Abstract
Background
Most health behavior models do not distinguish between determinants of behavior adoption and maintenance.
Purpose
This study compared psychosocial predictors of physical activity (PA) adoption and predictors of PA maintenance among 205 initially sedentary adults enrolled in a home-based PA promotion trial.
Methods
Psychosocial variables were measured at 6 months (at which point 107 participants remained inactive and 98 participants adopted regular PA) and used to predict 12-month PA status (an indicator of PA adoption among those inactive at 6 months and an indicator of PA maintenance among those active at 6 months).
Results
6-month PA status moderated the relationships between 6-month measures of home access to PA equipment (p = .049), self-efficacy (p = .086), and perceived satisfaction (p = .062) and 12-month PA status. Simple effects analyses revealed that home access to PA equipment was predictive of PA adoption (OR = 1.73; 95% CI: 1.05, 2.85), but not PA maintenance (OR = 0.88; 95% CI: 0.58, 1.35), whereas self-efficacy and perceived satisfaction were predictive of PA maintenance (OR = 2.65; 95% CI: 1.55, 4.52; OR = 1.95; 95% CI: 0.93, 4.06), but not PA adoption (OR = 1.50; 95% CI: 0.87, 2.57; OR = 0.82, CI: 0.44, 1.52).
Conclusion
Results suggest that these psychosocial variables may operate differently in predicting PA adoption versus maintenance.
Keywords: Adoption, Maintenance, Physical Activity, Social Cognitive Theory, Perceived Satisfaction
Psychosocial Predictors of Physical Activity Adoption and Maintenance
Regular physical activity has been linked to numerous health benefits (1, 2) and increasing physical activity is an important goal in Healthy People 2010 (2). The Surgeon General (1) recommends use of theoretical models, including social cognitive theory (SCT) and the transtheoretical model (TTM), to help design interventions for physical activity promotion. The TTM posits that 10 processes of change, adapted from multiple behavior change theories, are critical in helping formulate intentions, adopt a behavior, and maintain the behavior over time (3). Also critical to behavior change efforts are anticipated benefits (pros) and costs (cons) of physical activity (i.e., decisional balance). Specifically, the TTM posits that decisional balance and cognitive processes of change are more important during behavior adoption, whereas behavioral processes are more important to behavior maintenance (4). TTM constructs have been shown to be predictive of physical activity behavior (e.g., 5) and numerous physical activity promotion interventions have been based on the TTM (e.g., 6, 7).
SCT emphasizes the importance of self-efficacy, defined as one’s confidence that he or she can regularly engage in physical activity in the face of salient impediments (8). Other constructs, such as expected outcomes of physical activity, social support, and environmental access to physical activity facilities, also fit within the larger social-cognitive framework (8), and have been shown to predict physical activity behavior (e.g., 9, 10). Although SCT has been used extensively in studies examining predictors of physical activity behavior (for reviews, see 11, 12) and as the foundation for interventions promoting physical activity (e.g., 13)}, it has been criticized for not distinguishing between the determinants of behavior adoption versus behavior maintenance (14). For example, SCT posits that personal (i.e., self-efficacy) and environmental (i.e., social support) factors are critical to behavior maintenance; however, these factors do not differ from those that are posited to influence behavior adoption (8, 15, 16). Rothman and colleagues (14, 17) have posited a framework, grounded in SCT, which distinguishes between determinants of behavior adoption and behavior maintenance. In the context of this framework, they hypothesize that self-efficacy and outcome expectancies are most critical to behavior adoption, but social support and perceived satisfaction with the outcomes of initial attempts at behavior change are more important as determinants of behavior maintenance.
As indicated by Rothman and colleagues (17), “One way to discern whether a construct’s impact shifts as a function of phase is to separate individuals into subgroups according to their phase, then test its relative ability to predict behavior prospectively within each subgroup” (p. 140). Previous studies examining predictors of physical activity adoption and maintenance have, in predicting behavior maintenance, included all participants who reached a specific time point in the study (e.g., 6 or 12 months) regardless of whether they were active or inactive at that time point (18–20). This approach does not allow for a comparison of the predictors of adoption and maintenance. Other studies, consistent with Rothman and colleagues’ (17) suggestion, have divided participants into active versus inactive subgroups and then examined predictors of physical activity adoption in one subgroup and physical activity maintenance in the other subgroup (21–25). However, these studies have not directly compared predictors of physical activity adoption and maintenance by examining initial physical activity status as a moderator of relationships between the predictors and subsequent physical activity levels. Moreover, some of these studies used retrospective data to divide participants into active versus inactive subgroups at baseline (22–25). The disadvantage of a retrospective approach is that it results in heterogeneity within the active subgroup, such that participants who were active at baseline may have been regular exercisers who had been exercising for a period of several years or more or novice exercisers who recently adopted exercise. Finally, no studies that we know of have compared the SCT constructs of perceived satisfaction, enjoyment, or environmental access as predictors of physical activity adoption versus maintenance within the same study.
