Abstract
We report a chronic cerebral paragonimiasis from a 41-year-old Korean man who complains a headache and weakness of left motor neuron components. Magnetic resonance images of the brain revealed conglomerates of multiple ring-like enhancements in temporo-occipital and frontal lobes of the right hemisphere. An intradermal test for paragonimiasis westermani was positive. The patient was born near an endemic area of paragonimiasis and used to eat boiled or grilled freshwater crayfish in his childhood. Nodules in the brain were resected through craniotomies. The eggs of P. westermani were identified pathologically and parasitologically in the calcified necrotic lesions. Examinations on sputum and fecal specimens for the eggs of P. westermani were shown to be negative and a chest radiograph was normal. It is presumed that the brain lesions were formed by P. westermani approximately 30 years ago.
Keywords: Paragonimus westermani, cerebral involvement, MR image, egg
Paragonimus westermani infects millions of people in the Orient including China, Korea, Japan, and Taiwan (Blair et al., 1999). Human is contracted with P. westermani through eating raw or undercooked freshwater crabs or crayfish infected with the metacercariae. The metacercaria excysts in the small intestine and penetrates the wall into abdominal cavity, which then migrates through vicera and diaphragm to the lungs. In the human host, the lung is the principal habitat (Choi, 1990). The erratic migrations of juvenile flukes result in ectopic paragonimiasis in various organs, frequently in the peritoneal and pelvic cavities, diaphragm, subcutaneous tissues and the brain (Hong et al., 1982; Ogata et al., 1990; Nabeshima et al., 1991; Choi and Jeong, 1991, Lee et al., 1997). Symptoms of ectopic infections are solely dependent on the contracted organ and the number of flukes therein. Of the ectopic occasions, cerebral paragonimiasis is serious and sometimes fatal. With the aid of serodiagnostic, CT and MR imaging tools, cerebral paragonimiasis has been diagnosed in the early stages of the infection (Yoshida et al., 1982; Cha et al., 1994). We report a clinical case of chronic infection with cerebral involvement confirmed by the eggs of P. westermani.
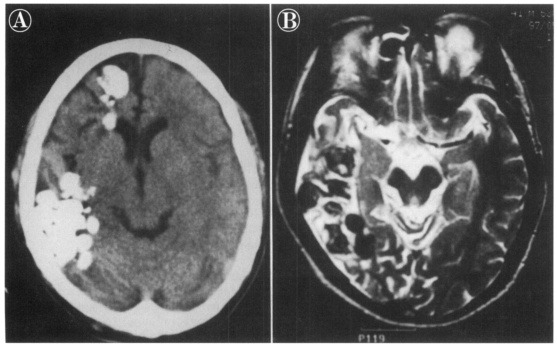
A Korean man, 41 years of age, was admitted to the Kangnam General Hospital, Seoul, on May 8, 1997 with complaints of headache and weakness of the left motor neuron components for one month. He had the first history of seizure at the age of 14 and the seizure has occurred occasionally during the ensuing years. Computerized tomography scans revealed multiple, densely calcified areas with a variety of nodular shapes in the right frontal and temporo-occipital regions (Fig. 1A). Magnetic resonance (MR) studies on his brain uncovered two conglomerates of multiple ring-shaped enhancements resembling a grape cluster, one consisted of 8-10 rings (4 × 5 × 3 cm in size) in the right lower temporo-occipital lobe and the other one with 8 rings (1 × 2 × 1 cm in size) in the right frontal lobe. T1-weighted axial images revealed that the nodules had an area of peripheral low density and central hypo- and isointensity. T2-weighted images showed widespread inflammatory changes in the surrounding tissue (Fig. 1B).
Fig. 1.
Brain images. (A) A computerized tomography shows multiple calcified density in the right frontal and temporal areas. (B) T2-weighted axial image shows inflammatory changes in surrounding tissue.
