Abstract
BACKGROUND:
Rectal thermometry correlates with core temperature and represents the criterion standard of measuring temperatures in young children. However, it has numerous disadvantages, and thus, an alternative method of measuring temperature with similar agreement with the core temperature as rectal thermometry is desired. A new, noninvasive temporal artery (TA) thermometer synthesizes the skin surface and ambient temperatures to produce an arterial temperature.
OBJECTIVE:
To examine the agreement between the TA and esophageal core thermometers, and to compare it with that between rectal and esophageal temperatures.
METHODS:
In the present prospective, cross-sectional agreement study, intubated surgical outpatients younger than 18 years of age had temperatures measured with esophageal and rectal probes, and rectal electronic and TA thermometers. The agreement between esophageal versus rectal and TA thermometers was analyzed by intraclass correlation coefficients and by differences between esophageal versus TA and rectal temperatures with 95% CIs. The esophageal-rectal and esophageal-TA slopes were compared by Student’s t test.
RESULTS:
In 80 enrolled children, the intraclass correlation coefficients for the esophageal probe versus rectal probe, rectal electronic thermometer and TA thermometer were 0.91, 0.95 and 0.88, respectively. The mean esophageal-rectal difference was 0.00±0.18°C and esophageal-TA difference was 0.14±0.20°C. Linear regression analysis of the relation between esophageal probe versus rectal probe, rectal thermometer and TA thermometer yielded slopes of 0.93, 0.94 and 0.89, respectively. The slopes were neither different from each other (P=0.70) nor from the value of 1.
CONCLUSION:
The TA and esophageal thermometers agree well, and the esophageal-TA and esophageal-rectal temperature agreements are not significantly different.
Keywords: Esophageal thermometry, Infants, Rectal thermometry, Temperature, Temporal artery thermometry
Abstract
HISTORIQUE :
La thermométrie rectale correspond à la température centrale et représente la norme évaluative de mesure des températures chez les jeunes enfants. Cependant, elle comporte de nombreux inconvénients. C’est pourquoi un autre mode de mesure de la température est souhaité, qui concorde autant avec la température centrale qu’avec la thermométrie rectale. Un nouveau thermomètre de l’artère temporale (AT), moins effractif, analyse la surface de la peau et la température ambiante pour la synthétiser en température artérielle.
OBJECTIF :
Analyser la concordance entre le thermomètre de l’AT et le thermomètre central de l’œsophage et la comparer avec celle entre les températures rectale et œsophagienne.
MÉTHODOLOGIE :
Dans la présente étude de concordance prospective et transversale, des opérés ambulatoires intubés de moins de 18 ans faisaient prendre leur température au moyen de sondes œsophagienne et rectale et de thermomètres électronique rectal et de l’AT. La concordance entre les thermomètres œsophagien, rectal et de l’AT a été analysée au moyen de coefficients de corrélation intraclasse et des différences entre la température œsophagienne et celles de l’AT et du rectum selon des IC de 95 %. Les pentes entre les températures de l’œsophage et du rectum et entre la température de l’œsophage et de l’AT ont été comparées d’après le test de Student.
RÉSULTATS :
Chez les 80 enfants participants, les coefficients de corrélation intraclasse de la sonde œsophagienne par rapport à la sonde rectale, au thermomètre électronique rectal et au thermomètre de l’AT étaient de 0,91, 0,95 et 0,88, respectivement. La différence moyenne entre les températures œsophagienne et rectale s’élevait à 0,00±0,18 °C et celle entre les températures de l’œsophage et de l’AT, à 0,14±0,20 °C. L’analyse de régression linéaire de la relation entre la sonde œsophagienne par rapport à la sonde rectale, au thermomètre rectal et au thermomètre de l’AT a donné des pentes de 0,93, 0,94 et 0,89, respectivement. Les pentes n’étaient ni différentes l’une de l’autre (P=0,70) ni par rapport à la valeur 1.
