Abstract
We attempted to describe, in a series of clear cell Renal Cell Carcinoma (RCC), the relationship between CAIX expression, VHL gene mutations, tumor characteristics and outcome. Radical nephrectomy was performed in 100 patients. Genomic DNA was extracted from frozen tumor samples. Four amplimers covering the whole coding sequence of the VHL gene were synthesized by PCR and sequenced. The monoclonal antibody M75 was used to score the expression of the CAIX protein immunohistochemically. VHL mutations were identified in 58 patients (58%) and high CAIX expression (>85%) was observed in 78 (78%). Tumors with VHL mutation showed higher CAIX expression than those without (p=0.02). Low CAIX expression and absence of VHL mutation were associated with a more advanced tumors e.g. higher T stages and presence of metastases. VHL mutation and high CAIX expression predicted longer progression-free survival (p=0.037) and disease-specific survival (p=0.001), respectively. In combination, they defined three prognostic groups (p=0.002): (1) good prognosis, defined as VHL mutation and high CAIX (2-year survival:86%), (2) intermediate prognosis with either VHL mutation or high CAIX (69%), and (3) poor prognosis with no VHL mutation and low CAIX (45%, median survival 18 months). CAIX expression, but not VHL mutational status, was an independent prognostic factor in multivariate analysis. Taken together, CAIX expression and VHL mutational status are able to stratify patients with clear cell RCC into distinct groups with regards to clinicopathological variables and prognosis, with low CAIX expression and absence of VHL mutation being associated with a poor clinicopathological phenotype and diminished survival.
Keywords: RenalCell Carcinoma, VHL, CAIX, Prognosis, Survival
Keywords: Aged; Antigens, Neoplasm; metabolism; Carbonic Anhydrases; metabolism; Carcinoma, Renal Cell; genetics; mortality; pathology; Down-Regulation; Female; Gene Expression Regulation, Enzymologic; Gene Expression Regulation, Neoplastic; Humans; Kidney Neoplasms; genetics; mortality; pathology; Male; Middle Aged; Multivariate Analysis; Mutation; Neoplasm Staging; Proportional Hazards Models; Survival Analysis; Von Hippel-Lindau Tumor Suppressor Protein; genetics
INTRODUCTION
Renal cell carcinoma (RCC) accounts for 3% of all solid tumors and is the sixth leading cause of cancer related deaths due to the lack of curative therapy for locally advanced or metastatic disease (1). About 80% of RCCs are clear cell carcinomas, which are highly vascularized tumors that over-express a number of growth factors, including vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF). Recently, significant progress has been made in the medical treatment of metastatic RCC (mRCC) by targeting tumor angiogenesis through VEGF-R and PDGF-R using receptor tyrosine kinase inhibitors. Both in first and second line therapy, progression-free survival has been improved in metastatic disease compared to standard treatment options (2;3).
The vascular phenotype of clear cell RCC is generally believed to be in large part due to VHL gene inactivation. The VHL gene is located to chromosome 3p25 and has been characterized as a tumor suppressor gene whose loss leads to familial RCC in affected families (4;5). Interestingly, in a high percentage of sporadic clear cell RCCs, one copy of the VHL gene is inactivated by mutation or by promoter hypermethylation while the other copy is lost by deletion, consistent with Knudson’s “two-hit” hypothesis (6–8). The VHL gene encodes a protein (pVHL) of 213 amino acid residues which is the substrate recognition component of a ubiquitin ligase complex that targets a protein transcription factor, hypoxia-inducible factor (HIF), for proteolysis (9–11). Under hypoxic conditions as well as in case of VHL gene inactivation, the pVHL elonginC/B-Cul2 complex does not degrade HIF-1α, which is stabilized and accumulates in the nucleus leading to subsequent over-expression of genes which are critical for tumor angiogenesis (VEGF), glucose transport (GLUT1, GLUT3), glycolysis, pH control (CAIX, CAXII), epithelial proliferation (PDGF, TGF-α), cell migration and homing (CXCR4) (12).
Conflicting results have been published regarding the relationship between VHL alterations and RCC tumor aggressiveness or survival. Several studies have suggested that VHL inactivation was associated with advanced disease whereas others found no association with usual prognostic parameters (13;14). Similarly, several authors failed to demonstrate any relationship between VHL inactivation and survival while others suggested that VHL genetic alterations were associated with a favorable outcome (15;16).
CAIX is a downstream gene activated following hypoxia and/or VHL inactivation (17;18). CAIX is over-expressed in a wide variety of cancers in relation to hypoxic conditions and its over-expression is invariably associated with tumor aggressiveness and poor outcome (19–24). CAIX has also been investigated in RCC and it turns out that it is a strong predictor for response to immunotherapy and an independent prognostic parameter in mRCC as well. However in RCC CAIX over-expression is associated with a good outcome by contrast to other malignancies (25;26).
Therefore, the objective of our study was to clarify the relationship between VHL mutations and CAIX expression in a series of localized and mRCCs and to evaluate the prognostic value, either alone or in combination.
MATERIALS AND METHODS
Patient Selection and Tumor Classification
The study cohort consisted of 100 patients treated by nephrectomy for sporadic RCC at Rennes University (France) and the David Geffen School of Medicine at UCLA Department of Urology (Los Angeles, USA). The study protocol was approved by institutional review boards at each institution. Age, gender, T, N, and M classification (27), ECOG performance status (28), pathologically defined tumor size, Fuhrman grade (29) and RCC-specific survival (RCC-SS) were collected for each case.
Histological Analysis, Tissue Sample Procurement and DNA Extraction
Formalin-fixed paraffin sections were stained with hematoxylin and eosin for light microscopy. The slides were reviewed by one dedicated genito-urinary pathologist at each institution (N.R.L. and J.W.S.). Clear cell carcinomas only were considered for analysis. Immediately after macroscopic examination of the nephrectomy specimen, small samples including normal and malignant tissue were obtained. Specimens were frozen in liquid nitrogen and stored at −80°C until DNA extraction. Genomic DNA was extracted from 25 to 35 mg of frozen tissue sections using QIAamp DNA minikit (Qiagen, Courtaboeuf, France). DNA quantity and quality were estimated by optical density (OD 260/280) measurement and 0.8% agarose gel electrophoresis using standard protocols.
