Abstract
Background
A model that predicts the economic benefit of reduced cancer mortality provides critical information for allocating scarce resources to the interventions with the greatest benefits.
Methods
We developed models using the human capital approach, which relies on earnings as a measure of productivity, to estimate the value of productivity lost as a result of cancer mortality. The base model aggregated age- and sex-specific data from four primary sources: 1) the US Bureau of the Census, 2) US death certificate data for 1999–2003, 3) cohort life tables from the Berkeley Mortality Database for 1900–2000, and 4) the Bureau of Labor Statistics Current Population Survey. In a model that included costs of caregiving and household work, data from the National Human Activity Pattern Survey and the Caregiving in the U.S. study were used. Sensitivity analyses were performed using six types of cancer assuming a 1% decline in cancer mortality rates. The values of forgone earnings for employed individuals and imputed forgone earnings for informal caregiving were then estimated for the years 2000–2020.
Results
The annual productivity cost from cancer mortality in the base model was approximately $115.8 billion in 2000; the projected value was $147.6 billion for 2020. Death from lung cancer accounted for more than 27% of productivity costs. A 1% annual reduction in lung, colorectal, breast, leukemia, pancreatic, and brain cancer mortality lowered productivity costs by $814 million per year. Including imputed earnings lost due to caregiving and household activity increased the base model total productivity cost to $232.4 billion in 2000 and to $308 billion in 2020.
Conclusions
Investments in programs that target the cancers with high incidence and/or cancers that occur in younger, working-age individuals are likely to yield the greatest reductions in productivity losses to society.
CONTEXT AND CAVEATS
Prior knowledge
A model to estimate the economic benefit of reduced cancer mortality would provide information regarding which interventions would have the greatest economic impact.
Study design
Models to estimate the value of productivity lost due to premature death due to cancer during 2000–2020 were developed using the human capital approach, which uses earnings to measure productivity. A model that included caregiving and household work was also developed.
Contribution
The annual productivity cost of cancer mortality was $115.8 billion in 2000 and was projected to be $147.6 billion in 2020. Including caregiving and household activity increased these values to $232.4 billion for 2000 and $308 billion for 2020. A 1% annual reduction in death from lung, colorectal, breast, pancreatic, and brain cancer and leukemia reduced costs by $814 million per year.
Implications
The most useful targets for cancer control programs, from an economic perspective of cost in terms of productivity, are those that have high incidence or occur at younger ages.
Limitations
The costs may be underestimated because factors such as productivity costs due to morbidity and disability of the cancer and/or its treatment were not included in the calculations, life expectancy was used rather than survivorship, and those who died from cancer before age 20 were not included.
From the Editors
Cancer is the second leading cause of death and a major cause of lost productivity in adults in the United States (1,2). Progress toward reducing mortality from cancer has been steady for many sites, including lung, breast, non-Hodgkin lymphoma, colon and rectum, and cervix. Overall, cancer mortality rates have decreased by 1.1% per year from 1993 through 2002 (3).
Decreased cancer mortality is attributable to many health initiatives, including prevention, early detection, and effective treatments. However, the economic gain from these investments is highly variable. A model that predicts the economic benefit of reduced cancer mortality provides critical information for allocating scarce resources to interventions with the greatest benefits. The value of productivity lost from premature mortality is a key element in such a model because these costs reflect substantial losses to society.
We developed a model based on the human capital method (4) to estimate and project the value of lost productivity attributable to death from cancer for the years 2000–2020. We estimated the value of lost productivity for all cancers combined and for the 19 most prevalent sites of cancer (urinary bladder, female breast, brain and other nervous system, cervix uteri, colorectal, corpus and uterus, stomach, head and neck, Hodgkin lymphoma, kidney and renal pelvis, leukemia, liver and intrahepatic bile duct, lung and bronchus, melanoma, non-Hodgkin lymphoma, ovary, pancreas, prostate, and testis). We also estimated the value of lost earnings per year, by sex and 5-year age groups, from paid employment as well as non-paid caregiving and housekeeping activities.
Data Sources and Methods
Study Design
The human capital method has a long history in economic and health services research as a means to calculate the expected lifetime earnings that would have been realized had the disease or death been avoided. This method assumes that earnings reflect underlying productivity. Because it relies on earnings as the basis for its cost estimations, this method gives greater weight to working-age men compared with women, the young, racial and ethnic minorities, and the elderly (5). Furthermore, the human capital method does not measure the value of a life, but instead, it measures only the value of labor, using earnings or imputed earnings as a proxy measure.
