Abstract
Although heterogeneity in the timing and persistence of maternal depressive symptomatology has implications for screening and treatment as well as associated maternal and child health outcomes, little is known about this variability. A prospective observational study of 1,735 low-income, multiethnic, inner-city women recruited in pregnancy from 2000 to 2002 and followed prospectively until 2004 (1 prenatal and 3 postpartum interviews) was used to determine whether distinct trajectories of depressive symptomatology can be defined from pregnancy through 2 years postpartum. Analysis was carried out through general growth mixture modeling. A model with 5 trajectory classes characterized the heterogeneity seen in the timing and magnitude of depressive symptoms among the study participants from Philadelphia, Pennsylvania. These classes included the following: 1) always or chronic depressive symptomatology (7%); 2) antepartum only (6%); 3) postpartum, which resolves after the first year postpartum (9%); 4) late, present at 25 months postpartum (7%); and 5) never having depressive symptomatology (71%). Women in these trajectory classes differed in demographic (nativity, education, race, parity) health, health behavior, and psychosocial characteristics (ambivalence about pregnancy and high objective stress). This heterogeneity should be considered in maternal depression programs. Additional research is needed to determine the association of these trajectory classes with maternal and child health outcomes.
Keywords: depression, longitudinal studies, postpartum period, pregnant women
Depression is the largest single contributor to disability worldwide, and women face twice the lifetime risk of major depression as men (1). Depressive symptomatology, a risk factor for major depression and a wide range of negative behavioral and physical health outcomes, is elevated during pregnancy and the postpartum period and disproportionately affects low-income and minority populations (2–5). Depressive symptomatology in mothers is also associated with important maternal child outcomes including low birth weight, preterm birth, and poor parenting practices (6–11).
With few exceptions, the typical study examining the correlates and effects of depressive symptomatology is cross-sectional in design and leaves unaddressed questions of variation in the timing and overall exposure to symptoms (12). It is likely that the consequences of symptomatology vary by their chronicity, with transient episodes having less effect on outcomes. Available retrospective and longitudinal data indicate that there is significant heterogeneity in the timing of the onset and persistence of elevated depressive symptomatology (2, 4). Moving beyond simple observations of the negative outcomes associated with depressive symptoms in pregnancy and the postpartum period requires information about 2 related phenomena: 1) the identification of distinct subgroups of women in terms of onset and persistence of depressive symptoms, and 2) the identification of demographic and clinical correlates of these subgroups to aid in the development of more refined models of mechanisms linking depressive symptoms to behavioral and physical health outcomes.
In this study, we determined whether distinct subgroups of low-income women could be identified by the magnitude and timing of depressive symptomatology from the antepartum period through 2 years following delivery. We assessed whether women could be placed into 4 trajectory classes defined a priori and then determined whether solutions with fewer or more classes better characterized the depressive symptom trajectories (2, 4, 13). We identified trajectory classes of depressive symptoms from the prenatal to the postpartum periods with general growth mixture modeling (GMM). GMM allows for the clustering of individuals into homogeneous subgroups with different trajectories over time (14, 15). Additionally, we described how these subgroups differed in terms of demographic, socioeconomic, health, health behavior, and psychosocial characteristics that have been associated with depressive symptomatology in pregnancy and the postpartum period.
MATERIALS AND METHODS
Institutional review board approval was received from all participating institutions, including the Drexel University College of Medicine and the University of Pennsylvania.
Setting
The current study made use of data from women enrolled in a prospective observational cohort study of pregnancy, birth, and infant health outcomes among low-income, inner-city women in Philadelphia, Pennsylvania. Women from the parent study were included (n = 1,735) who completed at least 1 postpartum interview (Figure 1). The design of this study and enrollment procedures have been described elsewhere (11, 16, 17). Briefly, women were recruited to the study from public health centers from February 2000 through November 2002. Eligibility criteria included English- or Spanish-speaking ability and a singleton intrauterine pregnancy. After providing written consent, participants at their first prenatal care visit (mean gestational age, 15.1 weeks; standard deviation (SD), 7.1) completed the first of 4 face-to-face interviews. Interviews were conducted orally in English or Spanish by trained female interviewers using standardized questionnaires. The second, third, and fourth interviews were conducted in women's homes at approximately 3 months postpartum (mean, 3.6; SD, 1.8), 11 months postpartum (mean, 11.1; SD, 1.3), and 25 months postpartum (mean, 25.3; SD, 3.0), respectively. Two percent of the eligible women declined participation at enrollment. Greater than 85% (n = 1,735) of the eligible women experiencing a livebirth (73% of the total eligible women) completed at least 1 subsequent interview, and 48% of these women completed all 3 of the postpartum interviews.
Figure 1.
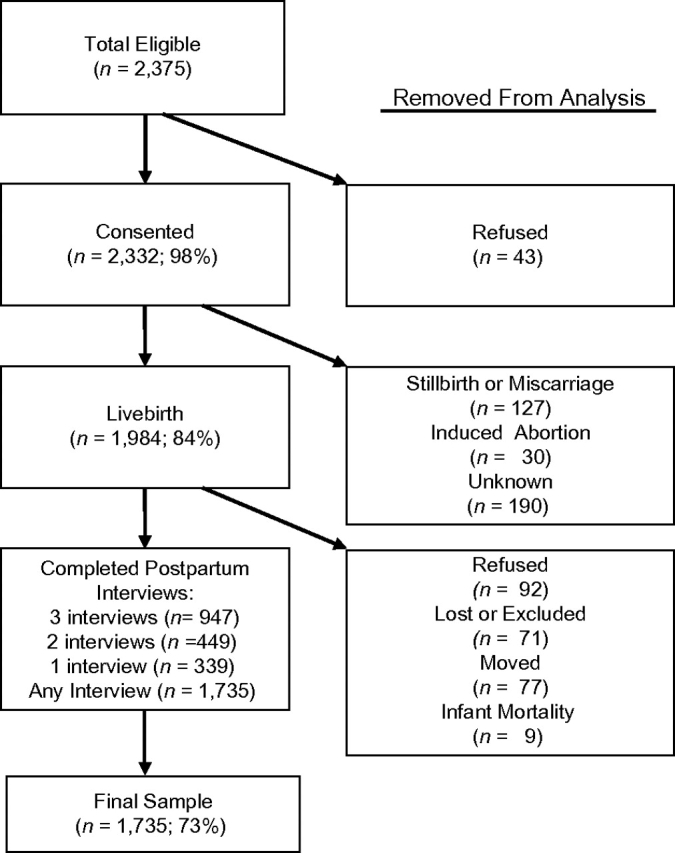
Enrollment and follow-up in study, Philadelphia, Pennsylvania, 2000–2004.
