Abstract
Heterotopic pancreas is defined as pancreatic tissue found outside the usual anatomical location of the pancreas. It is often an incidental finding and can be found at different sites in the gastrointestinal tract. It may become clinically evident when complicated by pathological changes such as inflammation, bleeding, obstruction, and malignant transformation. In this report, a 60-year-old man with carcinoid syndrome caused by heterotopic pancreatic tissue in the duodenum is described, along with a 62-year-old man with abdominal pain caused by heterotopic pancreatic tissue in the gastric antrum. The difficulty of making an accurate diagnosis is highlighted. The patients remain healthy and symptom-free after follow-up of 1 year. Frozen sections may help in deciding the extent of resection intraoperatively. Although heterotopic pancreas is rare, it should be considered in the differential diagnosis of gastrointestinal stromal tumor.
Keywords: Heterotopic pancreas, Gastrointestinal stromal tumor, Carcinoid syndrome, Ultrasonography, Gastroscopy
INTRODUCTION
Heterotopic pancreas is defined as pancreatic tissue found outside the usual anatomical location of the pancreas. It is usually found in the upper gastrointestinal tract. The incidence of heterotopic pancreas is low. Preoperative diagnose is difficult. Although echogastroscopy is helpful for diagnosis[1], it is difficult to distinguish from gastrointestinal stromal tumor (GIST). Frozen sections may help in deciding the extent of resection intraoperatively. We report two cases of heterotopic pancreatic lesions in the duodenum and gastric antrum.
CASE REPORT
Case 1
A 60-year-old man presented to the gastroenterology outpatient clinic complaining of joint pain all over the body of 2 years duration, and abdominal distension for 1.5 years. He had a history of dermatomyositis. Physical examination revealed some symptoms of carcinoid syndrome including face rubeosis, abdominal bulge, and abdominal distention after walking for several minutes. Laboratory findings were that routine blood examination was normal, blood clotting and erythrocyte sedimentation rate were normal, postprandial blood sugar was 11.10 mmol/L, anti-dsDNA antibody, anti-O antibody and antinuclear antibody were normal, serum rheumatoid factor was 34.00 IU/mL, total cholesterol was 6.1 mmol/L, triglyceride was 2.85 mmol/L, 24-h urinary protein was normal, tumor markers were normal except that CA72-4 was a little high. Epigastric CT revealed a duodenal bulb submucosal lump that showed exophytic growth, which was possibly a benign GIST. Gastroscopy revealed chronic atrophic gastritis. Echogastroscopy revealed a mass in the duodenal submucosa, which might have been GIST. The patient underwent exploratory laparotomy after general anesthesia. During the operation, surgeons discovered that there was a tenacious mass in the duodenal bulb subserosa, with a diameter of 1.5 cm, and it did not encroach on mucosal membrane. Local excision was carried out, and frozen sections showed heterotopic pancreas in the duodenal bulb. After surgery, paraffin sections showed that heterotopic pancreas in the duodenal bulb with papillary hyperplasia of the pancreatic duct epithelium. He was discharged 10 d after surgery without face rubeosis or abdominal distention after walking. He remained in good health during follow-up.
Case 2
A 62-year-old man complained of repeated, vague right upper quadrant pain for 2 years. Physical examination and laboratory findings were unremarkable. Endoscopy showed a solid tumor mass in the gastric antrum (Figure 1). Epigastric zone CT also showed a mass in the gastric antrum (Figure 2). Echogatstroscope showed that there was a solid tumor mass under the mucosal membrane in the gastric antrum (Figure 3), which was suggestive of GIST (a low-echogenicity mass under the gastric wall submucosal muscularis propria, with a clear boundary and uneven internal echo, and measuring 24.6 mm × 16.5 mm). Tumor markers were normal. During the operation, surgeons discovered that there was a tenacious mass with a diameter of 2 cm in the gastric antrum, which was considered to be GIST. Partial gastrectomy was performed because endoscopy could not rule out the possibility of malignancy. Frozen and paraffin sections showed heterotopic pancreas in the gastric antrum (Figure 4). He was discharged 14 d after surgery without abdominal pain or complications. He remained in good health during follow-up.
Figure 1.
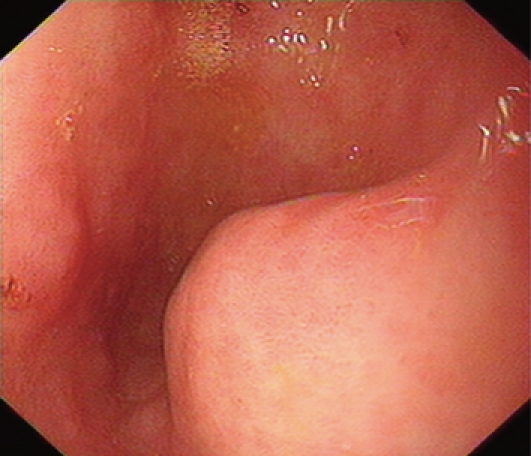
Endoscopy showing a solid tumor mass under the mucosal membrane in the gastric antrum.