The patient was born and grown up in Hoengsung-gun (a mountainous area), Kangwon-do, Korea. He used to eat grilled or bolied freshwater crayfish caught in the stream nearby the village in his childhood. He has never eaten the freshwater crayfish for about 20 years ever since he left his hometown. In enzyme-linked immunosorbant assays for serum and cerebrospinal fluid, IgG antibody for P. westermani was below the positive cuttings (Chang et al., 1993). In the intradermal tests, a wheel for Clonorchisis sinensis antigen was 20 mm2 and that of P. westermani was 80 mm2 (positive criterion: > 60 mm2). Two stool examinations for helminth eggs, protozoan cysts and trophozoites and occult blood gave negative results. No P. westermani eggs were found in sputum examination. The sputum culture was negative for pathogenic bacteria. On plain chest radiographies, any old inflammatory sequale was not found in the lungs, but they were suspected to be found in the right upper lobe. Electroencephalograms were within the normal extents. Labaratory data on the blood examination are as follow: RBC 1.02 × 106/mm3, WBC 4.7 × 103/mm3 (neutrophil 63.0%, lymphocyte 23.7%, monocyte 9.7%, eosinophil 3.3%, basophil 0.3%), Hb/Hct 14.9/45, PLT 3.06 × 105/mm3.
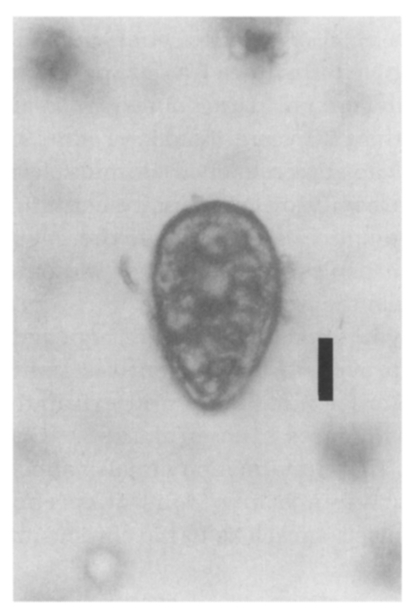
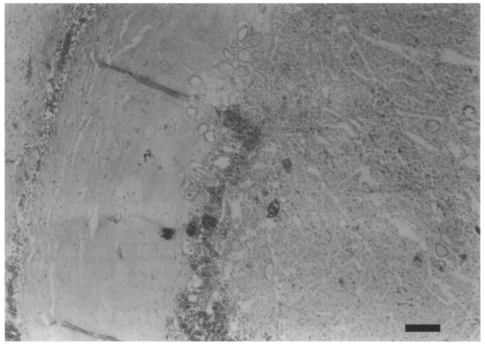
The masses surrounding the lesions in the temporo-occipital lobe were resected on May 20, 1997 and then in the frontal lobe on June 8, 1997 through the craniotomies. The resected masses were yellowish and looked like a branch of grape. Paragonimus westermani eggs were identified under light microscope from the stamp smears of the resected tissues (Fig. 2). The eggs were 81.6 ± 2.9 µm in length and 52.8 ± 2.0 µm in width. This case was diagnosed to be a cerebral paragonimiasis by P. westermani eggs. Pathologic preparations revealed the P. westermani eggs were concentrated near a border of the fibrous worm capsule and scattered in the calcified nodular lesions (Fig. 3). Any remnant of P. westermani was not found in the necrotic worm capsule, except for the eggs.
Fig. 2.
A Paragonimus westermani egg in smears from a mass resected from the brain lesions. Bar is 30 µm.
Fig. 3.
Paragonimus westermani eggs in a border of necrotic lesion and fibrous tissue of the worm capsule. Bar is 200 µm.
An effective antihelminthic for paragonimiasis, doses of praziquantel, was not prescribed. He was discharged with improved left motor components. After the operation, he did not experience a seizure, but he was experiencing intermittent headaches. He is still receiving a tapering administration of anticonvulsants.