CAIX Immunostaining
The mouse monoclonal antibody M75 (a gift from Dr. Eric Stanbridge, University of California at Irvine, Irvine, CA, United States) used to detect the CAIX protein has been described previously (30;31). Immunohistochemical staining of tissue sections with anti-CAIX antibody was done using a peroxidase technique with antigen retrieval using heat treatment, as previously described using the Dako staining systems (Dako Corporation, Carpenteria, CA; (Ref. (31)). The CAIX primary antibody was used at a 1:10,000 dilution. Semiquantitative assessment of the antibody staining was performed by a single pathologist blinded to the clinicopathological variables and the VHL analysis as well. The extent of staining was recorded as a percentage of the target tissue sample that had positive CAIX expression.
VHL Gene Mutational Analysis
Four primers pairs were designed (Primer3 software, Whitehead Research Institute, Cambridge, MA), to amplify two overlapping fragments for exon 1 (1A and 1B) and one fragment for each of exons 2 and 3 (Eurogentech, Belgium), covering part of the VHL 5′UTR, the entire coding sequence and exon-intron junctions (VHL Genbank accession AF010238). The 4 primers are presented in table 1. We amplified 50 to 150ng of tumour DNA and of renal cortex DNA in parallel, using AmpliTaq Gold (Applera, Courtaboeuf, France) and the following PCR conditions: 95°C 9 mins and 95°C 1 min, annealing T° 45 secs, 72°C 45 secs, 35 cycles, MgCL2 1.5 mM, dNTP 200μM. DMSO (5% v/v, Eurobio) was added to amplify exons 1A and 1B. Forward and reverse automatic sequencing was performed using BigDye Terminator v1.1 Cycling Sequencing kit on an ABI Prism 3100 Genetic Analyser (Applied Biosystems, Courtaboeuf, France). All mutations were confirmed in a second round of PCR and sequencing reactions.
Table 1.
Primers for VHL mutation analysis
| Exon: Direction | Primer sequence |
|---|---|
| 1A: Forward | 5′-CGC-GAA-GAC-TAC-GGA-GGT-3′ |
| 1A: Reverse | 5′-GGA-CTG-CGA-TTG-CAG-AAG-AT-3′ |
| 1B: Forward | 5′-GAG-TAC-GGC-CCT-GAA-GAA-GA-3′ |
| 1B: Reverse | 5′-GCT-TCA-GAC-CGT-GCT-ATC-GT-3′ |
| 2: Forward | 5′-CAC-CGG-TGT-GGC-TCT-TTA-AC-3′ |
| 2: Reverse | 5′-TGG-GCT-TAA-TTT-TTC-AAG-TGG-3′ |
| 3: Forward | 5′-GCA-AAG-CCT-CTT-GTT-CGT-TC-3′ |
| 3: Reverse | 5′-ACC-ATC-AAA-AGC-TGA-GAT-GAA-3′ |
Statistical Methods
Tumors with or without VHL mutations were compared for usual clinicopathological features, CAIX expression and RCC-SS. The Chi-square test and the independent sample t-test were respectively used for comparisons of proportions and means. Spearman test was used for correlation analysis. Kaplan-Meier plots were used to graphically illustrate the RCC-SS in the entire cohort, which were compared with the log-rank test. Univariable and multivariable Cox regression models addressed the effect of all predictors on RCC-SS. We categorized CAIX values using the previously described cut-off of 85% (25;26). To reduce overfit bias and to internally validate the accuracy estimates, all univariable and multivariable models were subjected to 200 bootstrap re-samples. All statistical tests were performed using S-PLUS Professional, version 1 (MathSoft Inc., Seattle, Washington).
RESULTS
Patient and Tumor Characteristics
There were 59 males and 41 females who underwent nephrectomy for localized or metastatic RCC. Median tumor size was 7 cm (range 2–22). Fifty one percent of the tumors were locally advanced (pT≥3) and 61% of the tumors were high grade (G3/4). Forty-eight tumors were localized (N0M0), 6 tumors were classified as N+M0, and 46 patients had distant metastases (M1) at the time of nephrectomy (Table 2).
Table 2.
Patients and tumor characteristics in 100 patients with clear cell RCC
| Variable | No. |
|---|---|
| Age, years | |
| Mean | 61.4 |
| SD | 12.2 |
| Gender | |
| Male | 59 |
| Female | 41 |
| ECOG PS | |
| 0 | 55 |
| ≥1 | 45 |
| Tumor size, cm | |
| Mean | 8.1 |
| SD | 3.9 |
| T stage | |
| T1 | 29 |
| T2 | 20 |
| T3 | 48 |
| T4 | 3 |
| N stage | |
| N0 | 85 |
| N1/2 | 15 |
| M stage | |
| M0 | 54 |
| M1 | 46 |
| Fuhrman grade | |
| G1 | 2 |
| G2 | 37 |
| G3 | 41 |
| G4 | 20 |
| VHL mutation | 58 |
| CAIX | |
| High (> 85%) | 78 |
| Low (≤ 85%) | 22 |
| VHL mutation and high CAIX | 50 |
| Deaths from cancer | 31 |
VHL mutational status and CAIX expression
The distribution of VHL mutations and CAIX expression is shown in Figure 1. A VHL mutation was identified in 58 cases. “Stop”, “frameshift”, “missense”, “splice site”, and “in frame insertion” accounted for 13 (22.4%), 26 (44.8%), 12 (20.7%), 6 (10.3%) and 1 (1.8%) cases, respectively. Mutations occurred in exons 1, 2 and 3 in 27 (46.6%), 20 (34.4%) and 11 (19%) cases respectively. The details regarding mutation types and corresponding exon locations are detailed in Table 3.
Figure 1.
