SVHD also revealed loadings on the same factor, reflecting mothers’ current alcohol problems (see Table 1). Most fathers in the alcoholic group drank about 2–3 drinks/day or 14–21 drinks/week, binged 2–3 days/month, and had one or two abuse and one or two dependence symptoms in the past year. However, there was considerable range in drinking and alcohol-related problems. The QFI ranged from 0.14 to 6 (less than 1 drink/day to 12 drinks/day), number of dependence symptoms ranged from 0 to 146 in the past year, number of abuse symptoms ranged from 0 to 52, and frequency of binging ranged from once or twice a year to every day. Similarly, the majority of mothers with alcohol problems drank about 1 drink/day (range from less than 1 drink/day to 4 drinks/day or 28 drinks/week), had 3 or 4 abuse symptoms (range of 0–23) and 3 or 4 dependence symptoms (range of 0–18), and binged about once a month (range of less than once/month to twice/week).
Table 1.
Standardized factor loadings for the latent constructs
| Father |
Mother |
|||
|---|---|---|---|---|
| Parameter | Factor Loading | ta | Factor Loading | ta |
| Alcohol Problem | ||||
| Quantity-Frequency (QF1) | 80b | — | .76 | — |
| Dependence Symptoms (LYNDS) | .78 | 13.84 | .68 | 10.36 |
| Severity of Heavy Drinking (SVHD) | .99 | 16.23 | .91 | 11.34 |
| Depression | ||||
| Subscale 1 (DP1) | .81b | — | .86 | — |
| Subscale 2 (DP2) | .86 | 11.52 | .78 | 12.41 |
| Subscale 3 (DP3) | .74 | 12.63 | .82 | 12.99 |
| Family Violence | ||||
| Moderate Aggression (MCTS) | .74b | — | .91 | 11.33 |
| Severe Aggression (SCTS) | — | — | .76 | 12.08 |
| Infant Temperament | ||||
| Difficult Scale 1 (ICQDF1) | .67 | 9.27 | .75b | — |
| Difficult Scale 2 (ICQDF2) | .69 | 9.49 | .80 | 10.59 |
| Sensitivity | ||||
| Positive Engagement (PAFF) | .76b | — | .78b | — |
| Negative Affect (NAFF) | .69 | 10.90 | .72 | 10.86 |
| Sensitivity (SENS) | .96 | 12.36 | .90 | 11.66 |
All significant at p < .001.
Unstandardized parameter fixed to 1.00 during estimation.
Parents’ depression
Parents’ depression was assessed with the Center for Epidemiological Studies Depression Inventory (CESD; Radloff, 1977), a scale designed to measure depressive symptoms in community populations. The CESD is a widely used, self-report, 4-point Likert type measure. Parents were asked to report how often they experienced 20 depressive symptoms (e.g., poor appetite, feeling sad, inability to concentrate) during the past week with responses including rarely or none, some or a little of the time (1–2 days), occasionally or a moderate amount of time (3–4 days), or most or all of the time (5–7 days). The scale has high internal consistency (Radloff, 1977) and strong test–retest reliability (Boyd, Weissman, Thompson, & Myers, 1982; Ensel, 1982).
The CESD items were divided into three subscales by taking the composite of every third item, in order to create three measured indicators of latent variables for paternal and maternal depression. Confirmatory factor analyses revealed that these three measured indicators had high loadings on a factor indicating depression, one for each parent (see Table 1).
Antisocial behavior
A modified version of the Antisocial Behavior Checklist (ASB; Zucker & Noll, 1980) was used in this study. Because of concerns about causing family conflict as a result of parents reading each others responses, items related to sexual antisociality and those with low population base rates (Zucker, personal communication, 1995) were dropped. This resulted in a 28-item measure of antisocial behavior. Parents were asked to rate their frequency of participation in a variety of aggressive and antisocial activities along a 4-point scale ranging from 1 (never) to 4 (often). The measure has been found to discriminate among groups with major histories of antisocial behavior (e.g., prison inmates, individuals with minor offenses in district court, and university students; Zucker & Noll, 1980) and between alcoholic and nonalcoholic adult males (Fitzgerald, Jones, Maguin, Zucker, & Noll, 1991). Parents’ scores on this measure were also associated with maternal reports of child behavior problems among preschool children of alcoholics (Jansen et al., 1995). The original measure has adequate test–retest reliability (.91 over 4 weeks) and internal consistency (coefficient α = .93). The antisocial behavior scores for both fathers and mothers were skewed and were transformed using square root transformations. The internal consistency of the 28-item measure in the current sample was quite high for both parents (α = .90 for fathers and .82 for mothers).
Family conflict
Mother and father reports of physical aggression were obtained from a modified version of the Conflict Tactics Scale (CTS; Straus, 1979). The items focusing on moderate (e.g., push, grab, or shove) to severe (e.g., hit with a fist) physical aggression, but not the very severe items (e.g., burnt or scalded, use of weapons), were used in this study. Parents were asked to report on the frequency of their own and their partner’s aggression toward each other on a seven-item scale. Four composite physical aggression scores, two for each parent, were created by taking the maximum of each parent and the partners’ reports of moderate and severe aggression. The resulting scores were highly skewed and were transformed using square root transformations.
Confirmatory factor analysis revealed that the subscale for severe aggression from father to mother did not load on the same factor reflecting family conflict (factor loading of .38). This variable was highly skewed even after transformation. Frequency of severe paternal aggression did not occur for the majority of families (84%), and when it did occur, the frequency of occurrence was very low. In order to improve this measurement model, a composite score reflecting fathers’ total aggression toward mother was computed and used as one of three measured indicators of family conflict (fathers’ total aggression toward mother, mothers moderate aggression toward father, and mothers’ severe aggression toward father). Confirmatory factor analysis indicated that these three indicator variables all loaded on one factor indicating family conflict.
Infant temperament
Mother and father reports of infant temperament were obtained by the Infant Characteristics Questionnaire (ICQ; Bates, Freeland, & Lounsbury, 1979). The scale yields four factors: Fussy-Difficult, Unadaptable, Dull, and Unpredictable (Bates et al., 1979) as well as a total score. The Fussy-Difficult factor has been found to be the most stable from 13 to 24 months and most highly correlated with other temperament scales. Thus, a latent variable reflecting a fussy/difficult temperament was created using mothers’ and fathers’ ratings on the ICQ. Four indicator variables were created, two for each parent, by summing every other item in that subscale into two separate scales in order to have adequate degrees of freedom to test the measurement model. Confirmatory factor analyses revealed that the four indicator variables for infant fussy/difficult temperament loaded on the latent variable indicating fussy/difficult temperament.
Parent–infant interactions
Parents were asked to interact with their infants as they normally would at home for 5 min in a room filled with toys. The free-play interactions were followed by 8 min of structured play. During structured play, parents were given four sets of problem-solving tasks. They were asked to help their infants complete these tasks one at a time and then move on to the next task. These interactions were coded using a collection of global 5-point rating scales developed by Clark, Musick, Scott, and Klehr (1980), with higher scores indicating more positive affect or behavior. These scales have been found to be applicable for children ranging in age from 2 months to 5 years (Clark et al., 1980). Further details about these scales have been reported in an earlier paper (Eiden, Chavez, & Leonard, 1999).
Two female coders rated the free-play interactions and two other coders rated the structured-play interactions. The coding of maternal and paternal behavior was alternated between the two coders so that the coder who coded one parent did not code the other parent. Both coders were trained on the Clark scales by the first author and were unaware of group membership and all other data. The interrater reliability was fairly high, ranging from r = .89 to r = .95 (Pearson correlations) for each of the six composite scales across the two interaction settings.
Exploratory factor analyses on the free-play variables had yielded three composite scales for parenting behavior (negative affect, positive affect/involvement, sensitivity). Based on these factor analyses, three composite parenting scales had been created for mother–infant and father–infant free-play interactions. The internal consistencies for these composite scales were quite high, ranging from .83 to .94 for mother–infant interaction scales and .77 to .90 for fathers.
Confirmatory factor analyses were conducted on a combination of free-play and structured-play variables in order to examine the fit of two measurement models, one for each parent. The three composite scales (summing similar items from free-play and structured-play variables) for each parent were used as measured indicators of the latent construct reflecting parental sensitivity. Confirmatory factor analyses indicated that the three parenting behavior scales for fathers loaded on one factor reflecting fathers’ sensitivity (high positive involvement, low negative affect, and high sensitive responding). Similarly, the three parenting behavior scales for mothers loaded on one factor reflecting mothers’ sensitivity. The standardized factor loadings from the confirmatory factor analyses testing the measurement models are presented in Table 1.
Parent–infant attachment
The Ainsworth Strange Situation paradigm (Ainsworth & Wittig, 1969), a 21-min videotaped, structured laboratory separation–reunion procedure was used to examine mother–infant attachment. The procedure consists of eight 3-min episodes that occur in a fixed order and are designed to induce increasing levels of stress in the infant so as to activate the attachment system. In each episode, the infant’s behavior is rated along six dimensions using 7-point scales. The ratings are used to classify the infants into three major categories: secure, insecure–avoidant, and insecure–resistant. In addition to these three classifications, the coding scheme has been extended to include an additional pattern that is especially prevalent in high risk infants, the disorganized (D) pattern (Main & Solomon, 1990). The D classification is considered to be an insecure pattern with behaviors representing a collapse of organized behavior in response to stress of separation, resulting from fear or apprehension in the parent’s presence. This may be exhibited in a variety of ways. Two major behavioral themes are contradictory behavior patterns or direct indices of fear or apprehension in the parent’s presence. Because the D classification does not represent an organized strategy for maintaining access to the caregiver, an alternative, best-fitting classification of secure, avoidant, or resistant is assigned as well, although in several cases, coding of this alternative classification is extremely difficult.