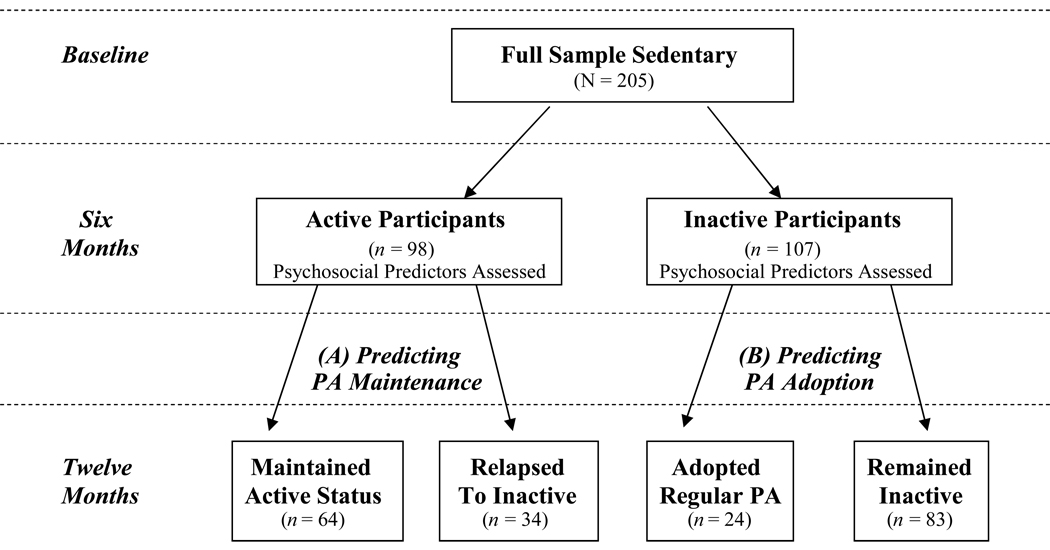
The purpose of the present study was to directly compare theoretical predictors of physical activity adoption versus maintenance among healthy adults enrolled in a physical activity promotion trial. All participants were sedentary at baseline and after 6 months in the trial, had either adopted regular physical activity or remained inactive. Psychosocial variables were measured at 6 months and used to predict 12-month physical activity status. Thus, 12-month physical activity status was an indicator of physical activity adoption among those who were inactive at 6 months and an indicator of physical activity maintenance among those who were regularly active at 6 months (Figure 1). In order to directly compare predictors of adoption and maintenance, 6-month physical activity status was examined as a moderator of relationships between each psychosocial predictor measured at 6 months and 12-month physical activity status.
Figure 1.
Participant Flow Chart and Plan for Predicting Physical Activity Maintenance (A) and Adoption (B).
Consistent with Rothman and colleague’s (14, 17) framework, we hypothesized that self-efficacy and outcome expectations would be more important for physical activity adoption, but that social support and perceived satisfaction (including perceived enjoyment) would be more important for physical activity maintenance. Additionally, consistent with the TTM, we hypothesized that decisional balance and cognitive process of change would be more important for physical activity adoption, while behavioral processes would be more important for physical activity maintenance (4). Finally, because neither SCT (8, 15, 16) nor Rothman and colleague’s (17) offer clear hypotheses, we explored the relative role of environmental access in physical activity adoption versus maintenance.
Methods
Participants
Participants were healthy, previously sedentary adults enrolled in a randomized controlled physical activity promotion trial, recruited primarily through local newspaper advertisements (for a full description of recruitment procedures see 26). A majority of participants were recruited from the Providence, RI area; however, in order to obtain a more diverse sample, 25% of participants were recruited from the Pittsburgh, PA area. For the purposes of this study, of the 249 participants randomized at baseline, we retained the 205 participants who provided physical activity data at both 6 and 12 months. The study was approved by The Miriam Hospital and University of Pittsburgh Institutional Review Boards and all participants provided written consent to participate.
Measures
Physical activity
The 7-Day Physical Activity Recall (PAR) interview was used to assess physical activity. This interview asks participants to recall sitting, sleep, and physical activity frequency and duration during the previous seven days. Several studies have demonstrated both the reliability and validity of the PAR (for reviews, see 27, 28). We took a number of steps to reduce bias and increase consistency of interview administration, including (a) having one Masters-level staff member, who was blinded to participant condition, conducted all of the 7-Day PARs; (b) audio-recording all 7-Day PAR interviews with independent scoring of a random subsample, and quarterly feedback sessions in which feedback was given based on interview discrepancies; and (c) demonstrating moderate intensity at baseline via a practice brisk walk and asking participants to refer to that demonstration when reporting their activity.
Self-efficacy
We measured self-efficacy using a 5-item questionnaire examining confidence in participating in physical activity in five different situations (i.e., bad weather, vacation, bad mood, feeling tired, and not having enough time; 29). This measure has shown test-retest reliability of .90 over 2 weeks (29), and has been significantly predictive of physical activity behavior in previous studies (5, 21). Internal consistency was .86 in the present study at 6 months.
