Abstract
As part of the longterm follow-up of amblyopic children who were enrolled in the Amblyopia Treatment Study1, we tested visual acuity in both eyes of 142 patients using two established visual acuity protocols, the Amblyopia Treatment Study HOTV (ATS HOTV) visual acuity protocol and the Electronic-Early Treatment of Diabetic Retinopathy Study (E-ETDRS) protocol, at one of the annual visits. Mean age at the time of testing was 9.0 years (range = 5.6 to 11.9 years). The ATS-HOTV protocol resulted in a slight mean overestimate of visual acuity relative to the E-ETDRS protocol (0.68 lines for amblyopic eyes; 0.25 lines for fellow eyes). The overestimation occurred primarily when the E-ETDRS visual acuity was poorer than 0.3 logMAR. ATS-HOTV acuity also underestimated interocular visual acuity differences by 0.42 lines. When using the ATS-HOTV protocol, it may be wise to exercise caution when interpreting “near normal” visual acuity or interocular differences as “within normal” because the ATS-HOTV method may have a slight bias toward better performance of amblyopic eyes than E-ETDRS.
Introduction
Standardization of visual acuity measurement is essential for accurate monitoring of the response to treatment in individual patients and in clinical trials. By consensus of experts, the Early Treatment for Diabetic Retinopathy (ETDRS) logMAR charts2 have become the gold standard for adult visual acuity testing. More recently, a computerized version of ETDRS that uses crowded, isolated letters was developed; the new Electronic-ETDRS (E-ETDRS) has high test-retest reliability and good agreement with ETDRS chart in adults3 and in children aged 7–12 years.4 Because the letters in the ETDRS charts are often too difficult for most children under the age of 7 years, the use of crowded isolated HOTV optotypes has been common in this age group and a standardized protocol (ATS-HOTV) has been developed by the Pediatric Eye Disease Investigator Group for use in multicenter studies.5, 6
Whether results from the E-ETDRS and ATS-HOTV visual acuity protocols are comparable is important for longitudinal clinical management and for analysis of longterm outcome measurement in clinical trials. The appropriateness of treatment decisions based on visual acuity measurements that span across the age range when the method of visual acuity assessment may change depends on an understanding of the performance of the two tests. In the only study that directly compared performance on the E-ETDRS and ATS-HOTV protocols, Rice et al7 found that ATS-HOTV visual acuity was, on average, 0.06 logMAR better than E-ETDRS visual acuity in a heterogeneous group of 236 children age 5–12 years. For a subgroup of 43 children with interocular differences of ≥ 0.2 logMAR with various etiologies, this study also reported similar interocular differences in visual acuity with both protocols.7 However, because not all the patients included in that study had amblyopia, the effect of different testing protocols on the assessment of amblyopia has not been definitively established. This is an important issue as amblyopia has a high prevalence and clinical management requires repeated visual acuity measurement across the age range where testing protocols typically change.
Methods
At the conclusion of the Amblyopia Treatment Study, a randomized trial comparing patching (6 hours/day to full time) with atropine (1% daily) as treatments for moderate amblyopia (20/40 to 20/100) in children younger than 7 years of age, parents of patients from a subset of participating sites (those with more than 5 patients enrolled and continuing with other PEDIG protocols) were invited to enter a long-term extension phase. The protocol and informed consent forms were approved by institutional review boards (IRB). Study oversight was provided by an independent data and safety monitoring committee. Written informed consent was obtained from the parent or guardian to continue follow up with annual exams through age 10 years and a future exam at age 15 years. One-hundred eighty-eight (188) patients consented to participate in the extension phase. Per study protocol, Visual acuity was tested in each eye using both the E-ETDRS and ATS-HOTV protocols at one of the annual visits; 142 patients (76%) completed this testing, where the primary reason for failure to complete both VA protocols was investigator error in following the protocol. Mean age at the time of testing was 9.0 years (range = 5.6 to 11.9 years); 41% of the patients were female, and 87% were white. Both tests were presented on the same video monitor and required best refractive correction. Testing using the E-ETDRS protocol was completed first, because it was the overall study’s primary outcome measure for the extension phase. Interocular difference was calculated as amblyopic eye minus fellow eye visual acuity. Visual acuity differences between the 2 testing protocols were calculated as logMAR acuity by E-ETDRS minus ATS-HOTV. When converting E-ETDRS letter scores to logMAR, scores were rounded to the nearest line and truncated at −0.1 logMAR to insure comparability of ranges for E-ETDRS and ATS-HOTV.