CONCLUSION :
Les thermomètres de l’AT et de l’œsophage concordent bien, et les concordances entre les températures de l’œsophage et de l’AT et celles de l’œsophage et du rectum ne différaient pas de manière considérable.
Temperature measurement constitutes an important aspect of paediatric health care. Ideally, temperature measurement should be accurate, noninvasive, time efficient and relatively technique-independent. It should also closely reflect the core body temperature. None of the current thermometry methods meet all these criteria and the search continues for an improved way of measuring temperatures in children.
The temperature of the central organs is best reflected by the core temperature measured in the pulmonary artery. The distal esophagus has also been found to be an accurate site for core temperature determination (1,2). However, these invasive thermometry methods are limited to the intensive care unit (ICU) and/or operating room settings. Therefore, other methods of thermometry using various peripheral body sites are used as core temperature approximations. Several adult and paediatric studies have demonstrated closer agreement between the core temperature taken in the pulmonary artery and rectal temperature than those taken in the axilla, the ear or the mouth (3–6). The rectal method has therefore been considered the criterion standard for measuring temperature in infants (7). However, rectal thermometry is time consuming, uncomfortable (8,9) and contraindicated in immunosuppressed children (10). Thus, it is inconvenient to use in busy clinical settings, such as triage in paediatric emergency departments (EDs). Another, more user-friendly method of thermometry that meets the aforementioned criteria is therefore desired.
A new type of thermometry based on infrared arterial temperature measurement has recently been developed. This method automatically synthesizes the skin surface temperature and the ambient temperature to produce an arterial temperature. Recent evaluations of the temporal artery (TA) thermometer in the ED setting have yielded disparate results. While one study found the sensitivity of the TA device for detecting rectal fever to be only 66% (11), another ambulatory study found this thermometer to be an effective screening device (12). However, no published paediatric study to date has examined the agreement between TA temperatures and core temperatures measured either in the pulmonary artery or in the esophagus.
The objective of the present study was to examine the agreement between the esophageal criterion standard and TA temperature measurements and to investigate if this correlation was significantly lower than that between esophageal and rectal temperature readings. The present study represents the first validation component for TA thermometry and is a prerequisite for further evaluation of this new technology.
METHODS
Patient population
The study population comprised children who were undergoing elective dental surgery requiring endotracheal tube placement. Exclusion criteria included an abnormal esophageal or anorectal anatomy, immunosuppression, disturbances of thermoregulation and family history of malignant hyperthermia. Patients requiring spinal/epidural anesthesia, heating blankets or use of high flow/high humidity inspired gases, and those requiring induction of hypothermia, were also excluded. The study was approved by the Human Research Ethics Board of The Hospital for Sick Children and written consent was obtained from each patient’s parents.
Study design
The present study was a cross-sectional agreement study. Eligible children had their temperatures measured simultaneously by a single esophageal temperature probe (Tele-Thermometer, YSI Incorporated, USA), rectal temperature probe (Tele-Thermometer, YSI Incorporated, USA) and TA thermometer (Temporal Scanner, model LXTA, Exergen Corporation, USA). One-half of the study patients also had their temperature measured with an electronic rectal thermometer (IVAC 2000, ALARIS Medical Systems, USA). Temperatures were measured immediately after thermometer placement, 30 s and 60 s later to establish reliability and one to three more times at 15 min to 30 min intervals, depending on the length and conditions of the procedure. Temperature readings with the electronic rectal thermometer were only taken at baseline and at the end of the procedure. TA measurements were obtained on both sides of the head to establish reliability.
Temperature measurements
Before the study, the study nurse was trained by the manufacturer in the use of the TA thermometer and by the collaborating staff anesthetist in measuring temperatures via the temperature probes. All esophageal measurements were taken using a single esophageal probe, which was inserted by the staff anesthetist behind the heart using the auscultatory method. The rectal readings were obtained by inserting the instrument 6 cm into the rectum. The TA temperature readings were obtained by moving the probe slowly from the centre of the forehead into the hairline over the temporal region, while the probe was in continuous contact with the skin.