Measures
Depressive symptomatology.
Depressive symptomatology was measured utilizing the Center for Epidemiologic Studies Depression (CES-D) Scale, a 20-item instrument widely used to assess depressive symptomatology with scores ranging from 0 to 60 (18). The CES-D Scale is used in a range of populations including minority and low-income women and women in pregnancy and postpartum (9, 11, 17, 19). The scale can be used as a continuous variable with increasing levels of emotional distress represented by higher scores or as a categorical variable with standard cutpoints of ≥16 and ≥23 indicating significant levels of depressive symptomatology but with corresponding differences in sensitivity and specificity for major depressive disorder in community samples (18, 20, 21). Trajectory classes from the current study that crossed these cutpoints at any point were considered to be characterized by depressive symptomatology while varying in severity and/or timing. The mean score for general population samples is approximately 7–9, while those for inpatient and outpatient psychiatric patients are approximately 24–27 (21, 22).
Correlates of trajectory class membership.
Potential correlates of trajectory class membership were identified a priori through a review of the literature on depressive symptomatology in pregnancy and the postpartum period. The demographic and socioeconomic variables selected were age, income, nativity (US born), educational attainment, self-reported race/ethnicity, marital status, and parity (previous livebirths) (3, 23–29). To differentiate women still in school from those who will not complete school, we divided the “less than high school” completion category on the basis of age: 1) ≤19 years and potentially still in high school, and 2) >19 years and less than high school (since no longer eligible). Because women's physical health status is linked to depression in pregnancy and to parenting behaviors (3, 30), we measured health status by 2 items: 1) self-rated physical health over the previous 12 months, and 2) the report of any of the following chronic comorbid physical conditions: heart disease, hypertension, asthma, diabetes, and “other serious illness.” Self-rated physical health status was measured with a 5-point Likert scale ranging from poor to excellent. For these analyses, the lowest 2 categories were combined. As a past history of mood disturbance has been associated with depression in pregnancy and the postpartum period (30–32), we assessed emotional health status prior to pregnancy with a self-rated measure of mental health status in the past 12 months (the scale response ranged from poor to excellent). Self-rated assessments of physical and emotional health are strong predictors of objective measures of physical and emotional health (33). The negative health behaviors associated with depressive symptomatology and poor pregnancy and infant outcomes were smoking during pregnancy, alcohol use in the previous year, and marijuana use in the previous year (34–38).
Ambivalence regarding the timing of pregnancy has also been associated with perinatal mood disorders (39). We assessed this construct using responses to the question: “Many women have mixed feelings when they find out that they are pregnant. When you found out you were pregnant this time, did you feel ….” Response choices were “happy,” “sad,” “disappointed,” “worried,” and “scared” (responses were recorded as “yes” or “no”). Exploratory factor analysis indicated that these responses were better grouped into 2 factors than 1 factor (results available on request). The first factor, ambivalence toward the pregnancy with a depressed character, was characterized by responding “no” to the response option “happy” or “yes” to the options “sad” or “disappointed,” while the second factor, ambivalence with an anxious character, was characterized by answering “yes” to the response options “worried” or “scared.” The average factor loading for depressed items was 0.74 and for anxious items was 0.88. The correlation between the 2 factors was r = 0.68.
Both acute and chronic stressors are also related to depressive symptomatology in the perinatal period (40, 41). We assessed objective stress with a previously described scale (16). This 13-point scale is based on self-reported difficulties in 4 domains: 1) housing (0–3 points), 2) intimate partner violence (0–3 points), 3) material hardship (other than housing; 0–3 points), and 4) neighborhood danger (0–4 points). A 3-category variable based on tertiles of the distribution was used in the analysis: 1) low (≤2 points; lower third of sample), 2) moderate (3–4 points; middle third of sample), and 3) high (≥5 points; upper third of sample).
Statistical analysis
GMM was used to identify latent classes in the trajectory of depressive symptomatology from the prenatal to the postpartum periods (refer to the description below). Once these trajectory classes were identified, women were assigned to 1 and only 1 class on the basis of their highest estimated posterior probabilities. We then assessed bivariate associations between women's characteristics and the dependent variable representing trajectory class membership using the χ2 test and analysis of variance. We used multinomial regression to predict the effect of women's characteristics on the probability of belonging to a specific trajectory class compared with the never group (explanation below). Goodness of fit was assessed by the likelihood ratio test (χ2 statistic) comparing the full model with reduced or less restrictive models (i.e., decrements in fit after removing each covariate). Bivariate and multinomial regression analyses were carried out with SPSS, version 15.0, software (SPSS, Inc., Chicago, Illinois).
Identification of latent trajectories.
We used GMM to identify latent classes (14, 15). GMM uses a categorical latent variable to identify qualitatively different population subgroups (42). This categorical latent variable captures the heterogeneity in the trajectories of depressive symptoms of each class when compared with the overall population growth. Parameter estimates were obtained with maximum-likelihood estimation by using the expectation-maximization algorithm. Maximum-likelihood estimation with missing data assumed ignorable missing data (i.e., missing at random) (43). Analyses of all cases tend to yield less biased parameter estimates than analyses restricted to only those cases with complete data even when missing-at-random assumptions are not fully met (44).
