Abstract
In the last decade, a number of quantitative epidemiological studies of specific diseases have been done in developing countries that for the first time allow estimation of the total burden of disease (mortality and morbidity) attributable to use of solid fuels in adult women and young children, who jointly receive the highest exposures because of their household roles. Few such studies are available as yet for adult men or children over 5 years. This paper evaluates the existing epidemiological studies and applies the resulting risks to the more than three-quarters of all Indian households dependent on such fuels. Allowance is made for the existence of improved stoves with chimneys and other factors that may lower exposures. Attributable risks are calculated in reference to the demographic conditions and patterns of each disease in India. Sufficient evidence is available to estimate risks most confidently for acute respiratory infections (ARI), chronic obstructive pulmonary disease (COPD), and lung cancer. Estimates for tuberculosis (TB), asthma, and blindness are of intermediate confidence. Estimates for heart disease have the lowest confidence. Insufficient quantitative evidence is currently available to estimate the impact of adverse pregnancy outcomes (e.g., low birthweight and stillbirth). The resulting conservative estimates indicate that some 400–550 thousand premature deaths can be attributed annually to use of biomass fuels in these population groups. Using a disability-adjusted lost life-year approach, the total is 4–6% of the Indian national burden of disease, placing indoor air pollution as a major risk factor in the country.
Air pollution has become a major concern in India in recent years both because it is now clear that large parts of the Indian urban population are exposed to some of the highest pollutant levels in the world (1, 2) and also because new studies around the world on the health effects of air pollution have increased confidence in estimates of the risks posed by air pollution exposures (3, 4). The situation in China and a number of other developing countries is similar.
Overall premature mortality from outdoor urban air pollution has been calculated using exposure-response results from studies of urban outdoor pollution in developed countries to estimated air pollution levels based on the limited available measurements. Table 1 presents the results of such studies for India. Because they are most frequently measured worldwide and have been the subject of intense epidemiological investigation in the last 15 years, particulates are used in most studies as the indicator pollutant, although other health-damaging pollutants (SOx, volatile organics, NOx, O3, etc.) are also usually present.
Table 1.
Estimate of annual premature mortality from air pollution in India (thousands of deaths)
| Outdoor exp. ('000) | Indoor exp. ('000) | Pollutant used as indicator | Comments (ref.) |
|---|---|---|---|
| 50–300 | 850–3300 | PM | Using urban air quality data and rural exposures from rural microenvironment studies and urban distribution; MDC exposure-response information; range from spread between daily and annual studies (7) |
| 40 | — | PM | 36 cities based on MDC exposure-response data (8) |
| 86 | — | PM/SOx | Chinese exposure-response data (9) |
| 84 | 590 | PM | Using local air pollution monitoring data and Chinese exposure-response data (10, 11) |
| 200 | 2,000 | PM | Based on estimates of time and exposures in major microenvironments by important population groups and MDC exposure-response data (12) |
| 52 | — | PM | Extrapolation of ref. 8 with 1995 data (13) |
Most of these estimates applied the pollutant-based method discussed in the text. exp, exposure.
Annual concentrations reported at urban monitors in India for PM10, particles less than 10 microns in diameter,‡ range 90–600 μg/m3, with a population mean of about 200 μg/m3 (5). For comparison, at about 60 μg/m3, the most polluted urban area in the Unites States (6) in the early 1990s had annual concentrations substantially less than the cleanest Indian city reported, although, unlike the U.S. cities, many Indian cities are not yet instrumented. [The U.S. population mean is now less than 30 μg/m3 (2).]
Even higher concentrations result, however, from the widespread practice of using unprocessed solid fuels (biomass and coal) for cooking and/or space heating in India and other developing countries, often in unventilated situations. Such concentrations result from high emissions factors from such fuels in simple small-scale combustion devices (14, 15). The frequent result is indoor particulate concentrations well above even the dirtiest of cities (1). Available data show a distribution of indoor PM10 24-h concentrations measured in Indian solid-fuel-using households ranging to well over 2000 μg/m3. The distribution of village means overlap with the higher end of Indian urban concentrations but extends considerably higher. During the cooking period itself, of course, much higher levels are reached indoors (see the supplemental data, which are published on the PNAS web site at www.pnas.org). In addition, high household emissions from solid-fuel use result in elevated “neighborhood” pollution in densely populated communities (16).
In contrast to simple concentration, exposure is a function not only of the pollution level but also of the number of people involved and frequency and duration of their contact with the pollution—the number of person-hours of exposure (17). Few other activities involve as many person-hours as cooking does, because it is done in essentially every household every day in most of the world. The combination of high pollution levels in places with many person-hours is a prescription for large total population exposures. Indeed, indoor exposures to the combustion products of unprocessed solid fuels have been estimated to produce the majority of (nonsmoking) human exposures to particulates and probably to a range of other pollutants as well (1, 18). With its large, poor, urban and rural populations still using simple solid fuels, the Indian population bears a significant fraction of this exposure (10). It can be expected, of course, that the pattern of health effects would follow exposure patterns.
The approach represented by Table 1 has become commonly used in developed countries (see, for example, refs. 6 and 19–21) and, indeed, is suggested as a standard method for application more broadly (22–24) and has been applied globally (25). It has the distinct advantage of being derived from a large number of separate epidemiological studies, lending considerable confidence to the exposure-response relationships. When applied to the much higher indoor pollution levels in rural India, extremely high total ill-health is predicted, as can be seen, for example, in the estimates by Saksena and Dayal (12) in Table 1.
That such exposure-response relationships have been derived for outdoor air pollution in developed-country urban situations, however, raises a number of questions about their suitability for application in developing-country (LDC) populations, particularly those exposed to indoor air pollution in rural areas. The principal differences between developed-country urban and developing-country rural populations are as follows:
- 1.
Differences in the pollutant mix attributable to different fuel sources mean that existing exposure-response estimates may not be applicable in developing countries; i.e., although particulates can be used as indicator of hazard in both cases, biomass fuels as commonly used in Indian households produce relatively more organic compounds (e.g., benzene, formaldehyde, 1,3-butadiene, polyaromatic hydrocarbons), and fossil fuels produce more sulfur oxides. Thus risk estimates derived for the latter fuel may not apply to the former.
- 2.
In a similar fashion, the chemical and other characteristics of the particles produced by biomass combustion are not the same as those produced by fossil fuel use, although of course woodsmoke is found seasonally in the outdoor air of many developed-country cities.
- 3.
Different populations have different exposure patterns; i.e., indoor concentrations tend to vary much more during the day (because of household cooking and heating schedules) than do outdoor urban levels.
- 4.
Exposure levels are also different; i.e., the average exposure levels of concern in households using unvented biomass fuels are 10–50 times greater than the levels studied in most recent urban outdoor studies (1). As is common with toxicants, there may be a diminishing of the effect per unit increase in exposure (shallowing of the exposure-response curve's slope) at these high levels.
- 5.
The patterns of disease, competing risk factors, and age distributions differ dramatically between urban developed-country populations, the world's richest, healthiest, and oldest populations, and people exposed to indoor air pollution in developing countries, who tend to be the poorest, most stressed, and youngest in the world.
- 6.
Most developed-country studies are time-series studies that determine short-term changes in mortality and other endpoints in association with short-term changes in air pollution. Implications for long-term health are unclear (26).
- 7.
The few long-term cohort studies may be confounded by even slight misclassification of smokers, because smoking is such a powerful risk factor for the same health endpoints.
- 8.
Becuase it is not realistic to define zero pollution as the baseline value (the counterfactual level), it is unclear what level is appropriate for calculating attributable risk to air pollution.
- 9.
These more fundamental concerns are in addition to severe constraints imposed by incomplete information on the distribution of air pollution levels experienced by the Indian population. There have been no studies of pollution levels in Indian households based on stratified random sampling designs, for example. (This is also a problem, although to a lesser extent, with outdoor pollution levels in Indian cities.)
- 10.
Additional uncertainty is created because those relatively few particulate measurements done to date have been mostly with respect to total particulates, although most of the consistent exposure-response results have been with regard to smaller size fractions (PM10 or PM2.5; particles less than 10 μm or 2.5 μm in mean aerodynamic diameter, respectively).
