Abstract
Objectives:
To determine if loop diuretic use is associated with hip bone loss, and increased risk of falls and fractures in older women.
Design:
Prospective cohort study from August 1992 to April 2004.
Setting:
Four regions in the US from the Study of Osteoporotic Fractures (SOF).
Participants:
Women aged 65 and older (N = 8127) with medication use data who participated in the 4th SOF examination, from which 3 study cohorts were derived.
Measurements:
1) Bone mineral density (BMD) of the total hip assessed by dual-energy x-ray absorptiometry at the 4th and 6th examinations (N = 2980); 2) recurrent (2 or more) falls in the year following the 4th examination (N = 6244); and 3) incident fracture including nonspine (N = 6778) and hip fractures (N = 7272).
Results:
After multivariable-adjustment, loop diuretic users had greater loss of total hip BMD compared to nonusers (mean annualized % BMD −0.87 vs. −0.71, p=0.03) after a mean of 4.4 years (+/− 0.6). The risks of recurrent falls (OR 0.99, 95% CI 0.71 to 1.39), nonspine (RR 1.04, 95% CI 0.90 to 1.21) and hip fracture (RR 1.03, 95% CI 0.81 to 1.31) were not increased among loop diuretic users compared with nonusers.
Conclusion:
In this cohort of older women, loop diuretic use was associated with a small, but significantly higher rate of hip bone loss compared to nonuse after a mean duration of 4.4 years. However the risk of falls or fracture did not differ between the two groups.
Keywords: loop diuretics, osteoporosis, falls, fractures
INTRODUCTION
Loop diuretics are one of the most commonly prescribed medications among older adults. In 2006 alone, Over 36 million prescriptions were written for furosemide, the 8th most commonly prescribed generic medication in the United States 1. It is the third most commonly prescribed medication among community-dwelling women aged 65 years and older, with an estimated 9% prevalence of usage 2. Loop diuretics are commonly prescribed to treat fluid overload conditions (e.g. congestive heart failure) and hypertension.
Loop diuretics increase urinary calcium excretion by inhibiting the Na-K-2Cl co-transporter in the Loop of Henle of the kidney 3. Thus, chronic use of loop diuretics might result in higher rates of bone loss 4. Cross-sectional studies that have examined the association between loop diuretic use and bone density have reported inconsistent results 5, 6. In a recent prospective study of older men, concurrent loop diuretic use was associated with higher rates of hip bone loss 7. In addition, in a small randomized controlled trial, postmenopausal women treated with the loop diuretic, bumetanide, experienced a 2% decrease in total hip BMD compared to placebo 8. To our knowledge, no prior large prospective studies have examined the association between loop diuretic use and rates of change in BMD in older women.
Diuretics are the third most common cause of medication-induced adverse reactions in older community-dwelling adults 9. Loop diuretics can induce hypotension, potentially causing dizziness and falls. Although diuretics as a group have been found to be associated with an increased risk of falling, there is some uncertainty as to whether loop diuretics, in particular, are associated with fall risk 10.
There are conflicting data on whether loop diuretic are associated with an increased risk of hip and other osteoporotic fractures. Some observational studies suggest a positive association 11-14, while others demonstrate no association 15, 16. Furthermore, there is uncertainty as to whether the increased fracture risk with loop diuretic use shown in the former studies were due to the negative effects of loop diuretics on BMD, increased falls risk, or co-morbidities associated with loop diuretic use.
To test the hypotheses that loop diuretic use is associated with a higher rate of hip bone loss and increased risk of falls and fractures, we ascertained loop diuretic use and measured hip BMD in a cohort of older women enrolled in the Study of Osteoporotic Fracture. We followed participants prospectively for changes in loop diuretic use and hip BMD, and risk of incident falls and nonspine fractures.
METHODS
Participants
Study participants were women recruited from the Study of Osteoporotic Fracture (SOF). This study recruited 9704 women aged 65 years and older between September 1986 and October 1988 from 4 regions in the United States: Baltimore County, Maryland; Minneapolis, Minnesota; Portland, Oregon; and the Monongahela Valley, Pennsylvania.17 African American women were excluded due to their low incidence of hip fracture. Women who were unable to walk without assistance and those with a previous history of bilateral hip replacements were also excluded.
Between August 1992 and July 1994, all surviving participants (93% of the original cohort) were invited to return for a 4th examination. A total of 8412 women completed at least the questionnaire portion of the 4th examination. Of these, 8127 provided data on medication use at this examination, of whom 7584 had at least partial data for the 5th examination (December 1994 to December 1996); 6793 had at least partial data for the 6th examination (January 1997 to February 1999); and 4199 had at least partial data for the 8th examination (January 2002 to April 2004). The proportion of survivors from the original cohort at the 5th, 6th, and 8th examinations were 95%, 93% and 75% respectively.
Written informed consent was obtained from all study participants and appropriate institutional review boards were approved for the study.
