Abstract
We report results on the seroprevalence of antibodies to Coxiella burnetii in cattle and healthy people in Korea. Upon agreement with dairy owners, serum samples from 414 dairy cattle were collected between March and June 2001 and samples from 205 people for health screening were collected between April and December 2002. The sera were analyzed for the presence of anti-C. burnetii phase II antibodies using an indirect microimmunofluorescence test; strong fluorescence at a 1:32 dilution was regarded as positive. The overall seroprevalence of C. burnetii in cattle in Korea was 25.6%, with regional variation from 8.9 to 59.3%. Of the positive serum samples, 75.5% had antibody titers ≥1:256. By contrast, only 1.5% of people in a rural area were seropositive, and most of the positive samples had low antibody titers. In conclusion, this study showed that relatively high seropositivity of C. burnetii in dairy cattle, accordingly, the studies on the high-risk groups are needed to evaluate the seroprevalence for this organism in Korea.
Keywords: Coxiella burnetii, Seroepidemiological Studies, Seroprevalence, Korea, Q Fever
INTRODUCTION
Q fever is a zoonotic disease that is caused by Coxiella burnetii, a microorganism that frequently infects domestic ungulates, as well as wild mammals in many genera (1). In animals, Q fever is rarely symptomatic, except for manifestations as reproductive disorders in females. The disease is transmitted to humans incidentally by inhalation of aerosols from infected cattle and sheep (1, 2). In humans, C. burnetii infection may be asymptomatic, acute, or chronic. Acute Q fever may manifest as pneumonia, hepatitis, or both. Chronic Q fever is rare, with endocarditis presenting as the most common complication (1, 3).
Q fever has been reported in almost every country, except New Zealand (4). In Canada, 6 to 20% of cats have anti-C. burnetii antibodies (5). In Japan, 60 to 84% of cattle with reproductive disorders are seropositive (6). A study conducted in southern France showed that 5 to 8% of endocarditis cases in humans were due to C. burnetii, and the prevalence of acute Q fever was 50 cases per 100,000 inhabitants (7). Researchers have suggested that the incidence of Q fever is chronically underestimated because clinical manifestations of the disease are often nonspecific or even absent. Therefore, concerns with the disease focus on the importance of detection (1, 3, 8).
In Korea, there is a little information concerning the epidemiology of C. burnetii infection in either animals or humans. A few cases of acute Q fever in humans have been reported (9, 10). One study showed that the seroprevalence of anti-C. burnetii antibodies was less than 1% in healthy people in Korea (11).
We examined the prevalence of antibodies to C. burnetii in dairy cattle nationwide and in people for health screening in a rural area of Korea, and used the data to evaluate the impact of Q fever in both animals and humans in Korea. The analyses were done retrospectively.
MATERIALS AND METHODS
Subjects
Upon agreement with dairy owners, serum samples from 414 dairy cattle were collected on 31 farms from March to June, 2001. No clinical history of reproductive problems in the herds was obtained. All of the sampled cattle were more than 24 months old and female.
Serum was collected from people who visited Kangwon National University Hospital for health examinations between April and December 2002. The subjects were interviewed to confirm the absence of symptoms of respiratory tract infection during the preceding two weeks. All the sera were stored at -70℃ until tested.
Informed consent was obtained from all people for health screening and the animals are treated by the ethical guidelines of Kangwon National Univesity. This study was approved by the ethics committee of Kangwon National University Hospital.
Indirect microimmunofluorescence antibody (IFA) assay
Coxiella burnetii phase II antigen (Nine Mile whole-cell antigen) was prepared as previously described at the National Institute of Infectious Diseases (NIID) in Tokyo, Japan (12), and dotted onto Teflon-printed glass slides. Each serum sample was diluted 1:16 with phosphate-buffered saline (PBS), overlaid on the antigen dots, and incubated for 45 min at 37℃ in a moist chamber. The slides were subsequently washed twice for 5 min in PBS plus 0.05% Tween-20 and then incubated with a 1:1,400 dilution of fluorescein isothiocyanate (FITC)-conjugated rabbit anti-bovine IgG (Sigma-Aldrich, St. Louis, MO, U.S.A.) or FITC-conjugated rabbit anti-human IgG (DakoCytomation, Glostrup, Denmark) for 45 min at 37℃ in a moist chamber. The slides were again washed twice using the same method and examined using fluorescence microscopy (Axioskop 2, Zeiss, Germany) at 200× magnification. We considered a sample positive if the 1:32 serum dilution resulted in strong fluorescence. All sera that produced positive or equivocal reactions at 1:32 were further analyzed using 2-fold serial dilutions up to 1:4,096. The end point was the highest dilution showing complete fluorescence. Approximately 10% of the sera were divided and tested concurrently at Kangwon National University and at the NIID for quality control of test reproducibility; there was greater than 95% concordance between the results from the two laboratories.