Model selection.
We used statistical indices as well as the overall interpretability of the model to select the optimal model. Statistical criteria for model selection included the following: 1) reliability of the classifications via the estimated posterior probabilities of group membership for each individual and the average posterior probabilities for each group and entropy (range, 0–1); 2) information criteria fit indices such as Akaike's Information Criterion, the Bayesian Information Criterion, and the sample-size–adjusted Bayesian Information Criterion; and 3) the bootstrap likelihood ratio test or k versus k − 1 groups (45). A significant bootstrap likelihood ratio test for k groups (i.e., P < 0.05) indicates that the fit of the specified model is an improvement over a model with k − 1 groups. The substantive criteria included 1) group prevalence greater than 5% of the sample because smaller groups are difficult to replicate and 2) theoretical and practical interpretability of the groups. Specifically, we excluded models with k + 1 groups if the additional group did not provide substantive and/or unique information.
Analysis procedure.
The general growth mixture models were based on a basic latent growth model with a piecewise trajectory for continuous depressive symptomatology scores (CES-D Scale, 0–60). This model captured 2 phases of changes in depressive symptoms over the 4 time points. Accordingly, the first phase modeled the change from ante- to peripartum (from time 1 to time 2). The second phase modeled the change from 11 months to 24 months postpartum (from time 2 to time 4). This overall model had an excellent fit to the data (χ22 = 5.47, not significant; comparative fit index = 0.99; Tucker-Lewis fit index = 0.99; root mean squared error of approximation = 0.032, 90% confidence interval: 0.000, 0.065; and standardized root mean square residual = 0.011).
To determine the optimal number of groups, we first estimated the fit of the hypothesized 4-group model. Then we compared this solution against models ranging from 2 to 7 groups. The identification of groups was based on the mean of the growth factors alone. The variances for the first growth factor phase were constrained at 0 for all groups, and the variances across groups for the second growth factor were not allowed to differ from one another because freeing these parameters resulted in model nonconvergence. All GMM models were estimated by using Mplus, version 4.1, software (46).
RESULTS
Descriptive characteristics of the full study sample are shown as variables in Table 1. Overall, the sample consisted of young, low-income, US-born, black women with demographic, health, behavioral, and psychosocial characteristics consistent with those of a low-income urban population. The mean age was approximately 24 years, and the mean annual personal income was less than $9,000. Most women reported their race/ethnicity as African American (70%) with smaller groups of Latina (17%) and white/other (13%) women. Nearly 80% of the sample reported being US born. One-quarter of the women had less than high school educational status (>19 years of age), 15% did not have a diploma but were potentially still in school (≤19 years of age), 42% reported a high school diploma (or equivalency degree), and the remaining 18% had attended at least some college. For this relatively young sample, a high proportion reported only poor/fair physical health (12%) and emotional health status (18%) in the preceding year, as well as the presence of comorbid conditions (18%). In addition, the sample had a high prevalence of negative health behaviors. Twenty-three percent of the women reported smoking in pregnancy, 33% reported alcohol use, and 19% reported marijuana use in the previous year.
Table 1.
Characteristics of the Study Sample, Philadelphia, Pennsylvania, 2000–2004
| Variable | Total (n = 1,735) | Chronic (n = 114) | Antepartum (n = 110) | Postpartum (n = 162) | Late (n = 112) | Never (n = 1,237) | P Value | ||||||||||||
| No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | ||
| Demographic and socioeconomic characteristics | |||||||||||||||||||
| Age, years | 23.9 (5.9) | 24.0 (6.1) | 23.0 (5.5) | 23.8 (6.4) | 24.0 (6.1) | 23.9 (5.8) | 0.580 | ||||||||||||
| Income/year, $ | 8,131 (9,876) | 7,590 (10,081) | 8,054 (7,795) | 6,572 (6,730) | 8,647 (10,254) | 8,344 (10,313) | 0.277 | ||||||||||||
| Race | |||||||||||||||||||
| Hispanic | 297 | 17 | 28 | 25 | 10 | 9 | 21 | 14 | 24 | 21 | 214 | 18 | 0.020 | ||||||
| Black | 1,212 | 70 | 65 | 57 | 84 | 76 | 119 | 74 | 77 | 69 | 867 | 70 | |||||||
| White/other | 226 | 13 | 21 | 18 | 16 | 15 | 22 | 14 | 11 | 10 | 156 | 13 | |||||||
| Nativity—US born | 1,351 | 78 | 91 | 80 | 83 | 75 | 122 | 76 | 82 | 73 | 973 | 79 | 0.564 | ||||||
| Education | |||||||||||||||||||