We used the human capital method with an incidence-based approach to estimate the costs of cancer deaths that occurred and are predicted to occur between 2000 and 2020. The base model reflects employment and income transitions over the life cycle by summing the expected earnings in each year of forgone life over a given life expectancy, accounting for changes in the probability of employment and wages that occur from year to year and from age group to age group. For example, life expectancy for a man aged 35 in 2000 was an additional 42.2 years (6). Using assumptions in our model, a man who died at age 35 years in 2000 had a .93 probability of being employed, and his average annual full-time earnings plus the value of fringe benefits would be $56 519. Had he lived, his probability of employment would have decreased to 0.87 at age 50, but his annual average earnings would have increased to $87 706 (including fringe benefits) in the year 2015. His probability of employment would have further decreased at age 65 in the year 2030 and continued to decline for his remaining life span. We accounted for such year-by-year transitions in employment probabilities and expected earnings throughout the expected lifetime of the individuals who would have otherwise lived in the absence of cancer.
Because our society relies on individuals to provide essential household and caregiving functions that would otherwise be filled by other potentially more expensive providers and because these activities may also impact providers’ participation in the labor force (7), we added the estimated value of informal caregiving and household activities to the base model. We estimated the value of informal caregiving and housekeeping separately by imputing a wage for the hours spent engaged in these activities.
We report the present value of lifetime earnings (PVLE) as the sum of productivity costs and the sum of the imputed value of caregiving and household activities. Thus, the PVLE takes into account life expectancy for different sex and age groups, the percentage of people in the labor force, and/or those who are engaged in caregiving and household activities, the current pattern of earnings at successive ages, an imputed value of caregiving and household activities, and the discount rate (8). A discount rate (3%) is applied to convert future dollars to their present value.
Data
The base model used aggregate age- and sex-specific data from four sources. First, the US Bureau of the Census provided the National Interim Projections of the US population from 2000 through 2020 (9). Second, US death certificate data covering 1999 through 2003 were used to estimate age-adjusted cancer site-specific mortality rates. Third, cohort life tables from the Berkeley Mortality Database for birth years 1900–2000 were used to estimate and project sex-specific life expectancy in the years 2000–2020. The Berkeley Mortality Database, which was developed from historical series of national vital statistics (ie, births, deaths, and census populations), is part of the Human Mortality Database project, whose aim is to construct high-quality national cohort life tables. Projections incorporate observed trends in life expectancy in the past century. Because these life tables only contain years of birth through 2000, we assumed that individuals born after 2000 (ie, 2001–2020) would have the same life expectancy as those born in 2000. These cohort life table data and related documentation are available at http://www.demog.berkeley.edu/∼bmd/states.html (10). Fourth, all estimates of wages, employment rates, and full- and part-time employment rates were from the Current Population Survey (CPS). The CPS is a monthly survey of households that is conducted by the Bureau of the Census for the Bureau of Labor Statistics (BLS); it is the primary source of information on labor force characteristics and behavior of the US population (11). Fringe benefits constitute approximately 27.4% of compensation (12). These benefits include vacation pay, health insurance, retirement benefits, and annual and personal leave. It has been argued (12) that paid leave should not be used to adjust annual earnings. Therefore, Grosse (12) suggests that annual earnings should be adjusted upward by 22.4% instead of 27.4% to reflect the absence of paid leave and to compensate for worker categories (eg, agricultural workers) that do not have generous benefits (12). Following the example set by Grosse, we used a rate of 22.4% to upwardly adjust annual earnings for full-time workers and a rate of 10.3% to upwardly adjust part-time workers’ annual earnings.
Two additional data sources were used to estimate the number of caregivers and housekeepers in the population. First, we use estimates from Grosse (12) of the number of individuals who were engaged in both housekeeping and caregiving. These estimates are based on responses to the National Human Activity Pattern Survey (NHAPS) administered by the US Environmental Protection Agency. This survey collected information on household production (housework, food cooking and cleanup, taking care of plants and animals, home and auto maintenance, and obtaining goods and services) and providing care (childcare, child guidance, playing with children, transporting children, helping and caring for adults, helping adults with other personal activities, and personal care travel). Grosse (12) used these estimates to determine the prevalence of individuals living in households and time spent on various caregiving and household activities and then applied a wage rate, derived from the CPS, corresponding to the proportion of time spent doing various activities. Imputed housekeeping and caregiving wages were then adjusted up by a fringe benefit rate ranging from 10.3% to 14.1% (12). The second source was the Caregiving in the U.S. study (13), which was conducted by the National Alliance for Caregiving and the American Association of Retired Persons. This national survey identified 1247 caregivers primarily through the random digit dial technique and collected precise information on hours spent caregiving and the type of care provided. The estimates for caregiving and household activities reflect the value of unpaid activities in which individuals would have been engaged if they had not died from cancer. We used this study to estimate the percentage of the US population who were engaged in caregiving and, among those individuals, the percentage who provided round-the-clock care.
Analysis
We estimated the number of deaths, person-years of life lost (PYLL), and average person-years of life lost. Individual years of life lost estimates were summed into 5-year age groups starting with ages 20–24 and ending with a single group for persons aged 85 and older.