- 11.
To be most useful for policy making, such estimates should assess more than mortality but also derive lost life-years and time lost to associated diseases of different severities.
Given these concerns, estimating ill health (mortality) by using this “top-down” approach is a rather crude and uncertain way of predicting the impact of air pollution for the exposures of interest. Given the apparent high total exposure to these populations, however, it has seemed well justified to apply the best available risk information, even if far from ideal.
The “Bottom-Up” Method
Over the last decade or so, however, a number of epidemiological studies of individual diseases for particular age groups have been done in India and other developing countries in solid-fuel-using households. Although not in nearly the quantity or sophistication that are warranted by the size and exposure of the population involved, their number and consistency are sufficient to enable their use for estimating overall health impacts. The following steps summarize the approach taken here:
By using data from the National Census and other sources, the size of the exposed population is determined, which is defined simply as those that use solid fuels.
By using the results of epidemiological studies in biomass-burning households in South Asia, Latin America, SubSaharan Africa, and elsewhere, appropriate risk factors (relative risks) for specific diseases in specific age groups are determined. Such studies are available in sufficient quantity and quality only for adult women and children under 5, who have the highest exposures to stove emissions.
By using the national burden of disease (death and disability) database for India, the current patterns of these diseases in these population groups are determined.
By using the standard procedure for determining the population attributable fraction, the total disease burden attributable to use of household fuels is determined.
By using the known mortality-morbidity relationships for specific diseases for each age group in India, total lost life years and total sick days are estimated.
This approach, although not without weaknesses (see the supplemental data for a discussion), substantially reduces all of the problems noted above for the “top-down” method: 1–4. Being based on studies of biomass-using households, the differences in pollutant mix, particle composition, and exposure patterns and levels are greatly reduced. 5. Although not all done in India, the studies were all done in poor, mostly rural, developing-country populations presumably much more similar to the exposed Indian population than urban developed-country populations. 6. The studies address directly the specific health endpoints over time periods appropriate to the each and thus do not reflect the possible “harvesting” that may be seen in time-series studies. 7. Confining the assessment to women, who have very low smoking rates in India, and children under 5 greatly reduces possible confounding by smoking. 8. Because the epidemiological studies compare actual exposed populations with those using different stoves or fuels, there is no need for an arbitrary baseline. 9–10. Because the epidemiological studies used use binary exposure variables, i.e., exposed or less-exposed, it is not necessary to extrapolate quantitative pollution exposures from incomplete data or to estimate the relative contribution of different size fractions.
11. Use of the coherent Indian National Burden of Disease database allows estimation of lost life-years from deaths and illness as well as number of deaths.
Status of Household Fuel Use in India
The 1991 National Census included for the first time a question about the primary household fuel used and reflected that about 95% of the rural population still relied primarily on biomass fuels (dung, crop residues, and wood). A small fraction uses coal, which means about 97% of households relied principally on these unprocessed solid fuels. Nationwide, some 81% of all households relied on these fuels; 3% used coal and 78% used biomass. An independent probability-weighted national survey of 89,000 households in 1992 derived very similar results (27).
Unfortunately, such fuels are substantially more polluting per meal than the liquid and gaseous fuels further up on the “energy ladder.” The amount of important health-damaging pollutants (e.g., PM10, CO, PAH, HCHO, VOC) breathed by a cook during a typical meal is about 2 orders of magnitude lower when burning bottled gas than burning wood or crop residues (for examples, see refs. 1, 15, 16, 18, and 28). Thus, as a first approximation, the use of unprocessed solid fuels in the household is an indicator of the potential for excessive air pollution exposures. In this way, access to clean fuels is parallel to the often-cited statistic on access to clean water as an indicator of disease risk.
Improved Stoves.
India has active programs promoting introduction of improved biomass cookstoves (ICs) with chimneys and/or combustion improvements (29, 30). These include privately run programs run by nongovernment organizations as well as the large Government of India program itself, conducted by the Ministry of Non-conventional Energy Sources through nongovernment organizations and government agencies. The principal objective of the IC programs is to improve fuel efficiency, although lowering smoke exposures is a secondary goal. Although it has been found to be surprisingly difficult to disseminate ICs successfully over wide regions in India, some important progress has been made. Indeed, some 25–30 million ICs have been introduced since the mid-1980s (31). By 1991–1992, the target year for this study, about 12.5 million had been disseminated. Unfortunately, because most of introduced ICs apparently have lifetimes of 2 years at most, only a fraction of those introduced before 1990 were likely to be still in use in 1992 (32). To be conservative, however, I assume that 7.6 million households (6% of all solid-fuel households; 5% of all households) were using ICs in 1991–1992 that were 100% effective in eliminating air pollution exposures (33, 34). The latter condition is actually rarely the case, however, because even the best ICs leak smoke into the room and some of the smoke released from the flue outdoors will make its way back into the same house or others nearby (16, 35).
Ventilation.
Not all of the remaining households cook indoors at every meal, however. Many cook outdoors or in semienclosed courtyard settings for part of or all of the year. Some may cook indoors for one meal and outdoors for other meals during the same day. There seem to be few systematic surveys that would allow an estimate of the overall scale of this practice. I thus have arbitrarily assumed that 25% of all household meals are cooked outdoors annually throughout the nation. I have also assumed, quite conservatively, that cooking outdoors results in no air pollution exposure. In reality, solid-fuel stoves are sufficiently polluting to produce significant exposure even when used outdoors (36). Thus, the 25% figure could be interpreted to mean that 50–75% of the households cook outdoors part of the year.
In summary, of the approximately 152 million households in 1991–1992, 16% (24 million) did not use solid fuels, 5% (7.6 million) had ICs, and 25% household-equivalents (38 million) cooked outdoors. This leaves about 82 million households at full risk. Thus, about 460 million people were at risk.
Status of Disease in India
Although not consistent in every particular with other estimates of Indian health conditions, the India dataset from the global burden of disease (GBD) studies (37) is used here. Unlike any other available databases, the GBD has the considerable advantages of being coherent and internally consistent, i.e., the deaths and illness for all diseases, broken down by age and sex, add to the known totals in each category. In addition, the criteria used to determine disease categories, cause of death, duration of disease, etc., have been consistently applied across diseases and age groups in all major global regions, thus facilitating comparisons.
The number of deaths is not a very informative indicator of ill health. Better is the loss of healthy life entailed by injury, disease, and premature death. From the GBD, I use the disability-adjusted life-year (DALY), which is one such measure becoming common in international comparisons (37). The DALY basically indicates the amount of healthy life expectancy lost because of a disease or risk factor, including both mortality and morbidity. Shown in supplemental Table 7 is the national burden of disease (NBD) in India as a list of those disease categories causing at least 1% of the NBD or at least 1% of all deaths. Note that the first four categories mostly (87%) affect children younger than 5 years old, who as a result bear the largest overall burden.
Important Air-Pollution-Related Diseases and Their Relative Risks
To determine the portion of the NBD in supplemental Table 7 attributable to indoor air pollution, it would be best to have at hand the results of a wide range of epidemiological studies of specific diseases done in similar solid-fuel-using households around the world using careful clinical confirmation of disease conditions. In addition, to be sure that other factors were not confounding the results, multivariate analyses would have been done to statistically correct for them. In reality, however, the available published studies are less than ideal. Compared with the potential scale of the problem and to the effort spent on air pollution studies in developed countries, they are relatively meager. Some studies have not been able to control for potential confounders, although all have tried to deal with the problem in some way, for example, by matching exposed and unexposed groups. Few studies actually measured air pollution. Most relied on indirect exposure indicators such as type of fuel or stove or number of years cooking. No randomized trials have been done.
Tobacco smoking exacerbates basically the same set of diseases and may overwhelm the impact of air pollution in active smokers. In rural India, however, women probably receive the highest air pollution exposures because of their role as cook but they smoke at low rates (38). Children under 5 years have the highest risks for the acute respiratory disease thought to be affected by air pollution and of course do not smoke. In addition, particularly in the first few years, they spend much time with their mother and thus receive higher exposures than older children, who may spend much time away from the household. Because of these factors, I'm focusing entirely on the effects in women (over 15 years) and children under 5 years. No attempt is made here to calculate the burden on men, which is probably dominated by smoking or on older children (5–15 years) who spend more time out of the household.