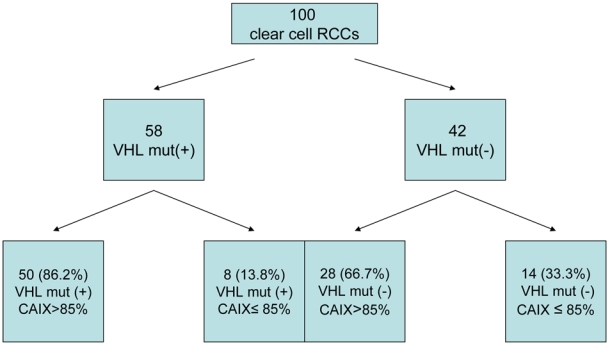
Distribution of VHL mutations and CAIX expression in 100 clear cell RCCs
Table 3.
VHL mutations types in 100 Clear Cell RCC tumors and consequences for CAIX expression
| Exon 1 (n=27) | Exon 2 (n=20) | Exon 3 (n=11) | High CAIX | |
|---|---|---|---|---|
| Stop (n=13) | 6 | 4 | 3 | 11(84.6%) |
| Frameshift (n=26) | 13 | 8 | 5 | 23 (88.5%) |
| Missense (n=12) | 6 | 4 | 2 | 9 (75%) |
| Splice site (n=6) | 1 | 4 | 1 | 6 (100%) |
| In frame insertion (n=1) | 1 | 0 | 0 | 1 (100%) |
| High CAIX | 22 (81.5%) | 17 (85%) | 11 (100%) | |
CAIX was expressed in 97% of tumor specimens and, as anticipated, was found predominantly in the plasma membrane. The staining intensity was generally uniformly strong with minimal variation. Overall, 78% of the tumors exhibited high CAIX expression (expression in >85% of the tumor). CAIX expression according to VHL mutation type and location is presented in Table 3. A significant association was found between the presence of a VHL mutation and the likelihood of having high CAIX expression. As many as 86.2% of the VHL mutated tumors demonstrated a high CAIX expression compared to 66.7% in the non-VHL mutated tumor group (p=0.02). Similarly, mean CAIX expression differed significantly between VHL mutated (91.9±21.1%) and non-mutated (78.7±32.8%) tumors (p=0.01).
Relationship between VHL Mutational Status, CAIX Expression and Standard Clinicopathological Features
A significant association was found between the presence of VHL mutations, high CAIX expression and a less aggressive tumor profile when defined using standard clinicopathological prognostic factors. Nearly 83% of pT1 tumors presented with a VHL mutation and 100% of this group were high CAIX expressors. With increasing pT stage, there was a trend toward reduced incidence of VHL mutation and fewer tumors with high CAIX expression. Similarly, the presence of VHL mutation was associated with the absence of nodal metastases (only 27.7% of N+ patients demonstrated VHL mutations, p=0.008), the absence of distant metastases (only 45.7% of M1 patients demonstrated VHL mutations, p=0.02), and a favorable ECOG performance status (p=0.004). Similar results were observed for high CAIX expression, which was likewise associated with the absence of nodal involvement (p=0.0001), low Fuhrman grades (p=0.02), and small tumor sizes (p=0.01). The associations between VHL mutation, CAIX expression and standard clinicopathological features are summarized in Table 4.
Table 4.
Relationship between CAIX tumor expression, VHL mutational status and main clinical and pathological variables in 100 clear cell RCCs
| Variable | VHL mutation | No VHL mutation | p | High CAIX | Low CAIX | p |
|---|---|---|---|---|---|---|
| ECOG PS | ||||||
| 0 | 39 (70.9%) | 16 (29.1%) | 0.004 | 43 (78.2%) | 12 (21.8%) | 0.9 |
| ≥1 | 19 (42.2%) | 26 (57.8%) | 35 (77.8%) | 10 (22.2%) | ||
| Tumor size, cm | ||||||
| ≤7 | 32 (62.7%) | 19 (37.3%) | 0.3 | 45 (88.2%) | 6 (11.8%) | 0.01 |
| > 7 | 26 (53.1%) | 23 (46.9%) | 33 (67.3%) | 16 (32.7%) | ||
| T stage | ||||||
| T1 | 24 (82.8%) | 5 (17.2%) | 0.01 | 29 (100%) | 0 | 0.007 |
| T2 | 10 (50%) | 10 (50%) | 15 (75%) | 5 (25%) | ||
| T3 | 22 (45.8%) | 26 (54.2%) | 32 (66.7%) | 16 (33.3%) | ||
| T4 | 2 (66.7%) | 1 (33.3%) | 2 (66.7%) | 1 (33.3%) | ||
| N, M stages | ||||||
| N0M0 | 34 (70.8%) | 14 (29.2%) | 0.04 | 41 (85.4%) | 7 (14.6%) | 0.2 |
| N1-2M0 | 3 (50%) | 3 (50%) | 4 (66.7%) | 2 (33.3%) | ||
| M1 | 21(45.7%) | 25 (54.3%) | 33 (71.7%) | 13 (28.3%) | ||
| Fuhrman grade | ||||||
| G1–G2 | 26 (66.7%) | 13 (33.3%) | 0.16 | 35 (89.7%) | 4 (10.3%) | 0.02 |
| G3–G4 | 32 (52.5%) | 29 (45.7%) | 43 (70.5%) | 18 (29.5%) | ||
| Death from cancer | ||||||
| No | 45 (65.2%) | 24 (34.8%) | 0.02 | 58 (84.1%) | 11 (15.9%) | 0.03 |
| Yes | 13 (41.9%) | 18 (58.1%) | 20 (64.5%) | 11 (35.5%) |
VHL Status, CAIX Expression and Cancer-specific Survival
In univariate analysis, patients with VHL mutated tumors had better prognosis than those without: progression-free survival (PFS) was longer (2-year survival: 76% ± 6% vs. 51% ± 8%, p=0.037), however, association of VHL mutational status with RCC-SS only approached statistical significance (2-year RCC-SS: 84% ± 5% vs. 61% ± 8%, p=0.079, Fig. 2A). Univariate Cox-regression analysis showed a hazard ratio of 0.53 (95% CI, 0.25–1.09) indicating a 47% decreased risk of death from RCC for patients with VHL mutated tumors. Additionally, there was a clear survival advantage for patients with high tumoral CAIX expression over patients with low tumoral CAIX expression (2-year RCC-SS: 80% ± 5% vs. 54% ± 12%, p=0.001, Fig. 2B) corresponding to a 70% decreased risk from RCC-specific death (95% CI, 0.14–0.64). Based on VHL mutational status and CAIX expression, we defined three distinct groups with regards to RCC-SS (p=0.002, Fig. 3). Patients with both VHL mutation and high CAIX yielded best survival (2-year survival: 86% ± 5%), while patients with either VHL mutation or high tumoral CAIX expression had intermediate prognosis (2-year survival 69% ± 8%). Finally, we were able to identify an aggressive tumor pattern in patients who had both low CAIX expression and the absence of VHL mutation; the median survival time for these patients was only 18 ± 6 months (2-year survival rate 45% ± 14%). In multivariate Cox regression analysis, CAIX expression, ECOG performance status, T stage, and presence of metastases achieved independent predictor status (Table 5).