We used mean weekly wages by sex for all races and occupations combined for the years 2000–2006, available from the BLS on request. Wages were reported for the 5-year age groups of interest but were combined for all aged 70 and older. We used the wages published in Grosse (12) to determine the imputed value of caregiving and household activities. Different wage rates were imputed for caregivers and housekeepers; these wages were then weighted by the time spent engaged in each type of activity. For example, a typical single individual without children who is employed full-time spends less time engaged in caregiving and household activities than an unemployed individual with children.
To estimate wages for future years, we adjusted wages beyond 2006 for inflation using the consumer price index (CPI) (14). Annual inflation conversion factors were 2.1% in 2007 and 2.2% in 2008–2020. The CPI-inflated wages were used as a proxy for real future wages.
We incorporated estimates of full- and part-time employment from the BLS for the years 2000 through 2007 for individuals who were age 18–79 years. Because comparable estimates were not available for individuals who were age 80 years and older, we applied the rates for the 75- to 79-year age group to those who were age 80 and older. We used the average employment rates from 2000 through 2007 to project future employment rates.
According to the Caregiving in the U.S. survey, approximately 21% of the US population older than 18 years is engaged in care giving activities, which includes housekeeping chores for another individual who is also 18 years or older. Approximately 10% of these caregivers provide more than 40 hours per week of care and assist another individual with two or more activities of daily living (ADLs). Therefore, we assigned an annual earning equivalent as the annual charge for nursing home care, which was $74 000 in 2005, and adjusted it using the CPI and a projection of the CPI for future years (15). This level of care was projected to last for 2.4 years, which is the average length of time patients reside in a nursing home (16).
Because a 20-year-old individual in 2020 was expected to live 62 additional years, all estimates of wages, employment, and caregiver and housekeeping rates were projected to 2082 to account for the maximum number of years this cohort of individuals could have lived. The number of deaths, PYLL, employment and caregiver and housekeeper rates, wages by sex and age, and the average PVLE for the year 2000 are reported (Table 1).
Table 1.
Model inputs and average PVLE for the year 2000*
| Sex and age, y | No. of deaths | Mean person-years of life lost | Person-years of life lost | Percent employed | Percent employed full time | Percent employed part time | Annual mean full-time earnings, $US | Annual mean part-time earnings, $US | Mean PVLE, $US | Proportion of persons living in households | Adjusted caregiving and household wages, $US | Mean PVLE including caregiving and household wages in $US |
| Females | ||||||||||||
| 20–24 | 394 | 61.39 | 24 190 | 73.3 | 69.0 | 31.0 | 27 050 | 12 188 | 1 338 188 | 91.5 | 9806 | 2 230 023 |
| 25–29 | 657 | 56.12 | 36 870 | 77.1 | 82.0 | 18.0 | 39 271 | 17 694 | 1 284 081 | 99.2 | 13 233 | 2 142 912 |
| 30–34 | 1378 | 51.07 | 70 370 | 75.6 | 82.0 | 18.0 | 41 308 | 18 612 | 1 167 549 | 99.2 | 13 233 | 1 972 799 |
| 35–39 | 3148 | 45.94 | 144 600 | 75.8 | 80.0 | 20.0 | 43 917 | 19 788 | 1 019 631 | 99.5 | 15 000 | 1 767 713 |
| 40–44 | 5956 | 40.93 | 243 760 | 78.7 | 80.0 | 20.0 | 43 917 | 19 788 | 873 166 | 99.5 | 15 000 | 1 551 323 |
| 45–49 | 9442 | 35.98 | 339 710 | 77.0 | 82.0 | 18.0 | 45 954 | 20 706 | 704 211 | 99.3 | 14 958 | 1 309 721 |
| 50–54 | 14 010 | 31.18 | 436 830 | 74.1 | 82.0 | 18.0 | 48 182 | 21 709 | 519 640 | 99.3 | 14 958 | 1 050 032 |
| 55–59 | 17 675 | 26.57 | 469 680 | 59.7 | 75.0 | 25.0 | 45 572 | 20 533 | 335 524 | 99.3 | 16 334 | 791 482 |
| 60–64 | 22 199 | 22.27 | 494 290 | 39.1 | 75.0 | 25.0 | 43 217 | 19 472 | 179 874 | 99.3 | 16 334 | 555 047 |
| 65–69 | 28 540 | 18.29 | 522 110 | 18.8 | 41.0 | 59.0 | 34 115 | 15 371 | 72 285 | 98.1 | 15 871 | 363 558 |
