Abstract
Background
The current study was designed to examine the cross-sectional association between perceived discrimination and blood pressure (BP) in a sample of older African American and white adults. We hypothesized that perceived discrimination would be associated with higher levels of BP and that this association would be stronger for older African Americans compared with whites.
Methods
Participants were 4,694 (60% African American, 60% women) community-dwelling older adults. Perceived discrimination and other relevant risk factors were assessed via interview, and BP was measured using standard sphygmomanometers. Multivariate linear regression models were conducted to test associations among race, perceived discrimination, and BP.
Results
In models adjusted for age, sex, race, and education, perceived discrimination was not associated with higher levels of systolic blood pressure (p = .10) but was associated with higher levels of diastolic blood pressure (DBP) (p = .01). Further analyses revealed that the association between perceived discrimination and DBP was present in older African Americans (p = .0003) but not whites (p = .46). Results persisted after adjusting for relevant risk factors.
Conclusions
Findings suggest that discrimination may be a unique risk factor for elevated DBP in older African Americans. Because these findings are cross-sectional, additional research is needed to determine whether the observed associations persist over time.
Keywords: Discrimination (psychology), Blood pressure, African Americans, Whites, Aging, Prejudice
ELEVATED blood pressure (BP) is a risk factor for a wide variety of illnesses, including heart disease, stroke, and end-stage renal disease (1–3). Studies have consistently observed higher rates of elevated BP in African Americans compared with (non-Hispanic) white adults (4,5), and these disparities persist into older age (4,6). Many factors are believed to contribute to racial disparities in elevated BP, including black–white differences in socioeconomic status (SES; 7), obesity (5,7), and negative health behaviors (e.g., lack of exercise; 8).
Researchers have also examined the role of perceived discrimination as a possible risk factor for elevated BP in African Americans (9–13). Self-reported rates of discriminatory treatment are significantly higher in African Americans compared with whites (14–16) and are believed to contribute to black–white disparities in health (17). Although some studies have observed positive associations between discrimination and BP (10–12,18,19), others have reported null findings (14,20), with negative associations observed in certain subgroups (9,13).
To date, most studies examining the association between discrimination and BP have been conducted in samples of adolescents or young- to middle-aged African American and white adults (9,12–14,19). To our knowledge, no studies have investigated this association in samples of older African Americans. Discrimination may have particular relevance for older African Americans, many of whom came of age at a time when discriminatory treatment was legal, and for the most part sanctioned, in the United States (21). African Americans of this generation may be particularly sensitive to discriminatory treatment and consequently more vulnerable to its negative health effects.
The current study was designed to examine the association between perceived discrimination and BP in a sample of community-dwelling older African American and white adults. We hypothesized that (i) perceived discrimination would be associated with higher levels of systolic blood pressure (SBP) and diastolic blood pressure (DBP) and that (ii) this association would be stronger for African Americans compared with whites.
METHODS
Participants were from the Chicago Health and Aging Project (CHAP), an ongoing, population-based longitudinal study of risk factors for Alzheimer's disease and other conditions of aging. CHAP includes a large number of African Americans and non-Hispanic whites living in a single geographically defined area with a broad representation of SES within each racial/ethnic group. Details of the CHAP study design have been previously reported (22). Briefly, the CHAP study began with a complete census of all households across three contiguous areas on the south side of Chicago, Illinois. All residents aged 65 and older were asked to participate, and 6,158 enrolled as original cohort participants, for an overall participation rate of 78.9%. Between 1993 and 1996, all participants received an in-home, face-to-face interview that was repeated in 3-year cycles. Beginning with the third interview cycle (2000–2002), CHAP added new participants to the cohort consisting of area residents who had attained the age of 65 since the inception of the study. These successive cohort participants received the same baseline interview as the original cohort and are also reinterviewed at 3-year intervals. The discrimination measure was added to the second interview (1997–1999) for participants of the original cohort but was included in the first (baseline) interview for successive cohort participants. Data from these two sources were combined for the present analysis.