Figure 2.
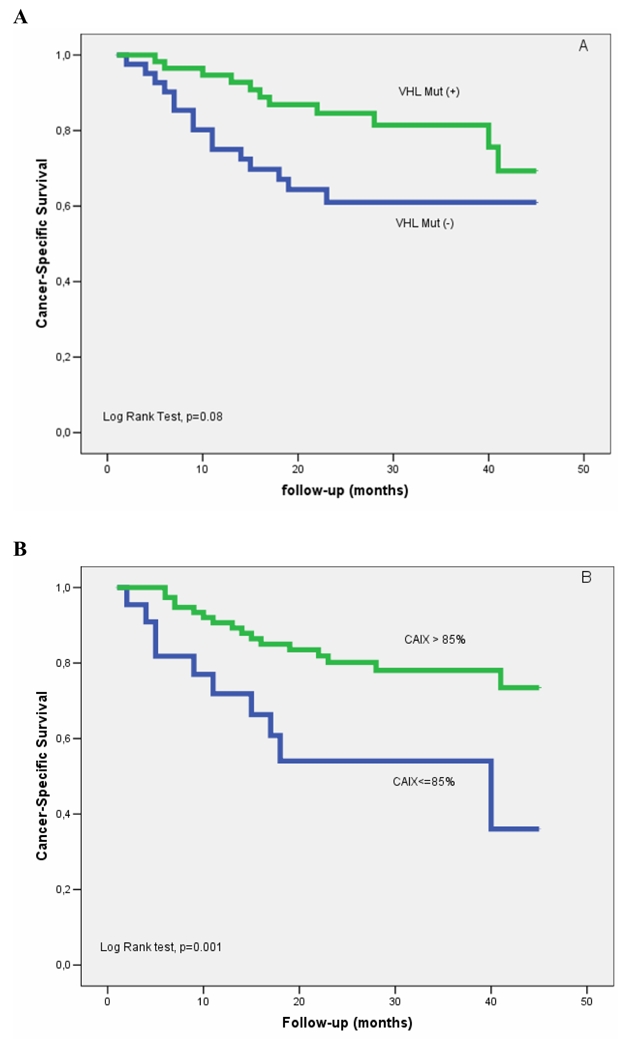
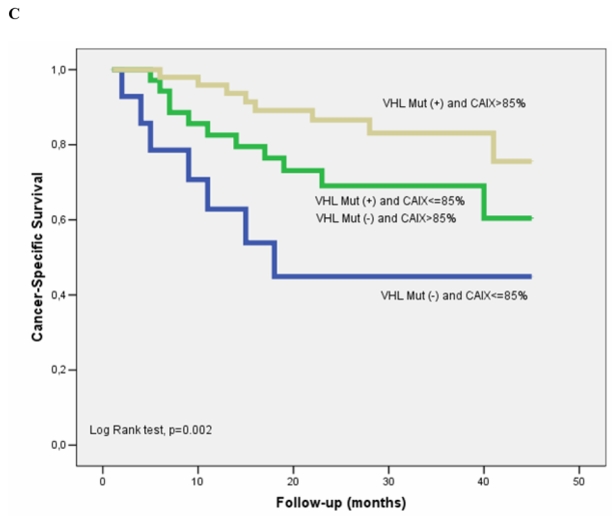
Cancer Specific Survival according to VHL mutational status (A) and CAIX expression (B), and combined (C) in 100 clear cell RCCs
Table 5.
Multivariate Cox regression model for prediction of RCC-SS
| Covariate | HR | 95.0% CI | p | |
|---|---|---|---|---|
| ECOG PS (1 vs. 0) | 3.16 | 1.10 | 9.07 | 0.032 |
| T stage (T3/4 vs. T1/2) | 3.17 | 1.13 | 8.90 | 0.029 |
| Metastastic disease* | 3.39 | 1.05 | 11.0 | 0.042 |
| Grade (G3/4 vs. G1/2) | 0.71 | 0.31 | 1.64 | 0.423 |
| VHL mutation | 1.39 | 0.59 | 3.31 | 0.455 |
| High CAIX | 0.33 | 0.14 | 0.79 | 0.013 |
N+M0 or NanyM1
DISCUSSION
The main findings of this study are that both CAIX expression and VHL mutational status are able to stratify patients with clear cell RCC into distinct groups with regards to clinicopathological variables and prognosis, with low CAIX expression and absence of VHL mutation being associated with a poor clinicopathological phenotype and diminished survival. Combination of CAIX expression and VHL mutational status further enhances prognostic stratification: patients with both VHL mutation and high CAIX expression have the most favorable prognosis, patients with either VHL mutation or high CAIX expression have intermediate prognosis, and patients with neither VHL mutation nor high CAIX expression have the worst prognosis. Our findings may have important implications for patient selection for targeted therapy.