Figure 2.

CT reconstruction showing a mass with a diameter of 2 cm in the gastric antrum.
Figure 3.
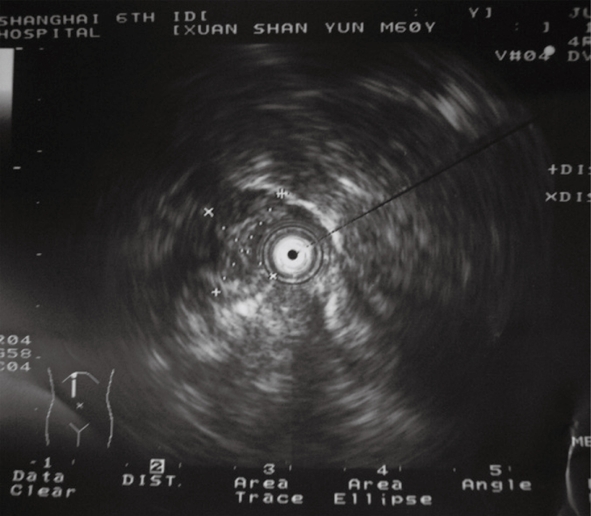
Echogatstroscope revealing low-echogenicity mass under the gastric wall submucosal muscularis propria, with a clear boundary and uneven internal echogenicity.
Figure 4.
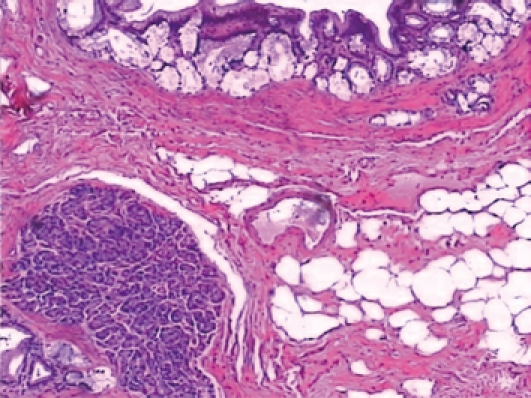
Lobules of pancreatic tissue with ducts located within the smooth muscle of the pylorus (HE, × 100).
DISCUSSION
Jean-Schultz was the first to report that heterotopic pancreas is pancreatic tissue found outside the usual anatomical location of the pancreas[2]. It is a congenital abnormality. Its precise incidence rate has not been reported either in China or abroad, but it is very low. The incidence rate is 0.11%-0.21% at autopsy, with a male to female ratio of 3:1[3]. Heterotopic pancreas can exist at any position in the abdominal cavity. It is usually found in the upper gastrointestinal tract, with > 90% of the cases involving the stomach, duodenum or jejunum. Unusual locations are the colon, spleen or liver[4,5]. Heterotopic pancreas is usually buried in the submucosa, which makes it difficult to distinguish from GIST[4,6–8]. The diameter of heterotopic pancreatic tissue is generally about 1-2 cm, and in our cases, the diameter was 1.5-2 cm.
Patients with heterotopic pancreas can be normal, or present with abdominal pain and distension. In addition, it can manifest clinically in some rare diseases of the pancreas including pancreatitis, islet cell tumor, pancreatic carcinoma, and pancreatic cyst[9]. In our study, one of the patients revealed some symptoms of carcinoid syndrome, which is rare, including face rubeosis, abdominal bulging, and abdominal distention after walking for several minutes. There is no specific examination and diagnostic method at present, and it is difficult to diagnose this disease definitely before laparotomy[2,10,11]. Echogatstroscope, CT and gastroscopy can be helpful in diagnosis. The literature shows that the rate of diagnosis of this disease is high with echogatstroscope[1]. In our two patients, echogatstroscope and epigastric CT before laparotomy did not reveal heterotopic pancreas, and diagnosis was dependent on frozen or paraffin sections postoperatively. Heterotropic pancreas should be considered in the differential diagnosis of GIST. Medical treatment is not effective for heterotropic pancreas, and surgical excision is the first and best choice[12–14]. It is often impossible to distinguish gastric heterotopic pancreas from primary or metastatic cancer because endoscopic biopsies are often unremarkable. Therefore, frozen sections should be taken rapidly and routinely so as to confirm the diagnosis and avoid unwanted radical surgery such as Whipple’s procedure or subtotal gastrectomy. Heterotopic pancreas may manifest some symptoms of carcinoid syndrome, and surgical treatment may eliminate such symptoms. Asymptomatic heterotopic pancreas is hard to diagnose. The treatment of asymptomatic histologically verified gastric heterotopic pancreas is debatable[15].