Bone loss study cohort
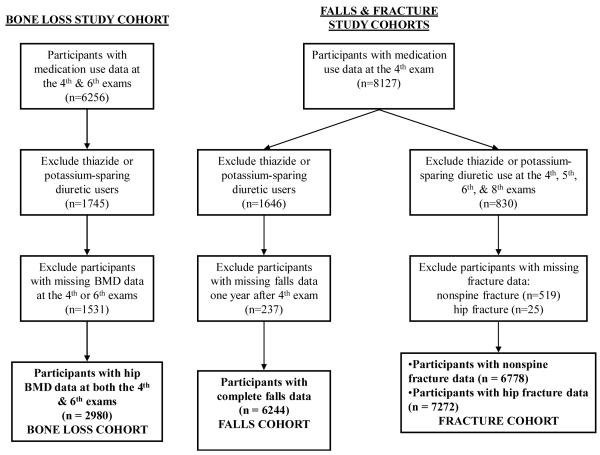
In order to be included in the bone loss cohort, participants must have had medication use data and hip BMD data at both the 4th and 6th examinations. The mean time between examinations was 4.4 +/− 0.6 years (range 2.8 to 6.3 years). Of the 8127 women at the 4th examination, 6256 also had medication use data at the 6th examination (Figure 1). Of these, 1745 were dropped from the analysis due to use of thiazides or potassium sparing diuretics at either examination. These diuretics facilitate the reabsorption of calcium in the convoluted distal tubule segment and may unduly affect our analyses pertaining to loop diuretics. Of the remaining 4511 participants, 2980 had data on hip BMD at both examinations and were included in the bone loss cohort.
FIGURE.
Flow Diagram of Bone Loss, Falls, and Fracture Study Cohorts
Participants were requested to bring all current (any use within the last 2 weeks) prescription and non-prescription medications at the 4th and 6th examinations. Medication usage was then verified by interviewers in the clinic, and a computerized dictionary was used to categorize type of medication from the brand and generic names obtained from the medication containers 18. Loop diuretics included furosemide, ethacrynic acid, bumetanide, and torsemide. Participants were initially categorized into two groups: if they used any loop diuretics at either examination, they were considered as loop diuretic users, and if they had no diuretic use at both examinations they were classified as diuretic nonusers. We subsequently categorized participants into three groups: continuous loop diuretic users, intermittent loop diuretic users, and diuretic nonusers. Continuous loop diuretic users were those who used loop diuretics at both the 4th and 6th examinations. Intermittent users were those who used loop diuretics at either but not both the 4th or 6th examinations; and nonusers were those with use of any loop diuretics at neither the 4th and 6th examinations.
BMD of the total hip and its subregions (femoral neck and trochanter) was assessed by dual-energy x-ray absorptiometry (DXA) with Hologic QDR-1000 scanners (Hologic, Inc., Bedford, MA) at the 4th and 6th examinations. Details of the measurement methods, the precision of the measurements, and densitometry control procedures in this cohort have been published elsewhere.19, 20 The change in bone density was expressed as an annualized percentage of the initial value, as percent change in BMD per year.
Falls study cohort
In order to be included in the analyses examining the association between loop diuretic use and risk of recurrent (2 or more) falls in the subsequent year, participants must have had medication use data for the 4th examination and falls data (collected every 4 months by postcard or telephone interview) for the year following the 4th examination. Of the 8127 women at the 4th examination with medication use data, 1646 were dropped from the analysis because they were using thiazides or potassium sparing diuretics at the 4th examination (Figure 1). Of these 6481 women, 6244 had complete data on recurrent falls and were included in the falls cohort.
A fall was defined as “falling all the way down to the floor or ground, or falling and hitting an object like a chair or stair”. We limited our fall analysis to the 1 year following the 4th examination (3 postcards). Our outcome of interest was recurrent falls, defined as 2 or more falls in the first year after the 4th examination.
Fracture study cohort
The incident fracture analysis required data on medication use at the 4th examination and follow-up data for at least one of the fracture endpoints. All nonspine fractures including hip fractures were verified by radiograph reports. There were 8127 women with medication use data at the 4th examination. Of these, 830 were on a thiazide or potassium sparing diuretic at every examination (4th, 5th, 6th and 8th), and were excluded from the analysis (Figure 1). Of the 7297 with medication-use data that were not on thiazide or potassium sparing diuretics at every examination, 6778 had data on nonspine fracture; and 7272 had hip fracture data. The average duration of follow up was 9.6 +/− 4.3 years for hip fractures and 8.0 +/− 4.7 years for nonspine fractures.
Other measurements
Participants were interviewed at the 4th examination and were asked about self-reported health, medical history, smoking status, alcohol consumption, physical activity, instrumental activities of daily living (IADL), and falls in the past year.