Results
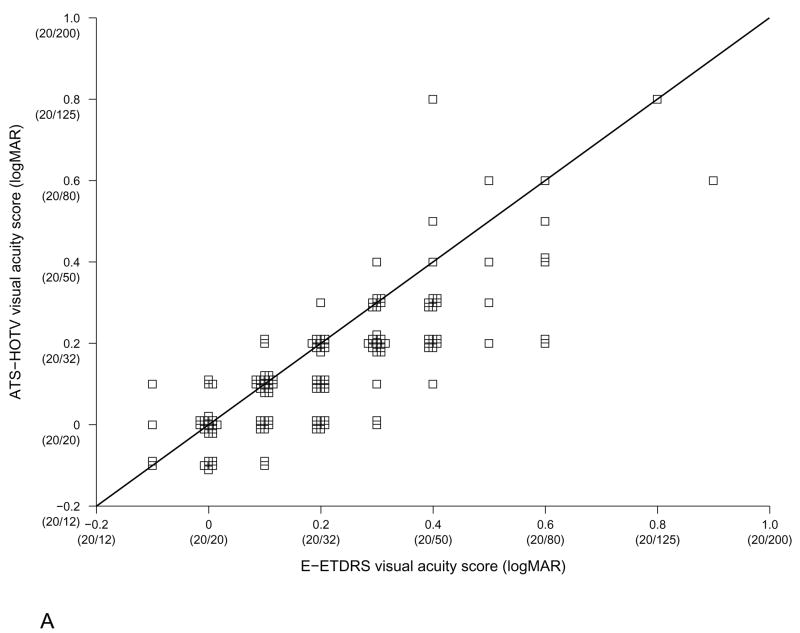
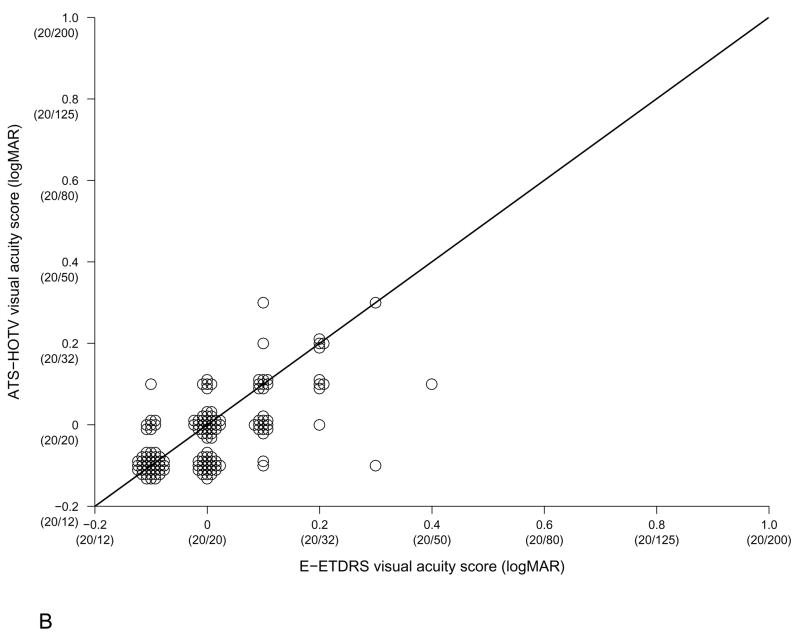
As shown in Figure 1, visual acuity of the previously treated amblyopic eyes ranged from −0.10 to 0.90 logMAR (20/16 to 20/160) using the E-ETDRS protocol and from −0.10 to 0.80 logMAR (20/16 to 20/125) using the ATS-HOTV protocol. Fellow eye visual acuity ranged from −0.10 to 0.40 logMAR (20/16 to 20/50) using the E-ETDRS protocol and from −0.10 to 0.30 logMAR (20/16 to 20/40) using the ATS-HOTV protocol.