In summary, the incidence of heterotopic pancreas is low and preoperative diagnosis is difficult. Although echogatstroscope is helpful for diagnosis[1], it is difficult to distinguish from GIST. Frozen sections should be taken so as to distinguish heterotropic pancreas from malignant tumor.
Peer reviewers: Tadatoshi Takayama, Professor, Department of Digestive Surgery, Nihon University School of Medicine, 30-1 Oyaguchikami-machi, Itabashi-ku, Tokyo 173-8610, Japan; Salvatore Gruttadauria, MD, Assistant Professor, Abdominal Transplant Surgery, ISMETT, Via E. Tricomi, 190127 Palermo, Italy
S- Editor Tian L L- Editor Kerr C E- Editor Zheng XM
References
- 1.Galloro G, Napolitano V, Magno L, Diamantis G, Nardone G, Bruno M, Mollica C, Persico G. Diagnosis and therapeutic management of cystic dystrophy of the duodenal wall in heterotopic pancreas. A case report and revision of the literature. JOP. 2008;9:725–732. [PubMed] [Google Scholar]
- 2.Jiang LX, Xu J, Wang XW, Zhou FR, Gao W, Yu GH, Lv ZC, Zheng HT. Gastric outlet obstruction caused by heterotopic pancreas: A case report and a quick review. World J Gastroenterol. 2008;14:6757–6759. doi: 10.3748/wjg.14.6757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mulholland KC, Wallace WD, Epanomeritakis E, Hall SR. Pseudocyst formation in gastric ectopic pancreas. JOP. 2004;5:498–501. [PubMed] [Google Scholar]
- 4.Chandan VS, Wang W. Pancreatic heterotopia in the gastric antrum. Arch Pathol Lab Med. 2004;128:111–112. doi: 10.5858/2004-128-111-PHITGA. [DOI] [PubMed] [Google Scholar]
- 5.Karahan OI, Kahriman G, Soyuer I, Artiş T, Comu NB. MR cholangiopancreatography findings of heterotopic pancreatic tissue in the distal common bile duct. Diagn Interv Radiol. 2006;12:180–182. [PubMed] [Google Scholar]
- 6.Thoeni RF, Gedgaudas RK. Ectopic pancreas: usual and unusual features. Gastrointest Radiol. 1980;5:37–42. doi: 10.1007/BF01888597. [DOI] [PubMed] [Google Scholar]
- 7.Chak A, Canto MI, Rösch T, Dittler HJ, Hawes RH, Tio TL, Lightdale CJ, Boyce HW, Scheiman J, Carpenter SL, et al. Endosonographic differentiation of benign and malignant stromal cell tumors. Gastrointest Endosc. 1997;45:468–473. doi: 10.1016/s0016-5107(97)70175-5. [DOI] [PubMed] [Google Scholar]
- 8.Sukumar N, Teoh CM. Heterotopic pancreas in the stomach. Med J Malaysia. 2004;59:541–543. [PubMed] [Google Scholar]
- 9.Rimal D, Thapa SR, Munasinghe N, Chitre VV. Symptomatic gastric heterotopic pancreas: clinical presentation and review of the literature. Int J Surg. 2008;6:e52–e54. doi: 10.1016/j.ijsu.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Shi HQ, Zhang QY, Teng HL, Chen JC. Heterotopic pancreas: report of 7 patients. Hepatobiliary Pancreat Dis Int. 2002;1:299–301. [PubMed] [Google Scholar]
- 11.Mönig SP, Selzner M, Raab M, Eidt S. Heterotopic pancreas. A difficult diagnosis. Dig Dis Sci. 1996;41:1238–1240. doi: 10.1007/BF02088243. [DOI] [PubMed] [Google Scholar]
- 12.Ayantunde AA, Pinder E, Heath DI. Symptomatic pyloric pancreatic heterotopia: report of three cases and review of the literature. Med Sci Monit. 2006;12:CS49–CS52. [PubMed] [Google Scholar]
- 13.Erkan N, Vardar E, Vardar R. Heterotopic pancreas: report of two cases. JOP. 2007;8:588–591. [PubMed] [Google Scholar]
- 14.Lucandri G, Castaldo P, Meloni E, Ziparo V. [Ectopic pancreas with gastric localization: a clinical case and review of the literature] G Chir. 1994;15:162–166. [PubMed] [Google Scholar]
- 15.Ormarsson OT, Gudmundsdottir I, Mårvik R. Diagnosis and treatment of gastric heterotopic pancreas. World J Surg. 2006;30:1682–1689. doi: 10.1007/s00268-005-0669-6. [DOI] [PubMed] [Google Scholar]