To provide some idea of the level of confidence in the disease risk estimates, the evidence is divided into three classes: strong, moderate, and suggestive. Diseases are categorized mainly on the basis of how many studies have been done in LDC solid-fuel-using households. In all cases, there are also other types of evidence from developed-country studies. Although not as directly relevant as the LDC studies themselves, except for the studies of active smokers, the developed-country studies are in conditions with substantially lower pollution levels as measured by particle concentrations.
Class I.
The strong evidence comes from passive and active smoking studies, urban air pollution studies, and multiple studies of solid-fuel use in developing countries.
ARI in children under 5 years (India: 13% of deaths; 11% of NBD; 24% of NBD for children under 5 years).
One of the major diseases thought to be associated with indoor air quality is ARI, a class that includes infections from a wide range of viruses and bacteria, but with similar symptoms and risk factors (28). In every country, young children contract these diseases at similar rates, but in India and other poor countries, they often proceed to severe stages, including pneumonia and death. It is generally acute lower respiratory infections (ALRI) that impose the highest burden and greatest risk of mortality.
As shown in supplemental Table 7, ARI is the largest single disease category for India, accounting for about one-ninth of the national burden. For the world as a whole, ARI is also the largest category, accounting for about 8.5% of the global burden. Astonishingly, Indian ARI is actually the largest single disease category in the world, in the sense of being subject to attention by one government. The Indian portion of this one disease class, which affects mainly one age group, accounts for 2.5% of the entire global burden of ill health.
Since severe childhood ARI is rare in developed countries, few air pollution studies there have focused on it through lack of interest or insufficient cases for statistical significance. Ironically, when developed-country exposure-response information is applied to LDC situations, ARI has often been left out. Recently, more attention has been paid to it, including investigation of the physiological mechanisms (39).
As documented (28), a number of studies have been done in the developing world that give quantitative estimates of the relative risk of severe ARI for children living in biomass-burning households: South Africa (40), Zimbabwe (41), Nigeria (42), Tanzania (43), Gambia (44–47), Brazil (48), India (49), Argentina (50), and Nepal (51). (See the supplemental data for details of these studies.) Although none of these studies had the resources to do the kind of sophisticated analysis commonly found in developed-country studies, as a group they make an intriguing case. A study among Native Americans (Navaho) also showed strong and significant effects or woodstove use at much lower indoor pollution levels than the levels found in developing countries (52, 53). There are even larger groups of studies that show various childhood respiratory symptoms (coughing, wheezing, etc.) to be associated with solid-fuel smoke exposures, but do not provide sufficient evidence to calculate odds ratios (i.e., the risk of contracting disease in the exposed vs. unexposed populations) of ARI itself. [For a review of the ARI and indoor air pollution epidemiology, see Smith et al. (28). For a bibliography of publications related to developing countries, see McCracken and Smith (54).] Some work has been done to identify possible mechanisms in the developing-country context as well (55).
Here I take a range of odds ratios (OR) from 2–3 for the calculations, which account for a range around the average in the published studies of about 2.5. It would be valuable to conduct a full-scale meta-analysis of these studies, but to do so most effectively would require searching for unpublished studies as well as those in the published literature (56). Here, to be conservative, the approach taken is to use only the lower end of the range of reported odds ratios. I apply these odds ratios to ARI only in children younger than 5 years, who account for 85% of ARI in India. Although a substantial proportion of perinatal deaths in India may also actually be attributable to ARI, to be conservative these are left out.
COPD in women (India: 1.5% of deaths; 0.9% of NBD; 1.8% of NBD for women).
Today in developed countries, nearly all cases of COPD are attributable to tobacco smoking. Undoubtedly, smoking is also a significant factor in COPD incidence among LDC men. In India, even though relatively few rural women smoked during the past decades, COPD in rural women today is not uncommon. Although a number of studies have looked at various symptoms of chronic respiratory ill health in women cooking with open biomass stoves, eight seem to have actually determined the prevalence of COPD in a way that allow quantification: Saudi Arabia (57), Columbia (58), Mexico (59), Nepal (60, 61), India (62, 63), Bolivia (64). I use a range of odds ratios from these studies of 2–4 in the calculations (see the supplemental data).
Note that cor pulmonale, a serious heart condition secondary to COPD, is also often found among rural women nonsmokers in India (18) and has long been attributed to chronic biomass smoke exposures (65). There is also good evidence of interstitial lung disease from long-term exposures to biomass smoke, but not of a character that allows determination of odds ratios (66, 67). Even silicosis has been attributed to such exposures, usually in association with soil dust (68, 69). In addition, several studies have found reductions in lung function, cough, and various other respiratory conditions associated with biomass smoke exposures in women. (For further discussions, see the reviews in refs. 18, 70, and 71.) Because there is insufficient quantitative evidence to develop odds ratios and relatively little total disease burden associated with these conditions, they are not included in calculations here.
Lung cancer in women (India: 0.4% of deaths; 0.1% of NBD; 0.1% of NBD for women).
Lung cancer in women is a well demonstrated outcome of cooking with open coal stoves in China (72–77). In China, there is also evidence of lung cancer from use of certain cooking oils (78, 79) and other health effects from arsenic and fluorine in household coal (80). There is little evidence connecting lung cancer to biomass fuel, however. Biomass smoke, however, contains a wide-range of chemicals that are known or suspected human carcinogens, and it contains particles in the small sizes known to penetrate the deep lung (18, 81). More careful studies of the relationship with lung cancer may well be warranted (82). Overall, being mainly nonsmokers and noncoal users, Indian women have low lung cancer rates (83). Only one study, in Japan (84), seems to have found an association of biomass fuel use and lung cancer (OR = 1.8). Therefore, a range of odds ratios is taken from the Chinese coal studies (3–5) but applied only to the relatively small number of coal users in India (3.8%). Like coal use, lung cancer itself is so uncommon in nonsmoking women in India that this calculation has little effect on the overall estimate of ill health from indoor air pollution.
Early studies in Africa seemed to implicate naso-pharyngeal cancer with wood smoke, but this association was not born out by later, more detailed studies in Asia (18, 72). Two studies in Brazil have shown a strong relationship with upper aero-digestive tract cancers, however, with adjusted odds ratios of 2.7 (85) and 2.5 (86). Adding aero-digestive tract cancers would increase the cancer burden attributable to indoor air pollution in India by more than 10-fold, but the total burden would still remain small compared with COPD and ARI. There are 7 times more DALYs associated with mouth and oropharynx cancers than with lung, trachea, and bronchus cancers in Indian women (37). The common practice of chewing pan (a mixture of leaves, spices, betel nut, and tobacco) is usually implicated, however, as the principal risk factor for these oral cancers in India (87, 88).
Class II.
The intermediate evidence is from smoking studies and at least two studies of solid-fuel use in developing countries.
Blindness (cataract) in women (India: ∼0 deaths; 1% of NBD; 2% of NBD for women).
India has a larger burden of blindness than any other major region of the world. Indeed, globally, one out of three cataracts occur in India where they are responsible for 80% of blindness in the country (89). One case-control study in Delhi found an excess cataract risk of about 80% among people using biomass fuel (OR = 1.6; ref. 90). Evaluation of the National Family Health Survey (27) found a somewhat lower rate for partial blindness (OR = 1.3; ref. 91), but no significant difference for total blindness. There is also evidence that environmental tobacco smoke (ETS) exposure is associated with cataracts (92), and animal studies show that cataracts can be caused by woodsmoke (93, 94). I take the values of the two available Indian studies as the range, recognizing that more work is needed. There are also studies linking trachoma with poor air quality in Africa (95), but trachoma causes only about 1% of the burden of cataracts in India (37).
TB in women (India: 8% of deaths; 5% of NBD; 5.5% of NBD for women).