VHL alteration and inactivation through mutation or hypermethylation occurs in more than 50% of sporadic clear cell RCCs (16). VHL alteration is directly linked to tumorigenesis via the hypoxia-induced pathway, which leads to over-expression of several important proteins such as VEGF and CAIX (32). The present study is the first that clearly associates VHL mutation with lower T stages, a lower propensity for nodal or distant metastases, a more favorable ECOG performance status and a lower rate of deaths from RCC. Univariate Cox proportional hazard analysis revealed a 50% decreased risk of death from RCC for patients with VHL mutation compared to those without. Our results are in accordance with the report of Yao et al. (16), who first presented a correlation of VHL mutation and better prognosis. In their series on 187 Japanese patients with sporadic clear cell RCC, VHL alteration was detected in 108 of 187 RCC tumor samples (58%). For TNM stage I–III, VHL alteration yielded significantly better cancer-free and cancer-specific survival times. Similarly, Parker et al. (33) demonstrated in a series of 273 clear cell RCCs that absence of pVHL detected by immunohistochemistry was associated with improved cancer-specific survival. Several studies, however, were not able to correlate VHL status to clinicopathological parameters (14) or prognosis (15), and others linked VHL alteration with more advanced tumor stages (13;34). These discrepancies may be partially explained by recruitment bias with an insufficient number of small low risk tumors being analyzed, inclusion of multiple histological subtypes, or the use of different methodology in that overall TNM grouping was analyzed and not separated into T, N, and M stages. Finally, usage of older and less prognostically relevant TNM classifications, and low statistical power due to small sample and group size may have also contributed to this discrepancy.
VHL alteration is intuitively believed to be associated with tumor aggressiveness (7). This belief was in part due to the fact that VHL alteration leads to stabilization of HIF-1α, which itself acts as a transcription factor for downstream genes responsible for angiogenesis, cancer progression, metastatic spread, glucose metabolism and resistance to hypoxia (35;36). Paradoxically, VHL mutation appears to be associated with lower TNM stages and improved survival. That might be explained by VHL independent activation of the hypoxia-induced pathway e.g. through hypoxia itself (37). Further, it is known that activation of other signal transduction pathways (e.g. the mTOR pathway, NF-kB, STAT-3, EGF-R) up-regulate HIF-1α expression (18;38–40). It might therefore be possible that a small renal tumor that has involved only one tumorigenic pathway is less likely to be aggressive than an advanced tumor in which HIF-1α is activated by several different mechanisms. Moreover, genes activated by the VHL-HIF axis are heterogeneously impacting tumor biology and survival, which could also explain the association of VHL alteration and survival. For example, higher expression of VEGF-A, VEGF-C and their putative epithelial receptors VEGFR-1, VEGFR-2, and VEGFR-3 are all associated with more aggressive tumors and poorer survival (41). Conversely, higher expression of vascular cell adhesion molecule 1 (VCAM1), which is also up-regulated through the VHL-HIF axis, correlates with better outcome (42).
Likewise, CAIX has been linked to better prognosis for patients with metastatic RCC (25). CAIX is a transmembrane enzyme that regulates the pH value by catalyzing the reversible reaction of carbonic acid to carbon dioxide and water allowing tumors to accommodate to an acidic hypoxic environment (18). Thus, one would expect that tumors with high CAIX expression are better adapted on hypoxic conditions, allowing tumor growth, tumor cell survival, and metastatic spread ultimately leading to poorer prognosis. Indeed, studies indicate that high CAIX expression yields an aggressive tumor phenotype and poor prognosis in several cancers (19;20;23;24;43–45). Paradoxically, the opposite has been shown for RCC (25;26), and no hypothesis can entirely explain this phenomenon. The landmark distinguishing RCC from other cancers is the VHL tumor suppressor gene is inactivated in the majority of clear cell renal cell carcinomas. In the majority of clear cell RCC, it is the underlying VHL inactivation, rather than the functional consequence of intratumoral hypoxia, that leads to high CAIX expression. RCC with inactivated VHL may have different pathways impacted, which control tumor growth, progression, and CAIX expression. Hence, the current data supports the concept that CAIX reflects VHL mutational status, and that VHL status is the major driver for the relationship between high CAIX expression and improved survival. It has been further proposed that high CAIX expression is associated with a greater spontaneous or cytokine related immune response leading to better outcome in some cases (26). The fact that immunotherapy with anti-CAIX antibodies shows clinical efficacy (46) reinforces this hypothesis.
Our study confirms that CAIX is regulated in part through VHL. CAIX expression was high (>85%) in 86% of the VHL mutated tumors; conversely, lower CAIX expression was observed in non VHL mutated tumors, probably due to the ability of pVHL to down regulate carbonic anhydrases via ubiquinization and proteasomal degradation of HIF-1α (47). In the present data, CAIX expression was homogeneous and uniformly expressed throughout tumoral epithelium irrespective of areas of hypoxia and necrosis, suggesting a constitutively up-regulated HIF pathway (48). However, CAIX was not entirely abolished suggesting an up-regulation independent of VHL. Taken together, targets of the hypoxia-induced pathway may have different abilities to promote or inhibit tumor growth and may therefore have a different prognostic impact. The divergent role of these up-regulated targets may be explained by other pathways.
It is expected that immunohistochemical and genetic profiling will guide intelligent patient selection for systemic therapy. Expanding on a finding in the study of Bui et al. (25), Atkins and colleagues (26) noted that CAIX expression strongly predicts response to IL-2 based immunotherapy in metastatic clear cell RCC. Thus, patients with high CAIX expression may be appropriate candidates for IL-2 based immunotherapy. Moreover, since combination of CAIX and VHL mutational status improved risk group stratification in the present study, utilization of both CAIX expression and VHL mutation status could further enhance patient selection.
Since VHL alteration leads to over-expression of VEGF and PDGF, patients with VHL alteration may be more susceptible for tyrosine kinase inhibitors such as sorafenib and sunitinib. Recently, Rini et al. (49) evaluated the relevance of the VHL status in 43 patients with metastatic RCC receiving VEGF-targeted therapy. Although median survival was longer in patients with VHL mutation or hypermethylation, no significant association with objective response and tumor shrinkage was observed. However, patient numbers were small and various drugs were evaluated, which may have hindered valid statistical analyses. The relationship between VHL status and response to tyrosine kinase inhibitors remains therefore unclear and needs further investigation.