Outcome measures
The comparison of the agreement in temperatures taken by the esophageal probe versus rectal probe, rectal thermometer and TA thermometer at the end of the operative procedure was the primary outcome measure. Because it takes several minutes for the esophageal and rectal probes to stabilize, and because all study children had all three temperatures taken at the end of the procedure, the final measurement was chosen as the primary outcome measure. Comparisons were also made during the operative procedure starting 10 min to 15 min after insertion of the probes to allow for stabilization of the instruments, and these measurements were considered secondary outcomes.
Analysis
The calculated sample size was based on the 95% CI for the estimated intraclass correlation coefficient (ICC) between the esophageal and TA temperature readings of 0.8 and α=0.05 (13). A standard nomogram yields a minimum sample size of 75 children. The ICC was used to examine the reliability of the TA thermometer and to determine the agreement between temperature readings taken by the esophageal probe and those taken using other thermometers. An ICC of 0.8 or greater was defined as representing excellent agreement, while an ICC of 0.6 or greater represented good agreement (14). A linear regression analysis was used to determine the slope and the intercept of the relationship between the esophageal probe versus the TA thermometer, rectal probe and rectal thermometer temperature measurements. Regression lines were thus generated by these regression models. In addition, Student’s t test was performed to compare the slopes of each of the regression lines with a value of 1 (using a critical P of 0.017 to adjust for multiple testing) to examine if the rectal and TA readings were significantly different from the esophageal temperature readings. The regression slopes were also compared with each other using the Student’s t test to examine if the esophageal versus rectal and esophageal versus TA correlations were significantly different from each other. The mean esophageal-rectal and esophageal-TA differences with observed 95% CIs were examined to determine the temperature ranges within which 95% of the measured differences lay, and the predicted 95% CIs around the mean differences were also calculated to assess the likelihood of the true estimate of the temperature differences falling within the observed range.
RESULTS
Between November 2001 and June 2002, 80 children were enrolled. Their mean age (±SD) was 45±35 months and the majority was undergoing elective dental procedures. Two children were febrile and they were operated on after an assessment in the ED for acute appendicitis. Temperature measurements taken at the end of the procedure were 36.6±0.4°C with the esophageal probe, 36.6±0.4°C with the rectal probe, 36.7±0.3°C with the rectal thermometer, and 36.7±0.4°C with the TA thermometer.
Agreement between right and left TA temperatures
