Abstract
The ultimate goal in treating zygomatic complex fracture is to obtain an accurate, stable reduction while minimizing external scars and functional deformity. The present authors present our experiences with a single transconjunctival incision and two-point (inferior orbital rim and frontozygomatic suture) fixation in 53 patients with zygomatic complex fracture which were not comminuted. All patients had transconjunctival approaches with lateral canthal extensions, and six out of 53 patients also had an additional small (about less than 2 cm) gingivobuccal incision to achieve an accurate reduction. There were 3 minor complications, and the overall esthetics and functional results were satisfactory with a long term follow-up. Our method has the following advantages in the reduction of zygomatic complex fracture; It leaves only an inconspicuous lateral canthal scar. In addition, it provides excellent simultaneous visualization of the inferior orbital rim and frontozygomatic suture area. Hence, two-point fixation through a single incision can be performed with a satisfactory stability.
Keywords: Surgical Procedures, Operative; Single Transconjunctival Incision; Zygomatic Fractures
INTRODUCTION
The zygomaticomaxillary complex is an important functional and aesthetic landmark of the midface, and it provides prominent cheek structure.
However, unfortunately it is very vulnerable to injury because of its intrinsically prominent convexity. There are four bony attachments between zygoma and other facial bones: a superior attachment to the frontal bone (frontozygomatic suture line), a medial attachment to the maxilla (zygomaticomaxillary suture line), a lateral attachment to the temporal bone (zygomaticotemporal suture line), and a deep attachment to the greater wing of the sphenoid bone (zygomaticosphenoidal suture line). When blunt trauma to the zygomatic complex results in fractures of all four suture lines, it is referred to as a tetrapod fracture.
Various surgical techniques have been described for the reduction of zygomatic complex fracture. Closed reduction without surgical incisions has virtually been abandoned because judgment on the adequate reduction of fracture could not been made and it often resulted in disappointing cosmetic results. Open reduction with surgical incisions has been accomplished through Keen's approach, Gillies' approach, bicoronal scalp flap approach or the more popular Dingman's approach (1).
Gillies' approach is the temporal approach. This procedure has advantages in that it leaves no facial scars and is simple to perform. However, the fracture site is not directly visualized and access to the orbit is not possible, which may result in incomplete surgical reduction.
The bicoronal scalp flap provides excellent exposure to the lateral orbit and zygoma. However, it necessitates a lengthy scalp incision and provides inadequate exposure to the inferior, medial aspect of orbit, and may leave a conspicuous long scalp scar. Also, because of its extensive dissection, the temporal branch of the facial nerve may be damaged.
The Dingman's approach has become the most popular method in repairing zygomatic complex fractures. This procedure utilizes a lateral eyebrow incision line and a second incision across the entire lower eyelid in the subciliary line. This technique provides good exposure and direct visualization of the frontozygomatic area, inferior orbital rim and orbital floor. But, it provides limited exposure of the lateral orbital rim because it consists of two separate facial incisions, and it leaves external cutaneous scars. Also, there is some risk of lower eyelid ectropion due to cicatrical contracture.
Since its first description for the removal of herniated orbital fat, there have been subsequent reports demonstrating the efficacy of transconjunctival approach not only for the lower eyelid blepharoplasty but also for the repair of orbital fractures (2-5).
McCord and Moses (6) described the addition of the lateral canthotomy incision to gain access to the lateral orbital wall and inferior orbital rim, and Nunery (1) reported a lateral superior cantholysis for the repair of trimalar fractures. Since then, a few authors (7-9) have described the advantages of this type of incision, but there has been no report that describe the long term results of two-point fixation through the single transconjunctival incision for the treatment of zygoma fracture.
MATERIALS AND METHODS
Patients
Between March 2002 and January 2006, a total of 53 patients with zygomatic complex fractures, which were not severely comminuted, were treated with this surgical method. Included were 48 men and five women, aged 15 to 88 yr (mean age 33.2 yr).