Data were available from a total of 7,195 participants, of whom 2,205 (30.7%) were excluded due to not having a same-race interviewer. This was done for methodological reasons. In previous analyses using the perceived discrimination measure in this cohort, there were substantial “race-of-interviewer” effects on discrimination scores, with participants reporting significantly lower levels of discrimination when interviewed by a person of a different racial background (16,23). This is consistent with other research (24,25), which suggests that questions about current levels of discrimination and unfair treatment are the most sensitive to race-of-interviewer effects, with effects being particularly pronounced for African Americans (24). To reduce the potential bias associated with race-of-interviewer effects, we restricted our analyses to participants with a same-race interviewer. Of these remaining 4,990 participants, an additional 296 (5.9%) were excluded because of missing data on discrimination or BP outcomes. The final sample consisted of 4,694 participants: 3,031 from the original CHAP cohort and 1,663 from the successive cohort.
Study procedures were approved by the Institutional Review Board of Rush University Medical Center. All participants provided written, informed consent.
Measures
Perceived discrimination.—
Perceived discrimination was assessed with the Everyday Discrimination scale (15). This 9-item scale asks participants to indicate the frequency with which they experienced various forms of interpersonal mistreatment in their day-to-day lives. Examples include “You are treated with less respect than other people” and “You receive poorer service than other people at restaurants or stores.” Items are framed in the context of general mistreatment, without reference to race, age, etc., and are assessed with a 4-point scale (0 = never, 1 = rarely, 2 = sometimes, and 3 = often). As in other studies (14), responses were recoded to a binary format (often or sometimes = 1 and rarely or never = 0) and then summed across items to obtain the total score (range 0–9). This scale has been previously validated in CHAP with good reliability (16).
Blood pressure.—
BP was measured using standard procedures (26). Two consecutive BP readings were taken with 30 seconds between measurements, using standard sphygmomanometers on seated participants. The average of the two measurements was recorded. SBP and DBP were modeled continuously in all analyses.
Covariates.—
Race was self-reported as non-Hispanic African American or non-Hispanic white. Age was assessed via self-reported date of birth. Education was measured in years. Cigarette smoking was quantified in pack-years, using questions from the Established Populations for Epidemiologic Studies of the Elderly (EPESE) project (27). Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (28). Information on physician-diagnosed heart disease, stroke, and/or diabetes was self-reported using standardized questions from EPESE (27). Antihypertensive medication use was established by direct inspection of all medications participants used during the 2-week period preceding the interview. With three exceptions (race, physician-diagnosed diseases, and antihypertensive use), covariates were modeled continuously in all analyses.
Statistical Analyses
Descriptive statistics were used to characterize the sample on demographics, risk factors, and BP variables at baseline. We then fit cross-sectional, linear regression models, modeling baseline BP levels as a function of perceived discrimination and potential confounders. Our primary model (Model 1) tested the association between perceived discrimination and BP, after adjusting for age, sex, race, and education. Model 2 added a term for the discrimination by race interaction to test whether the effect of discrimination differed between African Americans and whites. In Model 3, we added additional control variables for smoking, BMI, and physician-diagnosed diseases. Separate models were fit for SBP and DBP. All models were adjusted for antihypertensive medication use. In sensitivity analyses, we also ran models excluding individuals on antihypertensive medications and results were similar. Because the discrimination variable was slightly skewed, we also ran additional analyses after recoding it into four categories (0, 1, 2–3, and ≥4). Results were similar to those using the continuous discrimination variable; thus, to remain consistent with prior research in this area, the continuous variable was retained in all analyses.
Following this, we ran a series of exploratory analyses to determine whether any observed associations between discrimination and BP differed by education, age, or gender. None of the interaction terms were significant; thus, they were not included in our final models. All models were computed using sas, Version 9.1.3 (29).
RESULTS
Participant Characteristics
Sample characteristics for the full sample and by race are presented in Table 1. The sample was 60% African American and 60% women. On average, participants were 74.1 years old (standard deviation [SD] = 6.7) with 12.4 years (SD = 3.5) of education. The average discrimination score was 1.01 (SD = 1.6), and approximately 30% of participants were on antihypertensive medications. Mean SBP was 134.6 mm/Hg (SD = 17.2), and mean DBP was 77.9 mm/Hg (SD = 10.9).
Table 1.