| 70–74 | 37 440 | 14.67 | 549 330 | 9.7 | 41.0 | 59.0 | 32 651 | 14 712 | 33 291 | 98.1 | 15 871 | 240 800 |
| 75–79 | 42 004 | 11.37 | 477 460 | 3.5 | 41.0 | 59.0 | 32 651 | 14 712 | 16 821 | 87.3 | 13 606 | 174 422 |
| 80–84 | 36 395 | 8.48 | 308 500 | 3.5 | 41.0 | 59.0 | 32 651 | 14 712 | 11 531 | 87.3 | 13 606 | 114 175 |
| ≥85 | 42 777 | 5.30 | 226 850 | 3.5 | 41.0 | 59.0 | 32 651 | 14 712 | 6144 | 87.3 | 13 606 | 81 229 |
| Males | ||||||||||||
| 20–24 | 553 | 56.09 | 31 020 | 82.6 | 81.0 | 19.0 | 28 960 | 13 048 | 2 158 521 | 87.9 | 5234 | 2 692 877 |
| 25–29 | 699 | 51.03 | 35 670 | 92.4 | 95.0 | 5.0 | 43 090 | 19 415 | 2 100 893 | 96.4 | 7396 | 2 623 380 |
| 30–34 | 1164 | 46.16 | 53 730 | 94.2 | 95.0 | 5.0 | 49 200 | 22 168 | 1 944 784 | 96.4 | 7396 | 2 440 182 |
| 35–39 | 2325 | 41.25 | 95 890 | 93.2 | 97.0 | 3.0 | 56 519 | 25 466 | 1 721 472 | 97.8 | 9210 | 2 187 183 |
| 40–44 | 4869 | 36.46 | 177 520 | 92.1 | 97.0 | 3.0 | 58 747 | 26 470 | 1 464 748 | 97.8 | 9210 | 1 893 059 |
| 45–49 | 9153 | 31.72 | 290 310 | 90.1 | 96.0 | 4.0 | 60 593 | 27 301 | 1 195 154 | 98.7 | 9229 | 1 579 902 |
| 50–54 | 14 989 | 27.09 | 406 120 | 86.8 | 96.0 | 4.0 | 62 821 | 28 305 | 906 994 | 98.7 | 9229 | 1 250 273 |
| 55–59 | 20 535 | 22.68 | 465 640 | 77.1 | 90.0 | 10.0 | 59 638 | 26 871 | 623 565 | 98.7 | 11 234 | 921 947 |
| 60–64 | 27 265 | 18.59 | 506 710 | 54.8 | 90.0 | 10.0 | 54 928 | 24 749 | 340 503 | 98.7 | 11 234 | 584 905 |
| 65–69 | 35 826 | 14.94 | 535 180 | 30.1 | 55.0 | 45.0 | 46 272 | 20 849 | 167 294 | 98.2 | 12 395 | 377 325 |
| 70–74 | 45 706 | 11.74 | 536 690 | 17.9 | 55.0 | 45.0 | 48 245 | 21 738 | 79 668 | 98.2 | 12 395 | 229 796 |
| 75–79 | 47 732 | 8.93 | 426 230 | 8.0 | 55.0 | 45.0 | 48 245 | 21 738 | 41 351 | 93.1 | 11 351 | 138 485 |
| 80–84 | 36 849 | 6.63 | 244 260 | 8.0 | 55.0 | 45.0 | 48 245 | 21 738 | 27 890 | 93.1 | 11 351 | 103 292 |
| ≥85 | 31 997 | 4.42 | 141 260 | 8.0 | 55.0 | 45.0 | 48 245 | 21 738 | 17 832 | 93.1 | 11 351 | 58 479 |
PVLE = present value of lifetime earnings. Annual earnings are adjusted up by 22.4% to include the value of fringe benefits. Part-time earnings are adjusted by 10.3% to include the value of fringe benefits. Persons living in households and the upwardly adjusted caregiving and household wages are from Grosse (12). We assume that 2.1% of the population provides care for an individual that would otherwise be institutionalized. For these individuals, this care is provided for 2.4 years, which is the average nursing home length of stay, and estimated at a value of $74 000 in 2005 and adjusted using the CPI in all other years. Estimates of persons living in households and their adjusted wages are from Grosse (12).
We conducted a sensitivity analysis to determine the degree of influence certain assumptions had on the outcome of the overall model. We chose three assumptions for which uncertainty exists. First, we relaxed our assumption that individuals aged 80 and older were employed at the same rate as individuals aged 74–79 years because the BLS does not report the earnings and employment rate of persons aged 80 and older. To test the sensitivity of our results to this assumption, we assumed that no one over the age of 79 was engaged in paid work. Second, we removed the cost of nursing home care from the model. Finally, we reduced the prevalence of caregiving and housekeeping in the model.
The model was developed using Microsoft Excel 2003. The model included the ability to conduct sensitivity analyses on key assumptions.
Results
Base Model
In 2000, the total PVLE lost due to cancer deaths was approximately $115.8 billion, which steadily increased to approximately $147.6 billion in 2020 (Figure 1). The productivity costs were higher for men than women ($75.9 billion vs $39.9 billion in 2000), which is a function of the higher death rate among men (17 647 more men than women died in the year 2000), their higher labor force participation, and their higher wages.
Figure 1.
Present value of lifetime earnings due to cancer mortality, adults age 20 and older, years 2000–2020. Hatched bar, males; solid bar, females.