| Less than high schoola | 426 | 25 | 43 | 38 | 21 | 19 | 50 | 31 | 44 | 39 | 268 | 22 | <0.001 | ||||||
| Still in high schoola | 265 | 15 | 19 | 7 | 21 | 19 | 35 | 22 | 18 | 16 | 172 | 14 | |||||||
| High school or equivalent | 730 | 42 | 39 | 34 | 48 | 44 | 57 | 35 | 37 | 33 | 549 | 44 | |||||||
| Any college or more | 312 | 18 | 13 | 11 | 19 | 17 | 20 | 12 | 13 | 12 | 247 | 20 | |||||||
| Married | 432 | 25 | 30 | 26 | 23 | 21 | 37 | 23 | 26 | 23 | 316 | 26 | 0.759 | ||||||
| Parity (previous livebirths) | |||||||||||||||||||
| ≥3 | 439 | 25 | 51 | 45 | 27 | 25 | 41 | 25 | 30 | 27 | 290 | 23 | 0.046 | ||||||
| 1–2 | 456 | 26 | 21 | 18 | 27 | 25 | 53 | 33 | 29 | 26 | 326 | 26 | |||||||
| 0 | 840 | 48 | 42 | 37 | 56 | 51 | 68 | 42 | 53 | 47 | 621 | 50 | |||||||
| Health measures | |||||||||||||||||||
| Self-rated physical health | |||||||||||||||||||
| Fair/poor | 201 | 12 | 27 | 24 | 15 | 14 | 20 | 12 | 12 | 11 | 127 | 10 | <0.001 | ||||||
| Good | 620 | 36 | 37 | 33 | 45 | 41 | 58 | 36 | 52 | 46 | 428 | 35 | |||||||
| Very good | 449 | 26 | 25 | 22 | 27 | 25 | 41 | 25 | 14 | 13 | 342 | 28 | |||||||
| Excellent | 463 | 27 | 25 | 22 | 22 | 20 | 43 | 27 | 34 | 30 | 339 | 27 | |||||||
| Self-rated emotional health | |||||||||||||||||||
| Fair/poor | 316 | 18 | 45 | 40 | 38 | 35 | 43 | 27 | 28 | 25 | 162 | 13 | <0.001 | ||||||
| Good | 570 | 33 | 36 | 32 | 40 | 36 | 51 | 32 | 31 | 28 | 412 | 33 | |||||||
| Very good | 449 | 26 | 19 | 17 | 17 | 16 | 43 | 27 | 28 | 25 | 342 | 28 | |||||||
| Excellent | 394 | 23 | 14 | 12 | 15 | 14 | 24 | 15 | 24 | 22 | 317 | 26 | |||||||
| Comorbid condition | 319 | 18 | 29 | 25 | 24 | 22 | 39 | 24 | 21 | 19 | 206 | 17 | 0.029 | ||||||
| Health behaviors | |||||||||||||||||||
| Smoked in pregnancy | 392 | 23 | 42 | 37 | 33 | 30 | 39 | 24 | 31 | 28 | 247 | 20 | <0.001 | ||||||
| Recent alcohol use | 570 | 33 | 55 | 48 | 50 | 46 | 48 | 30 | 31 | 28 | 386 | 31 | <0.001 | ||||||
| Recent marijuana use | 324 | 19 | 36 | 32 | 28 | 26 | 36 | 22 | 24 | 21 | 200 | 16 | <0.001 | ||||||
| Other measures | |||||||||||||||||||
| Ambivalence about pregnancy | |||||||||||||||||||
| Depressed | 774 | 45 | 67 | 59 | 72 | 67 | 80 | 49 | 41 | 37 | 514 | 42 | <0.001 | ||||||
| Anxious | 872 | 50 | 79 | 69 | 79 | 72 | 88 | 54 | 48 | 43 | 578 | 47 | <0.001 | ||||||
| Objective stress | |||||||||||||||||||
| High | 607 | 35 | 66 | 57 | 54 | 50 | 70 | 44 | 50 | 45 | 368 | 30 | <0.001 | ||||||
| Moderate | 592 | 34 | 36 | 32 | 31 | 27 | 59 | 37 | 42 | 38 | 424 | 35 | |||||||
| Low | 524 | 30 | 13 | 11 | 23 | 21 | 32 | 20 | 20 | 18 | 436 | 36 | |||||||
Abbreviation: SD, standard deviation.
“Less than high school” is defined as less than high school status and more than 19 years of age; “still in high school” is defined as less than high school status and 19 years of age or less.
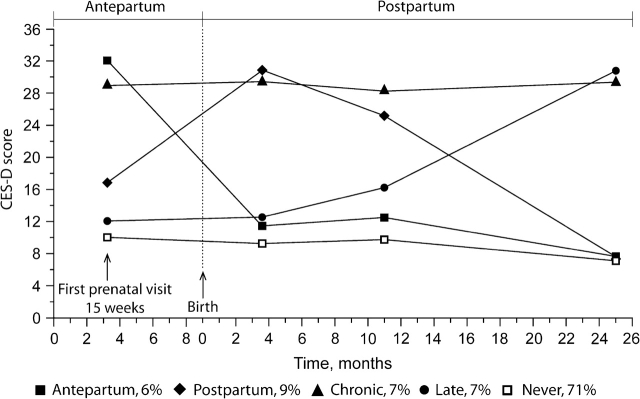
The fit of the depressive symptomatology trajectory models was tested from 2 to 7 trajectory classes. All goodness-of-fit statistics (Akaike's Information Criterion, Bayesian Information Criterion, sample-size–adjusted Bayesian Information Criterion, and bootstrap likelihood ratio test) became smaller with an increasing number of classes, indicating that solutions with more groups better fit the data (Table 2). The 7-group model, however, did not converge. The 6-group model yielded 1 small group (<5% of the sample) and did not improve the classification of subjects (i.e., entropy was identical to the 5-group solution). Additionally, the posterior average probability for one of the groups was not optimal (average probability = 0.66). The relaxation of assumptions such as equality of variance across trajectory groups did not improve the fit of the model (results available on request). On the basis of these empirical and substantive criteria, we chose the 5-group solution as the optimal solution. Our 5-group solution added a new group (group 4 below) to the initially hypothesized 4-group model. Thus, the following groups shown in Figure 2 were identified and labeled according to when the trajectory crossed the predetermined depressive symptom score cutpoint (CES-D score, ≥16): 1) chronic, persistently high level of depressive symptoms (7% of sample); 2) antepartum depressive symptomatology present only at the first prenatal visit (6% of sample); 3) postpartum depressive symptoms present within 6 weeks of delivery that subside over time (9% of sample); 4) late with low levels of depressive symptoms ante- and peripartum that increase in the second year postpartum (7% of sample); and 5) never elevated, with continuous low levels of depressive symptoms (71% of sample). The entropy of this model was high (entropy = 0.79), and the average posterior probability for the groups showing elevated symptomatology ranged between 0.78 and 0.84, while for the never-elevated group, it was 0.91.
Table 2.