Decisional balance
Decisional balance was assessed using a 16-item questionnaire (30) that assesses beliefs about the pros (i.e., benefits) and cons (i.e., costs) of physical activity. A decisional balance index score is computed based on the number of pros and cons endorsed. Decisional balance has significantly predicted physical activity behavior in previous studies (5, 21). In the present study, the internal consistency for the Pros subscale was .94 and .85 for the Cons subscale at 6 months.
Processes of change
We used a 40-item scale to assess cognitive and behavioral processes of change (31). Both cognitive and behavioral processes of change have been significantly predictive of physical activity behavior in previous studies (5, 21). Cognitive processes were derived from the following five subscales: (1) environmental reevaluation (caring about consequence to others); (2) self reevaluation (comprehending benefits); (3) social liberation (increasing healthy opportunities); (4) consciousness raising (increasing knowledge); and (5) dramatic relief (warning of risks). Behavioral processes were derived from the following five subscales: (1) Committing yourself; (2) reminding yourself; (3) substituting alternatives; (4) enlisting social support; and (5) rewarding yourself. In the present study, the average internal consistency for the subscales was .86 at 6 months.
Outcome expectations
We examined outcome expectations using a 19-item measure, in which participants are asked to rate their agreement with potential benefits of physical activity such as: “A major benefit of physical activity for me is good health” (32). In the initial study, the scale significantly predicted physical activity behavior in college and worksite samples (32). The internal consistency was .91 in the present study at 6 months.
Physical activity enjoyment
The 18-item Physical Activity Enjoyment Scale (PACES) was used to measure perceived attributes and enjoyment of physical activity. One study found that the test-retest reliability was .60 for bicycling and .93 for jogging (33). In this study, level of physical activity enjoyment was significantly related to type of physical activity chosen (33). This scale has also been significantly predictive of physical activity behavior (34). The internal consistency was .95 in the present study at 6 months.
Perceived satisfaction
Perceived satisfaction was measured with a 24-item scale adapted from Sears and Stanton (35). In that study, perceived satisfaction with physical activity as part of a weight-loss program was significantly predictive of adherence to the program. In the present study internal consistency was .96 at 6 months.
Social support
We assessed social support with a 13-item scale examining social support for physical activity from family and friends (calculated separately). In the validation study, the test-retest reliability ranged from .55 to .79, and the level of social support score significantly correlated with vigorous activity (36). Internal consistency in the present study ranged from .91 to .92 at 6 months.
Environmental access
The environmental access measure examines environmental barriers and facilitators to physical activity (9). The one-week test-retest reliability of this measure ranges from .68 - .89, and the measure was shown to significantly correlate with access to convenient facilities and home equipment (9). In the present study the internal consistency was .84, .70, and .30 for the facilities, home, and neighborhood subscales at 6 months.
Procedures
Interested participants responded to recruitment advertisements by calling our study telephone number. Eligibility and baseline assessments were then conducted over three sessions prior to randomization into one of three physical activity promotion conditions (26). As part of the assessment protocol, participants completed psychosocial questionnaires and the PAR was administered at baseline, 6 and 12 months. All psychosocial questionnaires were completed at home and returned in-person at the 6-month follow-up appointment. We used last value carried forward to impute missing data from the 6-month psychosocial predictor variables for all participants who had reported physical activity data at both 6 and 12 months (N = 205; 15 cases imputed for enjoyment; 2–6 cases imputed for all other predictor variables). The perceived satisfaction measure was added after the start of the study, and therefore, because of the much smaller sample size, we did not impute data, but simply analyzed the observed cases (n = 111).
Data Analyses
The goals of the analyses were to (a) examine 6-month psychosocial predictors of 12 month physical activity status among the full sample; and (b) compare 6-month predictors of 12-month physical activity status among participants who were active versus inactive at 6 months. We conducted preliminary analyses to examine the differences in psychosocial variables at 6 months among participants who were active versus inactive at 6 months, and to examine bivariate relationships among the 6-month psychosocial variables. These analyses provided a preliminary test of construct validity, as it was expected that active participants would be higher than inactive participants on each of the psychosocial variables and that there would be numerous interrelationships among the 6-month psychosocial variables. Additionally, we sought to examine whether response tendencies on the 6-month psychosocial variables would differentially influence—across participants who were active versus inactive at 6 months—the ability of these variables to predict 12 month physical activity status. Thus, we examined the number of occurrences of extreme responses on each of the predictor variables among the two subgroups.