The ICC for the right versus left TA temperatures was 0.90 at time 0, 0.92 at 30 s and 0.91 at 60 s. A paired sample Student’s t test found no significant difference between right-and left-sided TA temperatures (P>0.05).
Agreement between esophageal and rectal or TA temperatures
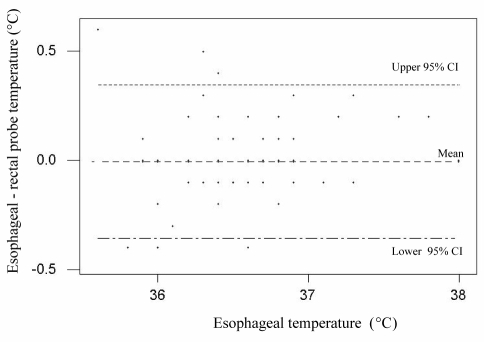
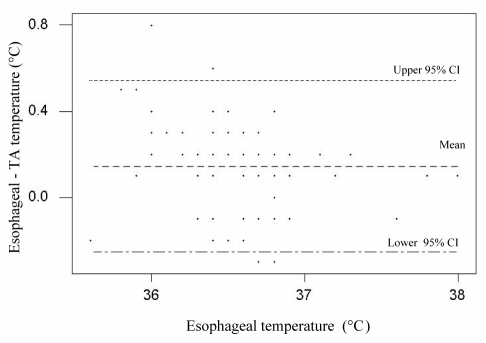
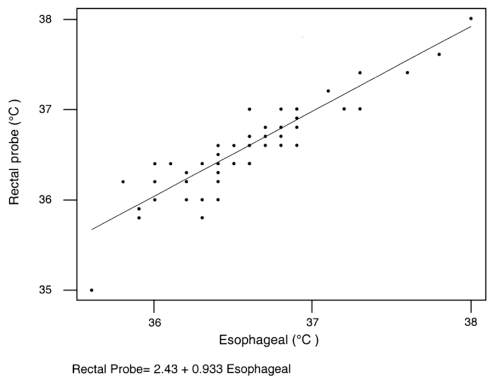
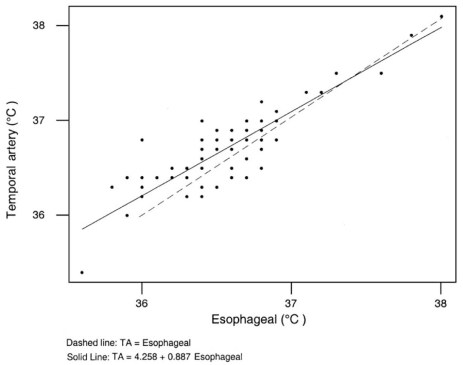
Differences between esophageal temperature readings and those taken with the other study thermometers during the procedure are summarized in Table 1. The 95% CIs of the differences were comparable throughout the observation period. The Bland-Altman plots of the esophageal-rectal and esophageal-TA differences versus the esophageal reference standard taken during the final measurement show that 95% of the differences lie within 0.72°C and 0.80°C, respectively (Figures 1 and 2). Table 2 shows ICCs reflecting excellent agreement between esophageal temperatures and temperatures taken by the other thermometers. A linear regression analysis of the relation between esophageal versus rectal probe temperatures yielded a slope of 0.93 and an r of 0.91 (Figure 3). The slopes and the r-values for the esophageal versus rectal thermometer temperatures were 0.94 and 0.95, respectively, and for the esophageal versus TA temperatures the slope was 0.89 and r was 0.88 (Figure 4).
TABLE 1.
Temperature differences between esophageal and other measurement methods during operative procedure with observed and predicted 95% CIs
| Time* | Esophageal minus rectal probe (°C) | Esophageal minus rectal thermometer† (°C) | Esophageal minus temporal artery (°C) |
|---|---|---|---|
| 10–30 min (n=52) (mean ± SD) | 0.14±0.30 | −0.11±0.21 | |
| Observed 95% CI | −0.46 to 0.74 | −0.53 to 0.31 | |
| Predicted 95% CI | 0.05 to 0.22 | −0.17 to −0.05 | |
| 31–60 min (n=10) (mean ± SD) | 0.08±0.17 | −0.26±0.20 | |
| Observed 95% CI | −0.26 to 0.42 | −0.66 to 0.14 | |
| Predicted 95% CI | −0.03 to 0.19 | −0.39 to −0.13 | |
| Final‡ (n=80) (mean ± SD) | −0.00±0.18 | −0.05±0.10 | 0.14±0.20 |
| Observed 95% CI | −0.36 to 0.36 | −0.25 to 0.15 | −0.54 to 0.26 |
| Predicted 95% CI | −0.04 to 0.04 | −0.08 to −0.02 | −0.18 to −0.10 |
Postintubation;
n=40 for rectal thermometer measurements;
Refers to measurement at the end of the procedure, time depends on length of procedure (65±21 min, range 25 min to 120 min)
Figure 1).
Bland-Altman plot of the esophageal-rectal temperature difference versus the esophageal reference standard. Because the esophageal-rectal temperature differences were the same in many patients, numerous points on this graph represent more than one patient
Figure 2).
Bland-Altman plot of the esophageal-temporal artery (TA) temperature difference versus the esophageal reference standard. Because the esophageal-TA correlations were the same in many patients, numerous points on this graph represent more than one patient
TABLE 2.
