Abstract
Studies of animal models have demonstrated that abnormal visual experience can lead to abnormal visual development. The provision of normal optical experience for human infants and children requires an understanding of their typical retinal image quality in the natural dynamic environment. The literature related to this topic is reviewed.
Keywords: infant, accommodation, retinal image quality, visual experience, aberrations, emmetropization
A large literature now suggests that abnormal visual experience leads to abnormal visual development in animal models. Visual experience can influence both the refinement of synapses in visual cortex1, 2 and the growth of the eye3–5. The manipulations of visual experience used in these experiments cannot be implemented in studies of human development and therefore direct evidence of the impact of abnormal visual experience on otherwise typically-developing infants and young children is much harder to gather. Infants receiving abnormal experience are typically only identified if the cause is detected easily (e.g. ptosis, cataract or strabismus6–9). We have only minimal evidence from humans regarding the natural history of other conditions, such as anisometropic amblyopia 10, 11, where the signs of abnormal experience are less obvious. As a result, approaches to prescribing spectacles for apparently asymptomatic infants and young children have primarily been derived from a combination of clinical consensus12, 13, the typical distribution of refractive errors during infancy and early childhoode.g.14, and the refractive error found at the diagnosis of an apparent consequence (e.g. amblyopia)15, 16. The goal of this perspective is to review our current understanding of the retinal visual experience of human infants and young children, and to pose questions that need to be answered if we are to promote normal visual development by providing ‘normal’ visual experience to young patients.
Much public effort in research, screening and healthcare is currently aimed at detecting and treating the apparent consequences of abnormal visual experience – primarily amblyopia and some forms of strabismus17–20. However, studies of form-deprivation and chronic defocus in animal models suggest it may instead be possible to prevent these consequences in humans with appropriate intervention at an earlier point. In attempts to explore this possibility and provide normal visual experience there have been three large-scale human population studies of randomized spectacle correction for hyperopia in infancy, with differing outcomes. These studies have suggested that it may be possible to reduce the prevalence of amblyopia at age three or four years with preventative use of spectacles21–23, but the results with regard to the incidence of strabismus are not consistent. Ingram’s group, who included infants aged 6 months with 4D of hyperopia or more in any one meridian, corrected one group with 2D less than their cycloplegic refraction and left another group untreated. They found that the prevalence of strabismus at age 3.5 years was the same in the treated and untreated groups (24% with treatment and 26% with no treatment)21. Atkinson’s group, however, found there was a reduction in the prevalence of strabismus in the treated group in their first programme, in which infants of six to eight months of age with more than 3.5 D of hyperopia in any meridian were randomized to glasses or no treatment (the initial spectacle corrections consisted of 1D less than the least hyperopic meridian, plus approximately half of the astigmatic correction). The prevalence of strabismus at four years was 6.3% in the group that were prescribed glasses and 21% in the untreated group22. The prevalence of strabismus was not significantly different in the two groups in their second programme however (20% of the treated group and 11% of the untreated group)23, which compared spectacle-treated and untreated hyperopes who had undergone uncyclopleged videorefraction screening at around 8 months of age and then cycloplegic retinoscopy follow-up (the prescribing approach was the same as used in the first programme, although the criterion for hyperopia was 4D or greater in any meridian). Abrahamsson and Sjostrand24 also assessed the success of preventative spectacle correction for a single group of anisometropes. They provided full anisometropic correction at two to three years of age to infants who had been found to have anisometropia of between 3 and 5.5D at 1 year. These children were found to have mixed outcomes at 10 years of age even with the correction and equal reported compliance. Some of the subjects lost their anisometropia while others retained it, and some of the subjects developed amblyopia and strabismus while others did not. Overall, while confirming that high refractive error is a risk factor for further abnormal visual development, these trials of prevention have been somewhat inconclusive.
If we are to make progress in understanding the parallels between experience-dependent development in animal models and clinical management of visual development for children it appears that we need to better define and quantify the parameters of ‘abnormal’ visual experience in humans. Without this understanding, we cannot clearly identify the children who are destined for abnormality and then target them for future large-scale tests of preventative intervention.