The total PVLE lost and PVLE lost per death by cancer site for the year 2010 were estimated (Table 2). Lung cancer deaths accounted for more than 27% of the total costs ($39.0 billion). The next most expensive cancers, in terms of productivity costs, were colon and rectal cancers ($12.8 billion) and female breast cancer ($10.9 billion), which accounted for approximately 9% and 8% of the total PVLE lost, respectively.
Table 2.
Site-specific present value of lifetime earnings (PVLE) among adults 20 and older in 2010
| Cancer site | PVLE, $US | Percentage of total cost | Deaths | PVLE/death, $US |
| Total (all cancers) | 142 373 887 175 | 100.00 | 657 005 | 216 701 |
| Lung and bronchus | 38 953 476 028 | 27.36 | 185 202 | 210 330 |
| Colon and rectum | 12 802 283 437 | 8.99 | 67 928 | 188 468 |
| Female breast | 10 878 840 020 | 7.64 | 48 776 | 223 037 |
| Pancreas | 7 058 015 604 | 4.96 | 35 474 | 198 963 |
| Leukemia | 5 879 620 378 | 4.13 | 24 459 | 240 387 |
| Brain and other nervous system | 5 851 151 373 | 4.11 | 14 894 | 392 853 |
| Non-Hodgkin lymphoma | 5 755 042 326 | 4.04 | 26 230 | 219 407 |
| Liver and intrahepatic bile duct | 4 638 204 280 | 3.26 | 16 041 | 289 147 |
| Ovary | 2 944 996 275 | 2.07 | 16 700 | 176 347 |
| Kidney and renal pelvis | 3 632 633 377 | 2.55 | 14 246 | 254 993 |
| Head and neck | 3 630 391 776 | 2.55 | 12 109 | 299 809 |
| Prostate | 3 537 601 571 | 2.48 | 37 819 | 93 540 |
| Stomach | 3 453 510 837 | 2.43 | 14 774 | 233 756 |
| Melanoma of the skin | 3 298 014 331 | 2.32 | 8871 | 371 775 |
| Urinary bladder | 1 976 965 144 | 1.39 | 14 794 | 133 633 |
| Cervix uteri | 1 807 797 110 | 1.27 | 4666 | 387 440 |
| Corpus and uterus | 1 101 322 676 | 0.77 | 7896 | 139 479 |
| Hodgkin lymphoma | 828 691 758 | 0.58 | 1523 | 544 118 |
| Testis | 471 622 615 | 0.33 | 372 | 1 267 803 |
| All other sites | 23 873 706 259 | 16.77 | 104 231 | 229 046 |
The most costly cancer per death in 2010 was testicular cancer ($1.3 million). Although there were few testicular cancer deaths relative to deaths from other sites of cancer, and therefore the total productivity cost was relatively low, the majority of deaths occur in younger working-age men. Likewise, the second most costly cancer per death was Hodgkin lymphoma ($544 118) followed by brain ($392 853) and cervical ($387 440) cancers because these deaths occur in working-age individuals. In contrast, prostate cancer was the least costly cancer per death ($93 540), due to its prevalence in older men who are no longer in the workforce.
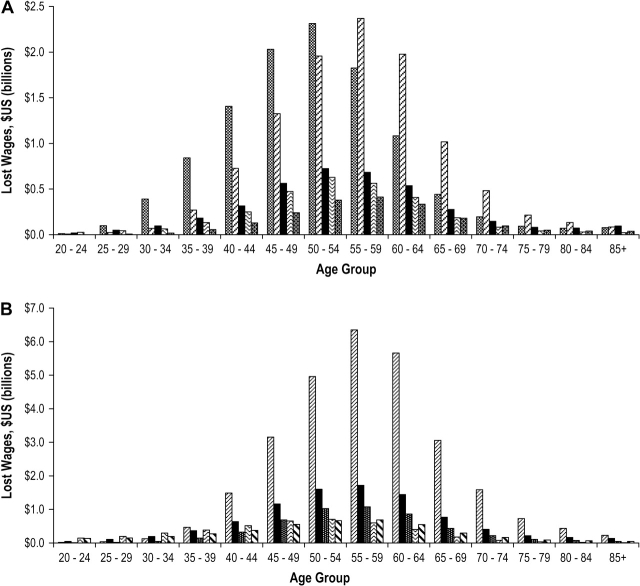
The total PVLE lost for the most costly cancers was estimated among women and men by age groups (Figure 2). For women younger than age 55, breast cancer resulted in the greatest productivity loss. For women age 55 and older, the mortality rate from lung cancer increased and it became the most costly cancer for women. The next most costly cancers for women were those of the colon and rectum, followed by ovarian and pancreatic cancer. The cost of lung cancer deaths dominated the cost of all other cancers for men aged 35 and older. Among men younger than age 35, death from brain cancer resulted in the greatest productivity costs.
Figure 2.
Cancers with highest present value of lifetime earnings, adults age 20 and older in the year 2010. A) Women. From left to right: female breast cancer, lung cancer, colorectal cancer, ovarian cancer, and pancreatic cancer. B) Men. From left to right: lung cancer, colorectal cancer, pancreatic cancer, brain cancer, non-Hodgkin lymphoma.