India has a larger fraction of its national burden of disease attributable to TB than any other region, although the actual risk per person is less than that in Sub-Saharan Africa. Analysis of the 1992–1993 National Family Health Survey found a strikingly strong and statistically significant relationship between reported use of biomass fuel and TB in India. Indeed, women over 20 years in biomass-using households were 3.0 times more likely to have someone reporting TB than households using cleaner fuels, even after correction for a range of socioeconomic factors (96). In addition, a recent study in and near Lucknow found a significant odds ratio of 2.5 for clinically confirmed TB in male and female householders using wood or dungcakes (63). A study in China has also found outdoor air pollution to be associated with TB (97). Animal studies show that respiratory immune suppression by woodsmoke (98, 99). Because of the preliminary nature of the available findings, I take the National Family Health Survey value, 3.0, as the high end, and one-quarter of the risk (1.5) as the low end. Given the importance of TB in India, because it is both prevalent and likely to increase with the HIV epidemic, it should be a high priority to follow-up these findings with more detailed studies.
Asthma (India: 0.2% of deaths; 0.5% of NBD).
Asthma rates are officially low in India, although there is some recent evidence that the true prevalence is higher than previously thought (e.g., ref. 100). Associated with urban outdoor pollution (101) and ETS (102), typical solid-fuel indoor smoke exposures are much higher. One of the many difficult aspects of studying asthma is the need to discriminate the type and size of risk factors for becoming asthmatic from those for asthma attacks, a task not done in most studies. Studies in Kenya, Malaysia, and China have quantitatively associated childhood asthma with various measures of indoor pollution from solid-fuel use (103–105). Other, less quantitative studies are reviewed in ref. 71. The range of significant odds ratios in these studies was 1.4–2.5, which has been used here to determine the burden in India. As the reported background rate is so small, however, asthma contributes relatively little to the total burden of deaths or DALYs.
Adverse pregnancy outcomes (India: perinatal conditions are 6% of deaths; 7.5% of NBD; 20% of NBD for children under 5).
A large proportion of perinatal effects consists of diarrhea and ARI, the chief killers of children younger than 5 years, but specific diagnosis/autopsy is difficult with such young infants. Only one study seems to have examined this factor in India as an outcome of biomass fuel use. This study, done in Ahmedabad, found an excess risk of 50% of stillbirth among women using biomass fuels during pregnancy (106). A Chinese study of urban ambient pollution also found a strong relationship of particulate levels with preterm delivery (107). The same group found that particulate air pollution was also associated with low birth weight (108) as was also found with exposure to household biomass smoke in Guatemala (109). Intrauterine mortality, low birth weight, prematurity, and early infant death have been strongly associated with urban outdoor pollution at much lower concentrations than typically found in biomass-using households (110–114). See the short review in ref. 115. ETS exposure to nonsmoking pregnant women has been associated with low birth weight in a meta-analysis of 17 studies (116), with low cognitive development (117), but not with spontaneous abortion (118).
Low birthweight is a risk factor for a number of childhood (119) and, probably, adult (120) diseases, not just those of the respiratory system. Although there is likely to be an important effect from this mechanism for indoor biomass and coal smoke, at present it is hard to provide an estimate of the potential burden in India.
Class III.
The suggestive evidence is from active and passive smoking literature, and urban outdoor air pollution, but there are no studies yet in solid-fuel using households.
Heart disease in women (India: 17% of deaths; 5% of NBD; 7.3% of NBD for women).
Ischemic heart disease (IHD) rates among Indian women are not high by world standards. As with all diseases associated with air pollution, IHD has other important risk factors, smoking and diet in this case being the largest. Indeed, studies in developed-country settings show that the risks of air pollution and smoking for heart disease are relatively modest compared, for example, to the risks for respiratory disease. Because the background rate of heart disease is so high, however, the absolute impact on public health is among the highest.
Although there are many studies of outdoor air pollution (121–123) and ETS (124, 125) unfortunately, there do not appear to be any studies of heart disease in developing countries related to indoor biomass use. Because it is such a potentially significant effect, even if a low risk, however, I apply the information from developed-country (MDC) urban studies to the distribution of exposures to particulates to obtain a range of heart disease risks (1.096–1.42; ref. 22. [Here, an average level of 160 μg/m3 PM10 is used in a linear calculation. Based on estimates in refs. 1 and 10, a higher level might be more accurate, but then the exposure-response relationship may not be linear at these levels, which are much higher than those in the developed-country studies from which the risks were derived. The 160 μg/m3 represents the difference between what people experience and what is represented by a feasible intervention, which of course cannot reduce exposures to zero.]
Estimated Premature Mortality
I use the formula for population attributable risk (126): (PAR) = PP∗(OR − 1)/(PP∗(OR − 1) + 1), where PP is the population prevalence of the exposure condition and OR is the odds ratio. The absolute burden due to the exposure is then determined by: Disease Burden of Exposure = PAR∗NBD, where NDB is the total national burden attributable to the particular disease. Thus, the range of odds ratios noted above has been combined with the estimated exposed percentage and national disease burdens to determine mortality for each disease attributable to use of household solid fuels. The results are shown in Table 2 (see the supplemental data for a sample calculation).
Table 2.
Estimated annual health effects of indoor air pollution exposures in India
| Disease | Deaths, thousands | YLL, millions | DALYs, millions | Sickday severity |
|---|---|---|---|---|
| I. Strong evidence | ||||
| ARI* (880,000) | 270–400 | 9.2–14 | 9.6–14 | 0.28 |
| COPD† (60,000) | 20–35 | 0.19–0.34 | 0.39–0.68 | 0.43 |
| Lung cancer† (6,000) | 0.42–0.79 | 0.0046–0.0086 | 0.0048–0.0090 | 0.15 |
| II. Moderate evidence | ||||
| Blindness† (∼0) | ≈0 | ≈0 | 0.064–0.13 | 0.5 |
| TB† (250,000) | 53–130 | 0.97–2.4 | 1.1–2.6 | 0.15 |
| APO (560,000) | ? | ? | ? | |
| Asthma (20,000) | 3.6–9.0 | 0.046–0.12 | 0.27–0.68 | 0.15 |
| III. Suggestive evidence | ||||
| IHD† (1,100,000) | 54–200 | 0.49–1.8 | 0.55–2.1 | 0.32 |
| Possible total (2,300,000) | 400–780 | 11–18 | 12–20 | |
| Range used§: | 400–550 | 11–16 | 12–17 | |
Estimates listed in order of the strength of evidence under Indian conditions. Mortality and conversion to life years lost and morbidity as in ref. 37. APO, adverse pregnancy outcomes. Severity is taken as the disability weighting in ref. 37 and varies from 0 (healthy) to 0.85 (severe disability). Indian total deaths for each disease are listed in parentheses.
Under 5 years only.
Women only.
Disability-adjusted life year = (years lost to premature death) + (years lost to disability) ∗ (severity factor) (37).
Full range for Class I plus low end of ranges for Classes II and III.
The range of mortality estimates from only those specific diseases for which there are a number of studies (Class I) in Table 2 range from 310,000–470,000. These are at the lower end of those from Table 1 (top-down approach) where general mortality was estimated to be 360,000–1,800,000. This is what might be expected in that the bottom-up estimates were not made of all specific diseases and age groups thought to be associated with air pollution because of lack of appropriate risk information. If the less well verified impacts from Classes II and III are added, however, the top end of the specific disease, at over 790,000, is still substantially less than the high end of the top-down approach, which came from extrapolating exposure-response results from long-term developed-country urban air pollution studies. There is reason to believe that the exposure-response curve for general mortality may flatten out at higher exposure concentrations (127). This provides justification for not accepting the extension of the cohort (chronic) studies to high exposure concentrations, which were the foundation of the high end of the general mortality ranges in Table 1.
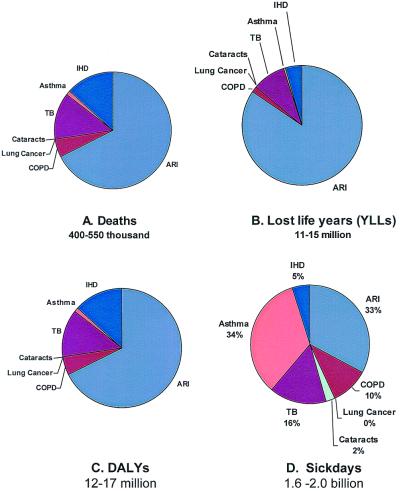
Shown in Table 2 is a “best estimate” of 400,000–550,000 premature deaths annually in India from indoor air pollution exposures to children under five and adult women. This is the range between the low and high estimates from the strong evidence class plus the low estimates from the other evidence classes. No estimate is included for adverse pregnancy outcomes. Fig. 1A shows the distribution of premature deaths by disease.