In an attempt to understand abnormal visual experience, we would first like to characterize our understanding of normal visual experience.
Quantifying Visual Experience Using Retinal Image Quality
It is not currently possible to measure visual experience at the critical pre-synaptic inputs in plastic visual cortex or at the final step in the pathway controlling eye growth, but it is possible and logical to quantify visual experience at the start of neural processing common to both pathways, the retinal image. It is the retinal image that would be manipulated with any form of preventative optical correction.
The quality of the image formed on the retina depends on the optical properties of the eye, eye size, and the neural control of accommodation. In the adult eye, higher order aberrations and chromatic aberration have been shown to reduce image quality of an optimally focused eye25–27. The impact of accommodation therefore depends on the relative importance of defocus compared with the other optical properties of the eye in disrupting the immature retinal image.
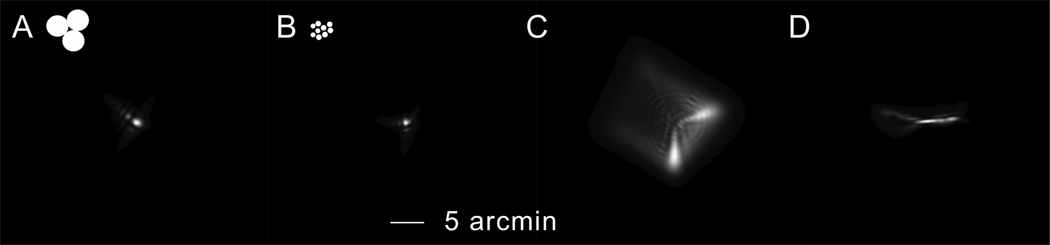
A fundus examination of even a premature infant suggests that the optical quality of the newborn eye is relatively good. The major landmarks, the vascular system and optic nerve head, are easily visible with only a correction for defocus. This qualitative impression has been confirmed by careful study of the transmission properties28 and aberrations (both higher-order monochromatic29 and chromatic30) of the young eye (see also31). The data suggest that these combined aberrations are within a factor of two of those of an adult within weeks after birth, as illustrated in Figure 1, and are close to predictions based on relatively simple optical models of infant and adult eyes29, 32. Figure 1 simulates the combined effects of higher-order monochromatic aberrations, chromatic aberration and diffraction on the retinal image of a point source for an infant of approximately 2 months of age (Panel A) and an adult (Panel B)27. The circles at the top of the images illustrate the size of the foveal photoreceptor inner segments in each case33, 34 and therefore the scale at which these images are sampled. Although the infant point spread function (PSF) in panel A is comparable in angular size to the adult version in panel B, the infant PSF would extend over fewer photoreceptors and be sampled more coarsely.
Figure 1.
Retinal images of point light sources (PSFs) simulating the combined effects of diffraction from the pupil, longitudinal chromatic aberration30 and higher order monochromatic aberrations (3rd to 6th order Zernike polynomials)29. The effect of longitudinal chromatic aberration was calculated every 10 nm, for wavelengths from 400 to 700nm, including the effect of Vλ and assuming 555 nm is in focus on the retina. The PSFs were then summed to demonstrate the size of the white light PSF, but not the chromatic content. The age appropriate photoreceptor inner segment diameters are illustrated in the top left corner of panels A and B, to demonstrate the spacing at which the PSF would be neurally sampled (neonate = 2.6 arcmin33, 34 & adult = 0.49 arcmin68). PANEL A: a young infant with a pupil size of 3mm29 (average monochromatic aberrations of a six-week-old & average chromatic aberration of a three-month-old). PANEL B: an adult with a pupil size of 4.5mm29. PANEL C: the infant with an additional 2D of hyperopic defocus. PANEL D: the infant with 0.5D of astigmatism and one meridian in focus. At three months of age, approximately 50% of infants have more than 0.75 D of astigmatism69 and therefore it has the potential to disrupt the retinal image in significant cases.