Results From Growth Mixture Modeling Information Criteria, Philadelphia, Pennsylvania, 2000–2004
| Classes | No. of Parameters | Akaike Information Criterion | Bayesian Information Criterion | Bayesian Information Criteriona | Entropy | Log-Likelihood Test | P Valueb |
| 2 | 15 | 42,913.52 | 42,995.40 | 42,947.74 | 0.78 | −21,441.76 | 0.001 |
| 3 | 20 | 42,638.97 | 42,748.14 | 42,684.61 | 0.72 | −21,299.48 | 0.001 |
| 4 | 22 | 42,574.75 | 42,694.84 | 42,624.95 | 0.80 | −21,265.38 | 0.001 |
| 5 | 24 | 42,501.81 | 42,632.82 | 42,556.58 | 0.79 | −21,226.91 | 0.001 |
| 6 | 28 | 42,440.47 | 42,593.31 | 42,504.36 | 0.78 | −21,192.23 | 0.001 |
Sample size adjusted.
Probability by parametric bootstrapped likelihood ratio test.
Figure 2.
Five group trajectories of depressive symptomatology in pregnancy and postpartum, Philadelphia, Pennsylvania, 2000–2004. CES-D, Center for Epidemiologic Studies Depression [Scale].
Bivariate correlations between demographic, socioeconomic, health, and psychosocial characteristics and the trajectory classes are also shown in Table 1. Members of the groups differed by 1) demographic and socioeconomic variables, 2) self-rated physical and emotional health and the presence of comorbid conditions, 3) negative health behaviors, 4) ambivalence about the pregnancy, and 5) objective stress. These analyses were based on membership obtained from the unconditional model and, therefore, these bivariate results are approximate estimates (14).
The independent association of maternal characteristics with the distinct depressive symptomatology groups when compared with the never group was then assessed by multinomial logistic regression (Table 3) with adjustment for all covariates simultaneously. Variables that significantly improved the overall model (P < 0.05) were nativity, educational status, race/ethnicity, recent alcohol use, self-rated emotional health in the previous year, ambivalence about pregnancy with anxious character, and objective stress. The variables that were independently associated with increased risk of membership in the chronic compared with the never group included race/ethnicity (black women were less likely to belong to this group than white women), higher parity, fair/poor emotional health, ambivalence about pregnancy with anxious character, and increased objective stress. For the antepartum group, significant associations included nativity (US born is protective), race/ethnicity with Latina/Hispanic women being less likely to belong to this group than white women, fair/poor self-rated emotional health, recent alcohol use, ambivalence about pregnancy with anxious character, and high level of objective stress. Membership in the postpartum group was independently associated with nativity (US born is protective), low educational attainment, race/ethnicity with Latinas/Hispanics being less likely to belong to this group than whites, 1–2 previous livebirths, fair/poor self-rated emotional health, and having comorbidity, as well as moderate and high levels of objective stress. Finally, for the late group, less than high school education and higher levels of objective stress significantly increased the risk of belonging to this group.
Table 3.
Multinomial Regression Model Assessing Characteristics of Depression Trajectory Group Membership in Comparison With Never, Philadelphia, Pennsylvania, 2000–2004
| Variables (N = 1,735) | Chronic (n = 114; 7%) | Antepartum (n = 110; 6%) | Postpartum (n = 162; 9%) | Late (n = 112; 7%) | ||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Demographics | ||||||||
| Age | 0.974 | 0.927, 1.022 | 0.963 | 0.914, 1.015 | 1.003 | 0.964, 1.043 | 0.997 | 0.952, 1.044 |
| Nativity—US born | 0.959 | 0.510, 1.803 | 0.384* | 0.215, 0.686 | 0.517* | 0.316, 0.845 | 0.588 | 0.330, 1.048 |
| Educational status | ||||||||
| Less than high schoola | 1.394 | 0.681, 2.856 | 1.005 | 0.546, 1.850 | 2.011* | 1.095, 3.692 | 2.234* | 1.105, 4.517 |
| Still in high schoola | 1.404 | 0.584, 3.377 | 1.125 | 0.498, 2.542 | 2.675* | 2.320, 5.424 | 1.697 | 0.722, 3.989 |
| High school or equivalent | 0.936 | 0.469, 1.865 | 0.813 | 0.392, 1.685 | 1.205 | 0.686, 2.115 | 1.113 | 0.565, 2.192 |
| Any college or more | Referent | Referent | Referent | Referent | ||||
| Married | 0.991 | 0.587, 1.675 | 0.939 | 0.526, 1.676 | 0.895 | 0.564, 1.420 | 0.792 | 0.461, 1.360 |
| Race | ||||||||
| Latina/Hispanic | 0.934 | 0.455, 1.916 | 0.386* | 0.154, 0.970 | 0.425* | 0.209, 0.865 | 1.099 | 0.480, 2.516 |
| Black non-Hispanic | 0.416* | 0.226, 0.766 | 0.989 | 0.528, 1.852 | 0.843 | 0.492, 1.445 | 1.075 | 0.528, 2.189 |
| White and other | Referent | Referent | Referent | Referent | ||||
| Parity (living children) | ||||||||
| ≥3 | 3.054* | 1.473, 6.329 | 1.234 | 0.532, 2.859 | 1.554 | 0.799, 3.024 | 1.047 | 0.485, 2.262 |
| 1–2 | 1.797* | 1.071, 3.017 | 1.107 | 0.664, 1.848 | 1.668* | 1.098, 2.533 | 1.042 | 0.644, 1.687 |
| 0 | Referent | Referent | Referent | Referent | ||||
| Health measures | ||||||||
| Self-rated physical health | ||||||||
| Fair/poor | 1.069 | 0.552, 2.072 | 0.884 | 0.407, 1.921 | 0.739 | 0.394, 1.388 | 0.612 | 0.287, 1.308 |
| Good | 0.653 | 0.366, 1.153 | 1.109 | 0.620, 1.983 | 0.725 | 0.461, 1.142 | 0.942 | 0.574, 1.547 |
| Very good | 0.830 | 0.450, 1.531 | 1.123 | 0.607, 2.079 | 0.805 | 0.499, 1.298 | 0.384* | 0.199, 0.741 |
| Excellent | Referent | Referent | Referent | Referent | ||||
| Self-rated emotional health | ||||||||
| Fair/poor | 3.207* | 1.615, 6.369 | 3.352* | 1.693, 6.636 | 2.911* | 1.626, 5.212 | 1.851 | 0.976, 3.509 |