The second author and two research assistants who were blind to group status were responsible for coding all the Strange Situations, with consultation on difficult to code tapes provided by the first author. The first author was originally trained in coding Strange Situations by Douglas Teti, with training on D coding provided by Dante Cicchetti and follow-up training by Alan Sroufe and Elizabeth Carlson. The second author was trained by Alan Sroufe and Elizabeth Carlson. Interrater reliability was established on 15% of the tapes. Individual dyads used for reliability were selected randomly and included all four classifications. The mean interrater reliability using Pearson’s r was .76 on the Strange Situation rating scales and .81 for the Disorganization scale score. Interrater agreement on the four attachment classifications was 93%.
In order to facilitate mediational analyses and use of structural equations modeling, a security rating was also assigned to each infant– mother and infant–father dyad, using guidelines provided by Cummings (1990) after the classification had been assigned. Security ratings were based on behavioral indices of felt security observed during the Strange Situation. These are described by Cummings (1990) and included ameliorative behaviors such as reciprocated contact seeking, proximity seeking, or distance interaction and avoidance, resistance, difficulty comforting, depressed affect, conflicted, disconnected, or punitive behaviors. Each dyad was assigned a security rating from 1 to 4, with higher scores indicating higher insecurity. The interrater reliability on security ratings for mother–infant and father–infant dyads were conducted on 15% of the tapes. Interrater reliability for mother–infant dyads was .99 and for father–infant dyads was .98. In order to examine the association between the classifications and the security ratings, an analysis of variance (ANOVA) was conducted for attachment with each parent. For infant attachment with mother, there was a significant difference between the four classifications on continuous security rating, F (3, 219) = 392.46, p < .001 (M = 1.54, 2.29, 2.44, and 3.65 for secure, avoidant, resistant, and disorganized classifications, respectively). Simple contrasts indicated a significant difference between the secure and the three insecure classifications, between disorganized and the two other insecure classifications (avoidant and resistant), and between the avoidant and resistant classifications. For infant attachment with father, there was a significant difference across the four classifications on the continuous security rating, F (3, 217) = 434.24, p < .001 (M = 1.48, 2.42, 2.58, and 3.44 for secure, avoidant, resistant, and disorganized classifications, respectively). Simple contrasts indicated that there was a significant difference between the secure and the three insecure classifications, between disorganized and the two other insecure classifications, and between the avoidant and resistant classifications.
Cumulative risk score
Two cumulative risk scores were calculated, one with alcohol problems and one without. In order to create a cumulative risk score and assign equal weight to each risk factor, composite scores were created for all the risk factors. These included difficult infant temperament, fathers’ depression, mothers’ depression, fathers’ antisocial behavior, mothers’ antisocial behavior, fathers’ education, fathers’ aggression toward mother, mothers’ aggression toward father, fathers’ sensitivity during play, and mothers’ sensitivity during play. Similar to previous studies (Sameroff et al., 1993), scores in the upper or lower quartile (depending upon the scale) were used as the cutoff for risk, with the exception of fathers’ education with clear criteria for risk (less than high school education). For infant temperament, the mean of paternal and maternal scores was computed. Scores above 3.61 on this composite score were assigned to the risk category (21% of the sample). For fathers’ depression, total depression scale scores above 10 were assigned to the risk category (24% of the sample). For mothers’ depression, total depression scale scores above 13 were assigned to the risk category (22% of the sample). For fathers’ antisocial behavior, scores above 43 were assigned to the risk category (25% of the sample). For mothers’ antisocial behavior, scores above 39 were assigned to the risk category (20% of the sample). For fathers’ education, less than high school education was assigned to the risk category (5% of the sample). For parents’ aggression toward each other (composite score computed by taking the sum of moderate and severe aggression transformed using square root transformation), scores above 1.41 were assigned to the risk category (15% of the sample for fathers’ aggression and 20% of the sample for mothers’ aggression). For fathers’ sensitivity during play (composite score was computed by taking the mean of positive engagement, negative affect, and sensitivity), scores below 3.59 were assigned to the risk category (24% of the sample). For mothers’ sensitivity during play, scores below 3.68 were assigned to the risk category (24% of the sample). The total risk score was computed by counting the total number of risk categories, with a possible range of scores between 0 and 10. The range of scores in this study was 0–8 (M = 2.22, SD = 1.76). A second risk score was computed by adding parents’ alcohol problems to the original risk score. Thus, composite scores for maternal and paternal alcohol problems were created by summing the transformed scores for total number of dependence symptoms, QFI, and severity of heavy drinking. For fathers’ alcohol problems, scores above 4.91 were assigned to the risk category (24% of the sample). For mothers’ alcohol problems, scores above 3.05 were assigned to the risk category (23% of the sample). A second total risk score including alcohol problems was created with a possible range from 0 to 12. The range of scores in this study was 0–10 (M = 3.22, SD = 2.07).
Plan of analyses
Structural Equations Modeling (SEM) was used to examine the major hypotheses. The first step in SEM analyses was to fit the measurement model for each latent variable. The confirmatory factor analyses used to test the measurement models are described above under each measure. The second step was to test the structural model. The latent variables for prediction of infant attachment security with father included fathers’ alcohol problems, fathers’ depression, fathers’ antisocial behavior, family conflict, and infant fussy/difficult temperament. The latent variables for prediction of infant attachment security with mother included fathers’ alcohol problems, mothers’ alcohol problems, mothers’ depression, family conflict, and infant fussy/difficult temperament. Infant attachment security rating was treated as a single indicator of its construct, and its error variance was computed according to guidelines provided by Bollen (1989). The 28-item antisocial behavior measure was also treated as a single indicator of its construct, and its error variance was fixed to equal the product of its variance and the quantity 1 minus its estimated reliability (Bollen, 1989). No adjustment for random measurement error was made for fathers’ education, the measurement error was set to zero.
To test if there was a direct association between alcohol or other risk factors and attachment, a direct effects model was evaluated in three steps. In step 1 a baseline model was estimated in which all the paths from alcohol and other risk factors to attachment were constrained to zero. This baseline model included noncausal relationships among risk factors that were significant. In step 2, an initial direct effects model was compared with the baseline model. In this initial direct effects model, the path from alcohol to attachment was freely estimated, but paths from all other risk factors to attachment was constrained to zero. In the third step, a direct effects model including paths from all risk factors and alcohol to attachment was estimated and compared with the baseline model.
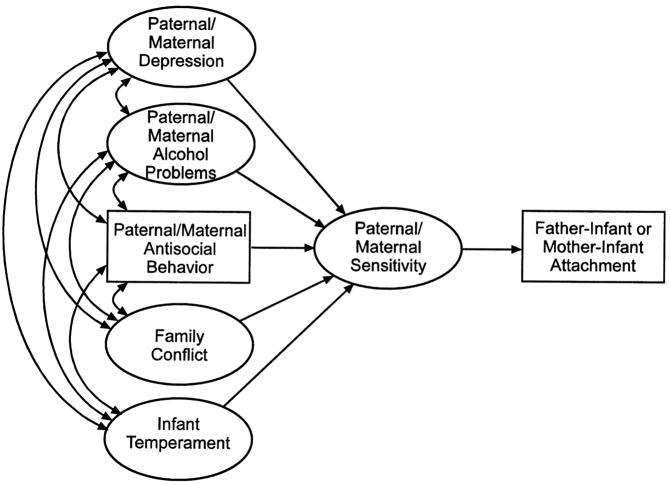
To test whether the associations between alcohol or other risk factors and attachment were indirect, via parental sensitivity, an indirect effects model was evaluated (see Figure 1 for conceptual models depicting associations with father–infant and mother–infant attachment). Direct paths not predictive of attachment were trimmed from the model before testing indirect paths. The indirect association between alcohol or other risk factors and attachment, via parental sensitivity, was tested in three steps. In the first step, a baseline indirect effects model was estimated in which all the paths from alcohol or other risk factors to parental sensitivity or attachment and the path from sensitivity to attachment were constrained to zero. The baseline indirect effects model included significant noncausal associations among alcohol and other risk factors. In step 2, the path from alcohol to sensitivity and from sensitivity to attachment was freely estimated. In step 3, the path from other risk factors to sensitivity was also freely estimated.
Figure 1.
Conceptual model: associations with parent–infant attachment.
All SEM analyses were conducted using AMOS software (Arbuckle, 1997). Maximum likelihood estimation procedures were used, and standardized parameter estimates are presented. The goodness of fit of the models was examined by using the comparative fit index (CFI), the nonnormed fit index (NFI), and the root mean square error of approximation (RMSEA). The CFI and NFI vary between 0 and 1.0 and values of .90 or higher indicate acceptable fit (Hu & Bentler, 1995). The RMSEA is bounded by zero and will take on that value when a model exactly reproduces a set of observed data. A value of .05–.06 is indicative of close fit, a value of .08 is indicative of marginal fit, and higher values are indicative of poor fit (Browne & Cudeck, 1994). The chi-square difference test was used to compare the fit of successive nested models. The means, standard deviations, and zero-order correlations for variables in the model are presented in Table 2.
Table 2.