For this study, we were not interested in the effects of the intervention. Therefore, data were pooled across treatment arms and the effects of treatment were controlled in the analyses. We used logistic regression analyses, with 12-month physical activity status (i.e., active versus not active) as the dependent variable. Active was defined as participating in at least 150 minutes of at least moderate intensity physical activity per week or at least 60 minutes of vigorous intensity physical activity per week (1). We first examined the main effects of each psychosocial variable measured at 6 months on physical activity status at 12 months among all participants. Second, we examined physical activity status at 6 months as a moderator of the relationship between the psychosocial predictors measured at 6 months and 12-month physical activity status after controlling for the main effects of 6-month physical activity status and the corresponding predictor variable. Third, we examined simple effects for each significant moderator model by dividing participants into active and inactive sub-samples based on their physical activity status at 6 months and examining predictors of 12-month physical activity status. In all analyses, predictors were converted to z-scores, such that the resulting odds ratios (ORs) reflect the odds of being physically active at 12 months for each standard unit increase in the predictor variable.
Results
Table 1 summarizes characteristics of the study sample (i.e., participants from the main trial who reported physical activity data at both 6 and 12 months; N = 205). Not included in the study sample (n = 44) were 15 participants missing 6-month data, of whom 7 were active at 12 months and 8 were not; 17 participants missing 12-month data, of whom 6 were active at 6 months and 11 were not; and 12 participants missing both 6- and 12-month physical activity data. Participants included in the analyses (N = 205) were significantly lower at baseline on social support from friends (mean = 9.71, SD = 9.01; versus mean = 13.89, SD = 10.06; p = .014; Cohen’s d = .44) and social support from family (mean = 7.12, SD = 8.32; versus mean = 10.20, SD = 8.26; p = .028; d = .37) than participant who were excluded (n = 44). Additionally, a greater proportion of the subsample of participants who responded to the perceived satisfaction measure (n = 111)—versus those who did not respond (n = 138)—were African American (23.0% versus 7.3%; p < .01), because the perceived satisfaction measure was added after the start of the study and there was more targeted recruitment of minority participants later in the study. There were no other significant differences on demographics or baseline psychosocial variables between participants who were included versus not included in the present analyses (alpha = .05).
Table 1.
Characteristics of the Study Sample
| Full Sample (N = 205) |
Active at 6 Months (n = 107) |
Inactive at 6 Months (n = 98) |
|
|---|---|---|---|
| Mean Baseline BMI (SD) | 29.4 (6.1) | 28.8 (5.6) | 30.1 (6.6) |
| % Female | 83.9 | 85.0 | 82.7 |
| % Caucasian | 80.5 | 80.4 | 80.6 |
| % African American | 16.6 | 16.8 | 16.3 |
| % Other Race | 2.9 | 2.8 | 3.1 |
| % Hispanic | 1.5 | 1.9 | 1.0 |
| % Income > 50,000 | 54.6 | 52.3 | 57.1 |
| % College Grad | 68.3 | 71.0 | 65.3 |
| % Active at 12 Months | 42.9 | 65.3 | 22.4 |
BMI = Body Mass Index
Preliminary Analyses
Table 2 shows descriptive statistics for the psychosocial variables measured at 6 months among the full sample (N = 205), participants active at 6 months (n = 98), and participants inactive at 6 months (n = 107). As expected, participants who were active at 6 months were significantly higher on 9 of the 12 psychosocial variables, with non-significant trends in the expected direction for the other 3 variables and effect sizes (i.e., Cohen’s d) ranging from .17 to .73 (Table 2). Table 3 illustrates the numerous bivariate relationships among the 6-month psychosocial variables. Regarding extreme responses on the 6-month psychosocial variables, cell sizes were too small to conduct chi-square analyses; however, for most of the predictor variables there were few participants (i.e., < 5) whose 6-month scores were at either the lowest or highest possible value. Similarly, for most of the predictor variables, there were small differences (i.e., < 2) between the number of participants in each subgroup (i.e., active versus inactive at 6 months) whose 6-month scores were at either the lowest or highest possible value. Exceptions were: (a) outcome expectations, for which 17 participants who were inactive at 6 months versus 9 participants who were active at 6 months scored the highest possible value; (b) social support for family, for which 23 participants who were inactive at 6 months versus 10 participants who were active at 6 months scored the lowest possible value; and (c) social support for friends, for which 40 participants who were inactive at 6 months versus 22 participants who were active at 6 months scored the lowest possible value.
Table 2.