Figure 1.
Estimated distribution of the annual health burden from indoor air pollution in India in terms of deaths (A), YLL (B), DALYs (C), and sickdays (D).
These estimates may seem shockingly high. It should be noted, however, that they are conservative in comparison with estimates for U.S. cities of close to 60,000 annual deaths from ambient particulates (6, 128). Compared with the Indian solid-fuel-using population, the U.S. urban population is 3 times smaller, experiences average particulate levels 5–20 times lower, and has a lower overall mortality rate (which is the basis of the calculations for such risk factors). A U.K. Department of Health study used a similar approach to estimate 8,100 premature deaths from acute PM10 effects annually for U.K. cities, the population of which is about 50 million (19).
Healthy Life-Years Lost.
By assuming that the age pattern of mortality due to this risk factor is similar to that for each disease as a whole, the NBD in lost healthy life-years (DALYs) can be also be estimated. Based on the distribution in Table 2 and the exposed populations, Fig. 1B illustrates the number of years of lost life (YLL) to death in each category of disease in India. Here the method used for calculating lost life-years is that used in the GBD studies (37). It applies age weighting and discounting such that the maximum difference in life-years lost between the death of a child and an adult is about 37 years. Unweighted and/or undiscounted life-years would favor ARI even more than shown here because it largely affects children under 5. ARI dominates YLL and YLL per capita because of the young age of its victims. Also shown in Table 2 are the total DALYs by disease and disease grouping (YLLs plus life years lost to morbidity). Note the somewhat greater relative importance of TB and COPD compared with the distribution of deaths or YLL because they have more disability associated with them than do IHD and ARI.
Morbidity.
For every death attributable to a particular disease, there are of course many days of disease, both to those who eventually die of the disease and to those who may recover. Days of illness are more important for some kinds of societal impacts than actual mortality. By assuming that the illness associated with this risk factor is similar in duration and severity to that for that illness as a whole, it is possible to estimate morbidity as well. (Disease severities are listed in Table 2.) The distribution of “sick days” and the is shown in Fig. 1C, showing that there are big differences in sickdays per death for the disease categories considered here. Note that COPD, although it did not add much to the total lost life-years, being relatively less common and killing people at relatively old ages, has a much larger impact in sickdays per death: over 8,000 days/death compared with fewer than 2,000 for ARI and IHD. In addition, as indicated in Table 2, the average severity of illness for COPD sickdays (disability weighting) is more than half again that for ARI and a third more than the average IHD sickday.
As a result, the total COPD sickdays in Fig. 1C are a larger proportion of the total from indoor air pollution than are COPD's contribution to death or life-years lost. This effect is even larger for asthma, which contributes about a third of the sickdays, even though accounting for less than 1% of the deaths. The full range of burdens in Table 2 indicates average burdens of illness in lost healthy lost life-days per year for each Indian woman of 3–8 and 30–45 for each child under 5 years.
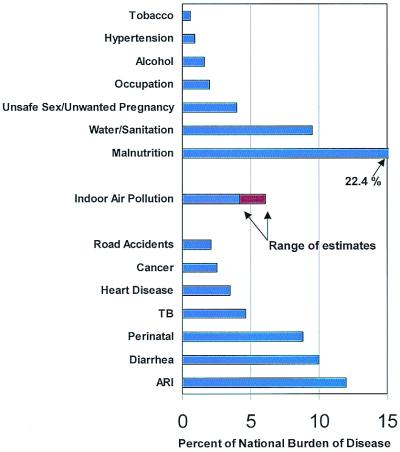
Comparisons with Indian NBD
If verified, the ill health estimated here from indoor air pollution is a substantial portion of the national total in India, 4.2–6.1% (11). It is equivalent to 6.3–9.2% of the burden for women and children under 5, who make up about 44% of the population but bear about two-thirds of the disease burden. As compared with supplemental Table 7, indoor air pollution would seem to classify as a major cause of ill health in India for it rivals or exceeds TB, IHD, all cancers, road accidents, or all of the “tropical” diseases combined. On a risk factor basis, the burden of dirty air at the household level lies behind only dirty water at the household level (poor water/sanitation/hygiene = 10%) and poor food at the household level (malnutrition = 22%), the largest two risk factors in India in the early 1990s. As shown in Fig. 2, it apparently substantially exceeded other major risk factors, such as hypertension, alcohol, unsafe sex, and tobacco. The burdens of the latter two, however, are steadily increasing in India, unlike indoor air pollution. Nevertheless, by any standard, indoor air quality would seem to be a major health issue in the country.
Figure 2.
Estimated burden of disease (DALYs) in India for selected major risk factors and diseases compared with that from indoor air pollution.
Adding urban outdoor pollution, the total would be even greater. Taking the dubious but simple approach of adding the estimates by Saksena and Dayal of the burden from outdoor air pollution in Table 1 using the “top-down” method to those done here in Table 2 for indoor air pollution, total annual deaths would be 600,000–750,000. Assuming a similar mix of morbidity and mortality, the total burden from air pollution in India would be 5.9–9.2% of the total NBD, nearly rivaling poor water/sanitation/hygiene, although still well below malnutrition.
Discussion and Conclusion
At the global level, India seems to have some 30% of all household solid-fuel stoves, although the estimates are generally much less reliable than in India where fuel use is determined in the national census (129). On that basis, the total world health impact on women and children would be roughly three times larger than the Indian estimates. A large fraction undoubtedly occurs in China, where application of broad-brush methods have also derived large health impacts of indoor and outdoor pollution with relatively more COPD and lung cancer and less ARI than found in India (130, 131). To be more precise, would require duplicating the entire process used here of combining exposures, risks, and background disease rates in each country or region.
By themselves, epidemiological studies do not prove causality, only association. Nevertheless, when a number of studies find similar associations in different populations, places, and times; in situations of different mixes of confounders; and done by different investigators with different methods; the argument for causality starts to become stronger. The case for causality is not helped, however, by the current poor understanding of the actual physiological mechanisms that link airborne particles with ill health (132).
The studies in LDC solid-fuel-using households reviewed here have generally not directly measured exposures, nor have they been as nearly as extensive or sophisticated as those in developed-country urban settings. Nevertheless, particularly for the Class I diseases above, a number of studies have been done by different investigators in different countries that found similar results. Combined with the evidence that the average particle levels in such households often reach 1,000–2,000 μg/m3 PM10 (1), their results seem qualitatively consistent with the developed-country studies, which have been done at levels below 150 μg/m3 (23). On the other hand, given that most actually measured the risk of solid fuel use, there may be risks to health in addition to air pollution, perhaps through the physical burden of harvesting such fuels.
The estimates made here should be viewed as tentative. They rely on distressingly few studies and many untested assumptions. Their alarming scale, however, argues for additional efforts to understand and ameliorate the conditions that lead to such severe pollution levels in the village and urban slum homes of India and elsewhere in the Third World. At the very least, they call for a serious effort to conduct the medical and abatement research that would pin down more accurately the impact of the pollution and effective ways to reduce it. Over the next decade, millions of lives may depend on it.
Supplementary Material
Acknowledgments
This work was partly funded by the United Nations Development Program through the Indira Gandhi Institute for Development Research, Mumbai, India.
Abbreviations
- PM10
particles less than 10 microns in diameter
- LDC
less-developed country
- MDC
more-developed country
- IC
improved biomass cookstove
- GBD
global burden of disease
- NBD
national burden of disease
- DALY
disability-adjusted life-year
- ARI
acute respiratory infection
- COPD
chronic obstructive pulmonary disease
- OR
odds ratio
- IHD
ischemic heart disease
- YLL
years of lost life
Footnotes
This contribution is part of the special series of Inaugural Articles by members of the National Academy of Sciences elected on April 29, 1997.
Particles of this range are thought to be better indicators of health risk than measurement of total suspended particles, which include particles of sizes too large to penetrate into the deep respiratory system.