These aberrations have a small effect (equal to less than a diopter of equivalent defocus based on Figure 1) relative to the typical amounts of hyperopia at birth (the population mean is around +2D with a standard deviation of approximately 2D14, 35). Thus defocus and, if present, astigmatism logically become significant factors in infants’ retinal image quality. This is illustrated in Figure 1, panels C and D, where the mean value of 2 D of hyperopic defocus has been added to the infant PSF in panel C and 0.5D of astigmatism has been added in panel D. In turn, therefore, the control of retinal defocus by accommodation becomes a central factor in retinal image quality and postnatal visual experience. This is discussed in the following section.
The Role of Accommodation in Postnatal Visual Experience
Infants’ ability to eliminate defocus with accommodation has been studied by a number of groups, primarily since the mid 1960’s36–42. The consensus from these studies of accommodative accuracy to static targets as a function of viewing distance is that infants less than approximately 3 months of age tend to over-accommodate for distant objects and exhibit a low accommodative response function gain. At around three months, however, their gain increases and the mean population accuracy as measured with retinoscopy is around half a diopter of error (e.g. Banks38, Figure 5), which is similar to the accuracy of young adults as reviewed by Ciuffreda43.
Habitual visual experience in a dynamic environment also depends on the dynamics of accommodation. Delayed or slow velocity responses would lead to poor tracking of stimuli and additional retinal defocus. The first evidence regarding the dynamics of infants’ responses to step stimuli was provided by Howland, Dobson & Sayles40. In their Figure 5 they present data from a 4.5-month-old and a 9-month-old as they change fixation between targets at 1m and 25cm. In both cases the infants make rapid accommodative responses lasting approximately one second, after a latency of less than a second. We have recently examined infants’ ability to track moving stimuli and the latency after which they can initiate a response44, 45. We found that by the earliest age tested, 8 weeks, many infants can track accommodative stimuli moving at velocities between 50 and 5 cm/s at viewing distances of less than a meter, and initiate a response after less than a second. This compares well with typical adult responses and latencies of 300 to 400 ms46–48. We have also studied the stability of infants’ steady-state responses to static targets49. Adults exhibit microfluctuations of accommodation50 with an RMS on the order of 0.1 to 0.2 D and a temporal power spectrum containing most of the energy at lower temporal frequencies, below 3 Hz. Infants of eight to thirty weeks of age also exhibited microfluctuations. They had an RMS three to four times greater than the adults, but a power spectrum with a similar shape49.
In combination this literature suggests that most typical infants are not experiencing chronic bilateral retinal defocus equivalent to their isometropic hyperopic refractive error, and that they are in fact accommodating with an almost adult-like accuracy within the first months after birth. Thus normal postnatal visual experience is likely to consist of a relatively well-focused retinal image for a large proportion of an infant’s waking hours. Although this is consistent with the theoretical requirements for normal activity-dependent synaptic refinement in visual cortex, it suggests that any activity-dependent signal for emmetropization is more subtle than simple retinal defocus equal to the current refractive error. Thus, while the animal models of refractive development incorporating chronic anisometropic defocus may be an appropriate model for human anisometropia during infancy51, they are unlikely to reflect the retinal experience of a relatively symmetric bilateral hyperope who emmetropises during the first years after birth14, 52–54. How might retinal visual experience be influencing emmetropization in typical hyperopic human infants?