Figure 1.
Comparison of E-ETDRS and ATS-HOTV visual acuity in A. amblyopic eyes and B. fellow eyes; unity line.
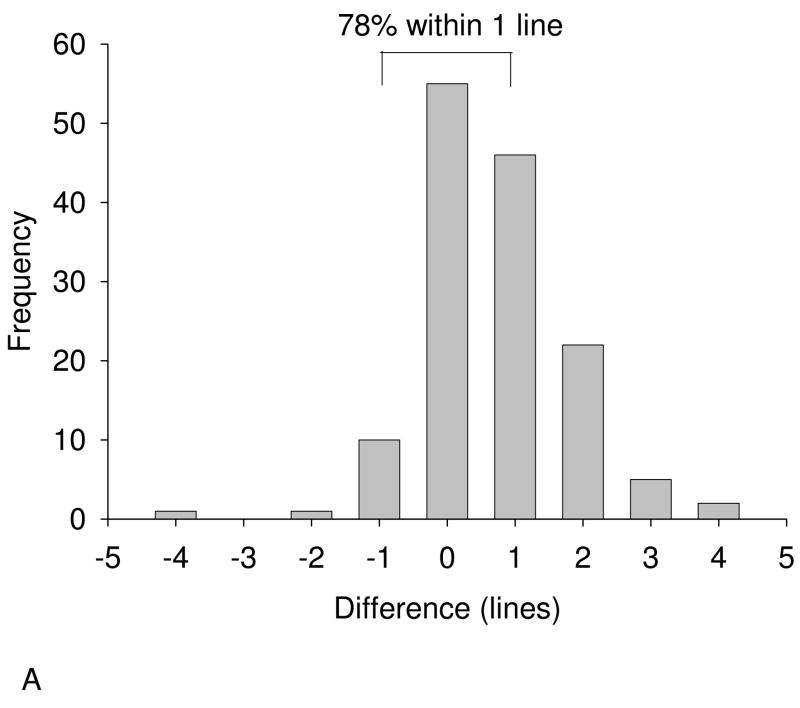
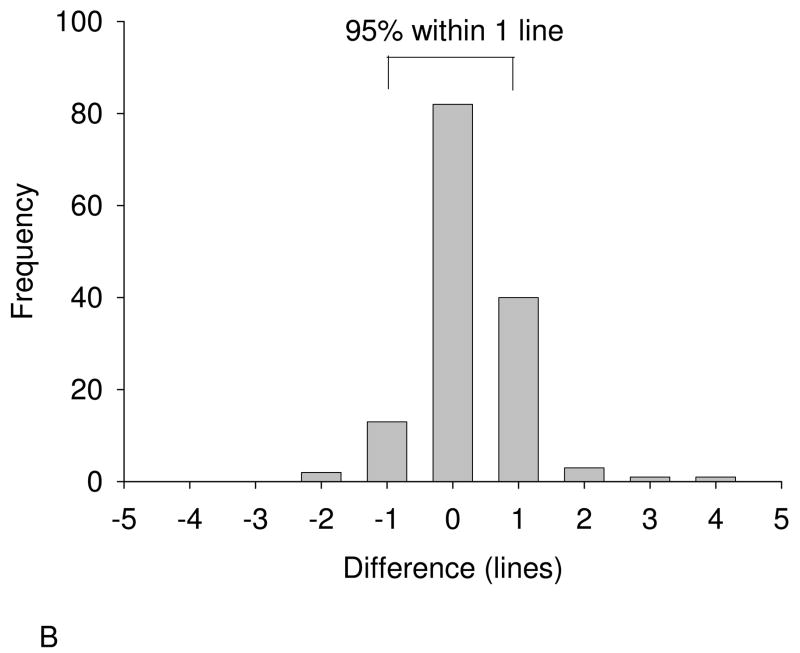
Treated amblyopic eyes had the same visual acuity or were within 1 line for E-ETDRS and ATS-HOTV in 111 cases (78%), tested ≥ 2 lines better with ATS-HOTV in 29 cases (20%) and tested ≥ 2 lines better with E-ETDRS in 2 cases (1%) (Figure 2A). Fellow eyes had the same visual acuity or were within 1 line using both protocols in 135 cases (95%), tested ≥ 2 lines better with ATS-HOTV in 5 cases (4%) and tested ≥ 2 lines better with E-ETDRS in 2 cases (1%)(Figure 2B). Agreement (within one line) between ATS-HOTV acuity and E-ETDRS acuity was more frequent for fellow eyes than for previously treated amblyopic eyes (95% vs. 78%; p < 0.001).
Figure 2.
Frequency distribution of the difference between E-ETDRS and ATS-HOTV visual acuity for A. amblyopic and B. fellow eyes. Difference is calculated as logMAR acuity by E-ETDRS minus that by ATS-HOTV.
On average, ATS-HOTV visual acuity was 0.68 lines (95% CI: 0.50 – 0.87 lines) better than E-ETDRS visual acuity for treated amblyopic eyes and 0.25 lines (95% CI: 0.12 – 0.39 lines) better than E-ETDRS visual acuity for fellow eyes. However, for previously treated amblyopic eyes with excellent visual acuity (20/20 or 20/16; ≤0.00 log MAR by E-ETDRS), the average discrepancy was 0.0 lines (95% CI: −0.4 – 0.4 lines) while, for previously treated amblyopic eyes that remained amblyopic (20/40 or poorer; ≥0.30 log MAR by ETDRS), was 1.1 lines (95% CI: 0.7 – 1.6 lines). Thus, in estimating visual acuity with a single test administration, the ATS-HOTV method may bias toward a slightly better visual acuity, particularly in amblyopic eyes with 20/40 or poorer acuity.