Means, standard deviations, and correlation matrices for variables in the models
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 0.16 | 0.72 | −0.08 | 2.83 | 3.67 | 2.08 | 1.22 | 0.68 | 10.85 | 17.84 | 3.95 | 4.37 | 3.77 | 36.03 | 0.90 | 7.52 | 0.03 | 2.82 | 2.94 | 1.76 | 0.90 | 11.45 | 17.78 | 3.71 | 4.40 | 3.77 | 39.86 |
| SD | 0.26 | 0.79 | 0.61 | 0.95 | 0.91 | 0.93 | 0.76 | 0.67 | 3.34 | 4.16 | 0.72 | 0.55 | 0.70 | 5.60 | 0.53 | 2.31 | 0.53 | 0.95 | 0.91 | 0.90 | 0.74 | 3.36 | 3.46 | 0.76 | 0.52 | 0.67 | 8.88 |
| 1. | |||||||||||||||||||||||||||
| 2. | 0.55 | ||||||||||||||||||||||||||
| 3. | 0.69 | 0.61 | |||||||||||||||||||||||||
| 4. | 0.00 | 0.15 | 0.06 | ||||||||||||||||||||||||
| 5. | −0.08 | 0.05 | −0.05 | 0.68 | |||||||||||||||||||||||
| 6. | 0.01 | 0.13 | 0.05 | 0.70 | 0.63 | ||||||||||||||||||||||
| 7. | −0.02 | 0.07 | 0.12 | 0.27 | 0.27 | 0.32 | |||||||||||||||||||||
| 8. | −0.01 | 0.09 | 0.15 | 0.21 | 0.19 | 0.28 | 0.70 | ||||||||||||||||||||
| 9. | 0.08 | 0.00 | 0.03 | 0.05 | 0.13 | 0.08 | 0.05 | 0.05 | |||||||||||||||||||
| 10. | 0.06 | −0.02 | 0.08 | 0.19 | 0.21 | 0.20 | 0.05 | 0.02 | 0.68 | ||||||||||||||||||
| 11. | −0.07 | −0.09 | −0.10 | −0.12 | −0.05 | −0.08 | −0.10 | −0.17 | 0.01 | −0.07 | |||||||||||||||||
| 12. | −0.14 | −0.12 | −0.17 | −0.10 | −0.06 | −0.03 | −0.12 | −0.14 | 0.03 | −0.04 | 0.56 | ||||||||||||||||
| 13. | −0.16 | −0.11 | −0.17 | −0.15 | −0.04 | −0.11 | −0.07 | −0.14 | 0.04 | 0.04 | 0.70 | 0.64 | |||||||||||||||
| 14. | 0.24 | 0.32 | 0.34 | 0.22 | 0.23 | 0.30 | 0.24 | 0.28 | 0.03 | 0.05 | −0.03 | −0.17 | −0.05 | ||||||||||||||
| 15. | 0.28 | 0.18 | 0.34 | 0.11 | 0.07 | 0.15 | 0.24 | 0.16 | 0.11 | 0.12 | −0.02 | −0.03 | 0.03 | 0.24 | |||||||||||||
| 16. | 0.04 | 0.15 | 0.22 | 0.10 | 0.13 | 0.17 | 0.31 | 0.29 | 0.05 | 0.05 | 0.02 | 0.05 | 0.07 | 0.33 | 0.62 | ||||||||||||
| 17. | 0.19 | 0.23 | 0.36 | 0.16 | 0.13 | 0.24 | 0.32 | 0.26 | 0.10 | 0.08 | −0.08 | −0.03 | 0.01 | 0.34 | 0.80 | 0.77 | |||||||||||
| 18. | −0.08 | 0.02 | 0.03 | 0.20 | 0.16 | 0.18 | 0.28 | 0.29 | −0.01 | 0.10 | −0.14 | −0.06 | −0.10 | 0.15 | 0.18 | 0.27 | 0.17 | ||||||||||
| 19. | −0.10 | 0.00 | 0.00 | 0.07 | 0.14 | 0.14 | 0.18 | 0.22 | 0.06 | 0.07 | −0.03 | 0.01 | 0.12 | 0.18 | 0.12 | 0.26 | 0.22 | 0.61 | |||||||||
| 20. | −0.12 | 0.01 | 0.04 | 0.11 | 0.11 | 0.13 | 0.23 | 0.29 | 0.06 | 0.11 | −0.07 | 0.02 | 0.02 | 0.16 | 0.12 | 0.30 | 0.20 | 0.70 | 0.65 | ||||||||
| 21. | −0.00 | 0.09 | 0.08 | 0.26 | 0.29 | 0.30 | 0.65 | 0.57 | 0.02 | 0.03 | −0.13 | −0.17 | −0.11 | 0.32 | 0.14 | 0.30 | 0.27 | 0.37 | 0.29 | 0.35 | |||||||
| 22. | −0.01 | −0.03 | −0.02 | 0.10 | 0.16 | 0.10 | 0.09 | 0.14 | 0.50 | 0.45 | −0.14 | −0.07 | −0.02 | 0.11 | 0.07 | 0.12 | 0.15 | 0.17 | 0.24 | 0.35 | 0.16 | ||||||
| 23. | −0.09 | −0.08 | −0.06 | 0.12 | 0.17 | 0.07 | 0.11 | 0.10 | 0.43 | 0.53 | −0.10 | −0.08 | −0.05 | 0.12 | 0.06 | 0.10 | 0.13 | 0.15 | 0.23 | 0.20 | 0.13 | 0.59 | |||||
| 24. | −0.02 | −0.08 | −0.02 | −0.08 | −0.08 | −0.05 | −0.10 | −0.11 | −0.06 | 0.06 | 0.22 | 0.14 | 0.19 | −0.07 | −0.14 | −0.10 | −0.16 | −0.15 | −0.10 | −0.15 | −0.20 | −0.17 | −0.20 | ||||
| 25. | 0.01 | −0.03 | −0.10 | 0.00 | −0.03 | −0.07 | −0.10 | −0.05 | −0.05 | 0.04 | 0.14 | 0.23 | 0.21 | −0.02 | −0.09 | −0.03 | −0.16 | −0.08 | 0.01 | −0.03 | −0.17 | −0.06 | 0.04 | 0.50 | |||
| 26. | −0.02 | −0.13 | −0.10 | −0.07 | −0.08 | −0.14 | −0.14 | −0.10 | −0.06 | 0.04 | 0.22 | 0.19 | 0.25 | −0.08 | −0.12 | −0.13 | −0.18 | −0.19 | −0.06 | −0.13 | −0.19 | −0.05 | 0.06 | 0.72 | 0.66 | ||
| 27. | 0.10 | 0.20 | 0.24 | 0.20 | 0.17 | 0.27 | 0.29 | 0.23 | 0.08 | 0.09 | −0.05 | −0.14 | −0.06 | 0.45 | 0.40 | 0.49 | 0.48 | 0.26 | 0.20 | 0.24 | 0.33 | 0.20 | 0.17 | −0.17 | −0.17 | −0.18 |
Note: Correlations at .13 or higher are significant at p < .05 level. Correlations at .17 or higher are significant at p < .01 level.
High scores on MNAFF and FNAFF indicate low negative affect. 1, mothers’ QFI; 2, mothers’ dependence symptoms; 3, mothers’ severity of heavy drinking; 4, mothers’ depression subscale 1; 5, mothers’ depression subscale 2; 6, mothers’ depression subscale 3; 7, mothers’ moderate aggression; 8, mothers’ severe aggression; 9, maternal report of difficult temperament subscale 1; 10, maternal report of difficult temperament subscale 2; 11, mothers’ positive engagement; 12, mothers’ negative affect; 13, mothers’ sensitivity; 14, mothers’ antisocial behavior; 15, fathers’ QFI; 16, fathers’ last year dependence symptoms; 17, fathers’ severity of heavy drinking; 18, fathers’ depression subscale 1; 19, fathers’ depression subscale 2; 20, fathers’ depression subscale 3; 21, fathers’ total aggression; 22, fathers’ difficult temperament sub-scale 1; 23, fathers’ difficult temperament subscale 2; 24, mothers’ positive engagement; 25, mothers’ negative affect; 26, mothers’ sensitivity; 27, mothers’ antisocial behavior.
The final set of analyses involved the risk scores. We were interested in addressing two questions involving risk: (a) was there an association between cumulative risk and attachment security and was this association stronger when cumulative risk included parental alcohol problems, and (b) was there an interaction effect of risk and alcohol problems such that the association between attachment security and alcohol was exacerbated in the presence of other cumulative risk. To address the first question, we first used correlational analyses to examine the associations between the two risk scores and the continuous scores on attachment security. Next, we used ANOVA with the four attachment classifications as the independent variable and the two risk scores as the dependent variables in order to examine differences in risk across the four attachment classifications. To answer the second question, we used regression analyses, entering the main effects in the first step (alcohol problems and risk score) followed by the two interaction terms (fathers’ alcohol problem and risk, mothers’ alcohol problem and risk).
Results
Demographics and gender differences
ANOVA were used to examine group differences on variables including family income, parental education, parental age, number of parental work hours, parity, amount of time fathers spent playing with their infants, and ratings of frequency of participation in changing, feeding, and taking care of the baby. These analyses yielded no group differences on any of the demographic variables other than fathers’ education, F (1, 219) = 6.64, p < .05. Alcoholic fathers were somewhat less educated (M = 13.09, SD = 2.57) compared to those in the nonalcoholic group (M = 14.11, SD = 3.29). Fathers’ education was not associated with infant attachment patterns with mother or father but was associated with fathers’ parenting behavior during play with Pearson correlations ranging from r = .20, p < .05, for sensitivity to r = .28, p < .01, for positive engagement. All SEM analyses involving fathers’ parenting behavior were conducted after including a path from fathers’ education to fathers’ parenting behavior.
Possible gender differences on all study variables including demographics were examined using multivariate ANOVA (MANOVA). The dependent variables included composite measures of parents’ depression, antisocial behavior, family conflict, fathers’ sensitivity, and mothers’ sensitivity. These multivariate analyses indicated no significant gender differences. Chi-square analyses were used to examine gender differences in attachment patterns (secure/insecure and the continuous ratings). There were no gender differences in infant attachment to mother or father. In order to examine potential alcohol group by gender interactions on all variables, 2 (alcoholic, nonalcoholic) × 2 (boys, girls) MANOVAs were conducted with parents’ depression, antisocial behavior, family conflict, and parenting behavior. These analyses yielded no group by gender interaction effects.