Participant Characteristics for the Total Sample and by Race
| Characteristics | Total (N = 4,694) | African Americans (N = 2,826) | Whites (N = 1,868) | p Value |
| Age | 74.1 (6.7) | 72.9 (5.9) | 75.8 (7.3) | <.0001 |
| Women (%) | 60.0 | 59.2 | 60.7 | .32 |
| Education (years) | 12.4 (3.5) | 11.2 (3.3) | 14.2 (3.2) | <.0001 |
| Discrimination | 1.0 (1.6) | 1.3 (1.8) | .62 (1.17) | <.0001 |
| Antihypertensive use (%) | 29.9 | 32.1 | 26.7 | <.0001 |
| SBP (mm/Hg) | 134.6 (17.2) | 135.4 (16.3) | 133.5 (18.5) | .001 |
| DBP (mm/Hg) | 77.9 (10.9) | 79.8 (10.5) | 74.9 (10.8) | <.0001 |
| BMI (kg/m2) | 27.6 | 28.5 (6.3) | 26.3 (5.2) | <.0001 |
| Smoking (pack-years) | 15.0 | 13.2 (22.9) | 17.5 (30.2) | <.0001 |
| Diabetes (%) | 6.4 | 8.6 | 3.2 | <.0001 |
| Heart disease (%) | 14.1 | 14.3 | 13.9 | .68 |
| Prior stroke (%) | 6.9 | 7.9 | 5.4 | .001 |
Note: Values are mean (SD) or percentage. BMI = body mass index; DBP = diastolic blood pressure; SBP = systolic blood pressure.
Compared with whites, African Americans were younger, less educated, reported more discrimination, and had higher SBP and DBP (see Table 1). African Americans also had higher BMIs, were more likely to be on antihypertensive medications, and were more likely to report a history of diabetes and/or stroke than whites. Conversely, African Americans reported fewer pack-years of smoking than whites.
Perceived Discrimination and BP
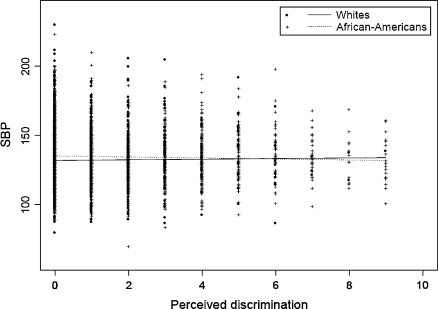
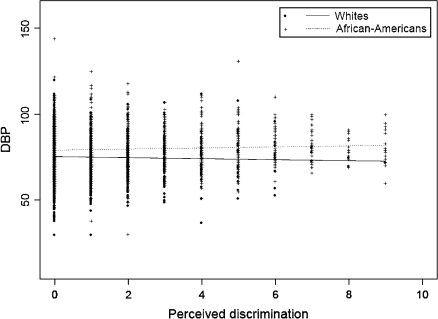
The bivariate associations between perceived discrimination and BP for African Americans and whites are presented as scatterplots for SBP and DBP in Figures 1 and 2, respectively. Results differed for SBP and DBP. The fitted lines indicate a clear racial difference in the association between perceived discrimination and BP, although these differences seem to be less pronounced for SBP compared with DBP. There appears to be a slight positive relationship between perceived discrimination and DBP for African Americans and a slight negative relationship for whites.
Figure 1.
Scatterplot of perceived discrimination and systolic blood pressure (SBP) for African Americans and whites.
Figure 2.
Scatterplot of perceived discrimination and diastolic blood pressure (DBP) for African Americans and whites.
In the multivariate model (Model 1; Table 2) adjusted for age, sex, race, education, and antihypertensive use, perceived discrimination was not significantly associated with SBP (p = .12). The Race × Discrimination interaction for SBP was also nonsignificant (p = .43). The association between perceived discrimination and SBP remained nonsignificant after additional adjustments for smoking, BMI, and physician-diagnosed diseases (Model 3; Table 2).
Table 2.
Linear Regression Models of Perceived Discrimination and SBP
| SBP |
|||||||||
| Model 1* (R2 = .019) |
Model 2* (R2 = .019) |
Model 3† (R2 = .029) |
|||||||
| Estimate | SE | p Value | Estimate | SE | p Value | Estimate | SE | p Value | |
| Discrimination | −.25 | .16 | .12 | −.01 | .34 | .97 | −.15 | .35 | .67 |
| Race × discrimination | −.30 | .39 | .43 | −.26 | .39 | .50 | |||
Notes: SBP = systolic blood pressure.