In Korea, the endemic areas of paragonimiasis were sporadically spread over the villages near small streams in the southwestern and eastern parts of the country in the 1960s. In some villages the P. westermani egg positive rates were around 20%. The infection rates of P. westermani metacercaria of the freshwater crabs ranged from 36% to 78% in the 1960s (Cho, 1994). According to the national surveys conducted in every 5 years, P. westermani egg positive rate in stool specimens was 0.09% in 1971 which has declined ever since to the point where the detection was not possible in 1997 (the Ministry of Health and Social affairs and the Korea Association of Health, 1997). In this period, paragonimiasis was detected on hospital bases by serodiagnosis. Most of them were referred to be differentiation from suspected diseases such as tuberculosis and eosinophilic lungs. Ectopic paragonimiasis cases have been reported with medical significances from abdominal and pelvic cavities, subcutaneous tissue and the brain (Hong et al., 1982; Choi and Jeong, 1991; Cha et al., 1994; Kim et al., 1994). The present case is reported here as a Paragonimus infection which presently is uncommon in Korea.
Cerebral involvement has been reported in 1.6-26.6% of the patients with paragonimiasis based on the hospital statistics. It was, however, estimated on a community based study that cerebral involvement constituted of 0.8% active paragonimiasis cases and 0.2% positive reactors to the intradermal tests (Oh, 1969). Clinical symptoms of cerebral paragonimiasis include epilepsy (frequently Jacksonian type), headache, hemiplesia, monoplesia, hemiparesis, and aphasia. Visual disturbances are infrequently caused by basal arachnoiditis in the brain involvement (Choi, 1990). In the present case, it is suggested from the episodes of occasional seizure attacks that the patient could get along with the impaired cerebral lesions for about 30 years since he was contracted with the disease.
Some juvenile P. westermani in pleural cavity migrate through soft tissues around Vena jugularis interna into the intracranial cavity and reaches to the brain via lateral sinus. By this migrating route, one cerebral hemisphere, especially the occipital lobe of brain was affected frequently in cerebral paragonimiases. It was suggested that in children the cerebral paragonimiasis may be more frequent since the juvenile fluke can get to the cerebrum through the less resistant perivascular soft tissues in children (Seo, 1980). It is likely that the patient in this study was contracted by P. westermani in his childhood and the cerebral lesions were developed over a long period in the right hemisphere.
Radiologic findings for cerebral paragonimiasis have been recorded to be conglomerates of multiple ring-shaped shadows or enhancements so-called "grape cluster" or "soap bubble" formed in one hemisphere in general (Cha et al., 1994; Kadota et al., 1989), and the present case showed a "grape cluster". In chronic cerebral paragonimisis, persisting for more than 20 years (Katoda et al., 1989), the worm capsules remained as multiple nodules with a cavity of low density containing the Paragonimus eggs. Most of the eggs in the worm capsules retained a shell without yolk as shown in the present case.
Enzyme-linked immunosorbent assey has been proven to be efficiently sensitive and sepecific for pulmonary and extrapulmonary paragonimiases (Cho et al., 1981; Cha et al. 1994). These information are also applicable to the early stage infections of cerebral paragonimiasis as well as to the chronic infections in the brain.
An early diagnosis of cerebral paragonimiasis is of clinical importance because it can be cured successfully by chemotherapy with the use of praziquantel (Rhee et al., 1987). On the admission of the present case, CT findings provided a clue for cerebral paragonimiasis but the serologic data did not. Then, the tentative diagnosis was postulated with P. westermani eggs found in the pathologic preparations of the resected brain masses. It is very interesting that juvenile P. westermani in the brain may fully develop into adult worms and the eggs are well preserved for a long time without causing significant damages in the central nervous system.