Interocular differences showed good agreement for the two protocols in 117 cases (82%), with 54 cases in which both protocols found ≤ 1 line interocular difference (consistent with no amblyopia) and 63 cases in which both protocols found 2 or more lines interocular difference (consistent with amblyopia). In 20 cases (14%), the ATS-HOTV protocol found ≤ 1 line interocular difference while the E-ETDRS protocol found ≥ 2 lines interocular difference. In 5 cases (4%), the E-ETDRS protocol found ≤ 1 line interocular difference while the ATS-HOTV protocol found ≥ 2 lines interocular difference. On average, the ATS-HOTV interocular difference was 0.42 lines (95% CI: 0.22 – 0.61) smaller than the E-ETDRS interocular difference.
Discussion
Similar to the study by Rice et al, we found that the ATS-HOTV protocol resulted in a slight mean overestimate of visual acuity relative to the E-ETDRS protocol (0.68 lines, equivalent to 3.4 letters). Our novel finding is that most of the discrepancy was due to overestimation by ATS-HOTV of amblyopic eye visual acuity when the E-ETDRS visual acuity was ≥ 0.3 logMAR (i.e., 20/40 or worse). Thirty-six percent of the children with E-ETDRS visual acuity ≥ 0.3 logMAR (20/40) had an overestimate of visual acuity by ATS-HOTV. The slightly better ATS-HOTV visual acuity compared to E-ETDRS in children with poorer acuity may be due to the child’s awareness that there are only four letters in the ATS-HOTV protocol and the dissimilarity of the four letters in overall shape. Another possibility is the difference in crowding bar spacing for the two tests. However, the 0.5 letter separation of crowding bars in the ATS-HOTV protocol is the separation which has been reported to have maximum effect on visual acuity8, so the E-ETDRS protocol crowding bar separation of 1.0 letter would be expected to result in better acuity, opposite to our observations.