Adjusted for age, sex, race, education, and antihypertensive medications.
Adjusted for age, sex, race, education, antihypertensive medications, smoking, body mass index, heart disease, diabetes, and stroke.
In contrast, perceived discrimination was associated with higher levels of DBP (regression estimate = .25, p = .01), after adjusting for age, sex, race, education, and antihypertensive use (see Model 1; Table 3). The Race × Discrimination interaction term was also significant for DBP (regression estimate = .55, p = .02) (Model 2; Table 3).
Table 3.
Linear Regression Models of Perceived Discrimination and DBP
| DBP |
|||||||||
| Model 1* (R2 = .068) |
Model 2* (R2 = .069) |
Model 3† (R2 = .08) |
|||||||
| Estimate | SE | p Value | Estimate | SE | p Value | Estimate | SE | p Value | |
| Discrimination | .25 | .10 | .01 | −.18 | .21 | .38 | −.26 | .21 | .23 |
| Race × discrimination | .55 | .24 | .02 | .62 | .24 | .01 | |||
Notes: DBP = diastolic blood pressure.
Adjusted for age, sex, race, education, and antihypertensive medications.
Adjusted for age, sex, race, education, antihypertensive medications, smoking, body mass index, heart disease, diabetes, and stroke.
In race-stratified models (Table 4), there was a significant positive association between perceived discrimination and DBP (regression estimate = .39, p = .0003) for older African Americans. The regression estimate indicates that, at baseline, every additional unit in the discrimination score was associated with a .39-mm/Hg higher DBP in African Americans. In older whites, there was a slight negative but nonsignificant association between perceived discrimination and DBP (regression estimate = −.16, p = .46).
Table 4.
Linear Regression Models of Perceived Discrimination and Diastolic Blood Pressure by Race
| African Americans |
Whites |
|||||
| Estimate | SE | p Value | Estimate | SE | p Value | |
| Discrimination (Model 2)* | .39 | .11 | .0003 | −.16 | .21 | .46 |
| Discrimination (Model 3)† | .37 | .11 | .001 | −.21 | .22 | .33 |
Notes: *Adjusted for age, sex, education, and antihypertensive medications. Model R2 = .029 for African Americans, R2 = .019 for whites.
Adjusted for age, sex, education, antihypertensive medications, smoking, body mass index, heart disease, diabetes, and stroke. Model R2 = .034 for African Americans, R2 = .037 for whites.
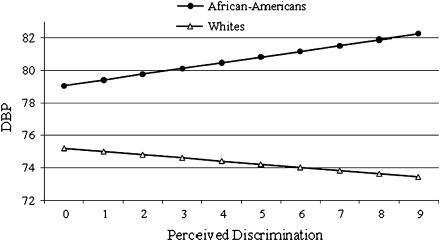
To illustrate these associations, we plotted the predicted values of DBP by levels of discrimination for older African Americans and whites (Figure 3). Higher levels of perceived discrimination were associated with increased levels of baseline DBP in older African Americans only. The association between discrimination and DBP in older whites although nonsignificant, appeared to be slightly inverse.
Figure 3.
Predicted diastolic blood pressure (DBP) by Perceived discrimination scores in older African Americans and whites.
Additional adjustments for smoking, BMI, and physician-diagnosed diseases did not change the patterning of our results in the full (Model 3; Table 3) or race-stratified samples (Table 4).
DISCUSSION
We examined the association between perceived discrimination and BP in a population-based cohort of older African American and white adults. Findings revealed a significant cross-sectional association between discrimination and DBP in older African Americans but not whites. In older African Americans, higher levels of perceived discrimination were associated with higher levels of DBP. This association was independent of demographic variables and potential confounders such as hypertensive medication use, smoking, BMI, and physician-diagnosed diabetes, heart disease, and/or stroke. Interestingly, our findings were limited to DBP. No significant associations were observed with SBP.
The positive association between perceived discrimination and elevated DBP observed in our cohort of older African Americans (but not whites) is consistent with findings from laboratory and community-based cohort studies of younger African American adults and adolescents (9–12,19,30,31). Although a number of these studies have focused on African Americans exclusively (10,11,19), those that compare African Americans with whites typically find significant associations between discrimination and BP in African Americans but do not observe similar associations in whites (12,30,31). Hence, our findings provide additional support for the notion that experiences of discrimination may negatively affect BP levels in African American populations (17).