RESULTS
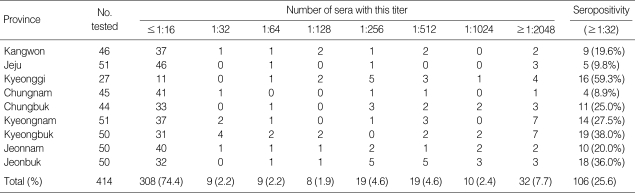
Table 1 shows the regional prevalence of antibodies against C. burnetii in dairy cattle. Each province had a relatively high prevalence, ranging from 8.9 to 59.3%; the overall national prevalence was 25.6%. Of the positive sera (n=106), 80 (75.5%) had high antibody titers (≥1:256).
Table 1.
Regional seroprevalence of antibodies against C. burnetii in dairy cattle
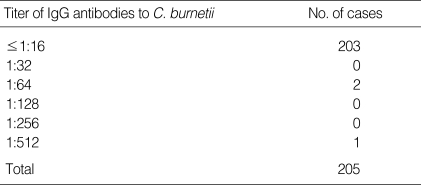
The mean age of the subjects was 43.7 yr (standard deviation 15.9, range 19-82), and the male-to-female ratio was 1:0.86 (n=110:95). Three (1.5%) of the 205 healthy people tested were seropositive. Of these, one had a serum sample with a high antibody titer (1:512), and two had samples with low antibody titers (1:64) (Table 2).
Table 2.
Presence of anti-C. burnetii antibodies in people for health screening (n=205)
DISCUSSION
This study examined the seroprevalence of C. burnetii infection in cattle and people for health screening in Korea. The sera of cattle showed a high prevalence (25.6%) of anti-C. burnetii antibodies, with 75.5% of the positive sera having high titers (≥1:256). By contrast, the sera of healthy people showed a relatively low prevalence (1.5%) of anti-C. burnetii antibodies.
The sera of dairy cattle were collected regardless of the disease status of each animal, which is a limitation of this study. Since we could not find an association between a history of reproductive failure and seropositivity of the cows because of the absence of the data on the disease status, no prediction concerning seropositive status and reproductive problems can be made. However, C. burnetii infection is prevalent in all areas of Korea; every region had a seroprevalence above 8%, and the national prevalence was 25.6%. Moreover, the high prevalence of high-titer sera provides evidence that the disease might be very active in this country. In neighboring Japan, the seroprevalence of C. burnetii in healthy cattle ranges from 2 to 46%; in cattle with reproductive disorders, the range was 60 to 84% (6). Bildfell et al. reported that bovine placentitis was highly associated with the presence of C. burnetti (13). In addition, 9% of abortions in goats are reported to be caused by this microorganism (14). This is the first report to provide data that suggest that C. burnetii infection might be one of the important causes of reproductive problems in cattle in Korea. Further studies based on the isolation of C. burnetii are needed to elucidate the etiologic role of this microorganism in the reproductive problems of cattle in this country. Furthermore, the high seroprevalence of C. burnetii among cattle suggests the possibility of contamination of the environment around farms. Since C. burnetii is widely distributed in wild animals and ticks and causes Q fever to humans (1, 3), it is necessary to evaluate the environmental hazards associated with C. burnetii infection that may threaten public health in the near future. In addition, the survey on the high-risk group such as farmers and butchers is strongly needed.
The finding that people in a rural area demonstrated a relatively low seroprevalence of C. burnetii, as well as lower titers, suggests that infection with this microorganism seems to be relatively low in the rural area of Korea. In a previously published report (11), less than 1% of both healthy people and patients with fever of unknown origin tested positive for anti-C. burnetii antibodies using an IFA assay. Another report showed none of the sera from 70 healthy people was reactive for C. burnetii antigen (15). Recent data showed that 11 out of 448 healthy people were reactive (16). With sera from acute febrile episode, 11.5% were reactive (17). On the other hand, our group previously reported that only one of 88 patients with community-acquired pneumonia was diagnosed with Q fever with an IFA assay using both phase I and II antigens (18).
Despite the low seroprevalence of C. burnetii in humans, we cannot exclude the risk of Q fever to individuals with high-risk occupations, such as farmers, veterinarians, and meat-processing workers, considering the high rate of infection observed in cattle in this study. Previous Korean report showed two of 46 stock breeders had an antibody titer of 1:20 (15), and 5 sera from 202 abattoir workers reacted with phase II antigen (16).