References
- 1.Smith K R. Annu Rev Energy Environ. 1993;18:529–566. [Google Scholar]
- 2.World Health Organization. Air Management Information System (AMIS) Geneva: World Health Organization; 1999. [Google Scholar]
- 3.Holgate S T, Samet J M, Koren H S, Maynard R L, editors. Air Pollution and Health. San Diego: Academic; 1999. [Google Scholar]
- 4.Lippmann M, editor. Environmental Toxicants. New York: Wiley-Interscience; 2000. [Google Scholar]
- 5.Smith, K. R. & Jantunnen, M. (2001) Atmos. Environ. 35, in press.
- 6.Shprentz D S, Bryner G C, Shprentz J S. Breath-taking: Premature Mortality Due to Particulate Air Pollution in 239 American Cities. Washington, DC: Natural Resources Defense Council; 1996. [Google Scholar]
- 7.Smith K R. Workshop on the Energy-Environment Nexus: Indian Issues and Global Impacts. Univ. of Pennsylvania, Philadelphia: Center for the Advanced Study of India; 1994. [Google Scholar]
- 8.Brandon C, Hommann K. The cost of inaction: Valuing the economy-wide cost of environmental degradation in India in Conf. on the Sustainable Future of the Global System. Tokyo: United Nations Univ.; 1995. [Google Scholar]
- 9.Hong C. Global Burden of Disease from Air Pollution. Geneva: World Health Organization; 1995. [Google Scholar]
- 10.World Health Organization. Health and Environment in Sustainable Development. Geneva: World Health Organization; 1997. [Google Scholar]
- 11.Schwela D. Toxicol Lett. 1996;86:131–142. doi: 10.1016/0378-4274(96)03684-3. [DOI] [PubMed] [Google Scholar]
- 12.Saksena S, Dayal V. Energy Environ Monitor. 1997;13:93–102. [Google Scholar]
- 13.Kumar P. Down Earth. 1997;6(12):29–43. [Google Scholar]
- 14.Zhang J, Smith K R, Ma Y, Ye S, Weng X, Jiang F, Qi W, Khalil M A K, Rasmussen R A, Thorneloe A A. Atmos Environ. 2000;34:4537–4549. [Google Scholar]
- 15.Smith K R, Uma R, Kishore V V N, Lata K, Joshi V, Zhang J, Rasmussen R A, Khalil M A K. Greenhouse Gases from Small-Scale Combustion Devices in Developing Countries, EPA-600/R-00-052. Washington, DC: U.S. Environmental Protection Agency; 2000. [Google Scholar]
- 16.Smith K, Apte M, Ma Y, Wongsekiarttirat W, Kulkarni A. Energy. 1994;19:587–600. [Google Scholar]
- 17.U.S. National Research Council. Exposure Assessment. National Academy of Sciences, Washington, DC: National Research Council; 1990. [Google Scholar]
- 18.Smith K R. Biofuels, Air Pollution, and Health: A Global Review. New York: Plenum; 1987. [Google Scholar]
- 19.Holgate S. Quantification of the Effects of Air Pollution on Health in the United Kingdom. London: The Stationery Office; 1998. [Google Scholar]
- 20.Samet J M. In: Air Pollution and Health. Holgate S T, Samet J M, Koren H S, Maynard R L, editors. London: Academic; 1999. [Google Scholar]
- 21.Kunzli N, Kaiser R, Medina S, Studnicka M, Chanel O, Filiger P, Herry M, Horak F, Puybonnieux-Texler V, Quenet P, et al. Lancet. 2000;356:795–801. doi: 10.1016/S0140-6736(00)02653-2. [DOI] [PubMed] [Google Scholar]
- 22.Ostro B D. A Methodology for Estimating Air Pollution Health Effects. Geneva: WHO/EHG/96.5 (World Health Organization; 1996. [Google Scholar]
- 23.World Health Organization. Air Quality Guidelines for Europe. Copenhagen: World Health Organization; 2000. [Google Scholar]
- 24.World Health Organization. Global Air Quality Guidelines. Geneva: World Health Organization; 1999. [Google Scholar]
- 25.Working Group on Public Health and Fossil Fuels. Lancet. 1997;350:1341–1349. [PubMed] [Google Scholar]
- 26.McMichael A J, Anderson H R, Brunekreef B, Cohen A J. Int J Epidemiol. 1998;27:450–453. doi: 10.1093/ije/27.3.450. [DOI] [PubMed] [Google Scholar]
- 27.National Family Health Survey. National Family Health Survey (MCH and Family Planning): India, 1992–93. Bombay: International Institute for Population Sciences; 1995. [PubMed] [Google Scholar]
- 28.Smith K R, Samet J M, Romieu I, Bruce N. Thorax. 2000;55:518–532. doi: 10.1136/thorax.55.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramakrishna J. India Country Report, EWC/World Bank Study Global Review of Improved Stove Programs. Honolulu: East-West Center; 1991. [Google Scholar]
- 30.Kohli S, Ravi M R. Solar Energy Soc India J. 1996;6:101–145. [Google Scholar]
- 31.Ministry of Non-Conventional Energy Sources. Annual Report 1998–99. New Delhi: Ministry of Non-Conventional Energy Sources; 1999. [Google Scholar]
- 32.Natarajan I. Objectives of the National Programme on Improved Cookstoves. New Delhi: National Council of Applied Economic Research; 1999. [Google Scholar]
- 33.Tata Energy Research Institute. Evaluation of Improved Chulha Programme in Tamil Nadu, Rajasthan and West Bengal Report to Ministry of Nonconventional Energy Sources. New Delhi: Tata Energy Research Institute; 1989. [Google Scholar]
- 34.National Council for Applied Economics Research. Evaluation of National Programme on Improved Chulha, Vols. I and II. Delhi: National Council for Applied Economics Research; 1993. [Google Scholar]
- 35.Ramakrishna J, Durgaprasad M B, Smith K R. Environ Int. 1989;15:341–352. [Google Scholar]
- 36.Albalak R, Keeler G, Frisancho A, Haber M. Environ Sci Technol. 1999;33:2505–2509. [Google Scholar]
- 37.Murray C, Lopez A. Global Burden of Disease. Cambridge, MA: Harvard Univ Press; 1996. [Google Scholar]
- 38.World Health Organization. Tobacco or Health: A Global Status Report. Geneva: World Health Organization; 1997. [Google Scholar]
- 39.Becker S, Soukup J M. J Toxicol Environ Health. 1999;57:445–457. doi: 10.1080/009841099157539. [DOI] [PubMed] [Google Scholar]
- 40.Kossove D. S Afr Med J. 1982;61:622–624. [PubMed] [Google Scholar]
- 41.Collings D A, Sithole S D, Martin K S. Trop Doct. 1990;20:151–155. doi: 10.1177/004947559002000403. [DOI] [PubMed] [Google Scholar]
- 42.Johnson A W, Aderele W I. Ann Trop Paediatr. 1992;12:421–432. doi: 10.1080/02724936.1992.11747609. [DOI] [PubMed] [Google Scholar]
- 43.Mtango F D, Neuvians D, Broome C V, Hightower A W, Pio A. Trop Med Parasitol. 1992;43:229–233. [PubMed] [Google Scholar]
- 44.de Francisco A, Morris J, Hall A J, Armstrong-Schellenberg J R, Greenwood B M. Int J Epidemiol. 1993;22:1174–1182. doi: 10.1093/ije/22.6.1174. [DOI] [PubMed] [Google Scholar]
- 45.O'Dempsey T, McArdle T F, Morris J, Lloyd-Evans N, Baldeh I, Lawrence B E, Secka O, Greenwood B M. Int J Epidemiol. 1996;25:885–893. doi: 10.1093/ije/25.4.885. [DOI] [PubMed] [Google Scholar]
- 46.Campbell H, Armstrong J R, Byass P. Lancet. 1989;1:1012. doi: 10.1016/s0140-6736(89)92647-0. [DOI] [PubMed] [Google Scholar]