Our finding that discrimination was associated with elevations in DBP, but not SBP, in older African Americans has not previously been reported in a community-based cohort but has been observed in a number of laboratory-based studies with younger African American adults (12,30,31). For example, Guyll and colleagues (12) found that higher reports of discriminatory treatment were associated with greater DBP, but not SBP, reactivity to laboratory stressors in middle-aged African American women. Lepore and colleagues (30) found similar associations in younger African American women. Studies including men have produced comparable results, with discriminatory stressors showing stronger associations with elevated DBP, rather than SBP (31–33).
To date, there have been few explanations proposed for this particular patterning of results. Recently, Thomas and colleagues (33, 696) hypothesized that experiences of discrimination may not lend themselves to active coping efforts, which would increase heart rate and SBP, but might instead require a greater amount of “quiet attentiveness and vigilance” that would lead to increased total peripheral resistance and elevated DBP. Indeed, there is some evidence that the underlying hemodynamic pattern of BP responses to stress differs for African Americans compared with whites, with African Americans exhibiting both increased vascular α-adrenergic receptor sensitivity and enhanced total peripheral resistance (34,35). Whether these factors would contribute to a differential increase in DBP compared with SBP in response to discriminatory stressors remains to be determined.
Historically, there has been some controversy over the clinical significance of DBP versus SBP in older adult populations—with SBP believed to be more of a contributor to clinical outcomes (36–38). However, a recent meta-analysis of more than 61 prospective cohort studies found that both SBP and DBP were linearly associated with vascular mortality in middle-aged and older adult cohorts (39). Thus, in many studies, DBP continues to have a dose–response association with vascular events and vascular mortality well into older age. In this respect, experiences of discrimination could ultimately influence vascular outcomes in older African American populations via elevations in DBP. Our effect sizes are relatively small; however, although small effects at the individual level can translate into meaningful effects at the population level, the implications of these results should be interpreted with some caution. Nonetheless, future studies should begin to examine associations between discrimination and vascular outcomes in older adults, with DBP as a potential mediator.
Our study has limitations. To begin with, our measure of perceived discrimination was a brief measure of fairly subtle, day-to-day forms of discriminatory treatment. Given the age of our cohort and the historical relevance of discrimination in the lives of African Americans who came of age prior to the Civil Rights movement in the United States, the study could have benefited from a more comprehensive assessment of both subtle and not-so-subtle forms of discriminatory treatment across the life span. Our measure is also limited by the fact that we did not assess the reason for the discriminatory experiences (race, gender, age, etc.). Findings from at least one study suggest that nonracial discrimination may be more strongly associated with vascular outcomes than with racial discrimination (13); conversely, findings from another cohort indicate that the attribution for discriminatory experiences matters less than the experiences themselves, with nonracial and racial discrimination having a similar impact on vascular health (40). It is difficult to gauge which forms of discrimination are accounting for our results—it is possible that older African American adults are particularly vulnerable to certain types of discrimination (e.g., racism and ageism) and less vulnerable to others. Further research in this area is warranted. Finally, these findings are cross-sectional in nature. Additional research is needed to determine if the observed cross-sectional associations persist over time.
Our study also has several strengths. To our knowledge, this study is the first to examine the association between perceived discrimination and BP in an older adult cohort. The study features a large, population-based sample, with a high participation rate. We also used a well-established measure of discrimination and standardized methods for the assessment of BP and other covariates.
In summary, perceived discrimination was associated with higher levels of baseline DBP in a community-based sample of older African Americans, but not whites, even after controlling for a number of potential confounders. These findings provide further support for the notion that discriminatory experiences might be a unique risk factor for elevated BP in African American populations.
FUNDING
This work was supported by National Institute on Aging grant AG11101, and by a National Heart, Lung, and Blood Institute Grant HL092591.
Acknowledgments
Preliminary findings from this study were presented at the American Psychosomatic Society's annual meeting in Baltimore, Maryland, on March 14, 2008.