For self-reported health, participants were dichotomized as excellent or good health vs. fair, poor or very poor health. Past medical history reported included whether participants had physician-diagnosed hypertension, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD) or diabetes mellitus. Smokers were dichotomized as current vs. non-smokers. Alcohol consumption was quantified by the number of standard alcoholic drinks consumed weekly over the past 30 days. Physical activity levels were quantified by estimating total kilocalories expended in physical activity per week 21. The number of IADLs the participant had difficulty performing were noted (range 0 to 5) 22, 23. Participants were requested to bring all current prescription and nonprescription medications, including supplements to the clinic examination. Use of estrogen and HMG-CoA reductase inhibitors (statins) was verified using the same criteria utilized for determining use of loop diuretics. Calcium supplement use was ascertained by obtaining information about dose and frequency of multivitamin use, specific vitamin and mineral supplements, and antacids with calcium. Dietary calcium intake was estimated using the validated 60-item block semiquantitative food-frequency questionnaire developed from the Second National Health and Nutrition Survey 24. Total calcium intake (mg/day) was computed by summing the daily dosage of calcium supplements and dietary calcium intake. Use of vitamin D supplements included vitamin D3, vitamin D2, and multivitamins containing vitamin D.
Body weight (kg) was measured by using a balance beam scale at the 4th, 5th, 6th, and 8th examinations. Change in weight (kg) was obtained by calculating the difference in weight between the 4th and 6th examinations.
Statistical analysis
Comparisons between the loop diuretic users and nonusers at the 4th examination were analyzed using t-tests for continuous variables that were normally distributed, Wilcoxon rank sum tests for continuous variables that had skewed distributions, and chi-square tests for categorical variables. After excluding 1646 thiazide and potassium-sparing diuretic users from the 8127 women with medication-use data at the 4th examination, the number of participants included in the comparison cohort was 6481.
For the analysis examining loop diuretic use and rate of change in hip BMD, the adjusted means and 95% confidence intervals (CI) for annualized percent change in BMD were calculated by category of loop diuretic use using the least squares means procedure. After MV adjustment, there was 80% power to detect a difference of 0.2 g/cm2 or greater in mean total hip BMD between the nonuser versus continuous loop diuretic user groups using the three group predictor.
Logistic regression models were used for the analysis examining loop diuretic use and odds of recurrent falls. Cox proportional hazards regression analysis was used to determine the age- and multivariable-adjusted association between loop diuretic use and risk of nonspine fracture, including hip fracture. The use of loop diuretics was coded as a time-dependent variable to allow for crossover and discontinuous use. If medication use data were missing for a given examination, the loop diuretic use data were used from the previous examination. Participants were removed from the analysis for the portion of time they were on thiazide diuretics.
Covariates were selected for use in multivariable-adjusted models for BMD, falls, and fracture analyses if associations were present between a variable and loop diuretic use status (p ≤ 0.10) and between the variable and the specific outcome of interest (p ≤ 0.10). Hip BMD at the 4th examination was forced into the multivariate models assessing the association between loop diuretic use and rate of change in hip BMD.
Additional sensitivity analyses by propensity scoring method were also used to assess the comparability of users and non-users of loop diuretics. Propensity scores were calculated indicating the likelihood of using loop diuretics based on a logistic regression model with covariates that are similar to the multivariate models used in our primary analyses. These propensity scores were then used in place of the covariates in our multivariate models 25.
RESULTS
At the 4th examination, there were a total of 6481 women in the comparison cohort with a mean age of 76.9 years (+/− 5.0), of which 654 (10.1%) used loop diuretics. There were no differences in BMD at the total hip, femoral neck, and trochanter between nonusers of any diuretics and loop diuretic users (TABLE 1). As a group, loop diuretic users were older, less physically active, heavier but also lost more weight from the 4th to 6th examinations, and had poorer self-perceived health compared to nonusers of any diuretics. They also were more likely to report a diagnosis of hypertension, CHF, COPD, diabetes mellitus type 2, and to be taking statin medications. However, participants who did not use diuretics were more likely to be active smokers, consume more alcohol, and have a higher level of calcium intake than loop diuretic users. There was no difference in the use of vitamin D supplements or estrogen between the two groups. Loop diuretic users had a slightly higher level of functional impairment and more frequently reported multiple falls for the year prior to the 4th examination.
Table 1.