- 47.Armstrong J R, Campbell H. Int J Epidemiol. 1991;20:424–429. doi: 10.1093/ije/20.2.424. [DOI] [PubMed] [Google Scholar]
- 48.Victora C, Fuchs S, Flores J, Fonseca W, Kirkwood B. Pediatrics. 1994;93:977–985. [PubMed] [Google Scholar]
- 49.Shah N, Ramankutty V, Premila P G, Sathy N. J Trop Pediatr. 1994;40:201–206. doi: 10.1093/tropej/40.4.201. [DOI] [PubMed] [Google Scholar]
- 50.Cerqueiro M C, Murtagh P, Halac A, Avila M, Weissenbacher M. Rev Infect Dis. 1990;12, Suppl. 8:S1021–S1028. doi: 10.1093/clinids/12.supplement_8.s1021. [DOI] [PubMed] [Google Scholar]
- 51.Pandey M R, Boleij J S, Smith K R, Wafula E M. Lancet. 1989;1:427–429. doi: 10.1016/s0140-6736(89)90015-9. [DOI] [PubMed] [Google Scholar]
- 52.Morris K, Morgenlander M, Coulehan J L, Gahagen S, Arena V C, Morganlander M. Am J Dis Child. 1990;144:105–108. doi: 10.1001/archpedi.1990.02150250117047. [DOI] [PubMed] [Google Scholar]
- 53.Robin L F, Less P S, Winget M, Steinhoff M, Mouton L H, Santosham M, Correa A. Pediatr Infect Dis J. 1996;15:859–865. doi: 10.1097/00006454-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 54.McCracken J D, Smith K R. ARI and Indoor Air Pollution: An Annotated Bibliography. U.S. Agency for Int. Dev., Washington, DC: Environ. Health Project; 1997. [Google Scholar]
- 55.Verma B K, Thakur D K. Cent Eur J Public Health. 1995;3:25–29. [PubMed] [Google Scholar]
- 56.Petitti D B. Meta-Analysis, Decision Analysis, and Cost-Effectiveness Analysis: Methods for Quantitative Synthesis in Medicine. New York: Oxford Univ. Press; 2000. [Google Scholar]
- 57.Døssing M, Khan J, al-Rabiah F. Respir Med. 1994;88:519–522. doi: 10.1016/s0954-6111(05)80334-8. [DOI] [PubMed] [Google Scholar]
- 58.Dennis R J, Maldonado D, Norman S, Baena E, Martinez G. Chest. 1996;109:115–119. doi: 10.1378/chest.109.1.115. [DOI] [PubMed] [Google Scholar]
- 59.Perez-Padilla R, Regalado J, Vedal S, Pare P, Chapela R, Sansores R, Selman M. Am J Respir Crit Care Med. 1996;154:701–706. doi: 10.1164/ajrccm.154.3.8810608. [DOI] [PubMed] [Google Scholar]
- 60.Pandey M R. Thorax. 1984;39:337–339. doi: 10.1136/thx.39.5.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pandey M R, Basnyat B, Neupane R P. Chronic Bronchitis and Cor Pulmonale in Nepal. Kathmandu: Mrigendra Medical Trust; 1988. [Google Scholar]
- 62.Malik S K. Indian J Chest Dis Allied Sci. 1985;27:171–174. [PubMed] [Google Scholar]
- 63.Gupta B, Mathur N, Mahendra P, Srivastava A, Swaroop V, Agnihotri M. Energy Environ Monitor. 1997;13:61–67. [Google Scholar]
- 64.Albalak R, Frisancho A R, Keeler G J. Thorax. 1999;54:1004–1008. doi: 10.1136/thx.54.11.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Padmavati S, Pathak S N. Circulation. 1959;20:343–352. doi: 10.1161/01.cir.20.3.343. [DOI] [PubMed] [Google Scholar]
- 66.Dhar S N, Pathania A G S. Semin Respir Med. 1991;12:69–74. [Google Scholar]
- 67.Ramage J, Roggli V, Bell D, Piantadosi C. Am Rev Respir Dis. 1988;137:1229–1232. doi: 10.1164/ajrccm/137.5.1229. [DOI] [PubMed] [Google Scholar]
- 68.Saiyed H N, Sharma Y K, Sadhu H G, Norboo T, Patel P D, Patel T S, Venkaiah K, Kashyap S K. Br J Ind Med. 1991;48:825–829. doi: 10.1136/oem.48.12.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Norboo T, Angchuk P T, Yahya M, Kamat S R, Pooley F D, Corrin B, Kerr I H, Bruce N, Ball K P. Thorax. 1991;46:341–343. doi: 10.1136/thx.46.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen B H, Hong C J, Pandey M R, Smith K R. World Health Stat Q. 1990;43(3):127–138. [PubMed] [Google Scholar]
- 71.Bruce N, Perez-Padilla R, Albalak R. Bull WHO. 2000;78:1078–1092. [PMC free article] [PubMed] [Google Scholar]
- 72.Smith K R, Liu Y. In: The Epidemiology of Lung Cancer. Samet J, editor. New York: Dekker; 1994. pp. 151–184. [Google Scholar]
- 73.Xu Z Y, Brown L, Pan G W, Li G, Feng Y P, Guan D X, Liu T F, Liu L M, Chao R M, Sheng J H, et al. Lung Cancer. 1996;14, Suppl. 1:S149–S160. doi: 10.1016/s0169-5002(96)90220-2. [DOI] [PubMed] [Google Scholar]
- 74.Luo R X, Wu B, Yi Y N, Huang Z W, Lin R T. Lung Cancer. 1996;14, Suppl 1:S113–S119. doi: 10.1016/s0169-5002(96)90217-2. [DOI] [PubMed] [Google Scholar]
- 75.Shen X B, Wang G X, Huang Y Z, Xiang L S, Wang X H. Lung Cancer. 1996;14, Suppl. 1:S107–S112. doi: 10.1016/s0169-5002(96)90216-0. [DOI] [PubMed] [Google Scholar]
- 76.Dai X D, Lin C Y, Sun X W, Shi Y B, Lin Y J. Lung Cancer. 1996;14, Suppl. 1:S85–S91. doi: 10.1016/s0169-5002(96)90213-5. [DOI] [PubMed] [Google Scholar]
- 77.Wang S Y, Hu Y L, Wu Y L, Li X, Chi G B, Chen Y, Dai W S. Lung Cancer. 1996;14, Suppl. 1:S99–S105. doi: 10.1016/s0169-5002(96)90215-9. [DOI] [PubMed] [Google Scholar]
- 78.Zhong L, Goldberg M S, Gao Y T, Jin F. Epidemiology. 1999;10:488–494. [PubMed] [Google Scholar]
- 79.Zhong L, Goldberg M S, Gao Y T, Jin F. Cancer Causes Control. 1999;10:607–616. doi: 10.1023/a:1008962025001. [DOI] [PubMed] [Google Scholar]
- 80.Finkelman R B, Belkin H E, Zheng B. Proc Natl Acad Sci USA. 1999;96:3427–3431. doi: 10.1073/pnas.96.7.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Purvis C R, McCrillis R C, Kariher P H. Environ Sci Technol. 2000;34:1653–1658. [Google Scholar]
- 82.Boffetta P, Jourenkova N, Gustavsson P. Cancer Causes Control. 1997;8:444–472. doi: 10.1023/a:1018465507029. [DOI] [PubMed] [Google Scholar]
- 83.Samet J M. Epidemiology of Lung Cancer. New York: Dekker; 1994. [Google Scholar]
- 84.Sobue T. Int J Epidemiol. 1990;19, Suppl. 1:S62–S66. doi: 10.1093/ije/19.supplement_1.s62. [DOI] [PubMed] [Google Scholar]
- 85.Pintos J, Franco E L, Kowalski L P, Oliveira B V, Curado M P. Int J Epidemiol. 1998;27:936–940. doi: 10.1093/ije/27.6.936. [DOI] [PubMed] [Google Scholar]
- 86.Franco E L, Kowalski L P, Oliveira B V, Curado M P, Pereira R N, Silva M E, Fava A S, Torloni H. Int J Cancer. 1989;43:992–1000. doi: 10.1002/ijc.2910430607. [DOI] [PubMed] [Google Scholar]
- 87.Sankaranarayanan R. Oral Surg Oral Med Oral Pathol. 1990;69:325–330. doi: 10.1016/0030-4220(90)90294-3. [DOI] [PubMed] [Google Scholar]
- 88.Tominaga S. Cancer Lett. 1999;143, Suppl. 1:S19–S23. doi: 10.1016/s0304-3835(99)90005-8. [DOI] [PubMed] [Google Scholar]
- 89.Thylefors B, Negrel A, Pararajasegaram R, Dadzie K. Opthalmic Epidemiol. 1995;2:5–39. doi: 10.3109/09286589509071448. [DOI] [PubMed] [Google Scholar]
- 90.Mohan M, Sperduto R D, Angra S K, et al. Arch Opthalmol. 1989;107:670–676. doi: 10.1001/archopht.1989.01070010688028. [DOI] [PubMed] [Google Scholar]
- 91.Mishra, V. K., Retherford, R. D. & Smith, K. R. (2000) J. Environ. Med. 1 (4), in press.