Twenty eight patients (52.8%) had associated blow out fracture, two patients (3.7%) had associated nasal bone and mandible fracture, and one patient (1.9%) had associated nasal bone fracture (Table 1). Upon Knight and North classification, four patients (7.5%) belonged to group I, twenty one patients (39.6%) belonged to group II, eight patients (15%) belonged to group IV, eleven patients (20.7%) belonged to group V, and nine patients (16.9%) belonged to group VI. All patients were treated with two-point fixation through a single transconjunctival approach with a lateral canthal extension. If the reduction of zygoma was not complete, an additional small gingivobuccal incision (less than 2 cm) was made and subperiosteal dissection was performed to expose zygomaticomaxillary buttress and posterior surface of zygoma. Through the small gingivobuccal incision, Dingman's elevator was inserted and an accurate reduction was accomplished.
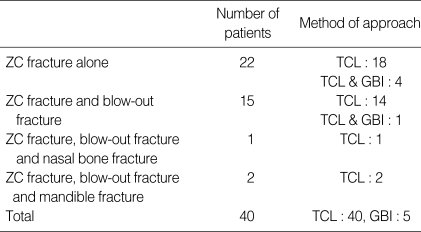
Table 1.
Patient data
ZC, zygomatic complex; TCL, transconjunctival approach with lateral canthal extension; GBI, small gingivobuccal incision.
The follow-up period ranged from 8 to 46 months (average 24.8 months). Preoperative and postoperative clinical examinations were performed with special attention paid to features such as symmetry of zygoma and canthal ligaments, enophthalmos, diplopia, limited ocular function, scarring and ectropion. Follow-up radiographs (Waters' view and zygomatic arch view) were routinely used to evaluate the adequacy of reduction.
Surgical techniques
Under general endotracheal anesthesia, a lateral canthal incision, about 1.0-2.0 cm, is made down to the periosteum of lateral orbital rim. Then, the conjunctiva is incised 2-3 mm below the tarsus extending from the commissure to a point just lateral to the punctum, and the transconjunctival incision is connected to the lateral canthal incision (Fig. 1). In the lateral canthal area, the lower eyelid flap is pulled down by cutting the superficial lateral canthal tendon and inferior limb of deep lateral canthal tendon with fine scissors. Dissection proceeds anteriorly and inferiorly between the orbicularis oculi muscle and orbital septum until the periosteum of the inferior orbital rim is exposed.
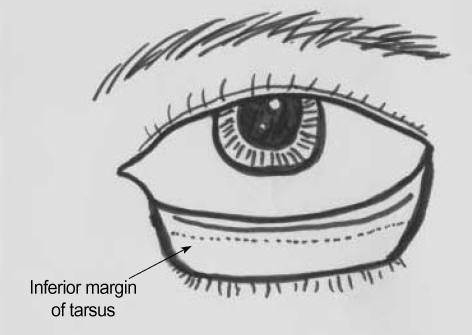
Fig. 1.
After lateral canthal incision is made down to the periosteum of lateral orbital rim, the conjunctiva is incised 2, 3 mm below the tarsus from a point just lateral to the punctum to the lateral canthal incision site.
Through the extended lateral canthal incision, the lateral aspect of the upper lid is retracted superiorly, and the periosteum of lateral orbital rim is exposed. The periosteum is incised and a subperiosteal dissection is done to expose the orbital floor, the inferior orbital rim, and the lateral orbital rim including the zygomaticofrontal suture area (Fig. 2).
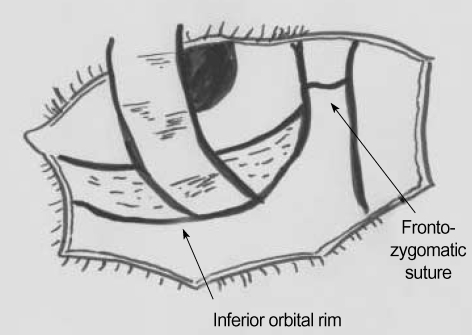
Fig. 2.
By pulling the lower eyelid flap down and pulling the upper eyelid flap up, the entire lateral and inferior orbital rim can be exposed.
Through the lateral canthal incision, the Dingman's elevator is placed posteriorly to the body of the zygoma along the zygomatic arch and a reduction of zygoma is done. If the reduction of zygoma is not complete or unsatisfactory, an additional small gingivobuccal incision (less than 2 cm) is made and a limited subperiosteal dissection is performed to expose the zygomaticomaxillary buttress and posterior surface of zygoma. Dingman's elevator is inserted through the small gingivobuccal incision and an accurate reduction can be accomplished. In all cases, complete reduction was confirmed by the accurate alignment of the lateral and inferior orbital wall. Then, the two-points (frontozygomatic suture and inferior orbital rim) are fixated with plates and screws (Fig. 3). Resorbable 2.0-mm miniplates systems, MacroSorb® (Macropore,San Diego, CA, U.S.A.) were used in 35 patients (87.5%) and titanium miniplates (Osteomed, Dallas, TX, U.S.A.) were used in 5 patients (12.5%).