Characteristics of 6,481 participants by loop diuretic use at the 4th examination
| Category of loop diuretic use | |||
|---|---|---|---|
| Variable | Nonuser n = 5827 |
User N = 654 |
P-value |
| Total hip BMD, g/cm2, mean (± SD) | 0.730 (0.131) | 0.728 (0.141) | .75 |
| Femoral neck BMD, g/cm2, mean (± SD) |
0.626 (0.114) | 0.628 (0.117) | .77 |
| Trochanter BMD, g/cm2, mean (± SD) |
0.551 (0.105) | 0.542 (0.110) | .14 |
| Age, y, mean (± SD) | 76.6 (4.8) | 79.4 (5.9) | < .001 |
| Alcoholic drinks consumed weekly, mean (± SD) |
1.4 (3.2) | 0.9 (2.9) | < .001 |
| Number of IADL impairments, mean (SD) |
0.6 (1.2) | 1.8 (1.7) | < .001 |
| Total daily calcium intake, mg, mean (± SD) |
1003 (790) | 861 (678) | <.001 |
| Total energy expended per week, kcal, mean (± SD) |
1279 (1454) | 646 (1115) | <.001 |
| Weight, kg, mean (± SD) | 65.3 (12.3) | 68.9 (15.1) | <.001 |
| Weight change v4 to 6, kg, mean (± SD) |
−1.09 (4.89) | −3.09 (6.66) | <.001 |
| Self-rated health, good/excellent vs. fair/poor/very poor (%) |
4703 (80.9) | 415 (63.7) | < .001 |
| Hypertension (%) | 1842 (31.7) | 423 (64.9) | <.001 |
| CHF (%) | 185 (3.2) | 212 (32.5) | <.001 |
| Chronic obstructive pulmonary disease (%) |
564 (9.7) | 128 (19.6) | <.001 |
| Diabetes (%) | 321 (5.5) | 95 (14.6) | <.001 |
| Current estrogen use (%) | 985 (16.9) | 99 (15.1) | .25 |
| Current cigarette smoker (%) | 380 (6.5) | 21 (3.2) | <.001 |
| Current statin use (%) | 207 (3.6) | 39 (6.0) | .002 |
| Current vitamin D supplement use (%) |
2258 (38.8) | 251 (38.4) | .85 |
| 2 or more falls in the past year (%) | 661 (11.4) | 107 (16.4) | <.001 |
BMD = bone mineral density
CHF = congestive heart failure
IADL = instrumental activities of daily living
Effect of loop diuretics on BMD
Of the 2980 women in the bone loss cohort, 358 (12.0%) were loop diuretic users at either the 4th or 6th examinations. After adjustment for age, loop diuretic users experienced greater BMD losses compared to diuretic nonusers at the total hip (mean annualized % BMD −0.94 vs. −0.70, p = 0.001), femoral neck (mean annualized % BMD −0.66 vs. −0.53, p = 0.14), and trochanter (mean annualized % BMD −0.86 vs. −0.66, p = 0.03). After multivariable adjustment (for age, weight, 4th examination site-specific BMD, functional status, alcohol use, total daily calcium intake, physical activity, self reported health status, history of hypertension, CHF and diabetes mellitus type 2, change in weight, smoking status, and use of statin medications), loop diuretic users had greater loss of total hip BMD compared to nonusers (mean annualized % BMD −0.87 vs. −0.71, p=0.03) (TABLE 2). No significant differences were noted at the hip subregions of femoral neck and trochanter.
Table 2.
Comparison of mean annualized % BMD change from baseline between loop diuretic users and nonusers (n=2980)
| Loop diuretic category | ||||
|---|---|---|---|---|
| Nonuser | User | P | ||
| Total hip | Age-adjusted (95% CI) |
−0.70 (−0.75, −0.65) |
−0.94 (−1.08, −0.81) |
.001 |
| Multivariable adjusted (95% CI)† |
−0.71 (−0.76, −0.66) |
−0.87 (−1.01, −0.73) |
.03 | |
| Propensity score method (95% CI) |
−0.71 (−0.76, −0.66) |
−0.88 (−1.03, −0.73) |
.03 | |
| Femoral neck |
Age-adjusted (95% CI) |
−0.53 (−0.59, −0.47) |
−0.66 (−0.82, −0.49) |
.14 |
| Multivariable adjusted (95% CI)† |
−0.53 (−0.59, −0.47) |
−0.62 (−0.79 −0.44) |
.39 | |
| Propensity score method (95% CI) |
−0.53 (−0.60, −0.47) |
−0.62 (−0.80, −0.44) |
.39 | |
| Trochanter | Age-adjusted (95% CI) |
−0.66 (−0.72, −0.59) |
−0.86 (−1.04, −0.69) |
.03 |
| Multivariable adjusted (95% CI)† |
−0.66 (−0.73, −0.60) |
−0.81 (−0.99 −0.62) |
.15 | |
| Propensity score method (95% CI) |
−0.66 (−0.73, −0.60) |
−0.82 (−1.01, −0.63) |
.13 | |
Adjusted for age, baseline weight (kg), baseline site-specific BMD (g/cm2), functional status, alcohol use (drinks/week), total daily calcium intake (mg), physical activity (kcals burned per week), self reported health status, history of hypertension, history of CHF, change in weight (kg), history of diabetes mellitus type 2, smoking status, and use of statins. There were N=82 women who were not included in the multivariate models due to missing covariate data.
When participants were categorized by loop diuretic nonusers (n=2622), intermittent (n=197) and continuous use (n=161) of loop diuretics, nonusers experienced the least decline in BMD compared with intermittent and continuous loop diuretic users (TABLE 3). Intermittent users tended to have greater BMD decreases at the total hip and trochanter compared with continuous users of loop diuretics. However, these differences were not statistically significant (p ≥ 0.08 for all models). Sensitivity analyses using propensity score method showed results consistent with the main analyses, whether participants were grouped by 2 or 3 loop diuretic categories.
Table 3.