Intra-class correlation coefficients for agreement between esophageal temperatures versus rectal and temporal artery temperatures during operative procedures
| Time* | Esophageal versus rectal probe | Esophageal versus rectal thermometer† | Esophageal versus temporal artery |
|---|---|---|---|
| 10–30 min (n=52) | 0.77 | 0.83 | |
| 95% CI | 0.63 to 0.86 | 0.72 to 0.90 | |
| 31–60 min (n=10) | 0.93 | 0.88 | |
| 95% CI | 0.79 to 0.98 | 0.60 to 0.97 | |
| 61–120 min (n=39) | 0.91 | 0.82 | |
| 95% CI | 0.83 to 0.95 | 0.62 to 0.91 | |
| Final‡ (n=80) | 0.91 | 0.95 | 0.88 |
| 95% CI | 0.86 to 0.94 | 0.91 to 0.97 | 0.82 to 0.92 |
Postintubation;
n=40 for rectal thermometer measurements;
Refers to measurement at the end of the procedure, time depends on length of procedure (65±21 min, range 25 min to 120 min)
Figure 3).
Scatter plot of the rectal versus esophageal temperatures. Because the esophageal-temporal artery difference was the same in many patients, numerous points on this graph represent more than one patient
Figure 4).
Scatter plot of the temporal artery (TA) versus esophageal temperatures. Because the esophageal-TA correlations were the same in many patients, numerous points on this graph represent more than one patient
Neither slope was significantly different from 1 (esophageal versus TA, P=0.03; esophageal versus rectal, P=0.46; and esophageal versus rectal probe, P=0.24 [significance level of 0.017]). This indicates that neither the rectal nor the TA temperatures were significantly different from the esophageal readings and that the TA thermometer predicted the core body temperature determined by the esophageal temperatures as well as the rectal instruments. The slopes did not significantly differ from one another (P=0.70), meaning that the rectal temperatures were not significantly closer to the esophageal temperatures than to the TA temperatures.
DISCUSSION
The present study suggests that the measured TA temperatures in afebrile children were not significantly different from the esophageal reference standard. In this setting, rectal and TA temperature comparisons with the esophageal standard were similar.
To our knowledge, these are the first published data on validation of the TA method of thermometry against an esophageal reference standard. A recent ICU study of patients recovering from cardiopulmonary bypass found poor agreement between the TA device (SensorTouch, Philips Inc, Netherlands) and core temperature measurements in adults and only a modest agreement in children (15). However, this study (15) was limited by a small sample size, the use of bladder temperatures, which do not represent true core measurements, and an analysis of repeated measurements on the same subjects as independent data. During early recovery from cardiopulmonary bypass, the temperatures in the bladder and TA may be different and may therefore augment disagreement between the measurements.
The high degree of agreement between the rectal and esophageal temperatures in the present study’s population, parallels the results of several previous studies (3–6). These studies were done in the ICU setting and have shown that core temperatures taken in the pulmonary artery agreed well with those taken rectally, in both afebrile and febrile patients, thereby establishing rectal thermometry as a reasonable clinical reference standard. The bias for each thermometer is reflected in the calculated difference in the mean core reference temperature and the mean temperature of the other instruments. Ideally, the mean bias for each method pair should be zero. In the present study, the rectal and TA thermometers differed from core esophageal temperatures by a small, clinically insignificant amount. The variability of temperature measurements around this bias is reflected by the SD, which ultimately determines the usefulness of a new thermometry method. Our results show that the observed SDs of the mean differences were comparable throughout the procedure. The calculated predicted 95% CIs around the mean differences describe how confidently we can predict the esophageal core temperature in an individual patient using the rectal and TA methods. The narrower the 95% CIs are around the new method’s prediction, the more useful the new method is as an alternative to a reference standard (4). The axillary and tympanic methods, both of which miss large numbers of fevers in children (8,9,16–21), have been found to be significantly worse approximations of core temperatures than the rectal method (4,22,23). The calculated predicted 95% CIs in our study were narrow, indicating a high degree of likelihood that the true estimate of the differences between the thermometers would fall within this range.