References
- 1.Hsu CY, McCulloch CE, Darbinian J, Go AS, Iribarren C. Elevated blood pressure and risk of end-stage renal disease in subjects without baseline kidney disease. Arch Intern Med. 2005;165:923–928. doi: 10.1001/archinte.165.8.923. [DOI] [PubMed] [Google Scholar]
- 2.Vasan RS, Massaro JM, Wilson PWF, et al. Antecedent blood pressure and risk of cardiovascular disease: The Framingham Heart Study. Circulation. 2002;105:48–53. doi: 10.1161/hc0102.101774. [DOI] [PubMed] [Google Scholar]
- 3.Psaty BM, Furberg CD, Kuller LH, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: The Cardiovascular Health Study. Arch Intern Med. 2001;161:1183–1192. doi: 10.1001/archinte.161.9.1183. [DOI] [PubMed] [Google Scholar]
- 4.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 5.Harris MM, Stevens J, Thomas N, Schreiner P, Folsom AR. Associations of fat distribution and obesity with hypertension in a bi-ethnic population: The ARIC Study. Obes Res. 2000;8:516–524. doi: 10.1038/oby.2000.64. [DOI] [PubMed] [Google Scholar]
- 6.Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: An analysis of NHANES III, 1988–1994. J Am Geriatr Soc. 2001;49:109–116. doi: 10.1046/j.1532-5415.2001.49030.x. [DOI] [PubMed] [Google Scholar]
- 7.Dyer AR, Liu K, Walsh M, Kiefe C, Jacobs DR, Jr, Bild DE. Ten-year incidence of elevated blood pressure and its predictors: The CARDIA Study. Coronary Artery Risk Development in (Young) Adults. J Hum Hypertens. 1999;13:13–21. doi: 10.1038/sj.jhh.1000740. [DOI] [PubMed] [Google Scholar]
- 8.Marshall SJ, Jones DA, Ainsworth BE, Reis JP, Levy SS, Macera CA. Race/ethnicity, social class, and leisure-time physical inactivity. Med Sci Sports Exerc. 2007;39:44–51. doi: 10.1249/01.mss.0000239401.16381.37. [DOI] [PubMed] [Google Scholar]
- 9.Krieger N, Sidney S. Racial discrimination and blood pressure: The CARDIA Study of young black and white adults. Am J Public Health. 1996;86:1370–1378. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African-Americans. The metro Atlanta heart disease study, 1999–2001. Soc Sci Med. 2004;58:449–461. doi: 10.1016/s0277-9536(03)00211-9. [DOI] [PubMed] [Google Scholar]
- 11.Steffen PR, McNeilly M, Anderson N, Sherwood A. Effects of perceived racism and anger inhibition on ambulatory blood pressure in African Americans. Psychosom Med. 2003;65:746–750. doi: 10.1097/01.psy.0000079380.95903.78. [DOI] [PubMed] [Google Scholar]
- 12.Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: Relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20:315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- 13.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: The Pitt County Study. Am J Epidemiol. 2008;167:624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- 14.Brown C, Matthews KA, Bromberger JT, Chang Y. The relation between perceived unfair treatment and blood pressure in a racially/ethnically diverse sample of women. Am J Epidemiol. 2006;164:257–262. doi: 10.1093/aje/kwj196. [DOI] [PubMed] [Google Scholar]
- 15.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 16.Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older blacks and whites. J Aging Health. 2004;16:315–337. doi: 10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]
- 17.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 18.Armstead CA, Lawler KA, Gorden G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in black college students. Health Psychol. 1989;8:541–556. doi: 10.1037//0278-6133.8.5.541. [DOI] [PubMed] [Google Scholar]
- 19.Clark R. Perceived racism and vascular reactivity in black college women: Moderating effects of seeking social support. Health Psychol. 2006;25:20–25. doi: 10.1037/0278-6133.25.1.20. [DOI] [PubMed] [Google Scholar]
- 20.Matthews KA, Salomon K, Kenyon K, Zhou F. Unfair treatment, discrimination, and ambulatory blood pressure in black and white adolescents. Health Psychol. 2005;24:258–265. doi: 10.1037/0278-6133.24.3.258. [DOI] [PubMed] [Google Scholar]