Comparison of mean annualized % BMD change from baseline between continuous, intermittent, and non-loop diuretic users (n=2980)
| Loop diuretic group | |||||
|---|---|---|---|---|---|
| Nonuser (n=2622) |
Intermittent (n=197) |
Continuous (n=161) |
P(trend) | ||
| Total hip | Age-adjusted (95% CI) |
−0.70 (−0.75, −0.65) |
−0.98 (−1.16, −0.80) |
−0.90 (−1.10, −0.69) |
.004 |
| Multivariable adjusted (95% CI)† |
−0.71 (−0.76, −0.66) |
−0.93 (−1.11, −0.75) |
−0.79 (−1.00, −0.57) |
.12 | |
| Propensity score method (95% CI) |
−0.71 (−0.76, −0.66) |
−0.93 (−1.12, −0.74) |
−0.80 (−1.03, −0.56) |
.11 | |
| Femoral neck |
Age-adjusted (95% CI) |
−0.53 (−0.59, −0.47) |
−0.58 (−0.80, −0.36) |
−0.76 (−1.00, −0.51) |
.08 |
| Multivariable adjusted (95% CI)† |
−0.53 (−0.59, −0.47) |
−0.58 (−0.81, −0.36) |
−0.67 (−0.93, −0.40) |
.32 | |
| Propensity score method (95% CI) |
−0.53 (−0.59, −0.47) |
−0.57 (−0.80, −0.34) |
−0.68 (−0.95, −0.41) |
.31 | |
| Trochanter | Age-adjusted (95% CI) |
−0.66 (−0.72, −0.59) |
−0.93 (−1.16, −0.70) |
−0.78 (−1.04, −0.52) |
.08 |
| Multivariable adjusted (95% CI)† |
−0.66 (−0.73, −0.60) |
−0.88 (−1.12 −0.65) |
−0.70 (−0.98, −0.43) |
.33 | |
| Propensity score method (95% CI) |
−0.66 (−0.73, −0.60) |
−0.88 (−1.12 −0.64) |
−0.72 (−1.01, −0.43) |
.30 | |
Adjusted for age, baseline weight (kg), baseline site-specific BMD (g/cm2), functional status, alcohol use (drinks/week), total daily calcium intake (mg), physical activity (kcals burned per week), self reported health status, history of hypertension, history of CHF, change in weight (kg), history of diabetes mellitus type 2, smoking status, and use of statins. There were N=82 women who were not included in the multivariate models due to missing covariate data.
Of the 197 intermittent loop diuretic users, 35 and 162 used loop diuretics at the 4th and 6th examinations respectively. Baseline characteristics were similar among intermittent loop diuretic users except that CHF was more prevalent among users at the 4th compared to the 6th examinations (26% vs. 8%, p = 0.006). There were no significant differences in the rates of bone loss at the total hip, femoral neck, and trochanter between intermittent user groups (data not shown).
Effect of loop diuretics on fall and fracture risk
There were 621 loop diuretic users and 5623 nonusers within the falls study cohort (n=6244). A total of 718 women (11.5%) had 2 or more falls during the first year of follow-up. Loop diuretic users experienced more falls than nonusers during the first year of follow-up (16.3% vs. 11.0%, p < 0.001). The age-adjusted risk of recurrent (2 or more) falls was greater among loop diuretic users vs. non-users (OR 1.33, 95% CI 1.05 to 1.69), but after adjustment for potential confounders (age, weight, self-rated health, history of hypertension, CHF, COPD, diabetes mellitus type 2, IADL impairments, alcohol consumption, smoking status, use of statin medications, calcium intake, and physical activity), no increased fall risk was noted (OR 0.93, 95% CI 0.67 to 1.28). When results were further adjusted for history of multiple falls in the year prior to the 4th examination, results were similar (OR 0.99, 95% CI 0.71 to 1.39). Sensitivity analysis by propensity method also revealed similar results (OR 1.01, 95% CI 0.72 to 1.40). We observed that self-rated health, CHF, diabetes, IADL impairment, previous recurrent falls, and calcium intake explained the association between loop diuretic use and fall risk.
Within the incident fracture analysis cohort (n=7297), 2521 had nonspine fractures (37 per 1000 person-years) and 897 sustained hip fractures (12 per 1000 person-years). In both age- and multivariable-adjusted analyses, compared with diuretic nonusers, loop diuretic users were not at increased risk of nonspine or hip fracture (TABLE 4).
Table 4.
Relative Risk of Fracture Among Loop Diuretic Users vs. Nonusers
| RR†† | ||
|---|---|---|
| Nonspine | ||
| Any | Age-adjusted (95% CI) | 1.11 (0.98, 1.26) |
| Multivariable adjusted (95% CI)† |
1.04 (0.90, 1.21) | |
| Propensity score method (95% CI) | 1.00 (0.86, 1.17) | |
| Hip | ||
| Any | Age-adjusted (95% CI) | 1.03 (0.84, 1.26) |
| Multivariable adjusted (95% CI)† |
1.03 (0.81, 1.31) |
|
| Propensity score method (95% CI) | 0.98 (0.77, 1.25) |
Adjusted for age, time-dependent weight (kg), functional status, total daily calcium intake (mg), physical activity (kcals burned per week), self reported health status, history of CHF, history of COPD, history of diabetes mellitus type 2, smoking status, and history of 2 or more falls in the year prior to baseline.
reference is nonuser
DISCUSSION
We found, in a cohort of older women, that loop diuretic users experienced more than a 20% relative increase in annualized rate of total hip bone loss compared to diuretic nonusers. However, similar differences were not found within the individual subregions of femoral neck and trochanter. We also did not find any significant differences in the rate of bone loss between intermittent and continuous loop diuretic users.