Several authors have previously suggested that the rectum may be a physiologically suboptimal site for measuring core temperature because of its relatively high insulation (24). Indeed, the rectum has been shown to respond slowly to rapid changes in core body temperature in adults and children (25–29). Because our subjects were at low risk of marked core temperature changes, we were not in a position to demonstrate this. Studies comparing changes in esophageal versus rectal and TA temperatures in children undergoing major changes in core body temperature would be of interest to further validate the TA thermometer.
The vast majority of our study population was afebrile and over one year of age; therefore, we were unable to prove the generalizability of our results to young, febrile children. This was a pilot study, which represents the first step in the evaluation of the TA thermometry across a spectrum of children with varying degrees of temperature elevation or depression.
CONCLUSION
The temperatures taken by the TA device and the rectal thermometers appear to be in good agreement with the core temperatures measured in the esophagus in afebrile children. The agreement between esophageal and TA temperatures is not significantly different from that between esophageal and rectal temperatures.
Acknowledgments
The authors thank their medical and nursing colleagues for their support, and Diana Cristea for typing this manuscript.
Footnotes
FUNDING: Supported by an investigator initiated grant from Exergen Corporation, USA.
REFERENCES
- 1.Shoemaker WC, Holbrook PR. Accidental hypothermia. In: Elder P, editor. Textbook of Critical Care Medicine. Philadelphia: WB Saunders; 1984. pp. 85–93. [Google Scholar]
- 2.Hayward JS, Eckerson JD, Kemna D. Thermal and cardiovascular changes during three methods of resuscitation from mild hypothermia. Resuscitation. 1984;11:21–33. doi: 10.1016/0300-9572(84)90031-5. [DOI] [PubMed] [Google Scholar]
- 3.Milewski A, Ferguson KL, Terndrup TE. Comparison of pulmonary artery, rectal and tympanic membrane temperatures in adult intensive care unit patients. Clin Pediatr. 1991;30:13–6. doi: 10.1177/0009922891030004S05. [DOI] [PubMed] [Google Scholar]
- 4.Romano MJ, Fortenberry JD, Autrey E, et al. Infrared tympanic thermometry in the pediatric intensive care unit. Crit Care Med. 1993;21:1181–5. doi: 10.1097/00003246-199308000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Stavem K, Saxholm H, Smith-Erichsen N. Accuracy of infrared ear thermometry in adult patients. Intens Care Med. 1997;23:100–5. doi: 10.1007/s001340050297. [DOI] [PubMed] [Google Scholar]
- 6.Schmitz T, Bair N, Falk M, Levine C. A comparison of five methods of temperature measurement in febrile intensive care patients. Am J Crit Care. 1995;4:286–92. [PubMed] [Google Scholar]
- 7.Baraff LJ, Bass JW, Fleisher GR. Practice guideline for the management of infants and children 0 to 36 months of age with fever without source. Agency for Health Care Policy and Research. Ann Emerg Med. 1993;22:1198–210. doi: 10.1016/s0196-0644(05)80991-6. Erratum in: Ann Emerg Med 1993;22:1490. [DOI] [PubMed] [Google Scholar]
- 8.McDonald R. Objection to taking rectal temperatures. Clin Pediatr. 1968;7:707. doi: 10.1177/000992286800701204. [DOI] [PubMed] [Google Scholar]
- 9.McCaffery M. Children’s responses to rectal temperatures: An exploratory study. Nurs Res. 1971;20:32–45. [PubMed] [Google Scholar]
- 10.Schimpff SC, Wiernik PH, Block JB. Rectal abscesses in cancer patients. Lancet. 1972;2:844–7. doi: 10.1016/s0140-6736(72)92210-6. [DOI] [PubMed] [Google Scholar]