Mean (SD) for Psychosocial Predictors Measured at 6 Months for the Full Sample, Participants Active at 6 Months, and Participants Inactive at 6 Months
| Full Sample (N = 205) |
Active at 6 Months (n = 107) |
Inactive at 6 Months (n = 98) |
Cohen’s d for Difference between Active & Inactive |
|
|---|---|---|---|---|
| Self-Efficacy | 2.80 (0.92) | 3.13 (0.91)** | 2.50 (0.82)** | .73 |
| Decisional Balance | 0.17 (14.56) | 3.89 (13.42)** | −3.23 (14.79)** | .50 |
| Cognitive Processes | 3.00 (0.77) | 3.08 (0.77) | 2.93 (0.77) | .19 |
| Behavioral Processes | 2.96 (0.74) | 3.21 (0.68)** | 2.74 (0.72)** | .67 |
| Outcome Expectations | 4.12 (0.60) | 4.21 (0.51)* | 4.03 (0.67)* | .30 |
| Enjoyment | 84.45 (21.15) | 87.94 (20.89)* | 81.25 (20.98)* | .32 |
| Satisfactiona | 93.34 (26.29) | 100.58 (23.15)** | 85.70 (27.42)** | .59 |
| Social Support from Family | 9.71 (9.01) | 10.89 (8.93) | 8.63 (9.00) | .25 |
| Social Support from Friends | 7.12 (8.32) | 9.23 (9.18)** | 5.19 (6.96)** | .50 |
| Environ Access (Home) | 6.30 (2.91) | 6.84 (2.90)* | 5.80 (2.85)* | .36 |
| Environ Access (Neighborhood) | 5.56 (1.35) | 5.68 (1.30) | 5.45 (1.40) | .17 |
| Environ Access (Facilities) | 10.33 (4.24) | 10.97 (4.08)* | 9.74 (4.32)* | .29 |
p < .05
p < .01
for satisfaction, n = 111 for full sample, n = 57 for participants active at 6 months, n = 54 for participants inactive at 6 months
Table 3.
Bivariate Relationships among the 6-Month Psychosocial Variables (N = 205)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Self-efficacy | 1.00 | .47** | .38** | .68** | .49** | .55** | .57** | .37** | .30** | .27** | −.007 | .17* |
| 2. Decisional Balance | 1.00 | .49** | .53** | .65** | .49** | .16 | .18* | .21** | .20** | −.029 | .18* | |
| 3. Cognitive Processes | 1.00 | .73** | .50** | .31** | .05 | .37** | .29** | .20** | −.116 | .06 | ||
| 4. Behavioral Processes | 1.00 | .59** | .51** | .46** | .54** | .44** | .25** | −.034 | .12 | |||
| 5.Outcome Expectations | 1.00 | .58** | .37** | .19* | .19* | .24** | −.010 | .18* | ||||
| 6. Enjoyment | 1.00 | .38** | .19* | .21** | .22** | .04 | .26** | |||||
| 7. Satisfactiona | 1.00 | .23* | .07 | .21* | .09 | .19* | ||||||
| 8. Social Support from Family | 1.00 | .43** | .18** | .10 | .05 | |||||||
| 9. Social Support from Friends | 1.00 | .06 | .09 | .10 | ||||||||
| 10. Environ Access (home) | 1.00 | .06 | .27** | |||||||||
| 11. Environ Access (neighborhood) | 1.00 | .29** | ||||||||||
| 12. Environ Access (facilities) | 1.00 |
p < .05
p < .01
n = 111 for satisfaction
Main Effects of 6-Month Psychosocial Variables on 12-Month Physical Activity Status
Table 4 shows main effects of each predictor variable on 12-month physical activity status among the full sample (N = 205) when controlling for treatment condition. Following a Holm step-down procedure (37) self-efficacy, decisional balance, behavioral processes, outcome expectations, and enjoyment retained significance. Self-efficacy was the strongest predictor, with a 139% increase in odds of being physically active at 12 months with each one standard unit increase in self-efficacy.
Table 4.
Odds Ratios (95% CI) for 6-Month Predictors of 12-Month Physical Activity Status among the Full Sample of Participants (N = 205)
| OR (95% CI) | |
|---|---|
| Self-Efficacy | 2.39 (1.69, 3.36) |
| Decisional Balance | 1.70 (1.25, 2.32) |
| Cognitive Processes | 1.38 (1.03, 1.85) |
| Behavioral Processes | 1.92 (1.39, 2.65) |
| Outcome Expectations | 1.53 (1.13, 2.07) |
| Enjoyment | 1.71 (1.26, 2.32) |
| Satisfactiona | 1.48 (0.98, 2.24) |
| Social Support from Family | 1.35 (1.02, 1.80) |
| Social Support from Friends | 1.04 (0.79, 1.38) |
| Environ Access (Home) | 1.32 (0.99, 1.75) |
| Environ Access (Neighborhood) | 1.17 (0.88, 1.56) |
| Environ Access (Facilities) | 1.24 (0.93, 1.65) |
Note. All models controlled for treatment and used standardized versions of the predictor variables.
n = 111 for satisfaction
Moderator and Simple Effects Analyses
When controlling for treatment condition, 6-month physical activity status (i.e., active or inactive) moderated the relationship between home access to physical activity equipment measured at 6 months, and 12-month physical activity status (p = .049). Similarly, the interaction between 6-month physical activity status (i.e., active or inactive) and 6-month measures of self-efficacy (p = .086) and perceived satisfaction (p = .062) approached significance. No other moderator effects were found. Simple effects analyses revealed that home access to physical activity equipment was significantly predictive of physical activity adoption (OR = 1.73; 95% CI: 1.05, 2.85), but not physical activity maintenance (OR = .88; 95% CI: 0.58, 1.35), whereas self-efficacy was significantly predictive of physical activity maintenance (OR = 2.65; 95% CI: 1.55, 4.52), but not physical activity adoption (OR = 1.50; 95% CI: 0.87, 2.57). Similar to self-efficacy, perceived satisfaction was nearly significantly predictive of physical activity maintenance (OR = 1.95; 95% CI: 0.93, 4.06), but not physical activity adoption (OR = 0.82, CI: 0.44, 1.52).