Previous observational studies have reported inconsistent results between loop diuretics and bone mass5, 6. One cross-sectional study involving 1,405 people (55% women) aged 55 years and older found no association between loop diuretics and calcaneal ultrasound measurements after adjustment for age and BMI 6. However, major limitations of that study were its cross-sectional design and the poor correlation between calcaneal ultrasound measurements and hip BMD (r = 0.34 to 0.43), making calcaneal ultrasounds poorly predictive for low BMD. Another cross-sectional study involved BMD measurements by DXA in 348 women above the age of 70 5. In that study, users of loop diuretics (n = 41) had a significantly lower BMD (5%) at the femoral neck and trochanter compared to nonusers after adjustments for age, years since menopause, and body weight. Again, a limitation of these cross-sectional data is the introduction of potential biases that could have substantially under- or overestimated any association between loop diuretic use and BMD.
A randomized control trial involving 87 postmenopausal women examined the effect of a potent loop diuretic on BMD. After treatment for a year, women who received bumetanide (n = 46) experienced a significant 2% larger decline in total hip BMD compared to those who received placebo8. Mean serum parathyroid hormone (PTH) was increased in the bumetanide group and decreased in the placebo at the end of the study period. Bone resorption and formation markers were higher in the bumetanide group compared to placebo. There also were differences in the diurnal variation of urinary calcium and plasma PTH between the 2 groups, characterized by increases in urinary calcium excretion and plasma PTH levels in the first 4-6 hours following the administration of bumetanide. The 24-hour urinary calcium excretion was greater among women receiving bumetanide versus placebo. These observations suggest that the decrease in bone density seen in loop diuretic users may be partly explained by increased urinary calcium excretion and a PTH-driven imbalance in bone turnover induced by loop diuretics.
An analysis using data from the Osteoporotic Fractures in Men (MrOS) Study involved 3269 male participants (average age = 73 years) who were followed for an average of 4.6 years, of which 181 and 84 were intermittent and continuous loop diuretic users, respectively 7. The mean annualized change in total hip BMD was −0.33%, −0.58% and −0.78% for nonusers, intermittent and continuous users of loop diuretics, respectively, after multivariable adjustment. Similar results were seen at the femoral neck and trochanter. Although BMD loss was greater within intermittent and continuous users when each were compared to nonusers, there were no significant difference in loss of BMD between the intermittent and continuous loop diuretic groups at the 2 hip subregions. Unlike the MrOS Study, we found no evidence that total hip, femoral neck or trochanter BMD differed between the 3 loop diuretic use categories after adjustment for multiple potential confounders. Neither was there a trend toward greater bone loss with continuous over intermittent loop diuretic use in the current study. The magnitude of the effect of loop diuretic on BMD loss was smaller in our current study compared to in the MrOS study. We determined that intermittent loop diuretic users in our study population were generally similar in terms of characteristics and rates of bone loss, and the lack of power to detect a significant difference between the 3 groups remains as a plausible explanation. Participants in the MrOS and our study cohort were quite similar with respect to both baseline characteristics and the number of participants in each group. However, our study participants were slightly older (mean age 76.9 years) compared to the MrOS cohort (mean age 72.7 years), and loop diuretic users in our study consumed less calcium than nonusers of diuretics.
The fall rate of 11 to 16.3% observed in our study is similar to that of older women residing in the US 26. However, the observed aged-adjusted increased risk of falls among loop diuretic users in our study was no greater than that for nonusers of diuretics after adjustment for multiple confounders, suggesting that the age-adjusted finding of increased fall risk was accounted for by co-morbidities and other factors associated with loop diuretic use. A meta-analysis showed that diuretic use in older adults resulted in a slightly increased risk of falls (OR 1.08, 1.02 – 1.16) 10. However, when diuretics were examined specifically by class, the risk of falls was not significantly increased with thiazide (OR 1.06, 0.97 – 1.16) or loop diuretics (OR 0.90, 0.73 – 1.12).
Our observed hip fracture rates were fairly consistent with that of the national trend for women 27. However, we did not observe an increased risk of nonspine or hip fracture associated with loop diuretic usage in our study. Previous observational studies have shown conflicting results on fracture outcomes, with some studies showing a positive association 11-14, while other studies demonstrated no association between loop diuretics and fracture risk 15, 16. All but one study were case-control studies. Although case control studies are helpful for assessing rare outcomes such as fracture in small samples of participants, they are limited by confounder selection and information biases that can result in misclassification of exposure variables. In addition, they do not directly measure risk. The only prospective study included 348 older women who were followed for about 5 years 14. In that study, loop diuretic use was associated with a 2-fold increased risk of osteoporotic fracture (RR = 2.1, 1.0 – 4.7). While neither risk for nonvertebral (RR = 1.3, 0.6 – 2.7) or hip fracture (RR=2.2, 0.7 – 6.7) was significantly increased, the small sample size and these large confidence intervals suggest that the study had low power to detect an association of increased fracture risk.