Emmetropization in Human Infants
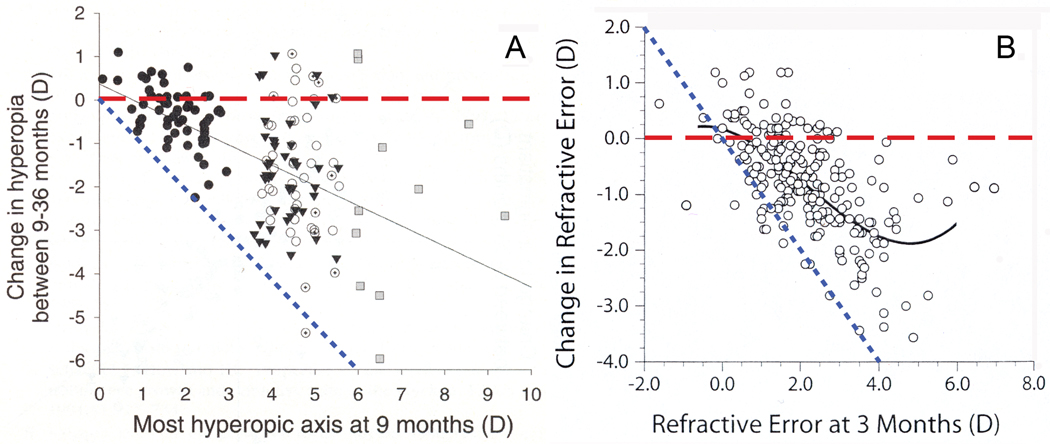
In thinking about human emmetropization, there are currently data available from two large-scale prospective studies. A graph based on Figure 4 from Atkinson’s study described above53 is shown here in Figure 2, panel A. The graph plots change in cycloplegic hyperopia between 9 and 36 months of age as a function of the amount of hyperopia in the most hyperopic axis at 9 months of age. A similar graph based on Figure 2, panel A from the BIBS study54 is shown here in Figure 2, panel B. This graph plots change in cycloplegic refractive error between three and nine months of age for infants with no optical correction, as a function of refractive error at three months. The dashed lines have been added to each graph. In both cases the horizontal line represents the prediction if the infants showed no change in refractive error over the study period, no emmetropization, and the lines of slope −1 illustrate the prediction if the infants fully compensated for their initial refractive error, full emmetropization. The trend in the variance in both data sets is for increasing variance with increase in baseline refractive error. This suggests that the infants fall fairly evenly between the two predictions and that infants with equal initial refractive errors undergo different proportions of emmetropization. In other words, the initial refractive error may be predictive of the dioptric range of changes in refractive error (anything between approximately zero and approximately 100% compensation for initial hyperopia), rather than the exact value represented by the mean. This additional alternative interpretation of the data was not discussed in either study.
Figure 2.
Data from two studies of emmetropization during infancy. PANEL A presents the data of Atkinson, et al53. The filled triangles were hyperopes who did not wear glasses, the open circles were hyperopes who were compliant with glasses, the circles with crosses in them are the hyperopes who were not compliant with their glasses and the squares were high hyperopes excluded from the spectacle trial. The filled circles are the control group of low hyperopes. PANEL B presents the data of Mutti et al54, from uncorrected infants whose refractions were measured at three and nine months of age. The added horizontal dashed lines demonstrate the prediction for no change in refractive error over time, and the added dotted lines represent the prediction for full emmetropization for the initial refractive error. A color version of this figure is available online at www.optvissci.com.
Why might some infants emmetropise fully and others not? Family history appears to play a role in the development of refractive or accommodative strabismus with hyperopia 55–57, but we have very little evidence to help make concrete predictions regarding emmetropization for individuals. The only prospective evidence relating accommodation, emmetropization and strabismus in human infants also suggests that bilaterally hyperopic human infants do not replicate the animal models of emmetropization58. Ingram, Gill and Goldacre58 found that infants who accommodate well to eliminate their retinal defocus were the ones who emmetropised and developed normally. Those who did not accommodate well and presumably experienced chronic defocus did not emmetropise.
Summary
If normal visual experience in the infant retinal image incorporates close to adult-like aberrations and accommodative accuracy within months after birth and leads to both normal cortical development and emmetropization, it appears that defining and detecting abnormal visual experience for symmetric refractions will be more complicated than measuring refractive error. Typical spherical refractive errors during infancy are greater than habitual accommodative errors and therefore an estimate of accommodative accuracy would be central to understanding habitual visual experience59. Which aspect or aspects of accommodative performance could be relevant? There is now evidence to suggest that the temporal structure of visual experience impacts development60–64. Perhaps we also need to study how well accommodation can be sustained? The peripheral retina is also now implicated in refractive error development65–67. Should we be studying peripheral refractions during accommodation? Is astigmatism an important factor in accommodative accuracy40? It appears that there are significant questions to be answered before we can define exactly what we mean by abnormal visual experience in human infants and children and before we can generate evidence-based guidelines for any preventative spectacle correction that will encourage both emmetropization and optimal cortical development.
ACKNOWLEDGMENTS
We thank Larry Thibos for the use of his simulation software and Arthur Bradley for helpful discussion. This project was supported by the National Eye Institute (EY 014460 awarded to TRC).