Discussion
This study compared psychosocial predictors of physical activity adoption and maintenance. All participants were sedentary at baseline, and had either successfully adopted physical activity or remained inactive over an initial 6-month period. Scores on 6-month psychosocial variables were then used to predict 12-month physical activity status (i.e., active versus inactive). Consistent with SCT (8) and the TTM (3), a number of variables measured at 6 months were predictive of 12-month physical activity status among the full sample of participants, including self-efficacy, decisional balance, behavioral processes, outcome expectations, and enjoyment. Similarly, differences in means on each psychosocial variable for participants who were active at 6 months versus inactive at 6 months were in the expected direction, with weak effects (d < .2) for 2 of 12 variables, small-medium effects (d = .2-.5) for 5 of 12 variables, and medium-large effects (d = .5-.8) for 5 of the 12 variables (38). However, when predictors of adoption and maintenance were compared through moderator analyses, self-efficacy and perceived satisfaction were more important in predicting physical activity maintenance than physical activity adoption, whereas access to home exercise equipment was more important in predicting physical activity adoption than physical activity maintenance.
In general, the results of the moderator analyses were not consistent with Rothman and colleagues’ (17) model, which proposes that self-efficacy and outcome expectancies are critical for behavior adoption, while perceived satisfaction and social support are more important predictors of behavior maintenance. Perceived satisfaction was more important during physical activity maintenance than during physical activity adoption, which is consistent with the model; but, self-efficacy was also more important for physical activity maintenance than physical activity adoption, which is contrary to the model. The latter finding may have been influenced by lack of experience with the target behavior among the inactive group when completing the self-efficacy measure at 6 months, as Bandura (8) has noted that participants must have some level of experience with the target behavior in order to have a basis for judging their self-efficacy. Also contrary to the model, neither outcome expectations nor decisional balance was a stronger predictor of physical activity adoption compared to physical activity maintenance. It should be noted, however, that the measure of outcome expectations grouped together the physical, social, and self-evaluative outcomes theorized to influence behavior (8). Thus, future research should examine the relative influence of these expectancy subtypes on physical activity adoption and maintenance.
Findings also did not support the TTM’s principle that cognitive processes of change are more important during behavior adoption and behavioral processes are more important during behavior maintenance (4). In the current study, both cognitive and behavioral processes were predictive of 12-month physical activity status, but there was no difference in these relationships among those who were inactive at 6 months and attempting physical activity adoption compared to those who were active at 6 months and attempting to maintain physical activity. Though contrary to the TTM, the present findings are consistent with previous research in the physical activity domain (39).
Finally, results also suggest that home access to exercise equipment may be more important during physical activity adoption than maintenance. According to SCT, the environment is important to both exercise adoption and maintenance (8). Its relative importance in predicting physical activity adoption versus maintenance is a novel finding that requires further study.
The strengths of the study include its longitudinal design and direct, statistical comparison of predictors of physical activity adoption versus maintenance. Additionally, unlike previous studies, which have relied on retrospective data to determine who was active or inactive at baseline (22–25) in this study all participants were sedentary at baseline and were followed for 6 months to determine their initial physical activity status. Moreover, previous studies have looked at predictors of physical activity “maintenance” by examining all participants, regardless of their initial physical activity status (18–20). As can be seen from the present results, separating out active and inactive participants can lead to different conclusions about the predictors of physical activity maintenance.
There were a number of limitations to the study. First, in order to operationally define adoption and maintenance, continuous physical activity data, as measured by the PAR, were used to classify participants into active versus inactive categories consistent with national guidelines (1). Thus, despite the multiple strategies used to reduce measurement error, there is the possibility of misclassification error (40, 41). Second, there was a large amount of missing data for the perceived satisfaction measure, resulting in a small sample size for analyses involving this variable. However, as noted above, the missing data resulted from late addition of the measure to the study protocol, instead of participant non-response. Nonetheless, the small sample size for this variable resulted in reduced power in the corresponding analyses. Third, the internal consistency for the neighborhood environmental access measure was low (i.e., 30); thus, further investigation into the influence of this variable on adoption and maintenance of physical activity is warranted. Fourth, although there were numerous bivariate relationships among the psychosocial predictor variables, the small sample size, relative to the number of predictor variables, precluded more sophisticated modeling techniques that are needed to understand more complex interrelationships among key variables in the adoption and maintenance processes. Fifth, due to the time elapsed between measurement of the predictors and the dependent variable (i.e., 6 months), the present analyses provide only a snapshot of the potential processes involved in physical activity adoption and maintenance, including potential changes in the predictors and/or the dependent variable. Sixth, despite recruitment of men and women, the sample was predominantly female (83.9%). Although this is typical for physical activity promotion trials (6, 7, 42), more research is needed among men to ensure generalizability of the findings.