Paternal alcoholism and infant attachment security with father
Of the 223 mother–infant dyads who completed the Strange Situation, 65% were classified as secure, 14% as avoidant, 13% as resistant, and 8% as disorganized. Of the 220 father–infant dyads who completed the Strange Situation, 61% were classified as secure, 12% as avoidant, 17% as resistant, and 11% as disorganized. Chi-square analyses with the four infant attachment classifications with mother and the three groups (nonalcoholic, father alcoholic, and father alcoholic/mother heavy drinking) revealed a significant association, χ2 (6) = 16.40, p < .01. Within the nonalcoholic group, 69% were classified as secure, 10% as avoidant, 16% as resistant, and 5% as disorganized. Within the father alcoholic group, 59% were classified as secure, 13% as avoidant, 16% as resistant, and 12% as disorganized. Within the father alcoholic/mother heavy drinking group, 30% were classified as secure, 15% as avoidant, 25% as resistant, and 30% as disorganized. Chi-square analyses with the four infant–father attachment classifications and the three groups (nonalcoholic, father alcoholic, father alcoholic/mother heavy drinking) revealed a significant association, χ2 (6) = 16.78, p < .01 (see Table 3). Within the nonalcoholic group, 70% were classified as secure, 9% as avoidant, 15% as resistant, and 6% as disorganized. Within the father alcoholic group, 62% were classified as secure, 15% as avoidant, 14% as resistant, and 9% as disorganized. Within the father alcoholic/mother heavy drinking group, 50% were classified as secure, 40% as avoidant, 0% as resistant, and 10% as disorganized. Thus, the infants in the father alcoholic/mother heavy drinking group were most at risk for insecure attachment with both parents.
Table 3.
Associations between group status and parent–infant attachment
| Attachment (%) |
||||
|---|---|---|---|---|
| Secure | Avoidant | Resistant | Disorganized | |
| Mother–infant attachment (n = 223) | ||||
| Nonalcoholic (n = 104) | 69 | 10 | 16 | 5 |
| Alcoholic father (n = 99) | 59 | 13 | 16 | 12 |
| Alcoholic father + heavy drinking mother (n = 20) | 30 | 15 | 25 | 30 |
| Father–infant attachment (n = 220) | ||||
| Nonalcoholic (n = 101) | 70 | 9 | 15 | 6 |
| Alcoholic father (n = 99) | 62 | 15 | 14 | 9 |
| Alcoholic father + heavy drinking mother (n = 20) | 50 | 40 | 0 | 10 |
Direct associations with father–infant attachment
Compared with the baseline direct effects model, the first direct effects model fit the data marginally better, Δχ2 (1) = 3.34, p < .10 (see Table 4), indicating a marginal association between fathers’ alcohol problem and infant attachment security with father (β = .12, p < .10). Higher paternal alcohol problem was associated with higher insecurity. Next, a second direct effects model was estimated in which the paths from all other risk factors including fathers’ alcohol problems to infant attachment security was freely estimated. The fit of this model was compared with the first direct effects model and indicated no significant improvement in fit, Δχ2 (4) = 2.35, ns (see Table 4). None of the paths from the other risk factors were directly associated with infant attachment security with father. However, the addition of these risk factors to the model reduced the direct association between fathers’ alcohol problems and infant security (β = .07, ns), indicating that these other risk factors accounted for some of the variance associated with fathers’ alcohol problems.
Table 4.
Goodness-of-fit summary for father–infant attachment
| Model | χ2 | df | NFI | CFI | RMSEA (90% CI) |
|---|---|---|---|---|---|
| Direct effects | |||||
| Baseline | 162.88 | 86 | 0.98 | 0.99 | .059 (.043, .073) |
| Model 1a | 159.42 | 85 | 0.98 | 0.99 | .058 (.043, .073) |
| Model 2b | 157.07 | 81 | 0.98 | 0.99 | .06 (.044, .075) |
| Indirect effects | |||||
| Baseline | 277.79 | 148 | 0.97 | 0.99 | .059 (.047, .071) |
| Model 1c | 269.60 | 146 | 0.98 | 0.99 | .060 (.049, .070) |
| Model 2d | 265.25 | 142 | 0.98 | 0.99 | .057 (.045, .069) |
Note: NFI, nonnormed fit index; CFI, comparative fit index; RMSEA, root mean square error of approximation; CI, confidence interval. All effects were significant at p < .001.
Direct paths from other risk factors to attachment constrained to zero.
Direct paths from other risk factors to attachment estimated.
Paths from other risk factors to fathers’ sensitivity constrained to zero—final model.
Paths from other risk factors to fathers’ sensitivity estimated.
Indirect associations with father–infant attachment via paternal sensitivity
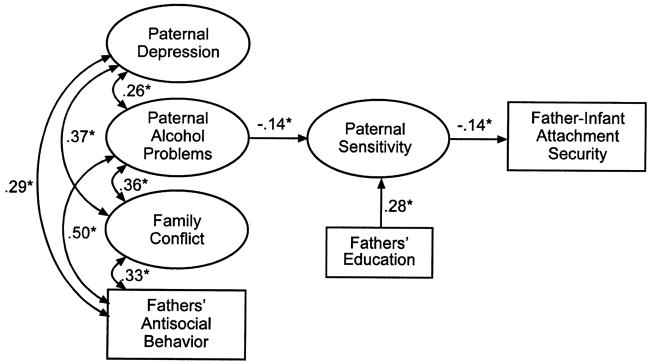
Compared with the baseline indirect effects model, the first indirect effects model, in which the paths from fathers’ alcohol problems to fathers’ sensitivity and from fathers’ sensitivity to infant attachment security were freely estimated, fit the data significantly better, Δχ2 (2) = 8.20, p < .05 (see Table 4). Fathers’ alcohol problem was significantly associated with fathers’ sensitivity (β = −.14, p < .05), and fathers’ sensitivity was significantly associated with infant attachment security with father (β = −.14, p < .05). Higher paternal alcohol problem was associated with lower paternal sensitivity, and lower paternal sensitivity was associated with higher insecurity. In the second indirect effects model, paths from all other risk factors to fathers’ sensitivity were freely estimated. Because the direct effects modeling did not yield any significant direct associations between alcohol or other risk factors and infant attachment, no direct paths were included. The second indirect effects model did not result in a significant improvement in fit, Δχ2 (4) = 4.42, ns (see Table 4). The paths from all of the additional risk factors to fathers’ sensitivity were not significant, although the addition of these paths to the model reduced the association between fathers’ alcohol problem and fathers’ sensitivity (β = −.08, ns). The final model predicting infant attachment security with father is depicted in Figure 2.
Figure 2.
Final model: associations with father–infant attachment. For purposes of clarity, only significant parameter estimates are displayed. *p < .05.
Direct associations with mother–Infant attachment
Compared with the baseline direct effects model, the first indirect effects model (in which the path from fathers’ alcohol problem and mothers’ alcohol problem to mother–infant attachment security was freely estimated) resulted in a marginal improvement in fit, Δχ2 (2) = 5.12, p = .06 (Table 5). The path from fathers’ alcohol problem to mother–infant attachment security was significant (β = .15, p < .05). Higher paternal alcohol problem was associated with higher insecurity. The path from maternal alcohol problem to mother–infant attachment security was not significant (β = .01, ns). A second direct effects model was estimated next with the paths from other risk factors to mother–infant attachment security freely estimated. This model did not result in a significant improvement in fit, Δχ2 (4) = 5.09, ns (Table 5). However, there was a significant association between maternal depression and mother–infant attachment security (β = .19, p < .05). Higher maternal depression was associated with higher insecurity. None of the other paths were significant. Moreover, with all other risk factors in the model, the path from fathers’ alcohol problems to mother–infant attachment security was not significant (β = .14, ns).
Table 5.
Goodness of fit summary for mother–infant attachment
| Model | χ2 | df | NFI | CFI | RMSEA (90% CI) |
|---|---|---|---|---|---|
| Direct Effects | |||||
| Baseline | 210.83 | 128 | 0.98 | 0.99 | .053 (.040, .065) |
| Model 1a | 205.72 | 126 | 0.98 | 0.99 | .052 (.039, .065) |
| Model 2b | 200.85 | 122 | 0.98 | .053 (.039, .065) | |
| Indirect effects | |||||
| Baseline | 291.82 | 182 | 0.97 | 0.99 | .051 (.040, .062) |
| Model 1c | 276.99 | 178 | 0.98 | 0.99 | .049 (.037, .060) |
| Model 2d | 268.37 | 174 | 0.98 | 0.99 | .048 (.036, .059) |
Note: NFI, nonnormed fit index; CFI, comparative fit index; RMSEA, root mean square error of approximation; CI, confidence interval. All effects were significant at p < .001.
Direct paths from other risk factors to attachment constrained to zero.
Direct paths from other risk factors to attachment estimated.
Paths from other risk factors to mothers’ sensitivity constrained to zero.
Paths from other risk factors to mothers’ sensitivity estimated—final model.
Indirect associations with mother–infant attachment via maternal sensitivity
Given the direct association between maternal depression and mother–infant attachment security, the direct path from maternal depression to mother–infant attachment security was freely estimated in the indirect model. Compared to the baseline model, Model 1 resulted in a significant improvement in fit, Δχ2 (4) = 14.87, p < .01 (Table 5). The direct path from maternal depression to attachment and from maternal alcohol problems to maternal sensitivity were both significant (see Figure 3). In Model 2, the paths from other risk factors were freely estimated. Compared with Model 1, this resulted in a marginal improvement in fit, Δχ2 (4) = 9.84, p < .05 (Table 5). In addition to the path from maternal alcohol problems to maternal sensitivity, the path from family conflict to maternal sensitivity was marginally significant. The final indirect model is depicted in Figure 3.