Some limitations of this study have to be addressed. We investigated a relatively small series of 100 patients with clear cell RCC. Consequently, subgroups are limited in size, which may explain why we were not able to demonstrate an independent prognostic value for CAIX, as observed previously (25). Secondly, we analyzed VHL alteration by mutational analysis only, therefore ignoring deletions and promoter hypermethylation. Of note, we found 28 patients with no VHL mutation and high CAIX expression. These tumors might correspond to VHL promoter hypermethylation which detection rate is close to 20% in the literature (13). Therefore, it is plausible that the correlation between VHL and CAIX is potentially better than the one we presented here.
CONCLUSIONS
CAIX expression and VHL mutational status are able to stratify patients with clear cell RCC into distinct groups with regards to clinicopathological variables and prognosis, with low CAIX expression and absence of VHL mutation being associated with a poor clinicopathological phenotype and diminished survival. Patients with both VHL mutation and high CAIX expression have the most favorable prognosis, patients with either VHL mutation or high CAIX expression have intermediate prognosis, and patients with neither VHL mutation nor high CAIX expression have the worst prognosis. Our findings may have important implications for patient selection for targeted therapy.
Acknowledgments
Short title: CAIX and VHL status in kidney cancer
NIH grant K23CA095151-01
Abbreviations
- VHL
von Hippel-Lindau
- CAIX
carbonic anhydrase IX
- RCC
renal cell carcinoma
- RCC-SS
renal cell carcinoma specific survival
References
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007 Jan;57(1):43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007 Jan 11;356(2):115–24. doi: 10.1056/NEJMoa065044. [DOI] [PubMed] [Google Scholar]
- 3.Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007 Jan 11;356(2):125–34. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 4.Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, Stackhouse T, Kuzmin I, Modi W, Geil L. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993 May 28;260(5112):1317–20. doi: 10.1126/science.8493574. [DOI] [PubMed] [Google Scholar]
- 5.Seizinger BR, Rouleau GA, Ozelius LJ, Lane AH, Farmer GE, Lamiell JM, Haines J, Yuen JW, Collins D, Majoor-Krakauer D. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature. 1988 Mar 17;332(6161):268–9. doi: 10.1038/332268a0. [DOI] [PubMed] [Google Scholar]
- 6.Linehan WM, Walther MM, Zbar B. The genetic basis of cancer of the kidney. J Urol. 2003 Dec;170(6 Pt 1):2163–72. doi: 10.1097/01.ju.0000096060.92397.ed. [DOI] [PubMed] [Google Scholar]
- 7.Gnarra JR, Tory K, Weng Y, Schmidt L, Wei MH, Li H, Latif F, Liu S, Chen F, Duh FM. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 1994 May;7(1):85–90. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- 8.Shuin T, Kondo K, Torigoe S, Kishida T, Kubota Y, Hosaka M, Nagashima Y, Kitamura H, Latif F, Zbar B. Frequent somatic mutations and loss of heterozygosity of the von Hippel-Lindau tumor suppressor gene in primary human renal cell carcinomas. Cancer Res. 1994 Jun 1;54(11):2852–5. [PubMed] [Google Scholar]
- 9.Iliopoulos O, Ohh M, Kaelin WG., Jr pVHL19 is a biologically active product of the von Hippel-Lindau gene arising from internal translation initiation. Proc Natl Acad Sci U S A. 1998 Sep 29;95(20):11661–6. doi: 10.1073/pnas.95.20.11661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blankenship C, Naglich JG, Whaley JM, Seizinger B, Kley N. Alternate choice of initiation codon produces a biologically active product of the von Hippel Lindau gene with tumor suppressor activity. Oncogene. 1999 Feb 25;18(8):1529–35. doi: 10.1038/sj.onc.1202473. [DOI] [PubMed] [Google Scholar]
- 11.Cockman ME, Masson N, Mole DR, Jaakkola P, Chang GW, Clifford SC, Maher ER, Pugh CW, Ratcliffe PJ, Maxwell PH. Hypoxia inducible factor-alpha binding and ubiquitylation by the von Hippel-Lindau tumor suppressor protein. J Biol Chem. 2000 Aug 18;275(33):25733–41. doi: 10.1074/jbc.M002740200. [DOI] [PubMed] [Google Scholar]
- 12.Kim WY, Kaelin WG. Role of VHL gene mutation in human cancer. J Clin Oncol. 2004 Dec 15;22(24):4991–5004. doi: 10.1200/JCO.2004.05.061. [DOI] [PubMed] [Google Scholar]
- 13.Brauch H, Weirich G, Brieger J, Glavac D, Rödl H, Eichinger M, Feurer M, Weidt E, Puranakanitstha C, Neuhaus C, Pomer S, Brenner W, et al. VHL alterations in human clear cell renal cell carcinoma: association with advanced tumor stage and a novel hot spot mutation. Cancer Res. 2000 Apr 1;60(7):1942–8. [PubMed] [Google Scholar]
- 14.Kondo K, Yao M, Yoshida M, Kishida T, Shuin T, Miura T, Moriyama M, Kobayashi K, Sakai N, Kaneko S, Kawakami S, Baba M, et al. Comprehensive mutational analysis of the VHL gene in sporadic renal cell carcinoma: relationship to clinicopathological parameters. Genes Chromosomes Cancer. 2002 May;34(1):58–68. doi: 10.1002/gcc.10054. [DOI] [PubMed] [Google Scholar]