Additionally, after conducting multiple tests for moderation, only home access to physical activity equipment was a statistically significant moderator (alpha = .05). Moreover, in conducting the moderator analyses it was necessary to examine all participants at the same time point. As a result, the analysis compares predictors of physical activity maintenance to predictors of what might be considered delayed physical activity adoption among a group of participants who did not immediately adopt physical activity over the first 6 months of an intervention program. The predictors of immediate physical activity adoption may be different from predictors of delayed adoption. Thus, an alternative approach would be to examine predictors of initial adoption among a sedentary sample, and then to examine predictors of maintenance among a sub-sample that has successfully adopted the behavior. In this approach, however, the two sets of predictors cannot be statistically compared through moderator analysis due to the different time frames. Thus, a combination of research approaches may be necessary to uncover differences between predictors of physical activity adoption and maintenance.
Finally, as with all observational research, the findings cannot be used to draw causal conclusions concerning determinants of physical activity adoption and maintenance. Instead, the findings may be viewed as a means for generating hypotheses to be tested in experimental research (43). Importantly, the present findings provide initial indication that different variables may operate in predicting physical activity adoption versus maintenance and highlight the need for separate examination of psychosocial predictors among those who are initially active versus inactive.
Acknowledgments
This project was supported in part through grants from the National Heart, Lung, and Blood Institute (R01 HL69866 to Dr. Marcus and F32 HL78709 to Dr. Williams) and a career development award (Dr. Williams, Scholar; Dr. Coustan, PI) from the National Institute of Child Health and Human Development (K12 HD043447). This study was performed at the Centers for Behavioral and Preventive Medicine at Brown Medical School and The Miriam Hospital. We would like to thank Santina Horowitz , B.S., Jaime Longval, M.S., and Susan Pinheiro, B.S. for research assistance and Barbara Doll for her assistance with manuscript preparation. Special thanks to Co-Investigators on R01 HL69866: Anna Albrecht, M.S., R.N., John Jakicic, Ph.D., Charles Neighbors, Ph.D., Alfred Parisi, M.D., Christopher Sciamanna, M.D., and Deborah Tate, Ph.D.
Contributor Information
David M. Williams, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, and Alpert Medical School of Brown University
Beth A. Lewis, School of Kinesiology, University of Minnesota
Shira Dunsiger, Program in Public Health, Brown University
Jessica A. Whiteley, Department of Exercise and Health Sciences, University of Massachusetts
George D. Papandonatos, Program in Public Health, Brown University
Melissa A. Napolitano, Department of Kinesiology, Temple University
Beth C. Bock, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, Alpert Medical School of Brown University, and Program in Public Health, Brown University.
Joseph T. Ciccolo, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, and Alpert Medical School of Brown University
Bess H. Marcus, Centers for Behavioral and Preventive Medicine, The Miriam Hospital, and Alpert Medical School of Brown University
References
- 1.U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 2.U.S. Department of Health and Human Services. 2nd ed. Washington, DC: U.S. Government Printing Office; 2000. Healthy People 2010: Understanding and Improving Health. [Google Scholar]
- 3.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 4.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 5.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. doi: 10.1037/0278-6133.27.4.409. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcus BH, Lewis BA, Williams DM, et al. A comparison of internet and print-based physical activity interventions. Arch Intern Med. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 7.Marcus BH, Napolitano MA, King AC, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol. 2007;26(4):401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 8.Bandura A. New York: W.H. Freeman and Co; 1997. Self-Efficacy: The Exercise of Control. [Google Scholar]
- 9.Sallis JF, Johnson MF, Calfas KJ, Caparosa S, Nichols JF. Assessing perceived physical environmental variables that may influence physical activity. Res Q Exerc Sport. 1997;68(4):345–351. doi: 10.1080/02701367.1997.10608015. [DOI] [PubMed] [Google Scholar]
- 10.Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006;25(4):510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- 11.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc Sport Sci Rev. 2000;28(2):85–88. [PubMed] [Google Scholar]
- 12.Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Ann Behav Med. 2005;29(1):70–79. doi: 10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]
- 13.Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T. Guide to health: nutrition and physical activity outcomes of a group-randomized trial of an Internet-based intervention in churches. Ann Behav Med. 2007;33(3):251–261. doi: 10.1007/BF02879907. [DOI] [PubMed] [Google Scholar]