REFERENCES
- 1.Mitchell DE, Timney B. Postnatal development of function in the mammalian visual system. In: Darian-Smith I, editor. Handbook of Physiology. Section 1: The Nervous System, Vol. 3, Part 1: Sensory Processes. Baltimore, MD: Williams & Wilkins; 1984. pp. 507–555. [Google Scholar]
- 2.Kiorpes L, Kiper DC, O'Keefe LP, Cavanaugh JR, Movshon JA. Neuronal correlates of amblyopia in the visual cortex of macaque monkeys with experimental strabismus and anisometropia. J Neurosci. 1998;18:6411–6424. doi: 10.1523/JNEUROSCI.18-16-06411.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Troilo D. Neonatal eye growth and emmetropisation—a literature review. Eye. 1992;6:154–160. doi: 10.1038/eye.1992.31. [DOI] [PubMed] [Google Scholar]
- 4.Smith EL., 3rd . Environmentally induced refractive errors in animals. In: Rosenfield M, Gilmartin B, editors. Myopia and Nearwork. Oxford: Butterworth-Heinemann; 2004. pp. 57–90. [Google Scholar]
- 5.Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron. 2004;43:447–468. doi: 10.1016/j.neuron.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Rabin J, Van Sluyters RC, Malach R. Emmetropization: a vision-dependent phenomenon. Invest Ophthalmol Vis Sci. 1981;20:561–564. [PubMed] [Google Scholar]
- 7.Birch EE, Stager D, Leffler J, Weakley D. Early treatment of congenital unilateral cataract minimizes unequal competition. Invest Ophthalmol Vis Sci. 1998;39:1560–1566. [PubMed] [Google Scholar]
- 8.Maurer D, Mondloch CJ, Lewis TL. Effects of early visual deprivation on perceptual and cognitive development. Prog Brain Res. 2007;164:87–104. doi: 10.1016/S0079-6123(07)64005-9. [DOI] [PubMed] [Google Scholar]
- 9.Birch EE, Stager DR. Monocular acuity and stereopsis in infantile esotropia. Invest Ophthalmol Vis Sci. 1985;26:1624–1630. [PubMed] [Google Scholar]
- 10.Fielder AR, Moseley MJ. Anisometropia and amblyopia—chicken or egg? Br J Ophthalmol. 1996;80:857–858. doi: 10.1136/bjo.80.10.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lempert P. The axial length/disc area ratio in anisometropic hyperopic amblyopia: a hypothesis for decreased unilateral vision associated with hyperopic anisometropia. Ophthalmology. 2004;111:304–308. doi: 10.1016/j.ophtha.2003.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Miller JM, Harvey EM. Spectacle prescribing recommendations of AAPOS members. J Pediatr Ophthalmol Strabismus. 1998;35:51–52. doi: 10.3928/0191-3913-19980101-17. [DOI] [PubMed] [Google Scholar]
- 13.Lyons SA, Jones LA, Walline JJ, Bartolone AG, Carlson NB, Kattouf V, Harris M, Moore B, Mutti DO, Twelker JD. A survey of clinical prescribing philosophies for hyperopia. Optom Vis Sci. 2004;81:233–237. doi: 10.1097/00006324-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Mayer DL, Hansen RM, Moore BD, Kim S, Fulton AB. Cycloplegic refractions in healthy children aged 1 through 48 months. Arch Ophthalmol. 2001;119:1625–1628. doi: 10.1001/archopht.119.11.1625. [DOI] [PubMed] [Google Scholar]
- 15.Cotter SA. Management of childhood hyperopia: a pediatric optometrist's perspective. Optom Vis Sci. 2007;84:103–109. doi: 10.1097/OPX.0b013e318031b08a. [DOI] [PubMed] [Google Scholar]
- 16.Donahue SP. Prescribing spectacles in children: a pediatric ophthalmologist's approach. Optom Vis Sci. 2007;84:110–114. doi: 10.1097/OPX.0b013e318031b09b. [DOI] [PubMed] [Google Scholar]