- 15.Kim JH, Jung CW, Cho YH, Lee J, Lee SH, Kim HY, Park J, Park JO, Kim K, Kim WS, Park YS, Im YH, et al. Somatic VHL alteration and its impact on prognosis in patients with clear cell renal cell carcinoma. Oncol Rep. 2005 May;13(5):859–64. [PubMed] [Google Scholar]
- 16.Yao M, Yoshida M, Kishida T, Nakaigawa N, Baba M, Kobayashi K, Miura T, Moriyama M, Nagashima Y, Nakatani Y, Kubota Y, Kondo K. VHL tumor suppressor gene alterations associated with good prognosis in sporadic clear-cell renal carcinoma. J Natl Cancer Inst. 2002 Oct 16;94(20):1569–75. doi: 10.1093/jnci/94.20.1569. [DOI] [PubMed] [Google Scholar]
- 17.Wykoff CC, Beasley NJ, Watson PH, Turner KJ, Pastorek J, Sibtain A, Wilson GD, Turley H, Talks KL, Maxwell PH, Pugh CW, Ratcliffe PJ, et al. Hypoxia-inducible expression of tumor-associated carbonic anhydrases. Cancer Res. 2000 Dec 15;60(24):7075–83. [PubMed] [Google Scholar]
- 18.Dorai T, Sawczuk I, Pastorek J, Wiernik PH, Dutcher JP. Role of carbonic anhydrases in the progression of renal cell carcinoma subtypes: proposal of a unified hypothesis. Cancer Invest. 2006 Dec;24(8):754–79. doi: 10.1080/07357900601062321. [DOI] [PubMed] [Google Scholar]
- 19.Swinson DE, Jones JL, Richardson D, Wykoff C, Turley H, Pastorek J, Taub N, Harris AL, O’Byrne KJ. Carbonic anhydrase IX expression, a novel surrogate marker of tumor hypoxia, is associated with a poor prognosis in non-small-cell lung cancer. J Clin Oncol. 2003 Feb 1;21(3):473–82. doi: 10.1200/JCO.2003.11.132. [DOI] [PubMed] [Google Scholar]
- 20.Maseide K, Kandel RA, Bell RS, Catton CN, O’Sullivan B, Wunder JS, Pintilie M, Hedley D, Hill RP. Carbonic anhydrase IX as a marker for poor prognosis in soft tissue sarcoma. Clin Cancer Res. 2004 Jul 1;10(13):4464–71. doi: 10.1158/1078-0432.CCR-03-0541. [DOI] [PubMed] [Google Scholar]
- 21.Span PN, Bussink J, Manders P, Beex LV, Sweep CG. Carbonic anhydrase-9 expression levels and prognosis in human breast cancer: association with treatment outcome. Br J Cancer. 2003 Jul 21;89(2):271–6. doi: 10.1038/sj.bjc.6601122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haapasalo JA, Nordfors KM, Hilvo M, Rantala IJ, Soini Y, Parkkila AK, Pastorekova S, Pastorek J, Parkkila SM, Haapasalo HK. Expression of carbonic anhydrase IX in astrocytic tumors predicts poor prognosis. Clin Cancer Res. 2006 Jan 15;12(2):473–7. doi: 10.1158/1078-0432.CCR-05-0848. [DOI] [PubMed] [Google Scholar]
- 23.Driessen A, Landuyt W, Pastorekova S, Moons J, Goethals L, Haustermans K, Nafteux P, Penninckx F, Geboes K, Lerut T, Ectors N. Expression of carbonic anhydrase IX (CA IX), a hypoxia-related protein, rather than vascular-endothelial growth factor (VEGF), a pro-angiogenic factor, correlates with an extremely poor prognosis in esophageal and gastric adenocarcinomas. Ann Surg. 2006 Mar;243(3):334–40. doi: 10.1097/01.sla.0000201452.09591.f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen J, Röcken C, Hoffmann J, Krüger S, Lendeckel U, Rocco A, Pastorekova S, Malfertheiner P, Ebert MP. Expression of carbonic anhydrase 9 at the invasion front of gastric cancers. Gut. 2005 Jul;54(7):920–7. doi: 10.1136/gut.2004.047340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bui MH, Seligson D, Han KR, Pantuck AJ, Dorey FJ, Huang Y, Horvath S, Leibovich BC, Chopra S, Liao SY, Stanbridge E, Lerman MI, et al. Carbonic anhydrase IX is an independent predictor of survival in advanced renal clear cell carcinoma: implications for prognosis and therapy. Clin Cancer Res. 2003 Feb;9(2):802–11. [PubMed] [Google Scholar]
- 26.Atkins M, Regan M, McDermott D, Mier J, Stanbridge E, Youmans A, Febbo P, Upton M, Lechpammer M, Signoretti S. Carbonic anhydrase IX expression predicts outcome of interleukin 2 therapy for renal cancer. Clin Cancer Res. 2005 May 15;11(10):3714–21. doi: 10.1158/1078-0432.CCR-04-2019. [DOI] [PubMed] [Google Scholar]
- 27.Sobin LH, Wittekind C TNM classification of malignant tumors. UICC International Union Against Cancer. 6. Willey-Liss; 2003. Kidney; pp. 193–5. [Google Scholar]
- 28.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982 Dec;5(6):649–55. [PubMed] [Google Scholar]
- 29.Fuhrman SA, Lasky LC, Limas C. Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol. 1982 Oct;6(7):655–63. doi: 10.1097/00000478-198210000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Zavada J, Zavadova Z, Pastorekova S, Ciampor F, Pastorek J, Zelnik V. Expression of MaTu-MN protein in human tumor cultures and in clinical specimens. Int J Cancer. 1993 May 8;54(2):268–74. doi: 10.1002/ijc.2910540218. [DOI] [PubMed] [Google Scholar]
- 31.Liao SY, Brewer C, Zavada J, Pastorek J, Pastorekova S, Manetta A, Berman ML, DiSaia PJ, Stanbridge EJ. Identification of the MN antigen as a diagnostic biomarker of cervical intraepithelial squamous and glandular neoplasia and cervical carcinomas. Am J Pathol. 1994 Sep;145(3):598–609. [PMC free article] [PubMed] [Google Scholar]
- 32.Pantuck AJ, Zeng G, Belldegrun AS, Figlin RA. Pathobiology, prognosis, and targeted therapy for renal cell carcinoma: exploiting the hypoxia-induced pathway. Clin Cancer Res. 2003 Oct 15;9(13):4641–52. [PubMed] [Google Scholar]