Figure 3.
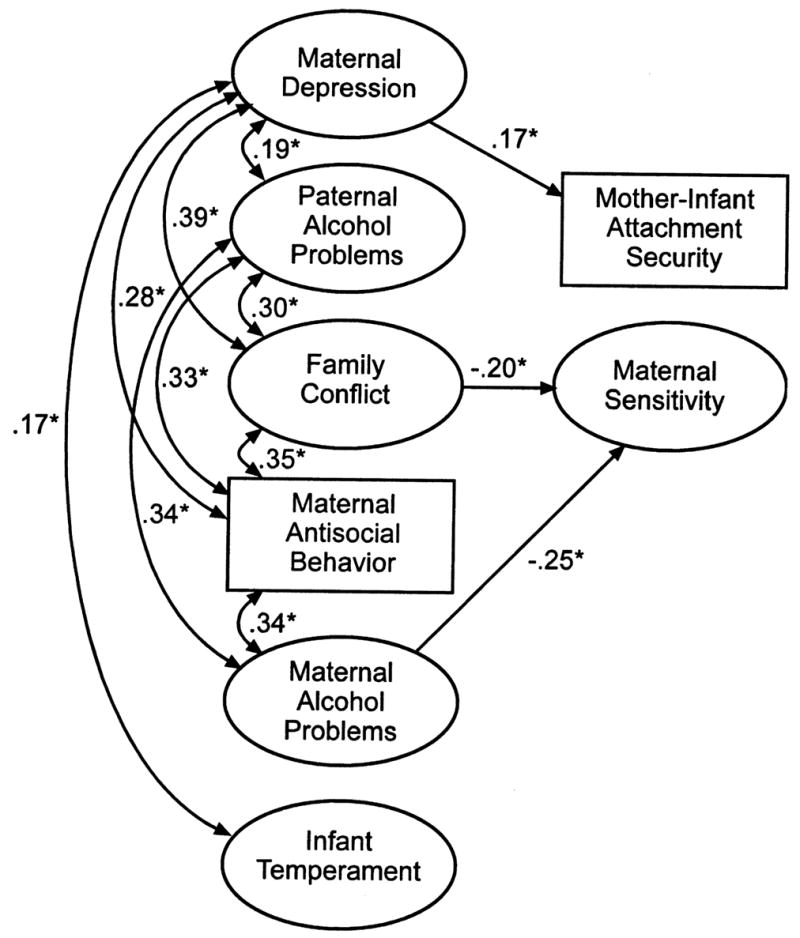
Final model: associations with mother–infant attachment. For purposes of clarity, only significant parameter estimates are displayed. *p < .05.
Analyses with cumulative risk scores: Associations between risk and attachment
There were significant associations between both the risk scores and infant attachment security with father and mother. The correlations between cumulative risk with and without alcohol and attachment security with mother were r = .17, p < .01, and r = .14, p < .05, respectively. The correlations between cumulative risk with and without alcohol and attachment security with father were r = .20, p < .01, and r = .15, p < .05, respectively. Test of the difference between nonindependent correlations indicated that the two correlations were not significantly different from each other. Thus, adding parental alcohol problems to cumulative risk did not increase the association between risk and infant attachment security with either parent.
Differences in risk scores with the four mother–infant attachment classifications were examined next. ANOVA indicated that the four groups differed in both risk with alcohol, F (1, 225) = 4.41, p < .01, and risk without alcohol, F (1, 225) = 3.80, p < .05. Simple contrasts indicated that infants who were classified as disorganized with mother were significantly different in cumulative family risk scores (both with and without alcohol) compared to infants who were classified as secure and those who were classified as resistant (see Table 6). For father–infant attachment classifications, infants who were avoidant with fathers were significantly different in cumulative family risk scores (both with and without alcohol) compared to infants who were classified as secure (see Table 6).
Table 6.
Means and standard deviations for the four attachment classifications on cumulative risk with and without alcohol
| Attachment with Mother |
Attachment with Father |
|||||||
|---|---|---|---|---|---|---|---|---|
| Risk | A | B | C | D | A | B | C | D |
| With alcohol | 5.72 (3.51) | 4.34a (3.05) | 4.00a (3.34) | 6.58b (3.32) | 6.54a (3.74) | 4.08b (3.04) | 4.92 (3.03) | 5.55 (2.84) |
| Without alcohol | 3.41 (2.59) | 3.04a (2.32) | 2.50a (2.54) | 4.79b (2.82) | 4.77a (2.80) | 2.78b (2.39) | 3.16 (2.14) | 3.48 (2.13) |
Note: The standard deviations are in parentheses. Means with different subscript letters are significantly different from each other. A, avoidant; B, secure; C, resistant; D, disorganized.
Analyses with cumulative risk scores: Interaction effects
Two hierarchical regression analyses were conducted: the first with mother–infant attachment security rating as the criterion and the second with father–infant attachment security as the criterion. The composite alcohol problem scores for both parents and the cumulative risk score without alcohol were entered in the first step followed by the interaction terms of fathers’ alcohol and risk and mothers’ alcohol and risk in the second step. These analyses yielded no significant interaction effects of alcohol and risk. Thus, cumulative family risk did not interact with parental alcohol problems to predict infant attachment security with either parent.
Discussion
The major goal of this study was to examine any association between parents’ alcohol problems and parent–infant attachment. Results indicate that infants in families with two alcohol problem parents are more likely to display insecure patterns of attachment with both mother and father. The rates of insecure attachment displayed within this group, both with mother and father, are similar to those in other high-risk groups (see Lyons–Ruth, Repacholi, McLeod, & Silva, 1991, for review). However, most of these earlier studies with high risk samples have been conducted with mothers only and have noted high rates of disorganized infant attachment behavior with mother. It is worth noting that in our study, the patterns of insecure infant attachment with mothers and fathers varied within the group of families with two alcohol problem parents. Similar to previous studies of infants exposed to other risk conditions, the predominant pattern of insecurity displayed by infants with two alcohol problem parents was the disorganized pattern. Approximately 30% of infants with problem drinking mothers and fathers displayed a disorganized pattern of attachment with mother compared with 5% in the nonalcoholic group. However, the predominant pattern of attachment displayed with the father by infants with two alcohol problem parents was the avoidant pattern. Approximately 40% of infants with two alcohol problem parents displayed an avoidant pattern of attachment with father compared with 9% in the nonalcoholic group. Few studies with high risk samples have included an examination of father–infant attachment. The developmental implications of different patterns of insecure attachment with mother and father are currently unclear. Future studies with larger sample sizes of heavy drinking mothers with alcoholic partners and longitudinal follow-ups will be better able to answer this question. It is worth noting that the differences in secure versus insecure patterns of attachment between families with alcoholic fathers and light drinking mothers and those with nonalcoholic parents were minor. One explanation for these minor differences may be the substantial heterogeneity in risk within alcoholic families. There was wide variation in the range of alcohol problems and associated risk characteristics within the alcoholic group. Other researchers have also noted that alcoholic families differ substantially in risk structure, and these differences might account for the heterogeneity in outcomes among children of alcoholics (Zucker et al., 1995).
Given this variation in risk structure, the next step was to examine the hypothesis that parenting and the quality of parent–infant attachment in alcoholic and nonalcoholic families would be associated with variables in three major domains: parent, child, and contextual. Within each domain, aspects of functioning that were of particular relevance to alcohol were chosen as the critical sources of influence. Thus, within the parent domain, we chose parents’ alcohol problems, depression, and antisocial behavior; within the child domain, we chose child fussy/difficult temperament; within the contextual domain, we chose family conflict as the major predictors of parenting and infant attachment security. The results of this study indicate that variables within the parent domain were associated with parenting and infant attachment security. Variables within the contextual domain were associated with maternal sensitivity but not attachment. The variables from the child domain did not contribute to our understanding of factors associated with the quality of parenting and infant attachment. However, our measurement of factors in the child domain was limited. An in-depth investigation of child’s regulatory capacities, including perhaps physiological or behavioral measures in addition to parent report, have yielded different results. Results indicated that fathers with higher alcohol problems were less sensitive during interactions with their infants, and this lower level of sensitivity was associated with a greater risk for attachment insecurity with fathers. Results also indicated that the association between fathers’ alcohol problem and infant attachment with mother was mediated through maternal depression. Moreover, maternal alcohol problems and family conflict were associated with maternal sensitivity but not with mother–infant attachment.
In their meta-analyses of infant–father attachment, van Ijzendoorn and De Wolff (1997) noted that studies examining the role of fathers in the development of infant attachment were few in number. The results from the present study add to a growing literature on the impact of fathers on the development of infant attachment. The result linking fathers’ alcoholism to father–infant attachment through the quality of fathers’ parenting behavior lends further support to previous studies indicating that fathers’ alcoholism is associated with negative family and child outcomes as early as infancy (Eiden & Leonard, 2000; Eiden et al., 1999). Fathers’ alcoholism has been linked with increased risk for fathers’ aggravation with their infants and with higher negative affect, lower positive engagement, and lower sensitivity during free-play interactions. The results from the present study further extend these associations linking fathers’ negative parenting behavior with one crucial aspect of socioemotional development in infancy: the development of infant attachment.