Recent trends suggest that overall cancer mortality has declined by approximately 1% per year. Reducing annual mortality rates by another 1%, starting in 2010, would reduce productivity costs of six costly cancers—lung, colon and rectum, female breast, pancreas, leukemia, and brain—by approximately $814 million per year (Figure 3). Clearly, a reduction in lung cancer mortality would offer the greatest reduction in productivity costs, of approximately $390 million in 2010 and $416 million in 2020.
Figure 3.
Reduction in productivity costs with an additional 1% annual reduction (starting in the year 2010) in cancer mortality in selected sites, years 2010 and 2020. From left to right: lung cancer, colorectal cancer, breast cancer, pancreatic cancer, leukemia, and brain cancer.
Caregiving and Household Activity
When the value of caregiving and household activities was included in the model, costs increased dramatically. In 2000, for example, the total cost was $232.4 billion (relative to $115.8 billion) and in 2020, the cost rose to $308 billion (relative to 147.6 billion). In 2010, the caregiving costs for men were 42% ($58.5 billion) of the total costs ($139.7 billion) and the caregiving costs for women were 64% ($78.3 billion) of the total costs ($122 billion). The percentage of total costs that were attributable to caregiving remained about the same in 2020 (Figure 4). The cost of nursing home care was only 1% in 2010 and 2% in 2020.
Figure 4.
Composition of total productivity costs by sex, years 2010 and 2020. Left diagonal, full-time employment; horizontal, part-time employment; solid, caregiver time; open, nursing home cost.
Sensitivity Analysis
We conducted a sensitivity analysis that was based on modifying three assumptions. First, we relaxed our assumption that individuals aged 80 and older were employed. Second, we removed the cost of nursing home care from the model. Finally, we reduced the prevalence of caregiving and housekeeping in our model.
The results were not sensitive to employment and earning rates for individuals who were age 80 and older or to the inclusion of nursing home costs in the model. In the base model, the exclusion of employment and earnings from paid work for individuals aged 80 and older reduced total costs by only 2.9%.
The inclusion of caregiving and housekeeping greatly increased mortality costs. However, nursing home costs were only 1% of costs in 2010 and 2% of costs in 2020. Caregiving and housekeeping services were 65% and 43% of the total cost in 2010 for women and men, respectively. The Caregiving in the U.S. survey to individuals age 18 and older (13) estimates that 21% of Americans provide caregiving services but does not provide the prevalence of caregiving by sex and age. Nevertheless, when we used the overall estimate of prevalence as 21%, the total productivity cost from cancer mortality was $153 billion in 2010 and rose to $164 billion in 2020.
Discussion
The productivity costs from premature cancer mortality are substantial. In the base model, we estimated that the total productivity costs in 2000 were approximately $115.8 billion and that, with current mortality rates, these costs would increase to $147.6 billion in 2020. A fixed cancer mortality rate based on the most recent available data was used for the projections. Therefore, the increases in cost over time strictly reflect expected growth and aging in the population. To put the productivity costs from cancer deaths into perspective, the annual cost amounts to approximately 1% of the US gross domestic product (GDP; $13.84 trillion) in 2007 (17).
Other reports estimate the cost due to both morbidity and premature mortality from cancer as $139.9 billion in fiscal year 2005 (18,19). Mortality cost alone has been estimated as $116.1 billion in 2007 by the National Heart, Lung, and Blood Institute (NHLBI) (19). This mortality cost estimate was obtained by first multiplying the number of deaths in 2004 in each age- and sex-specific group by the 2003 value of lifetime earnings discounted at 3%; summing these estimates for each diagnostic group; and multiplying the estimates by a 2003–2008 inflation factor (1.14) that was based on change in mean earnings. These estimates are similar to our reported productivity costs. The difference is due primarily to our use of more detailed methods and the inclusion of the dollar value of fringe benefits in addition to earnings, which increases full-time wages by 22.4% and part-time wages by 10.3%. Without the inclusion of fringe benefits and caregiving in the model, our estimates for 2007 would decrease to $115.3 billion. The remaining difference between the NHLBI estimates and our estimates may reflect more pessimistic employment data in our model, more optimistic mortality data, the exclusion of the cost of cancer deaths in individuals under age 20 in our model, and/or the differences in the methods used to estimate cost.
Death from lung cancer was the most costly—alone it accounted for more than a quarter of the total costs ($39 billion in 2010). Death from colon and rectum cancer was the second most costly ($12.8 billion in 2010), and death from female breast cancer was the third most costly ($10.9 billion in 2010). In addition to considering total costs, we reported costs per death by cancer site in 5-year age groups. These estimates highlight the impact of deaths in working-age individuals. For example, death from testicular cancer (approximately $1.3 million per death in 2010) was the most costly among men of working age, followed by death from Hodgkin lymphoma ($544 118 per death in 2010) among men and women of working age.