- 33.Parker AS, Cheville JC, Lohse CM, Igel T, Leibovich BC, Blute ML. Loss of expression of von Hippel-Lindau tumor suppressor protein associated with improved survival in patients with early-stage clear cell renal cell carcinoma. Urology. 2005 Jun;65(6):1090–5. doi: 10.1016/j.urology.2004.12.040. [DOI] [PubMed] [Google Scholar]
- 34.Schraml P, Struckmann K, Hatz F, Sonnet S, Kully C, Gasser T, Sauter G, Mihatsch MJ, Moch H. VHL mutations and their correlation with tumour cell proliferation, microvessel density, and patient prognosis in clear cell renal cell carcinoma. J Pathol. 2002 Feb;196(2):186–93. doi: 10.1002/path.1034. [DOI] [PubMed] [Google Scholar]
- 35.Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, Wykoff CC, Pugh CW, Maher ER, Ratcliffe PJ. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature. 1999 May 20;399(6733):271–5. doi: 10.1038/20459. [DOI] [PubMed] [Google Scholar]
- 36.Krieg M, Haas R, Brauch H, Acker T, Flamme I, Plate KH. Up-regulation of hypoxia-inducible factors HIF-1alpha and HIF-2alpha under normoxic conditions in renal carcinoma cells by von Hippel-Lindau tumor suppressor gene loss of function. Oncogene. 2000 Nov 16;19(48):5435–43. doi: 10.1038/sj.onc.1203938. [DOI] [PubMed] [Google Scholar]
- 37.Hockel M, Vaupel P. Tumor hypoxia: definitions and current clinical, biologic, and molecular aspects. J Natl Cancer Inst. 2001 Feb 21;93(4):266–76. doi: 10.1093/jnci/93.4.266. [DOI] [PubMed] [Google Scholar]
- 38.Zhong H, Chiles K, Feldser D, Laughner E, Hanrahan C, Georgescu MM, Simons JW, Semenza GL. Modulation of hypoxia-inducible factor 1alpha expression by the epidermal growth factor/phosphatidylinositol 3-kinase/PTEN/AKT/FRAP pathway in human prostate cancer cells: implications for tumor angiogenesis and therapeutics. Cancer Res. 2000 Mar 15;60(6):1541–5. [PubMed] [Google Scholar]
- 39.Rafajova M, Zatovicova M, Kettmann R, Pastorek J, Pastorekova S. Induction by hypoxia combined with low glucose or low bicarbonate and high posttranslational stability upon reoxygenation contribute to carbonic anhydrase IX expression in cancer cells. Int J Oncol. 2004 Apr;24(4):995–1004. [PubMed] [Google Scholar]
- 40.Pantuck AJ, Thomas G, Belldegrun AS, Figlin RA. Mammalian target of rapamycin inhibitors in renal cell carcinoma: current status and future applications. Semin Oncol. 2006 Oct;33(5):607–13. doi: 10.1053/j.seminoncol.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Lam JS, Leppert JT, Yu H, Seligson DB, Dong J, Horvath S, Pantuck AJ, Figlin RA, Belldegrun AS.Expression of the Vacular Endothelial Growth Factor Family in Tumor Dissemination and Disease Free Survival in Clear Cell Renal Cell Carcinoma J Clin Oncol 20052316S453816002845 [Google Scholar]
- 42.Shioi K, Komiya A, Hattori K, Huang Y, Sano F, Murakami T, Nakaigawa N, Kishida T, Kubota Y, Nagashima Y, Yao M. Vascular cell adhesion molecule 1 predicts cancer-free survival in clear cell renal carcinoma patients. Clin Cancer Res. 2006 Dec 15;12(24):7339–46. doi: 10.1158/1078-0432.CCR-06-1737. [DOI] [PubMed] [Google Scholar]
- 43.Trastour C, Benizri E, Ettore F, Ramaioli A, Chamorey E, Pouyssegur J, Berra E. HIF-1alpha and CA IX staining in invasive breast carcinomas: Prognosis and treatment outcome. Int J Cancer. 2007 Apr 1;120(7):1443–50. doi: 10.1002/ijc.22436. [DOI] [PubMed] [Google Scholar]
- 44.Loncaster JA, Harris AL, Davidson SE, Logue JP, Hunter RD, Wycoff CC, Pastorek J, Ratcliffe PJ, Stratford IJ, West CM. Carbonic anhydrase (CA IX) expression, a potential new intrinsic marker of hypoxia: correlations with tumor oxygen measurements and prognosis in locally advanced carcinoma of the cervix. Cancer Res. 2001 Sep 1;61(17):6394–9. [PubMed] [Google Scholar]
- 45.Lee S, Shin HJ, Han IO, Hong EK, Park SY, Roh JW, Shin KH, Kim TH, Kim JY. Tumor carbonic anhydrase 9 expression is associated with the presence of lymph node metastases in uterine cervical cancer. Cancer Sci. 2007 Mar;98(3):329–33. doi: 10.1111/j.1349-7006.2007.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bleumer I, Knuth A, Oosterwijk E, Hofmann R, Varga Z, Lamers C, Kruit W, Melchior S, Mala C, Ullrich S, De MP, Mulders PF, et al. A phase II trial of chimeric monoclonal antibody G250 for advanced renal cell carcinoma patients. Br J Cancer. 2004 Mar 8;90(5):985–90. doi: 10.1038/sj.bjc.6601617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ivanov SV, Kuzmin I, Wei MH, Pack S, Geil L, Johnson BE, Stanbridge EJ, Lerman MI. Down-regulation of transmembrane carbonic anhydrases in renal cell carcinoma cell lines by wild-type von Hippel-Lindau transgenes. Proc Natl Acad Sci U S A. 1998 Oct 13;95(21):12596–601. doi: 10.1073/pnas.95.21.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Potter C, Harris AL. Hypoxia inducible carbonic anhydrase IX, marker of tumour hypoxia, survival pathway and therapy target. Cell Cycle. 2004 Feb;3(2):164–7. [PubMed] [Google Scholar]
- 49.Rini BI, Jaeger E, Weinberg V, Sein N, Chew K, Fong K, Simko J, Small EJ, Waldman FM. Clinical response to therapy targeted at vascular endothelial growth factor in metastatic renal cell carcinoma: impact of patient characteristics and Von Hippel-Lindau gene status. BJU Int. 2006 Oct;98(4):756–62. doi: 10.1111/j.1464-410X.2006.06376.x. [DOI] [PubMed] [Google Scholar]