The results regarding infant–mother attachment extend the findings from a previous study (Eiden & Leonard, 1996) indicating associations between fathers’ heavy drinking and higher risk for attachment insecurity with mother. The present results suggest that maternal depression mediates the association between fathers’ alcoholism and infant–mother attachment. Depression is a common feature among women with alcoholic or substance abusing partners (Bresnahan, Zuckerman, & Cabral, 1992; Finney, Moos, Cronkite, & Gamble, 1983; Jacob, Dunn, Leonard, & Davis, 1985; Kocmur & Rus, 1996; Wilsnack & Wilsnack, 1995). Several studies have noted that maternal depression is associated with an increased risk for insecure attachment with mother, especially when this depression occurs in the context of family dysfunction (Carter et al., 2001). This is clearly the case with families with alcoholic fathers.
Somewhat surprisingly, there was no association between maternal alcohol problem and mother–infant attachment or between maternal sensitivity and the continuous measure of infant–mother attachment in this study. One explanation for lack of associations with maternal alcohol use may be the limited range of maternal alcohol problems in our study. The majority of the mothers were light to moderate drinkers with few alcohol problems. Although in an earlier report we noted associations between maternal alcohol problem and maternal sensitivity during free-play interactions, the lack of association between maternal sensitivity and attachment security with mother precluded the possibility of an indirect association between mothers’ alcohol problem and attachment security via maternal sensitivity. One explanation for this may be that the free-play and structured-play situations did not adequately capture the essential features of maternal sensitivity that were predictive of infant attachment. An examination of differences in maternal behavior across attachment classifications indicated that there were significant differences in positive engagement and sensitivity. Simple contrasts indicated that these differences were between the secure and disorganized classifications. There were no differences in maternal behavior between secure and avoidant or secure and resistant classifications. Thus, a second explanation for these findings may be that whereas the laboratory situations captured differences among mothers on the two ends of the distribution on the security rating (secure and disorganized), they did not adequately capture the differences between secure and the other two insecure dyads, resulting in lack of association with the continuous attachment security rating. Moreover, our ratings of mother–infant interactions measured aspects of maternal behavior beyond maternal sensitivity alone. Perhaps narrower measures of maternal sensitivity that are theoretically associated with the development of attachment would be more appropriate as predictors of infant–mother attachment (for further discussion of this issue, see De Wolff & van Ijzendoorn, 1997; Goldberg, Grusec, & Jenkins, 1999). Another explanation for this lack of association, especially in contrast with associations between fathers’ sensitivity and infant attachment, may be that mothers of infants with less extreme insecure attachment patterns with respect to the continuous rating of security (resistant and avoidant) were able to perform in a more positive way while being videotaped than were fathers.
Maternal alcohol problems and family conflict were both associated with maternal sensitivity during play interactions. Although the literature on the association between maternal alcohol problems, especially postnatal alcohol problems in the absence of prenatal problems, is limited, at least one previous study has demonstrated the association between maternal alcohol use and mother–infant interactions (O’Connor, Sigman, & Kasari, 1992). However, O’Connor and her colleagues reported that the association between maternal alcohol consumption during pregnancy and the quality of mother–infant interactions was mediated by negative infant affect (similar to the conceptualization of fussy/difficult temperament). Postnatal alcohol use was not associated with mother–infant interactions or infant attachment. The present study extends the findings by including a group of women with problematic postnatal alcohol use but low levels of pregnancy drinking (at least according to self-report) and excluding infants on the basis of perinatal risk (prematurity, low birth weight, etc.). Moreover, it extends the findings to other postnatal risk characteristics. The results suggest that women with higher postnatal alcohol problems are more likely to have partners with alcohol problems, are more antisocial, and have higher family conflict; and these risk characteristics are interrelated. Family conflict also had a direct association with maternal sensitivity. The importance of family conflict as a predictor of child outcomes has been well documented (see Cummings & Davies, 1994; Cummings, Goeke–Morey, & Papp, 2001). The results from the present study suggest that one explanation for the association between family conflict and negative child outcomes noted by previous researchers may be through the impact of family conflict on the quality of mothers’ parenting behavior.
Infant temperament was not associated with fathers’ alcohol problem, nor was it associated with the quality of the parent–infant relationships. In other reports, we have noted weak or sporadic associations between fathers’ reports of infant fussy/difficult temperament and fathers’ alcoholism (Edwards, Leonard, & Eiden, in press; Eiden et al., 1999). When we combined paternal and maternal reports into a single construct reflecting fussy/difficult temperament, this association was no longer significant. Thus, the association between fathers’ reports and fathers’ alcoholism may have been more a reflection of fathers’ personality and perceptions of infant behavior than a reflection of infant behaviors per se. Several studies have reported stronger associations between parental personality or psychological functioning and their reports of infant temperament than between observations of infant behavior and parent reports of infant temperament (e.g., Sameroff, Seifer, & Elias, 1982; Vaughn, Bradley, Joffe, Seifer, & Barglow, 1987; Vaughn, Taraldson, Crichton, & Egeland, 1981). As stated previously, more objective measures of infant temperament, such as physiological and behavioral measures, may have better captured variations in child temperament independent of parental functioning. Others have noted that the interaction between parental personality and child’s negative emotionality was predictive of parental behavior during interactions (Clark, Kochanska, & Ready, 2000) different patterns of emotionality are associated with each of the four attachment patterns, and children with different attachment histories varied in emotional development across the first 3 years (Kochanska, 2001). How this research relates to development among children of alcoholics is an area for further study.
Contrary to expectations, the association between parental alcohol problems and infant attachment was not exacerbated in the presence of additional family risk; that is, there were no interactive effects of alcohol and risk on infant attachment with either parent, nor did the addition of alcohol problems to the cumulative risk score improve the association between risk and attachment. The strength of association between higher family risk and higher insecurity with either parent remained the same with or without the addition of parental alcohol problems to the cumulative risk score. In this sample of alcoholic and nonalcoholic fathers, paternal alcoholism and maternal depression served as markers of overall parental risk for an insecure parent–infant relationship. However, no causal inferences can be drawn about the role of alcoholism or depression in predicting insecurity.
Interestingly, the association between risk and specific attachment patterns differed across parents, similar to those discussed previously. For mother–infant attachment classifications, infants who were classified as disorganized with mother had higher family risk scores compared to those who were classified as secure or resistant. For father–infant attachment classifications, infants who were classified as avoidant had higher risk scores compared to those who were classified as secure. This is a result that needs replication with other high risk samples.
There are several limitations in this study. First, although deriving our sample from birth records has important advantages over newspaper or clinic-based samples, there are also limitations. The response rate to our open letter of recruitment was slightly above 25%. This raises the possibility that respondents to our recruitment may have been a biased group. Our comparison of respondents with the entire population of birth records suggested that the bias was small with respect to the variables that we could examine. However, there could have been more significant biases in variables that we could not assess. Second, this study utilized self-report data with respect to parental alcohol problems and psychopathology. Third, the results reported here are based on cross-sectional data; hence, no causal inferences can be reached about the role of parental alcoholism or associated risk factors in predicting infant attachment. Fourth, given the nature of the design, the role of maternal alcohol problem cannot be examined independently from fathers’ alcohol problems. Further, because only a small proportion of the mothers in our sample experienced alcohol problems, our ability to fully examine the role of maternal alcohol problems was limited. However, it is important to note that in the majority of families with alcohol problems, maternal alcohol problem exists in the context of paternal alcohol problems. In other words, women with alcohol problems are more likely to have partners with alcohol problems than vice versa (see Roberts & Leonard, 1997, for further discussion). Future studies including samples of mothers with and without alcoholic partners may be able to better answer the question of the role of maternal alcohol problem in the development of infant attachment. Finally, the cutoffs used to create the composite risk indices are sample specific and, although consistent with methods used in other studies (e.g., Sameroff et al., 1993), might not generalize beyond this study. This is partly because many of the measures used to create the risk indices do not have clear clinical cutoffs (e.g., temperament, parental sensitivity, etc.). Nevertheless, this lack of clear clinical significance for the cutoffs may have been one reason why they did not distinguish between attachment patterns more clearly.
The results from this study demonstrated that infants with two alcohol problem parents were most at risk for insecure attachment with both mother and father. Fathers’ alcoholism was indirectly associated with infant attachment security with father via associations with fathers’ sensitivity. Maternal depression was associated with infant attachment security with mother. Further, fathers’ alcoholism was associated with other risk factors, such as parental depression, antisocial behavior, family conflict, and lower paternal sensitivity. These risk factors taken together were significantly associated with the parent–infant attachment security.
Acknowledgments
The authors thank the parents and infants who participated in this study and the research staff who were responsible for conducting numerous assessments with these families. Special thanks to Jenny Park, Melissa Peterson, Erica West, Felipa Chavez, and Chris Edwards for coding of parent–infant interactions and attachment and Dr. Douglas Teti for comments on earlier versions of this paper. This study was made possible by grants from NIAAA (1RO1 AA 10042–01A1) and NIDA (1K21DA00231–01A1).