- 14.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19(1 Suppl):64–69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Englewood Cliffs, NJ: Prentice-Hall; 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. [Google Scholar]
- 16.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 17.Rothman AJ, Baldwin A, Hertel A. Self-regulation and behavior change: Disentangling behavioral initiation and behavioral maintenance. In: Vohs K, Baumeister R, editors. Handbook of Self-Regulation. New York: Guilford Press; 2004. pp. 130–148. [Google Scholar]
- 18.McAuley E, Jerome GJ, Elavsky S, Marquez DX, Ramsey SN. Predicting long-term maintenance of physical activity in older adults. Prev Med. 2003;37(2):110–118. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 19.Stiggelbout M, Hopman-Rock M, Crone M, Lechner L, van Mechelen W. Predicting older adults' maintenance in exercise participation using an integrated social psychological model. Health Educ Res. 2006;21(1):1–14. doi: 10.1093/her/cyh037. [DOI] [PubMed] [Google Scholar]
- 20.Litt MD, Kleppinger A, Judge JO. Initiation and maintenance of exercise behavior in older women: predictors from the social learning model. J Behav Med. 2002;25(1):83–97. doi: 10.1023/a:1013593819121. [DOI] [PubMed] [Google Scholar]
- 21.Bock BC, Marcus BH, Pinto BM, Forsyth LH. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med. 2001;23(2):79–87. doi: 10.1207/S15324796ABM2302_2. [DOI] [PubMed] [Google Scholar]
- 22.Sallis JF, Hovell MF, Hofstetter CR. Predictors of adoption and maintenance of vigorous physical activity in men and women. Prev Med. 1992;21(2):237–251. doi: 10.1016/0091-7435(92)90022-a. [DOI] [PubMed] [Google Scholar]
- 23.Boutelle KN, Jeffery RW, French SA. Predictors of vigorous exercise adoption and maintenance over four years in a community sample. Int. J Behav Nutr Phys Act. 2004;1(1):13. doi: 10.1186/1479-5868-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhodes RE, Plotnikoff RC. Understanding action control: predicting physical activity intention-behavior profiles across 6 months in a Canadian sample. Health Psychol. 2006;25(3):292–299. doi: 10.1037/0278-6133.25.3.292. [DOI] [PubMed] [Google Scholar]
- 25.Burton LC, Shapiro S, German PS. Determinants of physical activity initiation and maintenance among community-dwelling older persons. Prev Med. 1999;29(5):422–430. doi: 10.1006/pmed.1999.0561. [DOI] [PubMed] [Google Scholar]
- 26.Marcus BH, Lewis BA, Williams DM, Step into Motion: a randomized trial examining the relative efficacy of Internet vs, et al. print-based physical activity interventions. Contemp Clin Trials. 2007;28(6):737–747. doi: 10.1016/j.cct.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 Suppl):S1–S205. [PubMed] [Google Scholar]
- 28.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(2 Suppl):S1–S14. [PubMed] [Google Scholar]
- 29.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 30.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11(4):257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 31.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11(6):386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 32.Steinhardt MA, Dishman RK. Reliability and validity of expected outcomes and barriers for habitual physical activity. J Occup Med. 1989;31(6):536–546. doi: 10.1097/00043764-198906000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Kendzierski D, DeCarlo KJ. Physical Activity Enjoyment Scale: two validation studies. J Sport Exerc Psychol. 1991;13:50–64. [Google Scholar]
- 34.Williams DM, Papandonatos GD, Napolitano MA, Lewis BA, Whiteley JA, Marcus BH. Perceived enjoyment moderates the efficacy of an individually tailored physical activity intervention. J Sport Exerc Psychol. 2006;28:300–309. [Google Scholar]
- 35.Sears SR, Stanton AL. Expectancy-value constructs and expectancy violation as predictors of exercise adherence in previously sedentary women. Health Psychol. 2001;20(5):326–333. [PubMed] [Google Scholar]
- 36.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 37.Holm S. A simple sequentially rejective Bonferroni test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 38.Cohen J. AtA power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 39.Marshall SJ, Biddle SJ. The transtheoretical model of behavior change: a meta-analysis of applications to physical activity and exercise. Ann Behav Med. 2001;23(4):229–246. doi: 10.1207/S15324796ABM2304_2. [DOI] [PubMed] [Google Scholar]
- 40.Sarkin JA, Nichols JF, Sallis JF, Calfas KJ. Self-report measures and scoring protocols affect prevalence estimates of meeting physical activity guidelines. Med Sci Sports Exerc. 2000;32(1):149–156. doi: 10.1097/00005768-200001000-00022. [DOI] [PubMed] [Google Scholar]
- 41.De Moor C, Baranowski T, Cullen KW, Nicklas T. Misclassification associated with measurement error in the assessment of dietary intake. Public Health Nutr. 2003;6(4):393–399. doi: 10.1079/PHN2002446. [DOI] [PubMed] [Google Scholar]
- 42.King AC, Friedman R, Marcus B, et al. Ongoing physical activity advice by humans versus computers: the Community Health Advice by Telephone (CHAT) trial. Health Psychol. 2007;26(6):718–727. doi: 10.1037/0278-6133.26.6.718. [DOI] [PubMed] [Google Scholar]
- 43.Weinstein ND. Misleading tests of health behavior theories. Ann Behav Med. 2007;33(1):1–10. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]