References
- 1.Blair D, Xu Z-B, Agatsuma T. Paragonimiasis and the genus Paragonimus. Adv Parasitol. 1999;42:113–127. doi: 10.1016/s0065-308x(08)60149-9. [DOI] [PubMed] [Google Scholar]
- 2.Cha SH, Chang KH, Cho SY, et al. Cerebral paragonimiasis in early active stage:CT and MR features. AJR Am J Roentgenol. 1994;162:141–145. doi: 10.2214/ajr.162.1.8273653. [DOI] [PubMed] [Google Scholar]
- 3.Chang KH, Cha SH, Han MH, et al. An imaging diagnosis of cerebral paragonimiasis: CT and MR findings and correlation with ELISA antibody test. Korean J Radiol Soc. 1993;29:345–354. [Google Scholar]
- 4.Cho SY. Collected papers on Parasite Control Activities in Korea. Seoul. Korea: The Korea Association of Health; 1994. Epidemiology of paragonimiasis in Korea; pp. 51–57. [Google Scholar]
- 5.Cho SY, Hong ST, Rho YH, Choi S, Han YC. Application of micro-ELISA in serodiagnosis of human paragonimiasis. Korean J Parasitol. 1981;19:151–156. doi: 10.3347/kjp.1981.19.2.151. [DOI] [PubMed] [Google Scholar]
- 6.Choi DW. Paragonimus and Paragonimiasis in Korea. Korean J Parasitol. 1990;28(Suppl):79–102. doi: 10.3347/kjp.1990.28.suppl.79. [DOI] [PubMed] [Google Scholar]
- 7.Choi W-Y, Jeong SS. A case of paragonimiasis in the abdominal subcutaneous tissue. Korean J Parasitol. 1991;29:407–409. doi: 10.3347/kjp.1991.29.4.407. [DOI] [PubMed] [Google Scholar]
- 8.Hong ST, Lee SH, Chi JG, Jin YS, Kim CS, Chang YS. A case of systemic paragonimiasis with ovarian involvement. Korean J Parasitol. 1982;20:53–59. doi: 10.3347/kjp.1982.20.1.53. [DOI] [PubMed] [Google Scholar]
- 9.Katoda T, Ishikura R, Tabuchi Y, et al. MR imaging of chronic cerebral paragonimiasis. Am J Neuroradiol. 1989;10:S21–S22. [PMC free article] [PubMed] [Google Scholar]
- 10.Kim SH, Choi BI, Im JG, Kook MC, Yeon KM, Chi JG. Chronic pelvic paragonimiasis:Radiological findings. Seoul J Med. 1994;35:289–293. [Google Scholar]
- 11.Lee SC, Jwo SC, Hwang KP, Lee N, Shieh WB. Discovery of encysted Paragonimus westermani eggs in the omentum of an asysmptomatic elderly woman. Am J Trop Med Hyg. 1997;57:615–618. doi: 10.4269/ajtmh.1997.57.615. [DOI] [PubMed] [Google Scholar]
- 12.The Ministry of Health and Welfare and the Korea Association of Health. Prevalence of intestinal parasitic infections in Korea. The sixth report. Seoul, Korea: 1997. pp. 1–70. [Google Scholar]
- 13.Nabeshima K, Inoue T, Sekiya R, et al. Intrahepatic paragonimiasis - A case report - Jpn J Parasitol. 1991;40:296–300. [Google Scholar]
- 14.Oh SJ. The rate of cerebral paragonimiasis: an epidemiologic study. Jpn J Parasitol. 1969;18:211–214. [Google Scholar]
- 15.Ogata K, Miyagi T, Inoue S, Imai JI, Nawa Y. Cutaneous paragonimiasis - A case report - Jpn J Parasitol. 1990;39:63–66. [Google Scholar]
- 16.Rhee CH, Chung CK, Jung HW, Cho SY, Son HJ. Cerebral paragonimiasis treated with praziquantel: case report. J Korean Neurosurg Soc. 1987;16:853–857. [Google Scholar]
- 17.Seo BS. Clinical Parasitology. 2nd ed. Seoul, Korea: Ilchokak; 1980. pp. 244–252. [Google Scholar]
- 18.Yoshida M, Moritaka K, Kuga S, Anegawa S. CT findings of cerebral paragonimiasis in the chronic state. J Comput Assist Tomogr. 1982;6:195–196. doi: 10.1097/00004728-198202000-00039. [DOI] [PubMed] [Google Scholar]