- 21.Klarman MJ. From Jim Crow to Civil Rights: The Supreme Court and the Struggle for Racial Equality. New York: Oxford University Press; 2004. [Google Scholar]
- 22.Bienias JL, Beckett LA, Bennett DA, Wilson RS, Evans DA. Design of the Chicago Health and Aging Project (CHAP) J Alzheimers Dis. 2003;5:349–355. doi: 10.3233/jad-2003-5501. [DOI] [PubMed] [Google Scholar]
- 23.Barnes LL, de Leon CFM, Lewis TT, Bienias JL, Wilson RS, Evans DA. Perceived discrimination and mortality in a population-based study of older adults. Am J Public Health. 2008;98:1241–1247. doi: 10.2105/AJPH.2007.114397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krysan M, Couper MP. Race in the live and the virtual interview: Racial deference, social desirability, and activation effects in attitude surveys. Soc Psychol Q. 2003;66:364–383. [Google Scholar]
- 25.Anderson BA, Silver BD, Abramson PR. The effects of the race of the interviewer on race-related attitudes of black respondents in Src/Cps national election studies. Public Opin Q. 1988;52:289–324. [Google Scholar]
- 26.Hypertension Detection and Follow-up Program Cooperative Group. Variability of blood pressure and the results of screening in the hypertension detection and follow-up program. J Chronic Dis. 1978;31:651–667. doi: 10.1016/0021-9681(78)90069-3. [DOI] [PubMed] [Google Scholar]
- 27.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 28.Chumlea WC, Roche AF, Mukherjee D. Some anthropometric indices of body composition for elderly adults. J Gerontol. 1986;41:36–39. doi: 10.1093/geronj/41.1.36. [DOI] [PubMed] [Google Scholar]
- 29.SAS Version 9.1.3. Cary, NC: SAS Institute; 2004. [Google Scholar]
- 30.Lepore SJ, Revenson TA, Weinberger SL, et al. Effects of social stressors on cardiovascular reactivity in Black and White women. Ann Behav Med. 2006;31:120–127. doi: 10.1207/s15324796abm3102_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richman LS, Bennett GG, Pek J, Siegler I, Williams RB., Jr Discrimination, dispositions, and cardiovascular responses to stress. Health Psychol. 2007;26:675–683. doi: 10.1037/0278-6133.26.6.675. [DOI] [PubMed] [Google Scholar]
- 32.Fang CY, Myers HF. The effects of racial stressors and hostility on cardiovascular reactivity in African American and Caucasian men. Health Psychol. 2001;20:64–70. doi: 10.1037//0278-6133.20.1.64. [DOI] [PubMed] [Google Scholar]
- 33.Thomas KS, Nelesen RA, Malcarne VL, Ziegler MG, Dimsdale JE. Ethnicity, perceived discrimination, and vascular reactivity to phenylephrine. Psychosom Med. 2006;68:692–697. doi: 10.1097/01.psy.0000238214.80871.e6. [DOI] [PubMed] [Google Scholar]
- 34.Kelsey RM, Alpert BS, Patterson SM, Barnard M. Racial differences in hemodynamic responses to environmental thermal stress among adolescents. Circulation. 2000;101:2284–2289. doi: 10.1161/01.cir.101.19.2284. [DOI] [PubMed] [Google Scholar]
- 35.Sherwood A, May CW, Siegel WC, Blumenthal JA. Ethnic differences in hemodynamic responses to stress in hypertensive men and women. Am J Hypertens. 1995;8:552–557. doi: 10.1016/0895-7061(95)00036-O. [DOI] [PubMed] [Google Scholar]
- 36.Glynn RJ, Field TS, Rosner B, Hebert PR, Taylor JO, Hennekens CH. Evidence for a positive linear relation between blood pressure and mortality in elderly people. Lancet. 1995;345:825–829. doi: 10.1016/s0140-6736(95)92964-9. [DOI] [PubMed] [Google Scholar]
- 37.Taylor JO, Cornoni-Huntley J, Curb JD, et al. Blood pressure and mortality risk in the elderly. Am J Epidemiol. 1991;134:489–501. doi: 10.1093/oxfordjournals.aje.a116121. [DOI] [PubMed] [Google Scholar]
- 38.Glynn RJ, Chae CU, Guralnik JM, Taylor JO, Hennekens CH. Pulse pressure and mortality in older people. Arch Intern Med. 2000;160:2765–2772. doi: 10.1001/archinte.160.18.2765. [DOI] [PubMed] [Google Scholar]
- 39.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 40.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]