- 17.Simons K. Amblyopia characterization, treatment, and prophylaxis. Surv Ophthalmol. 2005;50:123–166. doi: 10.1016/j.survophthal.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Ying GS, Kulp MT, Maguire M, Ciner E, Cyert L, Schmidt P. Vision in Preschoolers Study G. Sensitivity of screening tests for detecting vision in preschoolers-targeted vision disorders when specificity is 94%. The Vision in Preschoolers (VIP) Study Group. Optom Vis Sci. 2005;82:432–438. doi: 10.1097/01.opx.0000162660.14378.30. [DOI] [PubMed] [Google Scholar]
- 19.The Vision in Preschoolers Study Group. Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest Ophthalmol Vis Sci. 2005;46:2639–2648. doi: 10.1167/iovs.05-0141. [DOI] [PubMed] [Google Scholar]
- 20.Arnold RW, Donahue SP. The yield and challenges of charitable state-wide photoscreening. Binocul Vis Strabismus Q. 2006;21:93–100. [PubMed] [Google Scholar]
- 21.Ingram RM, Arnold PE, Dally S, Lucas J. Results of a randomised trial of treating abnormal hypermetropia from the age of 6 months. Br J Ophthalmol. 1990;74:158–159. doi: 10.1136/bjo.74.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atkinson J. Infant vision screening: prediction and prevention of strabismus and amblyopia from refractive screening in the Cambridge Photorefraction Program. In: Simons K, editor. Early Visual Development, Normal and Abnormal. New York: Oxford University Press; 1993. pp. 335–348. [Google Scholar]
- 23.Anker S, Atkinson J, Braddick O, Nardini M, Ehrlich D. Non-cycloplegic refractive screening can identify infants whose visual outcome at 4 years is improved by spectacle correction. Strabismus. 2004;12:227–245. doi: 10.1080/09273970490517935. [DOI] [PubMed] [Google Scholar]
- 24.Abrahamsson M, Sjostrand J. Natural history of infantile anisometropia. Br J Ophthalmol. 1996;80:860–863. doi: 10.1136/bjo.80.10.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thibos LN, Bradley A, Zhang XX. Effect of ocular chromatic aberration on monocular visual performance. Optom Vis Sci. 1991;68:599–607. doi: 10.1097/00006324-199108000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction between aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003;29:1487–1495. doi: 10.1016/s0886-3350(03)00334-1. [DOI] [PubMed] [Google Scholar]
- 27.Ravikumar S, Thibos LN, Bradley A. Calculation of retinal image quality for polychromatic light. J Opt Soc Am (A) 2008;25:2395–2407. doi: 10.1364/josaa.25.002395. [DOI] [PubMed] [Google Scholar]
- 28.Boettner EA, Wolter JR. Transmission of the ocular media. Investigative Opthamology. 1962;1:776–783. [Google Scholar]
- 29.Wang J, Candy TR. Higher order monochromatic aberrations of the human infant eye. J Vis. 2005;5:543–555. doi: 10.1167/5.6.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang J, Candy TR, Teel DF, Jacobs RJ. Longitudinal chromatic aberration of the human infant eye. J Opt Soc Am (A) 2008;25:2263–2270. doi: 10.1364/josaa.25.002263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Candy TR, Banks MS. Use of an early nonlinearity to measure optical and receptor resolution in the human infant. Vision Res. 1999;39:3386–3398. doi: 10.1016/s0042-6989(99)00035-8. [DOI] [PubMed] [Google Scholar]
- 32.Howland HC. Allometry and scaling of wave aberration of eyes. Vision Res. 2005;45:1091–1093. doi: 10.1016/j.visres.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 33.Hendrickson A, Drucker D. The development of parafoveal and mid-peripheral human retina. Behav Brain Res. 1992;49:21–31. doi: 10.1016/s0166-4328(05)80191-3. [DOI] [PubMed] [Google Scholar]
- 34.Candy TR, Crowell JA, Banks MS. Optical, receptoral, and retinal constraints on foveal and peripheral vision in the human neonate. Vision Res. 1998;38:3857–3870. doi: 10.1016/s0042-6989(98)00080-7. [DOI] [PubMed] [Google Scholar]