| Good | 1.360 | 0.692, 2.674 | 1.441 | 0.752, 2.760 | 1.547 | 0.906, 2.642 | 0.935 | 0.518, 1.686 |
| Very good | 1.076 | 0.515, 2.247 | 0.984 | 0.475, 2.040 | 1.651 | 0.958, 2.844 | 1.153 | 0.638, 2.082 |
| Excellent | Referent | Referent | Referent | Referent | ||||
| Comorbid condition | 1.577 | 0.966, 2.575 | 1.457 | 0.867, 2.449 | 1.653* | 1.094, 2.498 | 1.161 | 0.691, 1.952 |
| Health behaviors | ||||||||
| Smoked in pregnancy | 1.227 | 0.749, 2.010 | 1.459 | 0.868, 2.451 | 0.919 | 0.582, 1.451 | 1.254 | 0.740, 2.124 |
| Recent alcohol use | 1.336 | 0.853, 2.091 | 1.657* | 1.049, 2.618 | 0.814 | 0.543, 1.220 | 0.720 | 0.440, 1.178 |
| Recent marijuana use | 1.650 | 0.984, 2.765 | 0.980 | 0.564, 1.702 | 1.477 | 0.921, 2.368 | 1.374 | 0.777, 2.427 |
| Other measures | ||||||||
| Ambivalence about pregnancy | ||||||||
| Depressed | 1.207 | 0.744, 1.957 | 1.568 | 0.955, 2.574 | 1.032 | 0.689, 1.545 | 0.758 | 0.465, 1.236 |
| Anxious | 1.817* | 1.090, 3.029 | 1.845* | 1.095, 3.110 | 1.242 | 0.826, 1.869 | 0.938 | 0.578, 1.520 |
| Objective stress | ||||||||
| High | 4.757* | 2.421, 9.347 | 1.947* | 1.113, 3.407 | 2.011* | 1.250, 3.236 | 2.319* | 1.301, 4.133 |
| Moderate | 3.038* | 1.524, 6.055 | 1.155 | 0.644, 2.070 | 1.623* | 1.016, 2.593 | 1.962* | 1.117, 3.446 |
| Low | Referent | Referent | Referent | Referent | ||||
Abbreviations: aOR, adjusted odds ratio with variables run simultaneously; CI, confidence interval.
P < 0.05.
“Less than high school” is defined as less than high school status and more than 19 years of age; “still in high school” is defined as less than high school status and 19 years of age or less.
DISCUSSION
Using a novel approach, we described 5 distinct trajectory classes of depressive symptomatology (CES-D score, ever ≥16) from the first prenatal care visit through 2 years postpartum in a sample of over 1,700 low-income, mostly African-American women. By far, the largest class—never, comprising 71% of the women—did not have depressive symptomatology at any of the data collection time points. The remaining classes were considerably smaller and had varying degrees of severity and persistence of depressive symptoms. A range of characteristics were independently associated with membership in these 4 depressive symptom classes, including demographic and socioeconomic characteristics, emotional and physical health status, health behaviors, ambivalence regarding pregnancy, and a composite objective stress measure.
Our results are consistent with those from longitudinal studies in other populations where depressive symptomatology was associated with a heterogeneous group of individuals, of whom only a relatively small subset exhibited persistent depressive symptomotology (47). The timing and duration of depressive symptoms are likely to be associated with a varying risk of mood-related adverse outcomes relevant to maternal and child health. For example, we have previously shown that persistent depressive symptomatology with a score of ≥16 on the CES-D Scale from pregnancy through 1 year postpartum is associated with poor parenting practices (11). The chronic depressive symptomatology class identified in the current study represents a similar group of women but with more than 12 months longer duration of symptoms. Others have shown that women with depressive symptoms postpartum have a risk of persistent elevation over a substantial period of time (4, 12). However, we are not aware of other studies that have identified a discrete group of women who have elevated symptoms for a period spanning the first prenatal visit to 2 years postpartum. This group likely represents particularly at-risk women with a high need for intervention to reduce distress.
It is of particular interest that nearly three-quarters of our low-income, urban study women had low depressive symptomatology at all assessments and that the elevated depressive symptoms of another 15% were transient (antepartum and postpartum classes). Moreover, half of women with elevated symptoms at any single time were members of the chronic class. However, the classes with transient emotional distress were relatively small, making efficient screening and identification of the chronically depressed group difficult. The finding with the clearest clinical importance is that a low CES-D score of <16 is a good indicator of long-term emotional adjustment in ruling out not only current but also chronic emotional distress. In contrast, a high CES-D score is a more ambiguous indicator of persistent distress.
The demographic, socioeconomic, and health-related characteristics of women belonging to the various trajectory classes are also of interest because they suggest plausible linkages to causal pathways, as well as potential interventions targeting emotional distress among low-income pregnant and parenting women. Some of these variables were widely shared across the various depressive symptom classes including a high level of objective stress and fair/poor self-rated emotional health, indicating links between stressful exposures and a woman's self-assessment of emotional health and the risk of emotional distress in pregnancy and the postpartum period. Other variables were more uniquely associated with particular trajectory classes, such as high parity with the chronic class and ambivalence about the pregnancy with the chronic and antepartum classes. These findings are consistent with previous work linking unintended and mistimed pregnancy with emotional distress (37). Each of these sets of variables provides clues for future research to enhance the emotional health care of these vulnerable women.