- 92.West S. J Am Med Assoc. 1992;268:1025–1026. [Google Scholar]
- 93.Shalini V, Lothra M, Srinivas L. Indian J Biochem Biophys. 1994;31:261–266. [PubMed] [Google Scholar]
- 94.Rao C, Qin C, Robison W, Zigler J. Current Eye Res. 1995;14:295–301. doi: 10.3109/02713689509033529. [DOI] [PubMed] [Google Scholar]
- 95.Preuss A, Mariotti S. Bull WHO. 2000;78:258–265. [PMC free article] [PubMed] [Google Scholar]
- 96.Mishra V K, Retherford R D, Smith K R. Int J Infect Dis. 1999;3:119–129. doi: 10.1016/s1201-9712(99)90032-2. [DOI] [PubMed] [Google Scholar]
- 97.Xu Z, Chen B, Kjellstrom T, Xu X, Lin Y, Daqian Y. In: Air Pollution and Its Health Effects in China. Chen B, editor. Geneva: World Health Organization; 1995. pp. 47–88. [Google Scholar]
- 98.Zelikoff J. Center Indoor Air Res Curr. 1994;1(3):3. [Google Scholar]
- 99.Thomas P, Zelikoff J. In: Air Pollution and Health. Holgate S T, Samet J M, Koren H S, Maynard R L, editors. San Diego: Academic; 1999. [Google Scholar]
- 100.Shukla N, Trivedi C R, Moitra J K. Energy Environ Monitor. 1997;13:69–77. [Google Scholar]
- 101.García-Marcos L, Guillén J J, Dinwiddie R, Guillén A, Barbero P. Pediatr Allergy Immunol. 1999;10:96–100. doi: 10.1034/j.1399-3038.1999.00024.x. [DOI] [PubMed] [Google Scholar]
- 102.Strachan D P, Cook D G. Thorax. 1998;53:204–212. doi: 10.1136/thx.53.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mohamed N, Ng'ang'a L, Odhiambo J, Nyamwaya J, Menzies R. Thorax. 1995;50:74–78. doi: 10.1136/thx.50.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Azizi B H, Zulkifli H I, Kasim S. J Asthma. 1995;32:413–418. doi: 10.3109/02770909409077752. [DOI] [PubMed] [Google Scholar]
- 105.Xu X, Niu T, Christiani D C, Weisss S T, Chen C, Zhou Y, Yang J, Fang Z, Jiang Z, Liang W, et al. Int J Occup Environ Health. 1996;2:172–176. doi: 10.1179/oeh.1996.2.3.172. [DOI] [PubMed] [Google Scholar]
- 106.Mavalankar D V, Trivedi C R, Grah R H. Bull WHO. 1991;69:435–442. [PMC free article] [PubMed] [Google Scholar]
- 107.Xu X, Ding H, Wang X. Arch Environ Health. 1995;50:407–415. doi: 10.1080/00039896.1995.9935976. [DOI] [PubMed] [Google Scholar]
- 108.Wang X, Ding H, Ryan L, Xu X. Environ Health Perspect. 1997;105:514–520. doi: 10.1289/ehp.97105514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Boy E, Delgado H, Bruce N G. Birth Weight and Exposure to Kitchen Wood Smoke During Pregnancy. Guatemala: Inst. for Nutrition of Central Am. and Panama; 1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pereira L A, Loomis D, Conceição G M, Braga A L F, Arcas R M, Kishi H S, Singer J M, Böhm G M, Saldiva P H. Environ Health Perspect. 1998;106:325–329. doi: 10.1289/ehp.98106325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bobak M. Environ Health Perspect. 2000;108:173–176. doi: 10.1289/ehp.00108173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ritz B, Yu F. Environ Health Perspect. 1999;107:17–25. doi: 10.1289/ehp.9910717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Loomis D, Castillejos M, Gold D R, McDonnell W, Borja-Aburto V H. Epidemiology. 1999;10:118–123. [PubMed] [Google Scholar]
- 114.Woodruff T J, Grillo J, Schoendorf K G. Environ Health Perspect. 1997;105:608–612. doi: 10.1289/ehp.97105608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Scram R. Environ Health Perspect. 1999;107:A542–A543. doi: 10.1289/ehp.107-1566709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Windham G C, Eaton A, Hopkins B. Paediatric Perinatal Epidemiol. 1999;13:35–57. doi: 10.1046/j.1365-3016.1999.00150.x. [DOI] [PubMed] [Google Scholar]
- 117.Johnson D L, Swank P R, Baldwin C D, McCormick D. Psychol Rep. 1999;84:149–154. doi: 10.2466/pr0.1999.84.1.149. [DOI] [PubMed] [Google Scholar]
- 118.Windham G C, Von Behren J, Waller K, Fenster L. Am J Epidemiol. 1999;149:243–247. doi: 10.1093/oxfordjournals.aje.a009798. [DOI] [PubMed] [Google Scholar]
- 119.Walsh J. In: Disease Control Priorities in Developing Countries. Jamison D, editor. Oxford: Oxford Univ. Press; 1993. [Google Scholar]
- 120.Barker D. Nutrition. 1997;13:807–813. doi: 10.1016/s0899-9007(97)00193-7. [DOI] [PubMed] [Google Scholar]
- 121.Seaton A, Soutar A, Crawford V, Elton R, McNerlan S, Cherrie J, Watt M, Agius R, Stout R. Thorax. 1999;54:1027–1032. doi: 10.1136/thx.54.11.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Borja-Aburto V H, Castillejos M, Gold D R, Bierzwinski S, Loomis D. Environ Health Perspect. 1998;106:849–855. doi: 10.1289/ehp.106-1533229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dockery D W, Pope A C, Xu X, Spengler J D, Ware J H, Fay M E, Ferris B G, Jr, Speizer F E. N Engl J Med. 1993;329:1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- 124.Glantz S A, Parmley W W. J Am Med Assoc. 1995;273:1047–1053. [PubMed] [Google Scholar]
- 125.Steenland K, Sieber K, Etzel R A, Pechacek T, Maurer K. Am J Epidemiol. 1998;147:932–939. doi: 10.1093/oxfordjournals.aje.a009383. [DOI] [PubMed] [Google Scholar]
- 126.Beaglehole R, Bonita R, Kjellstrom T. Basic Epidemiology. Geneva: World Health Organization; 1993. [Google Scholar]
- 127.Schwartz J, Marcus A. Am J Epidemiol. 1990;131:185–194. doi: 10.1093/oxfordjournals.aje.a115473. [DOI] [PubMed] [Google Scholar]
- 128.Hilts, P. J. (July 19, 1993) Studies say soot kills up to 60,000 in US each year, NY Times, p. 1.
- 129.Goldemberg J, Anderson D, Holdren J P, Jefferson M, Jochem E, Khatib H, Nakicenovic N, Popescu A, Reddy A, Rogner H, et al. World Energy Assessment. New York: United Nations Development Programme; 2000. [Google Scholar]
- 130.World Bank. Clear Water, Blue Skies: China's Environment. Washington, DC: World Bank; 1997. [Google Scholar]
- 131.Florig H K. Environ Sci Technol. 1997;31:276A–279A. doi: 10.1021/es972315t. [DOI] [PubMed] [Google Scholar]
- 132.U.S. National Research Council. Research Priorities for Airborne Particulate Matter. Washington, DC: Natl. Acad. Press; 1998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.