- 35.Cook RC, Glasscock RE. Refractive and ocular findings in the newborn. Am J Ophthalmol. 1951;34:1407–1413. doi: 10.1016/0002-9394(51)90481-3. [DOI] [PubMed] [Google Scholar]
- 36.Haynes H, White BL, Held R. Visual accommodation in human infants. Science. 1965;148:528–530. doi: 10.1126/science.148.3669.528. [DOI] [PubMed] [Google Scholar]
- 37.Braddick O, Atkinson J, French J, Howland HC. A photorefractive study of infant accommodation. Vision Res. 1979;19:1319–1330. doi: 10.1016/0042-6989(79)90204-9. [DOI] [PubMed] [Google Scholar]
- 38.Banks MS. The development of visual accommodation during early infancy. Child Dev. 1980;51:646–666. [PubMed] [Google Scholar]
- 39.Brookman KE. Ocular accommodation in human infants. Am J Optom Physiol Opt. 1983;60:91–99. doi: 10.1097/00006324-198302000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Howland HC, Dobson V, Sayles N. Accommodation in infants as measured by photorefraction. Vision Res. 1987;27:2141–2152. doi: 10.1016/0042-6989(87)90128-3. [DOI] [PubMed] [Google Scholar]
- 41.Hainline L, Riddell P, Grose-Fifer J, Abramov I. Development of accommodation and convergence in infancy. Behav Brain Res. 1992;49:33–50. doi: 10.1016/s0166-4328(05)80192-5. [DOI] [PubMed] [Google Scholar]
- 42.Currie DC, Manny RE. The development of accommodation. Vision Res. 1997;37:1525–1533. doi: 10.1016/s0042-6989(97)85022-5. [DOI] [PubMed] [Google Scholar]
- 43.Ciuffreda KJ, The Glenn A. Fry invited lecture. Accommodation to gratings and more naturalistic stimuli. Optom Vis Sci. 1991;68:243–260. doi: 10.1097/00006324-199104000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Tondel GM, Candy TR. Human infants' accommodation responses to dynamic stimuli. Invest Ophthalmol Vis Sci. 2007;48:949–956. doi: 10.1167/iovs.06-0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tondel GM, Candy TR. Accommodation and vergence latencies in human infants. Vision Res. 2008;48:564–576. doi: 10.1016/j.visres.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Campbell FW, Westheimer G. Dynamics of accommodation responses of the human eye. J Physiol. 1960;151:285–295. doi: 10.1113/jphysiol.1960.sp006438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Phillips S, Shirachi D, Stark L. Analysis of accommodative response times using histogram information. Am J Optom Arch Am Acad Optom. 1972;49:389–400. doi: 10.1097/00006324-197205000-00001. [DOI] [PubMed] [Google Scholar]
- 48.Heron G, Charman WN, Schor CM. Age changes in the interactions between the accommodation and vergence systems. Optom Vis Sci. 2001;78:754–762. doi: 10.1097/00006324-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 49.Candy TR, Bharadwaj SR. The stability of steady state accommodation in human infants. J Vis. 2007;7:1–16. doi: 10.1167/7.11.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Charman WN, Heron G. Fluctuations in accommodation: a review. Ophthalmic Physiol Opt. 1988;8:153–164. doi: 10.1111/j.1475-1313.1988.tb01031.x. [DOI] [PubMed] [Google Scholar]
- 51.Almeder LM, Peck LB, Howland HC. Prevalence of anisometropia in volunteer laboratory and school screening populations. Invest Ophthalmol Vis Sci. 1990;31:2448–2455. [PubMed] [Google Scholar]
- 52.Saunders KJ, Woodhouse JM, Westall CA. Emmetropisation in human infancy: rate of change is related to initial refractive error. Vision Res. 1995;35:1325–1328. doi: 10.1016/0042-6989(94)00222-8. [DOI] [PubMed] [Google Scholar]
- 53.Atkinson J, Anker S, Bobier W, Braddick O, Durden K, Nardini M, Watson P. Normal emmetropization in infants with spectacle correction for hyperopia. Invest Ophthalmol Vis Sci. 2000;41:3726–3731. [PubMed] [Google Scholar]