A recent meta-analysis performed on both case-control and prospective observational studies showed that loop diuretic use was associated with a modestly increased risk of fracture that did not reach statistical significance (RR 1.43, 0.99 – 2.07) 28. Drawbacks of the meta-analysis included moderate to large heterogeneity in the pooled studies and that only 2 of the studies, which were case-control, were deemed high quality studies 11, 16.
Strengths of our study include its cohort design and large sample size. It is one of the few studies examining the association of loop diuretic use on BMD, falls and fracture in women. Our study cohort had a comparable BMD and pattern of loop diuretic usage similar to that of ambulatory older women in the US 2, 29. Diuretic use was verified by visual confirmation by trained personnel and categorized with a computerized dictionary, minimizing the potential for misclassification arising from self-report. BMD measurements were obtained at the hip with high precision using DXA, which is widely used in clinical practice. Our models examining the outcome of BMD change, falls and fracture included adjustments for multiple potential confounders. We performed additional sensitivity analyses using propensity scoring method to assess the comparability of users and non-users of loop diuretics. Although use of the propensity score methodology typically gives similar results compared with the traditional methods of multivariable regression, one benefit is that construction of the propensity model may be useful in revealing whether the loop diuretic groups are really exchangeable for observed confounders (that is, if loop diuretic users were from a very different population of people compared to non-loop diuretic users). It also helps to insure that traditional regression methods are not merely extrapolating results beyond the boundaries of the observed variables, which may lead to bias estimates of the “treatment effect”. Our results were similar for both the primary and sensitivity analyses, affirming the validity of our results.
Even though rigorous methods of analyses were employed in our present study, the conclusions that can be drawn from this and all observational studies are limited by variables that are not observed or measured, such as vitamin D levels and the precise indication or contraindication for the use of the loop diuretics. We also were unable to determine a dose-dependent relationship with loop diuretic use because information on loop diuretic dose was lacking. It also is possible that unmeasured changes in loop diuretic use may have occurred between examinations, but that would tend to bias the estimates of the “loop diuretic use” and “BMD change” association toward the null hypothesis. Although the baseline characteristics of intermittent loop diuretic users were generally similar, CHF diagnoses were more prevalent at the 4th versus the 6th examination (26% vs. 8%, p = 0.006). However, loop diuretic usage was more common at the latter examination. While it is possible that physicians may have initiated loop diuretics in participants experiencing worsening heart failure, our study lacked the indication for starting and stopping loop diuretic use, and we were not able to fully explore this issue. Finally, our study involved white older women who were relatively healthy, and therefore may not be representative of loop diuretic users. However, the results of our current study, when considered together with our recent study examining the association of loop diuretic use and hip BMD in older community-dwelling men, suggest that loop diuretics do exert detrimental effects on hip bone density, but are not sufficient to increase the risk of fracture in older women.
CONCLUSION
After adjustment for multiple potential confounders, loop diuretic users appear to have a higher rate of hip bone loss compared with nonusers in this cohort of older women. The effect appears on average to be small, and there was no evidence that rate of bone loss was higher among continuous as compared with intermittent users. Loop diuretic use in older women was not associated with an increased risk of falls or nonspine fractures, including hip fractures within the time frame of this study.
ELF.
ACKNOWLEDGMENTS
The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, and 2 R01 AG027574-22A1.
Sponsor's Role: The sponsors had no direct role in the conduct of the study; the collection, management, analyses, or interpretation of the data; or the preparation or approval of the manuscript.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Lionel Lim: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript.
Howard Fink: study concept and design, analysis and interpretation of data, and critical review of manuscript.
Terri Blackwell: Analysis and interpretation of data, preparation of the manuscript.
Brent Taylor: analysis and interpretation of data, and critical review of manuscript.
Kristine Ensrud: study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and critical review of manuscript
REFERENCES
- 1.Anonymous Top 200 generic drugs by units in 2006. 2007 (Accessed at http://www.drugtopics.com/drugtopics/data/articlestandard//drugtopics/092007/407652/article.pdf.)