Fig. 3.
Through a single transconjunctival incision, two-point fixation (inferior orbital rim and frontozygomatic suture) with four hole resorbable 2.0 mm miniplates systems (arrows) can be performed without difficulty.
If there is an associated impure blow-out fracture, orbital floor reconstruction with porous polyethylene implant (Medpor®) is performed. The periosteum is closed with a 4-0 absorbable suture, and the conjunctiva is closed by a 7-0 absorbable suture. In case of old patient with lid laxity, the canthopexy is accomplished by a 5-0 absorbable suture fixation in the direction of posterior-superiorly to the periosteum of lateral orbital rim to prevent the postoperative ectropion. In other cases, just accurate approximation of the incision site is sufficient. The orbicularis oculi muscle layer is closed with a 5-0 absorbable suture. Finally, the skin and subcutaneous layer at the lateral canthal incision site is closed with a 6-0 suture. The intraoral incision site is closed with a 5-0 absorbable suture.
RESULTS
During the average 24.8 months of follow up, most patients had functionally and esthetically satisfactory results. All patients showed satisfactory facial symmetry, no lateral canthal displacement, and no functional impairment. None of them had persistent diplopia, enophthalmos or alteration of visual acuity. Upon postoperative radiography (skull Waters view and zygomatic arch view), zygomatic symmetry was documented in all patients (Fig. 4, 5).
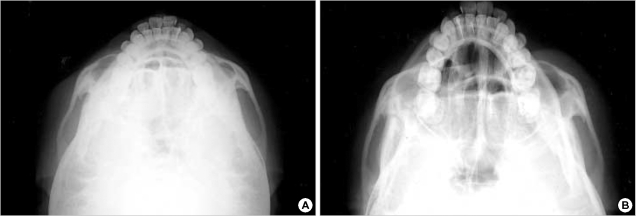
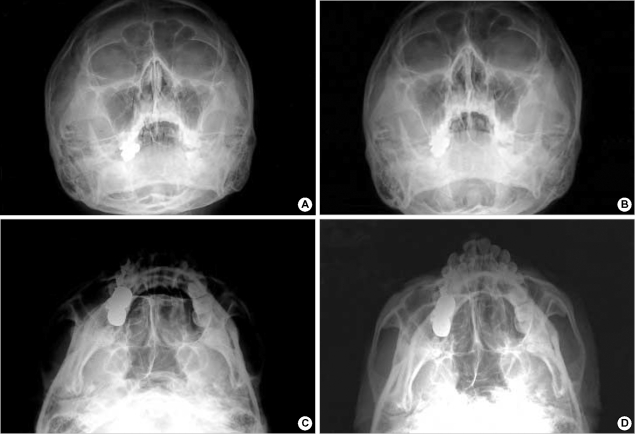
Fig. 4.
(A) Preoperative zygomatic arch view (submentovertical view) shows fracture and displacement of the left zygoma bone. (B) Postoperative zygomatic arch view.
Fig. 5.
(A) Preoperative skull Waters view, (B) Postoperative skull Waters view, (C) Preoperative zygomatic arch view, (D) Postoperative zygomatic arch view.
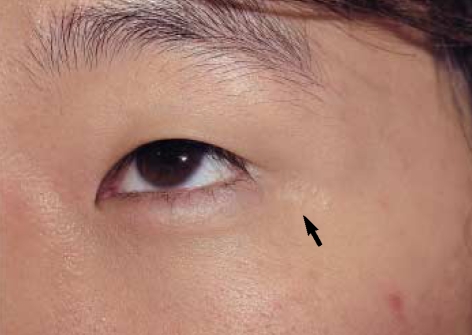
Three patients (5.7%) had a postoperative complication. One patient (1.9%) had persistent scleral show and was corrected three months after the repair of zygomatic complex fracture. This case was 78 yr-old patient who had lid laxity preoperatively and showed ectropion postoperatively, which may be due to scar contracture. And canthal reattachement procedure (canthopexy) with release of the scar was peformed. Two patients (3.7%) had mild hyperpigmentation at the lateral canthal incision site even after six months postoperatively. But most of patients showed hardly visible scar in the lateral canthal area (Fig. 6).