Unlike the study by Rice et al, we found that ATS-HOTV acuity also underestimated interocular visual acuity differences (by 0.42 lines, i.e., 2 letters). Due to a slight overestimation of visual acuity in amblyopic eyes with visual acuity ≥ 0.3 logMAR, ATS-HOTV interocular differences were smaller than E-ETDRS interocular differences.
A limitation of this study is that, since the primary outcome for the longterm extenstion study was E-ETDRS visual acuity, E-ETDRS testing was always administered first. Thus, it is possible that administering the E-ETDRS protocol first “warmed up” the child for better performance on the ATS-HOTV protocol. This is unlikely since the difference observed in the present study (0.07 logMAR) is similar to the 0.06 logMAR difference reported in the study by Rice et al7 where the testing order was randomized. A second potential limitation is that we included data from all children in the longterm extension study who were able to complete both visual acuity tests on an annual visit, even if they were younger than 7 years of age. Since ETDRS tests are difficult for some children under 7 years of age, it is possible that the slightly poorer visual acuity measured with the E-ETDRS protocol is a result of inclusion of these young patients. Nevertheless, a separate analysis, excluding the 10 patients who were <7 years old at the time of testing, revealed similar results.
A single administration of any visual acuity test will always be prone to sampling error, but the present study confirms a small bias of the ATS-HOTV protocol towards better visual acuities of amblyopic eyes and lower interocular differences. We therefore suggest the need for caution in interpreting “near normal visual acuity” and small interocular differences when using the ATS-HOTV protocol. Nevertheless, in 3 to 6 year-olds the ATS-HOTV protocol remains one of the few standardized methods of detecting amblyopia and monitoring its therapy.
Supplementary Material
Acknowledgments
Supported by National Eye Institute of National Institutes of Health, Department of Health and Human Services EY011751 (PEDIG).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pediatric Eye Disease Investigator Group. A randomized trial of atropine versus patching for treatment of moderate amblyopia: follow-up at age 10 years. Arch Ophthalmol. 2008 doi: 10.1001/archopht.126.8.1039. Accepted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong LM, Marsh MJ, Hawkins BS. Measurement and analysis of visual acuity in multicenter randomized clinical trials in the United States: findings from a survey. Ophthalmic Epidemiol. 2003;10:149–65. doi: 10.1076/opep.10.3.149.15080. [DOI] [PubMed] [Google Scholar]
- 3.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135:194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 4.Cotter SA, Chu RH, Chandler DL, et al. Reliability of the Electronic Early Treatment Diabetic Retinopathy Study testing protocol in children 7 to <13 years old. Am J Ophthalmol. 2003;136:655–61. doi: 10.1016/s0002-9394(03)00388-x. [DOI] [PubMed] [Google Scholar]
- 5.Holmes JM, Beck RW, Repka MX, et al. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 6.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 7.Rice ML, Leske DA, Holmes JM. Comparison of the Amblyopia Treatment Study HOTV and Electronic-Early Treatment of Diabetic Retinopathy Study visual acuity protocols in children aged 5 to 12 years. Am J Ophthalmol. 2004;137:278–82. doi: 10.1016/j.ajo.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 8.Simmers AJ, Gray LS, McGraw PV, Winn B. Contour interaction for high and low contrast optotypes in normal and amblyopic observers. Ophthal Physiol Opt. 1999;19:253–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.