- 2.Kaufman DW, Kelly JP, Rosenberg L, et al. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287:337–344. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 3.Rose BD. Diuretics. Kidney Int. 1991;39:336–352. doi: 10.1038/ki.1991.43. [DOI] [PubMed] [Google Scholar]
- 4.Rejnmark L, Vestergaard P, Pedersen AR, et al. Dose-effect relations of loop- and thiazide-diuretics on calcium homeostasis: A randomized, double-blinded Latin-square multiple cross-over study in postmenopausal osteopenic women. Eur J Clin Invest. 2003;33:41–50. doi: 10.1046/j.1365-2362.2003.01103.x. [DOI] [PubMed] [Google Scholar]
- 5.Ooms ME, Lips P, Van Lingen A, et al. Determinants of bone mineral density and risk factors for osteoporosis in healthy elderly women. J Bone Miner Res. 1993;8:669–675. doi: 10.1002/jbmr.5650080604. [DOI] [PubMed] [Google Scholar]
- 6.van Daele PL, Burger H, Algra D, et al. Age-associated changes in ultrasound measurements of the calcaneus in men and women: the Rotterdam Study. J Bone Miner Res. 1994;9:1751–1757. doi: 10.1002/jbmr.5650091112. [DOI] [PubMed] [Google Scholar]
- 7.Lim LS, Fink HA, Kuskowski MA, et al. Loop diuretic use and increased rates of hip bone loss in older men: The Osteoporotic Fractures in Men Study. Arch Intern Med. 2008;168:735–740. doi: 10.1001/archinte.168.7.735. [DOI] [PubMed] [Google Scholar]
- 8.Rejnmark L, Vestergaard P, Heickendorff L, et al. Loop diuretics increase bone turnover and decrease BMD in osteopenic postmenopausal women: results from a randomized controlled study with bumetanide. J Bone Miner Res. 2006;21:163–170. doi: 10.1359/JBMR.051003. [DOI] [PubMed] [Google Scholar]
- 9.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- 10.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: A systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc. 1999;47:40–50. doi: 10.1111/j.1532-5415.1999.tb01899.x. [DOI] [PubMed] [Google Scholar]
- 11.Heidrich FE, Stergachis A, Gross KM. Diuretic drug use and the risk for hip fracture. Ann Intern Med. 1991;115:1–6. doi: 10.7326/0003-4819-115-1-1. [DOI] [PubMed] [Google Scholar]
- 12.Rejnmark L, Vestergaard P, Mosekilde L. Fracture risk in patients treated with loop diuretics. J Intern Med. 2006;259:117–124. doi: 10.1111/j.1365-2796.2005.01585.x. [DOI] [PubMed] [Google Scholar]
- 13.Taggart HM. Do drugs affect the risk of hip fracture in elderly women? J Am Geriatr Soc. 1988;36:1006–1010. doi: 10.1111/j.1532-5415.1988.tb04367.x. [DOI] [PubMed] [Google Scholar]
- 14.Tromp AM, Ooms ME, Popp-Snijders C, et al. Predictors of fractures in elderly women. Osteoporos Int. 2000;11:134–140. doi: 10.1007/PL00004174. [DOI] [PubMed] [Google Scholar]
- 15.Cumming RG, Klineberg RJ. Psychotropics, thiazide diuretics and hip fractures in the elderly. Med J Aust. 1993;158:414–417. doi: 10.5694/j.1326-5377.1993.tb121839.x. [DOI] [PubMed] [Google Scholar]
- 16.Rashiq S, Logan RF. Role of drugs in fractures of the femoral neck. Br Med J (Clin Res Ed) 1986;292:861–863. doi: 10.1136/bmj.292.6524.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990;263:665–668. [PubMed] [Google Scholar]
- 18.Pahor M, Chrischilles EA, Guralnik JM, et al. Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol. 1994;10:405–411. doi: 10.1007/BF01719664. [DOI] [PubMed] [Google Scholar]
- 19.Ensrud KE, Palermo L, Black DM, et al. Hip and calcaneal bone loss increase with advancing age: Longitudinal results from the study of osteoporotic fractures. J Bone Miner Res. 1995;10:1778–1787. doi: 10.1002/jbmr.5650101122. [DOI] [PubMed] [Google Scholar]
- 20.Steiger P, Cummings SR, Black DM, et al. Age-related decrements in bone mineral density in women over 65. J Bone Miner Res. 1992;7:625–632. doi: 10.1002/jbmr.5650070606. [DOI] [PubMed] [Google Scholar]
- 21.Paffenbarger RS, Jr., Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 22.Fitti JE, Kovar MG. The Supplement on Aging to the 1984 National Health Interview Survey. Vital Health Stat 1. 1987:1–115. [PubMed] [Google Scholar]
- 23.Pincus T, Summey JA, Soraci SA, Jr., et al. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum. 1983;26:1346–1353. doi: 10.1002/art.1780261107. [DOI] [PubMed] [Google Scholar]
- 24.Cummings SR, Block G, McHenry K, et al. Evaluation of two food frequency methods of measuring dietary calcium intake. Am J Epidemiol. 1987;126:796–802. doi: 10.1093/oxfordjournals.aje.a114716. [DOI] [PubMed] [Google Scholar]
- 25.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127(8 Pt 2):757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention Self-reported falls and fall-related injuries among persons aged > or =65 years--United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:225–229. [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Trends in Health and Aging. 2008 (Accessed October, 2008, at http://www.cdc.gov/nchs/agingact.htm.)
- 28.Wiens M, Etminan M, Gill SS, et al. Effects of antihypertensive drug treatments on fracture outcomes: A meta-analysis of observational studies. J Intern Med. 2006;260:350–362. doi: 10.1111/j.1365-2796.2006.01695.x. [DOI] [PubMed] [Google Scholar]
- 29.Looker AC, Wahner HW, Dunn WL, et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8:468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]