- 54.Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, Moeschberger ML, Zadnik K. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest Ophthalmol Vis Sci. 2005;46:3074–3080. doi: 10.1167/iovs.04-1040. [DOI] [PubMed] [Google Scholar]
- 55.Abrahamsson M, Magnusson G, Sjostrand J. Inheritance of strabismus and the gain of using heredity to determine populations at risk of developing strabismus. Acta Ophthalmol Scand. 1999;77:653–657. doi: 10.1034/j.1600-0420.1999.770609.x. [DOI] [PubMed] [Google Scholar]
- 56.Ziakas NG, Woodruff G, Smith LK, Thompson JR. A study of heredity as a risk factor in strabismus. Eye. 2002;16:519–521. doi: 10.1038/sj.eye.6700138. [DOI] [PubMed] [Google Scholar]
- 57.Birch EE, Fawcett SL, Morale SE, Weakley DR, Jr, Wheaton DH. Risk factors for accommodative esotropia among hypermetropic children. Invest Ophthalmol Vis Sci. 2005;46:526–529. doi: 10.1167/iovs.04-0618. [DOI] [PubMed] [Google Scholar]
- 58.Ingram RM, Gill LE, Goldacre MJ. Emmetropisation and accommodation in hypermetropic children before they show signs of squint--a preliminary analysis. Bull Soc Belge Ophtalmol. 1994;253:41–56. [PubMed] [Google Scholar]
- 59.Hunter DG. Dynamic retinoscopy: the missing data. Surv Ophthalmol. 2001;46:269–274. doi: 10.1016/s0039-6257(01)00260-0. [DOI] [PubMed] [Google Scholar]
- 60.Winawer J, Wallman J. Temporal constraints on lens compensation in chicks. Vision Res. 2002;42:2651–2668. doi: 10.1016/s0042-6989(02)00300-0. [DOI] [PubMed] [Google Scholar]
- 61.Kee CS, Hung LF, Qiao-Grider Y, Ramamirtham R, Winawer J, Wallman J, Smith EL., 3rd Temporal constraints on experimental emmetropization in infant monkeys. Invest Ophthalmol Vis Sci. 2007;48:957–962. doi: 10.1167/iovs.06-0743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wensveen JM, Harwerth RS, Hung LF, Ramamirtham R, Kee CS, Smith EL., 3rd Brief daily periods of unrestricted vision can prevent form-deprivation amblyopia. Invest Ophthalmol Vis Sci. 2006;47:2468–2477. doi: 10.1167/iovs.05-0885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sakai E, Bi H, Maruko I, Zhang B, Zheng J, Wensveen J, Harwerth RS, Smith EL, 3rd, Chino YM. Cortical effects of brief daily periods of unrestricted vision during early monocular form deprivation. J Neurophysiol. 2006;95:2856–2865. doi: 10.1152/jn.01265.2005. [DOI] [PubMed] [Google Scholar]
- 64.Schwarzkopf DS, Vorobyov V, Mitchell DE, Sengpiel F. Brief daily binocular vision prevents monocular deprivation effects in visual cortex. Eur J Neurosci. 2007;25:270–280. doi: 10.1111/j.1460-9568.2006.05273.x. [DOI] [PubMed] [Google Scholar]
- 65.Nathan J, Kiely PM, Crewther SG, Crewther DP. Disease-associated visual image degradation and spherical refractive errors in children. Am J Optom Physiol Opt. 1985;62:680–688. doi: 10.1097/00006324-198510000-00003. [DOI] [PubMed] [Google Scholar]
- 66.Smith EL, 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–3972. doi: 10.1167/iovs.05-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith EL, 3rd, Ramamirtham R, Qiao-Grider Y, Hung LF, Huang J, Kee CS, Coats D, Paysse E. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48:3914–3922. doi: 10.1167/iovs.06-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Curcio CA. Diameters of presumed cone apertures in human retina. J Opt Soc Am (A) 1987;4:P70. [Google Scholar]
- 69.Saunders KJ. Early refractive development in humans. Surv Ophthalmol. 1995;40:207–216. doi: 10.1016/s0039-6257(95)80027-1. [DOI] [PubMed] [Google Scholar]