In conclusion, C. burnetii appears to be a highly prevalent pathogen in cattle in Korea and, accordingly, the studies on the high-risk groups are needed to evaluate the seroprevalence for this organism in Korea.
ACKNOWLEDGMENTS
The authors thank Dr. Won-Seo Park of the Clinical Research Institute of Kangwon National University Hospital for their useful advice and kind help with the quality control of the IFA test.
References
- 1.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laing-Brown G. Q fever. Brit Med J. 1973;2:43–45. doi: 10.1136/bmj.2.5857.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fournier PE, Marrie TJ, Raoult D. Diagnosis of Q fever. J Clin Microbiol. 1998;36:1823–1834. doi: 10.1128/jcm.36.7.1823-1834.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hilbink F, Penrose M, Kovacova E, Kazar J. Q fever is absent from New Zealand. Int J Epidemiol. 1993;22:945–949. doi: 10.1093/ije/22.5.945. [DOI] [PubMed] [Google Scholar]
- 5.Higgins D, Marrie TJ. Seroepidemiology of Q fever among cats in New Brunswick and Prince Edward Island. Ann N Y Acad Sci. 1990;590:271–274. doi: 10.1111/j.1749-6632.1990.tb42231.x. [DOI] [PubMed] [Google Scholar]
- 6.Hirai K, To H. Advances in the understanding of Coxiella burnetii infection in Japan. J Vet Med Sci. 1998;60:781–790. doi: 10.1292/jvms.60.781. [DOI] [PubMed] [Google Scholar]
- 7.Tissot-Dupont H, Raoult D, Brouqui P, Janbon F, Peyramond D, Weiller PJ, Chicheportiche C, Nezri M, Poirier R. Epidemiologic features and clinical presentation of acute Q fever in hospitalized patients; 323 French cases. Am J Med. 1992;93:427–434. doi: 10.1016/0002-9343(92)90173-9. [DOI] [PubMed] [Google Scholar]
- 8.Raoult D. Q fever: still a query after all these years. J Med Microbiol. 1996;44:77–78. doi: 10.1099/00222615-44-2-77. [DOI] [PubMed] [Google Scholar]
- 9.Kim KS, Lee WY. Coxiella burnetii infection in patients with various diseases. J Korean Pediatr Soc. 1994;37:356–367. [Google Scholar]
- 10.Park HS, Lee EG, Lee SY, Lyu CJ, Son YM, Kim DS, Kim KY. A case of Q fever: Association with pancytopenia, hepatitis, and myocarditis. Korean J Infect Dis. 1992;24:45–54. [Google Scholar]
- 11.Park YS, Lee KH, Park JY, Kim SK, Shin WS, Koh CM. Detection of antibodies to Coxiella burnetii antigen in the sera from residents in Korea. J Korean Soc Microbiol. 1994;29:333–339. [Google Scholar]
- 12.Williams JC, Peacock MG, McCaul TF. Immunological and biological characterization of C. burnetii, phase I and II, separated from host components. Infect Immun. 1981;32:840–851. doi: 10.1128/iai.32.2.840-851.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bildfell RJ, Thomson GW, Haines DM, McEwen BJ, Smart N. Coxiella burnetii infection is associated with placentitis in cases of bovine abortion. J Vet Diagn Invest. 2000;12:419–425. doi: 10.1177/104063870001200505. [DOI] [PubMed] [Google Scholar]
- 14.Moeller RB. Causes of caprine abortion: diagnostic assessment of 211 cases (1991-1998) J Vet Diagn Invest. 2001;13:265–270. doi: 10.1177/104063870101300317. [DOI] [PubMed] [Google Scholar]
- 15.Kim JM, Cho SN, Kim E, Kim HO, Chong Y, Kim JD, Hong CS. Prevalence of antibodies to Coxiella burnetii phase I antigen among Korean. Korean J Infect dis. 1993;25:103–109. [Google Scholar]
- 16.Jung KD, Jang WJ, Kim JH, Lee SH, Kim IS, Choi MS, Kim YW, Hwang YI, Park KH. Seroprevalence to Coxiella burnetii in patients with acute febrile episodes during 1993. J Bacteriol Virol. 2002;32:299–306. [Google Scholar]
- 17.Park MS, Park MY, Shin YO. Distribution of antibodies to Coxiella burnetii in patients with unknown fever and atypical pneumonia. J Bacteriol Virol. 2003;33:307–315. [Google Scholar]
- 18.Lee SJ, Lee MG, Jeon MJ, Jung KS, Lee HK, Kishimoto T. Atypical pathogens in adult patients admitted with community-acquired pneumonia in Korea. Jpn J Infect Dis. 2002;55:157–159. [PubMed] [Google Scholar]