Fig. 6.
Follow up at 2 yr after the operation. There is hardly visible scarring at the lateral canthal area (arrow).
DISCUSSION
Various surgical techniques have been described for the repair of a zygomatic complex fracture.
Although subciliary incision with lateral eyebrow incision (Dingman's approach) is the most common approach to the zygomatic complex (7, 10), it can leave a visible scar and ectropion of the lower eyelid. Factors predisposing to an eyelid retraction and ectropion include hematoma, eyelid edema, adhesions of the orbital septum, scar contracture, horizontal laxity of the eyelid margin, weakening of the pretarsal muscle, and wide dissection of the anterior periosteum (11). To decrease the complication rates of the subciliary approach, many authors have tried to treat zygoma complex fracture repair using the transconjunctival approach (1, 6-9). They emphasized the advantage of this approach over the Dingman's approach, in terms of minimal ectropion, hidden scars, and minimal lid lymphedema.
In the transconjunctival approach, the dissection can be performed in one of two separate planes; preseptal approach and retroseptal approach. Some authors (12, 13) advocated that the retroseptal approach is preferred because it can be performed easily and the integrity between orbital septum and orbicularis oculi muscle is not disturbed. However, the retroseptal approach has increased risk of injury to the inferior oblique muscle and prolapse of orbital fat into the surgical field (10, 11). Hence, all our patients were treated with the transconjunctival preseptal approach.
In the management of the lateral canthal extension site, Manson et al. (9) advocated that the canthal reattachment is not required in an acute fracture treatment but is necessary in fractures when treatment is delayed, in patients with established canthal deformities, or in patients in whom a simultaneous coronal incision is employed. According to them, the anterior limb of the lateral canthal tendon which is also referred to as the superficial lateral canthal tendon by other authors (14), is continuous to the temporal fascia and galea aponeurotica and the diffuse connections of this limb facilitate proper positioning of the canthus after mobilization of the posterior limb (deep lateral canthal tendon).
The current authors think that in addition to some indications mentioned above, patients of old age with lid laxity also needs lateral canthal reattachments or canthopexy. Its significance began to be considered following our case of a 78 yr-old patient who developed persistent ectropion when canthal reattachment had not been performed.
The precise physical stability of the zygoma with respect to the number and location of miniplates applied is not known, because it depends on fracture anatomy, extent, and the amount of displacement. Some laboratory studies, using human cadaver heads, have been conducted to investigate the stability of fixated zygoma. In 1989, Rinehart et al. (15) simulated noncomminuted zygoma fractures in eight human cadaver heads and the stability of fracture fixation was studied for various fixation patterns. In their study, double-miniplate fixation across the zygomaticofrontal and zygomaticomaxillary fracture lines is sufficient to withstand static and oscillating loading similar to physiologic masticatory forces. In 1990, Davidson et al. (16) analyzed different methods of internal fixation of simple displaced fractures of the zygoma in an attempt to define the simplest method of achieving postreduction stability. In their report, the three-point fixation (frontozygomatic suture, inferior orbital rim, and zygomaticomaxillary buttress) using either miniplates alone or interfragmentary wiring conferred the greatest stability. In addition, they proposed that the two-point fixation using miniplate alone conferred a degree of stability comparable to most methods of three-point fixation regardless of the site in which the miniplates were applied.
We concur with the above assertions and think that two-point miniplate fixation at the infraorbital rim and zygomaticofrontal suture would suffice, provided the comminution of the zygoma is not severe. Although not the focus of our attention in this study, in case of severely comminuted fracture, three-point fixation through the transconjunctival incision and gingivobuccal incision is preferably performed.
To fixate the fracture site and provide stability, we used four hole resorbable 2.0-mm miniplates systems, MacroSorb® (Macropore, San Diego, CA, U.S.A.) in most patients, and titanium miniplates (Osteomed, Dalllas, TX, U.S.A.) only when there was a segmental fracture at the infraorbital rim or when requested by the patient due to the lighter financial burden.