References
- Ainsworth MDS, Wittig BA. Attachment and exploratory behavior of one year olds in a strange situation. In: Foss BM, editor. Determinants of infant behavior. Vol. 4. London: Methuen; 1969. [Google Scholar]
- Andreason NC, Rice J, Endicott J, Reich T, Coryell W. The family history approach to diagnosis. Archives of General Psychiatry. 1986;43:421–429. doi: 10.1001/archpsyc.1986.01800050019002. [DOI] [PubMed] [Google Scholar]
- Anthony JC, Warner LA, Kessler RC. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Experimental and Clinical Psychopharmacology. 1994;2:244–268. [Google Scholar]
- Arbuckle JL. AMOS Users’ Guide (Version 4.0) Chicago: SmallWaters; 1997. [Google Scholar]
- Bates JE, Freeland CAB, Lounsbury ML. Measurement of infant difficultness. Child Development. 1979;50:794–803. [PubMed] [Google Scholar]
- Belsky J. Attachment, mating, and parenting: An evolutionary interpretation. Human Nature. 1997;8:361–381. doi: 10.1007/BF02913039. [DOI] [PubMed] [Google Scholar]
- Belsky J, Rovine M, Taylor DG. The Pennsylvania Infant and Family Development Project: III. The origins of individual differences in infant–mother attachment: Maternal and infant contributions. Child Development. 1984;55:718–728. [PubMed] [Google Scholar]
- Blackson TC. Temperament: A salient correlate of risk factors for alcohol and drug abuse. Drug and Alcohol Dependence. 1994;36:205–214. doi: 10.1016/0376-8716(94)90146-5. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Boyd JH, Weissman MM, Thompson WD, Myers JK. Screening for depression in a community sample: Understanding the discrepancies between depression syndrome and diagnostic scales. Archives of General Psychiatry. 1982;39:1195–1200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- Bresnahan K, Zuckerman B, Cabral H. Psychosocial correlates of drug and heavy alcohol use among pregnant women at risk for drug use. Obstetrics and Gynecology. 1992;80:976–980. [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long J, editors. Testing structural equation models. Newbury Park, CA: Sage; 1994. pp. 136–162. [Google Scholar]
- Cahalan D, Cisin IH, Crossley H. American drinking practices: A national study of drinking, behavior and attitudes. New Brunswick, NJ: Rutgers Center of Alcohol Studies Monograph 1; 1969. [Google Scholar]
- Campbell SB, Cohn JF. The timing and chronicity of postpartum depression: Implications for infant development. In: Murray L, Cooper PJ, editors. Postpartum depression and child development. New York: Guilford Press; 1997. pp. 165–197. [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, Briggs–Gowan MJ. Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:18–26. doi: 10.1097/00004583-200101000-00012. [DOI] [PubMed] [Google Scholar]
- Chan AWK, Welte JW, Russell M. Screening for heavy drinking/alcoholism by the TWEAK test. Alcoholism: Clinical and Experimental Research. 1993;17:463. doi: 10.1111/j.1530-0277.1993.tb05226.x. [DOI] [PubMed] [Google Scholar]
- Chassin L, Collins RL, Ritter J, Shirley M. Vulnerability to substance use disorders across the lifespan. In: Ingram RE, Price JM, editors. Vulnerability to psychopathology: Risk across the lifespan. New York: Guilford Press; 2001. pp. 165–172. [Google Scholar]
- Chassin L, Rogosch F, Barrera M. Substance use and symptomatology among adolescent children of alcoholics. Journal of Abnormal Psychology. 1991;100:449–463. doi: 10.1037//0021-843x.100.4.449. [DOI] [PubMed] [Google Scholar]
- Clark LA, Kochanska G, Ready R. Mothers’ personality and its interaction with child temperament as predictors of parenting behavior. Journal of Personality and Social Psychology. 2000;79:274–285. doi: 10.1037//0022-3514.79.2.274. [DOI] [PubMed] [Google Scholar]
- Clark R, Musick J, Scott F, Klehr K. The Mothers’ Project Rating Scales of Mother–Child Interaction. 1980. Unpublished document. [Google Scholar]
- Cohn JF, Campbell SB. Influence of maternal depression on infant affect regulation. In: Cicchetti D, Toth SL, editors. Developmental perspectives on depression. 4. Rochester, NY: University of Rochester Press; 1992. pp. 103–130. [Google Scholar]
- Colder CR, Chassin L. Affectivity and impulsivity: Temperament risk for adolescent alcohol involvement. Psychology of Addictive Behaviors. 1997;11:83–97. [Google Scholar]
- Cowan PA. Beyond meta-analysis: A plea for a family systems view of attachment. Child Development. 1997;68:601–603. [PubMed] [Google Scholar]
- Cummings EM. Classification of attachment on a continuum of felt security: Illustrations from the study of children of depressed parents. In: Greenberg MT, Cicchetti D, et al., editors. Attachment in the preschool years: Theory, research, and intervention. Chicago: University of Chicago Press; 1990. pp. 311–338. [Google Scholar]
- Cummings EM, Davies P. Children and marital conflict: The impact of family dispute and resolution. New York: Guilford Press; 1994. [Google Scholar]
- Cummings EM, Goeke–Morey MC, Papp LM. Couple conflict, children, and families: It’s not just you and me, babe. In: Booth A, Crouter AC, editors. Couples in conflict. Mahwah, NJ: Erlbaum; 2001. pp. 117–147. [Google Scholar]
- DeMulder EK, Radke–Yarrow M. Attachment with affectively ill and well mothers: Concurrent behavioral correlates. Development and Psychopathology. 1991;3:227–242. [Google Scholar]
- De Wolff M, van Ijzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Donovan WL, Leavitt LA, Walsh RO. Conflict and depression predict maternal sensitivity to infant cries. Infant Behavior and Development. 1998;21:505–517. [Google Scholar]
- Easterbrooks MA, Biesecker G, Lyons–Ruth K. Infancy predictors of emotional availability in middle childhood: The roles of attachment security and maternal depressive symptomatology. Attachment and Human Development. 2000;2:170–187. doi: 10.1080/14616730050085545. [DOI] [PubMed] [Google Scholar]
- Edwards EP, Leonard KE, Eiden RD. Temperament and behavioral problems among infants in alcoholic families. Infant Mental Health Journal. doi: 10.1002/imhj.1007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Chavez F, Leonard KE. Parent–infant interactions in alcoholic and control families. Development and Psychopathology. 1999;11:745–762. doi: 10.1017/s0954579499002308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiden RD, Leonard KE. Paternal alcohol use and the mother–infant relationship. Development and Psychopathology. 1996;8:307–323. [Google Scholar]
- Eiden RD, Leonard KE. Paternal alcoholism, parental psychopathology, and aggravation with infants. Journal of Substance Abuse. 2000;11:17–29. doi: 10.1016/s0899-3289(99)00016-4. [DOI] [PubMed] [Google Scholar]
- Ensel WM. The role of age in the relationship of gender and marital status to depression. Journal of Nervous and Mental Disease. 1982;170:536–543. doi: 10.1097/00005053-198209000-00004. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Exposure to interparental violence in childhood and psychosocial adjustment in young adulthood. Child Abuse and Neglect. 1998;22:339–357. doi: 10.1016/s0145-2134(98)00004-0. [DOI] [PubMed] [Google Scholar]
- Field T, Sandberg D, Garcia R, Bega–Lahr N, Goldstein S, Guy L. Pregnancy problems, postpartum depression, and early mother–infant interactions. Developmental Psychology. 1985;21:1152–1156. [Google Scholar]
- Finney JW, Moos RH, Cronkite RC, Gamble W. A conceptual model of the functioning of married persons with impaired partners: Spouses of alcoholic patients. Journal of Marriage and the Family. 1983;45:23–34. [Google Scholar]
- Fitzgerald HE, Jones MA, Maguin E, Zucker RA, Noll RB. Assessing parental antisocial behavior in alcoholic and nonalcoholic families. 1991 Unpublished Work. [Google Scholar]
- Fleming AS, Ruble DN, Flett GL, Shaul DL. Postpartum adjustment in first-time mothers: Relations between mood, maternal attitudes, and mother–infant interactions. Developmental Psychology. 1988;24:71–81. [Google Scholar]
- Goldberg S, Grusec JE, Jenkins J. Narrow view of attachment or broad view of protection? Rejoinder to the commentaries. Journal of Family Psychology. 1999;13:503–507. [Google Scholar]
- Handal PJ, Tschannen T, Searight HR. The relationship of child adjustment to husbands’ and wives’ marital distress, perceived family conflict, and mothers’ occupational status. Child Psychiatry and Human Development. 1998;29:113–126. doi: 10.1023/a:1025083915840. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage; 1995. pp. 76–99. [Google Scholar]
- Jacob T, Dunn NJ, Leonard KE, Davis P. Alcohol-related impairments in male alcoholics and the psychiatric symptoms of their spouses: An attempt to replicate. American Journal of Drug and Alcohol Abuse. 1985;11:55–67. doi: 10.3109/00952998509016849. [DOI] [PubMed] [Google Scholar]
- Jacob T, Krahn GL, Leonard KE. Parent–child interactions in families with alcoholic fathers. Journal of Consulting and Clinical Psychology. 1991;59:176–181. [PubMed] [Google Scholar]
- Jansen RE, Fitzgerald HE, Ham HP, Zucker RA. Pathways into risk: Temperament and behavior problems in three-to-five year-old sons of alcoholics. Alcoholism Clinical and Experimental Research. 1995;19:501–509. doi: 10.1111/j.1530-0277.1995.tb01538.x. [DOI] [PubMed] [Google Scholar]
- Johnson S, Leonard KE, Jacob T. Drinking, drinking styles, and drug use in children of alcoholics, depressives, and controls. Journal of Studies on Alcohol. 1989;50:427–431. doi: 10.15288/jsa.1989.50.427. [DOI] [PubMed] [Google Scholar]
- Jouriles EN, Norwood WD, McDonald R, Vincent JP, Mahoney A. Physical violence and other forms of marital aggression: Links with children’s behavior problems. Journal of Family Psychology. 1996;10:223–234. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wiltchen HE, Kendler KS. Lifetime and 12 month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kochanska G. Emotional development in children with different attachment histories: The first three years. Child Development. 2001;72:474–490. doi: 10.1111/1467-8624.00291. [DOI] [PubMed] [Google Scholar]