A number of limitations of the current study should also be reviewed. First, this study sample is not nationally representative. Rather it captures a low-income, inner-city population of pregnant women who have multiple disadvantages. Thus, our findings are most appropriately generalized to similar population subgroups. A higher income and more socially resourced sample might yield different trajectory classes. However, we chose this study population because these women are at high risk for depressive symptomatology in pregnancy and so deserve particular attention. In addition, the identification of the trajectory classes was post hoc: It requires data from a first prenatal visit to 2 years postpartum. Confirmation of these distinct trajectories with other prospective data sets is needed to test whether similar trajectory classes are found and whether characteristics assessed at the prenatal visit can predict subsequent depressive symptomatology. Further, there is potential for bias in the missing data. Data with more frequent assessments and fewer missing values may help to improve our ability to determine whether these trajectories are a good reflection of women's experiences.
In summary, we have found evidence that pregnant women represent a heterogeneous group with regard to the timing and persistence of depressive symptomatology. Developing means of identifying high-risk groups would reduce the burden of service delivery and allow more focused attention on women with greater need. Further studies are needed to identify correlates of membership in the classes of trajectories of depressive symptomatology, the antecedents, and the behavioral and physical health consequences.
Acknowledgments
Author affiliations: Institute for Health, Health Care Policy, and Aging Research, Rutgers, The State University of New Jersey, New Brunswick, New Jersey (Pablo A. Mora); Department of Family Medicine and Community Health, Leonard Davis Institute of Health Economics, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania (Ian M. Bennett); Department of Sociology and Population Studies Center, University of Pennsylvania, Philadelphia, Pennsylvania (Irma T. Elo); Department of Obstetrics and Gynecology, Drexel University School of Medicine and the Children's Hospital of Philadelphia, Philadelphia, Pennsylvania (Leny Mathew, Jennifer F. Culhane); and Department of Psychiatry, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania (James C. Coyne).
This research was supported in part by funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant 1ROl D36462-01A I to I. T. E. and J. F. C.) and the Centers for Disease Control and Prevention (grant TS 312-15/15 to J. F. C.). I. M. B. received funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant 1K23HD048915-01A2) and the National Institute of Mental Health (grant 1R03MH074750-01).
Portions of this work were presented at the 19th National Conference on Mental Health Services Research: “Enhancing the Impact of Mental Health Services Research,” Washington, DC, July 23–24, 2007.
Conflict of interest: none declared.
Glossary
Abbreviations
- CES-D
Center for Epidemiologic Studies Depression
- GMM
growth mixture modeling
- SD
standard deviation
References
- 1.Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 2.Stowe ZN, Hostetter AL, Newport DJ. The onset of postpartum depression: implications for clinical screening in obstetrical and primary care. Am J Obstet Gynecol. 2005;192(2):522–526. doi: 10.1016/j.ajog.2004.07.054. [DOI] [PubMed] [Google Scholar]
- 3.Howell EA, Mora PA, Horowitz CR, et al. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol. 2005;105(6):1442–1450. doi: 10.1097/01.AOG.0000164050.34126.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beeghly M, Olson KL, Weinberg MK, et al. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Matern Child Health J. 2003;7(3):157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- 5.Gordon TEJ, Cardone IA, Kim JJ, et al. Universal perinatal depression screening in an academic medical center. Obstet Gynecol. 2006;107(2 pt 1):342–347. doi: 10.1097/01.AOG.0000194080.18261.92. [DOI] [PubMed] [Google Scholar]
- 6.Bosquet M, Egeland B. Associations among maternal depressive symptomatology, state of mind and parent and child behaviors: implications for attachment-based interventions. Attach Hum Dev. 2001;3(2):173–199. doi: 10.1080/14616730010058007. [DOI] [PubMed] [Google Scholar]
- 7.Chung TK, Lau TK, Yip AS, et al. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med. 2001;63(5):830–834. doi: 10.1097/00006842-200109000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman S, Hatch MC. Depressive symptomatology during pregnancy: evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychol. 2000;19(6):535–543. [PubMed] [Google Scholar]
- 9.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 10.Orr ST, Miller CA. Maternal depressive symptoms and the risk of poor pregnancy outcome. Review of the literature and preliminary findings. Epidemiol Rev. 1995;17(1):165–171. doi: 10.1093/oxfordjournals.epirev.a036172. [DOI] [PubMed] [Google Scholar]
- 11.Chung EK, McCollum KF, Elo IT, et al. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6):e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 12.Beeghly M, Weinberg MK, Olson KL, et al. Stability and change in level of maternal depressive symptomatology during the first postpartum year. J Affect Disord. 2002;71(1-3):169–180. doi: 10.1016/s0165-0327(01)00409-8. [DOI] [PubMed] [Google Scholar]
- 13.Andersson L, Sundstrom-Poromaa I, Wulff M, et al. Depression and anxiety during pregnancy and six months postpartum: a follow-up study. Acta Obstet Gynecol Scand. 2006;85(8):937–944. doi: 10.1080/00016340600697652. [DOI] [PubMed] [Google Scholar]
- 14.Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- 15.Muthén B, Asparouhov T. Growth mixture modeling: analysis with non-Gaussian random effects. In: Fitzmaurice G, Davidian M, Verbeke G, et al., editors. Longitudinal Data Analysis. Boca Raton, FL: Chapman & Hall/CRC Press; 2008. [Google Scholar]