In addition to the inconspicuous scarring, the main advantage of this method is a direct and full visualization of the lateral and inferior orbital wall to be served as a guidance for an accurate reduction, which makes the reduction more successful. The only drawback we experienced in our method is a little difficulty in reducing the fracture-displaced zygoma because of limited space and a slightly inadequate vector for the elevator. Usually a fractured zygoma is displaced and rotated posteriorly and medially, so an anterior-lateral pull is required. However, the lateral canthal incision is located medially to the zygoma body and lateral pulling of the zygoma body may be a little difficult.
In conclusion, we believe that the proposed technique is very useful for the treatment of zygomatic complex fracture which is not severely comminuted, because it provides excellent exposure and postoperative stability of the zygoma with a lower incidence of complications, including visible scarring and ectropion.
Footnotes
The authors clearly indicate that there is no research grant support.
References
- 1.Nunery WR. Lateral canthal approach to repair of trimalar fractures of the zygoma. Ophthal Plast Reconstr Surg. 1985;1:175–183. doi: 10.1097/00002341-198501030-00004. [DOI] [PubMed] [Google Scholar]
- 2.Tenzel RR, Miller GR. Orbital blow out fracture repair, conjunctival approach. Am J Ophthalmol. 1971;71:1141–1142. doi: 10.1016/0002-9394(71)90592-7. [DOI] [PubMed] [Google Scholar]
- 3.Tessier P. The conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. J Maxillofac Surg. 1973;1:3–8. doi: 10.1016/s0301-0503(73)80005-0. [DOI] [PubMed] [Google Scholar]
- 4.Converse JM, Firman F, Wood-Smith D. The conjunctival approach in orbital fractures. Plast Reconstr Surg. 1973;52:656–657. doi: 10.1097/00006534-197312000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Lynch DJ, Lamp JC, Royster HP. The conjunctival approach for exploration of the orbital floor. Plast Reconstr Surg. 1974;54:153–156. [PubMed] [Google Scholar]
- 6.McCord CD, Jr, Moses JL. Exposure of the inferior orbit with fornix incision and lateral canthotomy. Ophthalmic Surg. 1979;10:53–63. [PubMed] [Google Scholar]
- 7.Waite PD, Carr DD. The transconjunctival approach for treating orbital trauma. J Oral Maxillofac Surg. 1991;49:499–503. doi: 10.1016/0278-2391(91)90174-k. [DOI] [PubMed] [Google Scholar]
- 8.Shaw GY, Khan J. Precise repair of orbital maxillary zygomatic fracture. Arch Otolaryngol Head Neck Surg. 1994;120:613–619. doi: 10.1001/archotol.1994.01880300029004. [DOI] [PubMed] [Google Scholar]
- 9.Manson PN, Ruas E, Iliff N, Yaremchuk M. Single eyelid incision for exposure of the zygomatic bone and orbital reconstruction. Plast Reconstr Surg. 1987;79:120–126. [PubMed] [Google Scholar]
- 10.Strong EB, Sykes JM. Zygoma complex fractures. Facial Plast Surg. 1998;14:105–115. doi: 10.1055/s-0028-1085306. [DOI] [PubMed] [Google Scholar]
- 11.Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg. 1993;119:1000–1007. doi: 10.1001/archotol.1993.01880210090012. [DOI] [PubMed] [Google Scholar]
- 12.Suga H, Sugawara Y, Uda H, Kobayashi N. The transconjunctival approach for orbital bony surgery: In which cases should it be used? J Craniofac Surg. 2004;15:454–457. doi: 10.1097/00001665-200405000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Manganello-Souza LC, de Freitas RR. Transconjunctival approach to zygomatic and orbital floor fractures. Int J Oral Maxillofac Surg. 1997;26:31–34. doi: 10.1016/s0901-5027(97)80843-0. [DOI] [PubMed] [Google Scholar]
- 14.Knize DM. The superficial lateral canthal tendon:anatomic study and clinical application to lateral canthopexy. Plast Reconstr Surg. 2002;109:1149–1157. doi: 10.1097/00006534-200203000-00056. [DOI] [PubMed] [Google Scholar]
- 15.Rinehart GC, Marsh JL, Hemmer KM, Bresina S. Internal fixation of malar fractures: An experimental biophysical study. Plast Reconstr Surg. 1989;84:21–25. [PubMed] [Google Scholar]
- 16.Davidson J, Nickerson D, Nickerson B. Zygomatic fractures: Comparison of method of internal fixation. Plast Reconstr Surg. 1990;86:25–32. [PubMed] [Google Scholar]