- 11.Greenes DS, Fleisher GR. Accuracy of a noninvasive temporal artery thermometer for use in infants. Arch Pediatr Adolesc Med. 2001;155:376–81. doi: 10.1001/archpedi.155.3.376. [DOI] [PubMed] [Google Scholar]
- 12.Siberry GK, Diener-West M, Schappell E, Karron RA. Comparison of temple temperatures with rectal temperatures in children under two years of age. Clin Pediatr. 2002;41:405–14. doi: 10.1177/000992280204100605. [DOI] [PubMed] [Google Scholar]
- 13.Streiner DL, Norman GR. Health Measurement Scales. 2nd edn. United Kingdom: Oxford University Press; 1998. [Google Scholar]
- 14.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 15.Suleman MI, Doufas AG, Akca O, Ducharme M, Sessler DI. Insufficiency in a new temporal-artery thermometer for adult and pediatric patients. Anesth Analg. 2002;95:67–71. doi: 10.1097/00000539-200207000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Yetman RJ, Coody DK, West MS, Montgomery D, Brown M. Comparison of temperature measurements by an aural infrared thermometer with measurements by traditional rectal and axillary techniques. J Pediatr. 1993;122:769–73. doi: 10.1016/s0022-3476(06)80024-7. [DOI] [PubMed] [Google Scholar]
- 17.Barber N, Kilmon CA. Reactions to tympanic temperature measurement in an ambulatory setting. Pediatr Nurs. 1989;15:477–81. [PubMed] [Google Scholar]
- 18.Frank JD, Brown S. Thermometers and rectal perforations in the neonate. Arch Dis Child. 1978;53:824–5. doi: 10.1136/adc.53.10.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau JT, Ong GB. Broken and retained rectal thermometers in infants and young children. Aust Paediatr J. 1981;17:93–4. doi: 10.1111/j.1440-1754.1981.tb01912.x. [DOI] [PubMed] [Google Scholar]
- 20.Ficarra BJ. Rectal thermometer misplaced. Am J Proctol. 1970;21:212–4. [PubMed] [Google Scholar]
- 21.Merenstein GB. Rectal perforation by thermometer. Lancet. 1970;1:1007. doi: 10.1016/s0140-6736(70)91139-6. [DOI] [PubMed] [Google Scholar]
- 22.Nierman DM. Core temperature measurement in the intensive care unit. Crit Care Med. 1991;19:818–23. doi: 10.1097/00003246-199106000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Shinozaki T, Deane R, Perkins FM. Infrared tympanic thermometer: Evaluation of a new clinical thermometer. Crit Care Med. 1988;16:148–50. doi: 10.1097/00003246-198802000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Rotello LC, Crawford L, Terndrup TE. Comparison of infrared ear thermometer derived and equilibrated rectal temperatures in estimating pulmonary artery temperatures. Crit Care Med. 1996;24:1501–6. doi: 10.1097/00003246-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Mead J, Bonmarito CL. Reliability of rectal temperatures as an index of internal body temperature. J Appl Physiol. 1949;2:97–109. doi: 10.1152/jappl.1949.2.2.97. [DOI] [PubMed] [Google Scholar]
- 26.Grayson J. Observations on the temperature of the human rectum. BMJ. 1951;2:1379–92. doi: 10.1136/bmj.2.4744.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buck SH, Zaritsky AL. Occult core hyperthermia complicating cardiogenic shock. Pediatrics. 1989;83:782–4. [PubMed] [Google Scholar]
- 28.Cranston WI, Gerbrandy J, Snell ES. Oral, rectal, and esophageal temperatures and some factors affecting them in man. J Physiol. 1954;126:347–58. doi: 10.1113/jphysiol.1954.sp005214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Molnar G, Read R. Studies during open-heart surgery on the special characteristics of rectal temperature. J Appl Physiol. 1974;36:333–6. doi: 10.1152/jappl.1974.36.3.333. [DOI] [PubMed] [Google Scholar]