These estimates provide an order of magnitude assessment of the mortality costs of cancer and can be used by policymakers to decide how funds should be allocated among health care programs and between programs that focus on specific sites of cancer. Relative to many other diseases, the productivity cost due to cancer mortality is high. For example, the annual lost earnings due to premature influenza deaths in the United States are approximately $10.1 billion, and the annual cost of lost earnings due to deaths from diabetes is approximately $26.9 billion (20,21).
When we included the value of caregiving and household activities in the model, the costs increased to $232.4 billion in 2000 and to $308 billion in 2020. The inclusion of some or all of these costs is subject to debate. The argument unfolds as follows. Many Americans provide care to young children and disabled family members. Few of these caregivers are paid for their work (7,22) and the value of their services is not included in the GDP, which suggests that they should not be included in estimates of productivity loss. Nevertheless, without the services caregivers provide, these services would have to be purchased using paid labor. These services range from housekeeping, meal preparation, and transportation to complex medical tasks, medication administration, and assistance with ADLs (7,22), which are valuable to the US society. We note, however, that the estimates we use are from the NHAPS, which does not distinguish between activities performed as part of caregiving and activities performed for oneself. Activities performed as part of self-care may be considered “consumption” rather than production. For these reasons, we reported costs from paid wages in the base model and added imputed caregiving and housekeeping wages separately. We also included a more modest estimate of caregiving prevalence in the sensitivity analysis.
We focused our estimations on productivity costs, which are heavily influenced by working-age individuals and earnings. Estimates that use a value of life (estimated to be approximately $150 000 per year) as opposed to earnings report that costs from cancer mortality in 2000 were approximately $1031 billion (nearly nine times the value of productivity loss) (23). This method values each year of life lost equally ($150 000 per year)—without regard to age, employment probability, caregiving or housekeeping activity, or earnings.
Several limitations of this study are noteworthy. First, we used all-cause mortality to approximate other-cause mortality in estimating PYLL. Because all-cause mortality includes cancer deaths, the hazards of death are overstated, and as a result, the PYLL estimates are understated. The understatement is the greatest when using all-cause mortality to approximate other-cause mortality for all cancers. Second, we used life expectancy to estimate the years of life lost rather than using the conditional probability of living an additional year given survivorship to a particular age. However, the two methods yield estimates that differ by less than 5% (data not shown). Third, we did not include employment and earnings from the underground economy (eg, unreported income). Fourth, we did not include the productivity costs of those who died before the age of 20 and we did not include childhood cancers in our model. Finally, we did not include morbidity costs of cancer in our estimates. Patients are often disabled by cancer, especially in the final phases of life. In addition, one-third or more of cancer survivors leave the workforce altogether during the 6 months immediately following diagnosis (2), and, if they return, they often report work-related disabilities that prohibit them from performing their jobs at their pre-diagnosis capacity (24). Absenteeism among patients who remain employed can add up to several months or more, and in one study (25) cancer survivors had the greatest absenteeism rate relative to patients with other chronic diseases (26). Taken together, these limitations suggest that our estimations reflect the lower end of the range of the true productivity costs of cancer.
Estimates such as the ones provided here support the Institute of Medicine's recommendation that the National Institutes of Health strengthen its use of data that estimate the burden and cost of disease in setting its research priorities (27). Methods for reducing cancer mortality include primary prevention (eg, vaccines, risk factor modification), early detection of cancers for which successful treatment is most likely, and delivery of effective treatments. Decision makers can use the information we provide as a basis to assess the costs of interventions relative to their benefits to determine how to best allocate resources among these strategies. From a productivity loss perspective, investments in programs that reduce lung, breast, colorectal, leukemia, and/or pancreatic cancer mortality are likely to yield the largest annual reduction in productivity costs for US society.
Funding
This research was supported by National Cancer Institute contract with C. J. Bradley, PhD.
Footnotes
We thank Danielle Melbert and Martin Krapcho of Information Management Services, Inc for assistance in calculating and projecting cancer mortality rates, other causes of death, and PYLL.
The authors take full responsibility for the study design, data collection, analysis and interpretation of the data, the decision to submit the manuscript for publication, and the writing of the manuscript.