- 16.Culhane JF, Rauh V, McCollum KF, et al. Exposure to chronic stress and ethnic differences in rates of bacterial vaginosis among pregnant women. Am J Obstet Gynecol. 2002;187(5):1272–1276. doi: 10.1067/mob.2002.127311. [DOI] [PubMed] [Google Scholar]
- 17.Bennett IM, Culhane JF, McCollum KF, et al. Unintended rapid repeat pregnancy and low education status: any role for depression and contraceptive use? Am J Obstet Gynecol. 2006;194(3):749–754. doi: 10.1016/j.ajog.2005.10.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radloff LS, Locke BZ. The Community Mental Health Assessment Survey and the CES-D scale. In: Weissman MM, Myers JK, Ross CE, editors. Community Surveys of Psychiatric Disorders. New Brunswick, NJ: Rutgers University Press; 1986. pp. 177–189. [Google Scholar]
- 19.McLennan JD, Kotelchuck M, Cho H. Prevalence, persistence, and correlates of depressive symptoms in a national sample of mothers of toddlers. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1316–1323. doi: 10.1097/00004583-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Weissman MM, Sholomskas D, Pottenger M, et al. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106(3):203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 21.Husaini BA, Neff JA, Harrington JB, et al. Depression in rural communities: validating the CES-D scale. J Community Psychol. 1980;8(1):20–27. [Google Scholar]
- 22.Craig TJ, Van Natta PA. Presence and persistence of depressive symptoms in patient and community populations. Am J Psychiatry. 1976;133(12):1426–1429. doi: 10.1176/ajp.133.12.1426. [DOI] [PubMed] [Google Scholar]
- 23.Berenson AB, Breitkopf CR, Wu ZH. Reproductive correlates of depressive symptoms among low-income minority women. Obstet Gynecol. 2003;102(6):1310–1317. doi: 10.1016/j.obstetgynecol.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Gotlib IH, Whiffen VE, Mount JH, et al. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269–274. doi: 10.1037//0022-006x.57.2.269. [DOI] [PubMed] [Google Scholar]
- 25.Hobfoll SE, Ritter C, Lavin J, et al. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol. 1995;63(3):445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 26.Howell E, Mora P, Leventhal H. Correlates of early postpartum depressive symptoms. Matern Child Health J. 2006;10(2):149–157. doi: 10.1007/s10995-006-0116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuo WH, Wilson TE, Holman S, et al. Depressive symptoms in the immediate postpartum period among Hispanic women in three U.S. cities. J Immigr Health. 2004;6(4):145–153. doi: 10.1023/B:JOIH.0000045252.10412.fa. [DOI] [PubMed] [Google Scholar]
- 28.Larsson D, Lager I, Nilsson PM. Socio-economic characteristics and quality of life in diabetes mellitus—relation to metabolic control. Scand J Public Health. 1999;27(2):101–105. [PubMed] [Google Scholar]
- 29.Flynn HA, Davis M, Marcus SM, et al. Rates of maternal depression in pediatric emergency department and relationship to child service utilization. Gen Hosp Psychiatry. 2004;26(4):316–322. doi: 10.1016/j.genhosppsych.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 30.Bernazzani O, Saucier JF, David H, et al. Psychosocial predictors of depressive symptomatology level in postpartum women. J Affect Disord. 1997;46(1):39–49. doi: 10.1016/s0165-0327(97)00077-3. [DOI] [PubMed] [Google Scholar]
- 31.Bernazzani O, Saucier JF, David H, et al. Psychosocial factors related to emotional disturbances during pregnancy. J Psychosom Res. 1997;42(4):391–402. doi: 10.1016/s0022-3999(96)00371-6. [DOI] [PubMed] [Google Scholar]
- 32.O'Hara MW, Schlechte JA, Lewis DA, et al. Prospective study of postpartum blues. Biologic and psychosocial factors. Arch Gen Psychiatry. 1991;48(9):801–806. doi: 10.1001/archpsyc.1991.01810330025004. [DOI] [PubMed] [Google Scholar]
- 33.McHorney CA, Ware JE, Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36). II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Pajulo M, Savonlahti E, Sourander A, et al. Antenatal depression, substance dependency and social support. J Affect Disord. 2001;65(1):9–17. doi: 10.1016/s0165-0327(00)00265-2. [DOI] [PubMed] [Google Scholar]
- 35.Zuckerman BS, Beardslee WR. Maternal depression: a concern for pediatricians. Pediatrics. 1987;79(1):110–117. [PubMed] [Google Scholar]
- 36.Higgins S. Smoking in pregnancy. Curr Opin Obstet Gynecol. 2002;14(2):145–151. doi: 10.1097/00001703-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Huizink AC, Mulder EJH. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci Biobehav Rev. 2006;30(1):24–41. doi: 10.1016/j.neubiorev.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 38.Hurd YL, Wang X, Anderson V, et al. Marijuana impairs growth in mid-gestation fetuses. Neurotoxicol Teratol. 2005;27(2):221–229. doi: 10.1016/j.ntt.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 39.Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. Br J Psychiatry. 1984;144:35–47. doi: 10.1192/bjp.144.1.35. [DOI] [PubMed] [Google Scholar]
- 40.Coyne JC, Whiffen VE. Issues in personality as diathesis for depression: the case of sociotropy-dependency and autonomy-self-criticism. Psychol Bull. 1995;118(3):358–378. doi: 10.1037/0033-2909.118.3.358. [DOI] [PubMed] [Google Scholar]
- 41.Mazure CM, Kincare P, Schaffer CE. DSM-III-R Axis IV: clinician reliability and comparability to patients’ reports of stressor severity. Psychiatry. 1995;58(1):56–64. doi: 10.1080/00332747.1995.11024711. [DOI] [PubMed] [Google Scholar]
- 42.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 43.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc; 2002. [Google Scholar]
- 44.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 45.Nylund KL, Asparouhov T, Muthén B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Struct Equation Model. 2007;14(4):535–569. [Google Scholar]
- 46.Muthen B, Asparouhov T. Item response mixture modeling: application to tobacco dependence criteria. Addict Behav. 2006;31(6):1050–1066. doi: 10.1016/j.addbeh.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 47.Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: identifying latent trajectories and early predictors. J Abnorm Psychol. 2005;114(3):331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]