- Kocmur M, Rus V. Depression and locus of control in alcoholics’ wives. Psychiatria Danubina. 1996;8:67–72. [Google Scholar]
- Leonard KE. Drinking patterns and intoxication in marital violence: Review, critique, and future directions for research. In: Martin SE, editor. Alcohol and interpersonal violence: Fostering multidisciplinary perspectives. Rockville, MD: U.S. Department of Health and Human Services; 1993. pp. 253–280. [Google Scholar]
- Leonard KE, Quigley BM. Drinking and marital aggression in newlyweds: An event-based analysis of drinking and the occurrence of husband marital aggression. Journal of Studies on Alcohol. 1999;60:537–545. doi: 10.15288/jsa.1999.60.537. [DOI] [PubMed] [Google Scholar]
- Loukas A, Fitzgerald HE, Zucker RA, von Eye A. Parental alcoholism and co-occurring antisocial behavior: Prospective relationships to externalizing behavior problems in their young sons. Journal of Abnormal Child Psychology. 2001;29:91–106. doi: 10.1023/a:1005281011838. [DOI] [PubMed] [Google Scholar]
- Lyons–Ruth K, Repacholi B, McLeod S, Silva E. Disorganized attachment behavior in infancy: Short-term stability, maternal and infant correlates, and risk-related subtypes. Development and Psychopathology. 1991;3:377–396. [Google Scholar]
- Main M, Solomon J. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. In: Greenberg MT, Cicchetti D, editors. Attachment in the preschool years: Theory, research, and intervention, The John D. and Catherine T MacArthur Foundation series on mental health and development. Chicago: University of Chicago Press; 1990. pp. 121–160. [Google Scholar]
- Mangelsdorf S, Gunnar M, Kestenbaum R, Lang S. Infant proneness-to-distress temperament, maternal personality, and mother–infant attachment: Associations and goodness of fit. Annual Progress in Child Psychiatry and Child Development. 1991:312–329. [PubMed] [Google Scholar]
- Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant–mother attachment: A meta-analytic investigation. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41:737–746. [PubMed] [Google Scholar]
- McNeal C, Amato PR. Parents’ marital violence: Long-term consequences for children. Journal of Family Issues. 1998;19:123–139. [Google Scholar]
- Mun EY, Fitzgerald HE, von Eye A, Puttler LI, Zucker RA. Temperament characteristics as predictors of externalizing and internalizing child behavior problems in the contexts of high and low parental psychopathology. Infant Mental Health Journal. 2001;22:393–415. [Google Scholar]
- Murphy CM, O’Farrell TJ. Marital violence among alcoholics. Current Directions in Psychological Science. 1996;5:183–186. [Google Scholar]
- Murray L, Cooper PJ. The role of infant and maternal factors in postpartum depression, mother–infant interactions, and infant outcomes. In: Murray L, Cooper PJ, editors. Postpartum depression and child development. New York: Guilford Press; 1997. pp. 111–135. [Google Scholar]
- Neighbors BD, Clark DB, Duncan B, Donovan JE, Brody GH. Difficult temperament, parental relationships, and adolescent alcohol use disorder symptoms. Journal of Child and Adolescent Substance Abuse. 2000;10:69–86. [Google Scholar]
- Noll RB, Zucker RA, Greenberg GS. Identification of alcohol by smell among preschoolers: Evidence for early socialization about drugs occurring in the home. Child Development. 1990;51:1520–1527. [PubMed] [Google Scholar]
- O’Connor MJ, Sigman M, Kasari C. Interactional model for the association among maternal alcohol use, mother–infant interaction, and infant cognitive development. Infant Behavior and Development. 1992;16:177–192. [Google Scholar]
- Pungello EP, Kupersmidt JB, Burchinal MR, Patterson CJ. Environmental risk factors and children’s achievement from middle childhood to early adolescence. Developmental Psychology. 1996;32:755–767. [Google Scholar]
- Quigley BM, Leonard KE. Alcohol and the continuation of early marital aggression. Alcoholism: Clinical and Experimental Research. 2000;24:1003–1010. [PubMed] [Google Scholar]
- Radke–Yarrow M, Cummings EM, Kuczynski L, Chapman M. Patterns of attachment in two-and three-year-olds in normal families and families with parental depression. Child Development. 1985;56:884–893. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roberts LJ, Leonard KE. Gender differences and similarities in the alcohol and marriage relationship. In: Wilsnack RW, Wilsnack SC, editors. Gender and alcohol: Individual and social perspectives. New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1997. pp. 289–311. [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Baldwin A, Baldwin C. Stability of intelligence from preschool to adolescence: The influence of social and family risk factors. Child Development. 1993;64:80–97. doi: 10.1111/j.1467-8624.1993.tb02896.x. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ, Seifer R, Elias PK. Sociocultural variability in infant temperament ratings. Child Development. 1982;53:164–173. [PubMed] [Google Scholar]
- Seifer R. Perils and pitfalls of high-risk research. Developmental Psychology. 1995;31:420–424. [Google Scholar]
- Shaw DS, Owens EB, Vondra JI, Keenan K. Early risk factors and pathways in the development of early disruptive behavior problems. Development and Psychopathology. 1996;8:679–699. [Google Scholar]
- Shaw DS, Vondra JI. Chronic family adversity and infant attachment security. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1993;34:1205–1215. doi: 10.1111/j.1469-7610.1993.tb01783.x. [DOI] [PubMed] [Google Scholar]
- Snyder JJ, Huntley D. Troubled families and troubled youth: The development of antisocial behavior and depression in children. In: Leone PE, editor. Understanding troubled and troubling youth. Newbury Park, CA: Sage; 1991. pp. 194–225. [Google Scholar]
- Spaccarelli S, Sandler IN, Roosa M. History of spouse violence against mother: Correlated risks and unique effects in child mental health. Journal of Family Violence. 1994;9:79–98. [Google Scholar]
- Sroufe LA, Carlson E, Shulman S. Individuals in relationships: Development from infancy through adolescence. In: Funder DC, Parke RD, editors. Studying lives through time: Personality and development. APA science volumes. Washington, DC: American Psychological Association; 1993. pp. 315–342. [Google Scholar]
- Steinglass P. The alcoholic family. New York: Basic Books; 1987. [Google Scholar]
- Straus MA. Measuring intra family conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Susman–Stillman A, Kalkose M, Egeland B, Waldman I. Infant temperament and maternal sensitivity as predictors of attachment security. Infant Behavior and Development. 1996;19:33–47. [Google Scholar]
- Tarter RE, Alterman AI, Edwards KL. Vulnerability to alcoholism in men: A behavior-genetic perspective. Journal of Studies on Alcohol. 1985;46:329–356. doi: 10.15288/jsa.1985.46.329. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM, Messinger DS, Isabella RA. Maternal depression and the quality of early attachment: An examination of infants, preschoolers, and their mothers. Developmental Psychology. 1995;31:364–376. [Google Scholar]
- Thompson RA. Sensitivity and security: New questions to ponder. Child Development. 1997;68:595–597. [Google Scholar]
- Urban J, Carlson E, Egeland B, Sroufe LA. Patterns of individual adaptation across childhood. Development and Psychopathology. 1991;3:445–460. [Google Scholar]
- van den Bloom DC, Hoeksma JB. The effect of infant irritability on mother–infant interaction: A growth-curve analysis. Developmental Psychology. 1994;30:581–590. [Google Scholar]
- van Ijzendoorn MH, De Wolff M. In search of the absent father—Meta-analysis of infant–father attachment: A rejoinder to our discussants. Child Development. 1997;68:604–609. [PubMed] [Google Scholar]
- Vaughn BE, Bradley CF, Joffe LS, Seiffer R, Waters E. Maternal characteristics measured prenatally are predictive of ratings of temperamental “difficulty” on the Carey Infant Temperament Questionnaire. Developmental Psychology. 1987;23:152–161. [Google Scholar]
- Vaughn BE, Taraldson BJ, Crichton L, Egeland B. The assessment of infant temperament: A critique of the Carey Infant Temperament Questionnaire. Infant Behavior and Development. 1981;4:1–17. [Google Scholar]
- West MO, Prinz RJ. Parental alcoholism and childhood psychopathology. Psychological Bulletin. 1987;102:204–218. [PubMed] [Google Scholar]
- Wilsnack SC, Wilsnack RW. Drinking and problem drinking in US women: Patterns and recent trends. In: Galanter M, et al., editors. Recent developments in alcoholism: Vol. 12. Alcoholism and women. New York: Plenum Press; 1995. pp. 381–443. [DOI] [PubMed] [Google Scholar]
- Windle M. Salient issues in the development of alcohol abuse in adolescence. Alcohol and Alcoholism. 1991;1:499–504. [PubMed] [Google Scholar]
- Wong MM, Zucker RA, Puttler LI, Fitzgerald HE. Heterogeneity of risk aggregation for alcohol problems between early and middle childhood: Nesting structure variations. Development and Psychopathology. 1999;11:727–744. doi: 10.1017/s0954579499002291. [DOI] [PubMed] [Google Scholar]
- Zeanah CH, Boris NW, Larrieu JA. Infant development and developmental risk: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:165–178. doi: 10.1097/00004583-199702000-00007. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Ellis LA, Bingham CR, Fitzgerald HE. The development of alcoholic subtypes: Risk variation among alcoholic families during the early childhood years. Alcohol Health and Research World. 1996;20:46–55. [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Fitzgerald HE. Early developmental factors and risk for alcohol problems. Alcohol Health and Research World. 1991;15:18–24. [Google Scholar]
- Zucker RA, Fitzgerald H, Moses HD. Emergence of alcohol problems and the several alcoholisms: A developmental perspective on etiologic theory and life course trajectory. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Risk, disorder, and adaptation. New York: Wiley; 1995. [Google Scholar]
- Zucker RA, Noll RB. The Antisocial Behavior Checklist. 1980. Unpublished manuscript. [Google Scholar]