References
- 1.National Center for Health Statistics. Deaths—Leading Causes. http://www.cdc.gov/nchs/fastats/lcod.htm. Accessed August 2, 2007. [Google Scholar]
- 2.Bradley C, Neumark D, Luo Z, Schenk M. Employment and cancer: findings from a longitudinal study of breast and prostate cancer survivors. Cancer Invest. 2007;25(1):47–54. doi: 10.1080/07357900601130664. [DOI] [PubMed] [Google Scholar]
- 3.Edwards B, Brown M, Wingo P, et al. Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst. 2005;97(19):1407–1427. doi: 10.1093/jnci/dji289. [DOI] [PubMed] [Google Scholar]
- 4.Hodgson T, Meiners M. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Q. 1982;60(3):429–462. [PubMed] [Google Scholar]
- 5.Cooper B, Rice D. The economic cost of illness revisited. Soc Secur Bull. 1976;39(2):21–36. [PubMed] [Google Scholar]
- 6.Natl Vital Stat Rep. 2002;51(3):1–38. [PubMed] [Google Scholar]
- 7.Donelan K, Hill CA, Hoffman C, et al. Challenged to care: informal caregivers in a changing health system. Health Aff. 2002;21(4):222–231. doi: 10.1377/hlthaff.21.4.222. [DOI] [PubMed] [Google Scholar]
- 8.Max W, Rice DP, Sung H, Michel M. Valuing Human Life: Estimating the Present Value of Lifetime Earnings, 2000. Center for Tobacco Control Research and Education. Economic Studies and Related Methods. 2004. http://repositories.cdlib.org/ctcre/esarm/PVLE2000. Accessed January 21, 2008. [Google Scholar]
- 9.US Bureau of the Census. National Interim Projections. http://www.census.gov/ipc/www/usinterimproj/. Accessed June 19, 2007. [Google Scholar]
- 10.Berkeley Mortality Database. http://www.demog.berkeley.edu/∼bmd/states.html. Accessed June 3, 2005. [Google Scholar]
- 11.U.S. Department of Labor, Bureau of Statistics and U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau. Current Population Survey, Design and Methodology. Technical Paper TP63RV. http://www.bls.census.gov/cps/tp/tp63.htm. Accessed August 2, 2007. [Google Scholar]
- 12.Grosse S. Appendix I: productivity loss tables. In: Haddix A, Teutsch S, Corso P, editors. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. 2nd ed. New York: Oxford University Press; 2003. pp. 245–259. [Google Scholar]
- 13.National Alliance for Caregiving and the American Association of Retired Persons. Caregiving in the U.S. 2004 http://www.caregiving.org/data04execsum.pdf. Accessed October 9, 2008. [Google Scholar]
- 14.U.S. Department of Labor, Bureau of Statistics. Consumer Price Index. http://stats.bls.gov/cpi/home.htm#data. Accessed December 18, 2006. [Google Scholar]
- 15.Metlife Mature Market Institute. Metlife Market Survey of Nursing Home and Home Care Costs, 2005. http://www.metlife.com/WPSAssets/41453139101127828650V1F2005%20NH%20and%20HC%20Market%20Survey.pdf. Accessed October 9, 2008. [Google Scholar]
- 16.National Center for Health Statistics. National Nursing Home Survey. Atlanta, GA: Centers for Disease Control; http://www.cdc.gov/nchs/about/major/nnhsd/ResidentTables_Estimates.htm#PaymentSource. Accessed October 9, 2008. [Google Scholar]
- 17.U.S. Department of Commerce, Bureau of Economic Analysis. National Income and Products Accounts Table. http://www.bea.gov/national/nipaweb/TableView.asp?SelectedTable=5&ViewSeries=NO&Java=no&Request3Place=N&3Place=N&FromView=YES&Freq=Year&FirstYear=2007&LastYear=2008&3Place=N&Update=Update&JavaBox=no#Mid. Accessed June 19, 2008. [Google Scholar]
- 18.National Cancer Institute. National Cancer Institute (NCI) Fact Book, 2007. http://obf.cancer.gov/financial/attachments/07Factbk.pdf. Accessed June 19, 2008. [Google Scholar]
- 19.National Institutes of Health. National Heart, Lung, Blood Institute Fact Book, 2007. http://www.nhlbi.nih.gov/about/factbook/FactBookFinal.pdf. Accessed June 19, 2008. [Google Scholar]
- 20.Molinari NM, Ortega-Sanchez IR, Messonnier JL, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Economic cost of diabetes in the U.S. in 2007. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 22.Johnson R, Schaner S. Many Older Americans Engage in Caregiving Activities. Perspectives on Productive Aging. The Urban Institute. http://www.urban.org/publications/311203.html. Accessed July 14, 2008. [Google Scholar]
- 23.Yabroff KR, Bradley CJ, Mariotto AB, Brown ML, Feuer EJ. Value of life lost due to early death from cancer. J Natl Cancer Inst. 2008;100(24):1755–1762. doi: 10.1093/jnci/djn383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Short PF, Vasey JJ, Belue R. Work disability associated with cancer survivorship and other chronic conditions. Psychooncology. 2008;17(1):91–97. doi: 10.1002/pon.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradley C, Oberst K, Schenk MJ. Absenteeism from work: experiences of employed breast and prostate cancer patients 6 months following diagnosis. Psychooncology. 2005;15(8):739–747. doi: 10.1002/pon.1016. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Greenberg PE, Mickelson KD, et al. The effect of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43(3):218–225. doi: 10.1097/00043764-200103000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine. Scientific Opportunities and Public Needs: Improving Priority Setting and Public Input at the National Institutes of Health. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]