Abstract
The aortic connector system may reduce stroke during proximal venous anastomosis. However, the overall anastomotic patency rate has been generally reported to be low. From October 2002 to March 2004, 68 patients who received proximal anastomosis using the St. Jude Aortic Connector System were included in the study. There were 47 men and 21 women and their mean age was 65.68±6.68 yr old (52 to 85 yr). Grafts were evaluated by coronary angiography or multi-slice 16 channel 3-D CT at 6 days and at 6 months postoperatively. In the immediate postoperative period, no stenosis was observed by either angiography (n=22) or 3D CT (n=46). At 6-month postoperatively, we performed either angiography (n=7) or 3-D CT (n=52). Of these patients, 5 patients showed graft stenosis in the midportion, and 3 in the ostium. There were no stroke. Simple, and effective proximal anastomosis with good protection from cerebrovascular accident was achieved especially when calcification or atheromatous plaque was observed at the ascending aorta in the operation room. However, our mid term patency results raise concerns related to venous graft stenosis in the midportion. Therefore, longer follow up is recommended.
Keywords: Coronary Artery Bypass, Aortic Connector System, Graft Stenosis
INTRODUCTION
Off-pump coronary artery bypass grafting (CABG) and minimally invasive coronary artery bypass have been widely applied as safe alternatives to conventional CABG by avoiding the possible undesirable effects associated with cardiopulmonary bypass and touching the atheromatous aorta. Traditionally a partial occluding clamp is placed on the ascending aorta and proximal anastomosis is achieved by hand-suturing the graft to a neo-ostium punched in the aortic wall during both on- and off-pump surgery. Hand suturing is an effective, standard technique to anastomose vein graft, but the quality of the anastomosis is depends on skill level, experience and the time permitted and furthermore manipulation of the aorta may exposes patients to possible embolization of the atheromatous debris from the aorta, as well as potential aortic dissection. Set against this background and growing interests in less invasive CABG techniques, semiautomatic devices that can facilitate proximal anastomosis without clamping the aorta have been developed.
The Aortic Connector System developed by St. Jude Medical Anastomotic Technology Group, Inc. (Minneapolis, MN, U.S.A.) has been used for years since approval of FDA of the United States was obtained in May 2001 for its use as alternative tools for proximal anastomosis (1). Some have reported early satisfactory results with this system comparable to those achieved using conventional method (2-5), however, others have reported early ostial saphenous vein graft stenosis (6-8).
In the present article, we review our initial experience and the mid-term results obtained using the Aortic Connector System (ACS; St. Jude Medical, Inc.) at the time of CABG and report some cases of venous graft stenosis in the mid portion which suggest the possibility of mechanical trauma to the endothelial lining which might be caused during saphenous vein loading onto the transfer sheath of the aortic connector.
MATERIALS AND METHODS
From October 2002 to March 2004, total 941 patients underwent CABG with or without cardiopulmonary bypass. Among these, 68 patients who received proximal anastomosis with the Symmetry Aortic connector were included in this study. We applied it whenever moderate to severe aortic calcification was observed in the preoperatively performed echocardiography or atherosclerotic plaque was palpable in operation field that did not allow to do side clamp. There were 47 men and 21 women and their mean age was 65.68±6.68 yr (52 to 85 yr). Sixty-two patients had three-vessel disease and six patients had two-vessel disease. The mean left ventricular ejection fraction was 53.4±13.2%.
All patients underwent CABG through a median sternotomy with or without cardiopulmonary bypass using the usual technique. 'On pump' surgery was performed in 21 patients and 'off pump' in 47 patients. The decision to use the bypass or not was made as each surgeon's preference.
The saphenous vein was harvested and its external diameter was assessed in 0.25 mm increments for matching with the most adequate size of the three different connector systems. It was introduced on the transfer sheath and then guided over the release system and was brought over the hooks of the connector with fine-tips forceps. Thus the ACS was loaded and prepared for deployment. During the loading procedure we used He-solution (a mix of verapamil and nitroglycerin at pH 7.0) for sufficient soaking (9-11). The aortic wall was punched out using a circular blade and an aortic cutter. The loaded ACS was then inserted into the aorta and the internal struts of the aortic connector were deployed, by pushing the button on the handle. The anastomosis was accomplished without side biting of the aorta. The procedure was concluded with a distal anastomosis. Intraoperative blood flows were assessed on all grafts using a Cardiomed Flowmeter (Medi-Stim, Oslo, Norway) based on the transit time principle.
Grafts were evaluated by coronary angiography or multislice 16 channel 3-D CT on the 6th postoperative days in all patients and at 6 months postoperatively in 59 patients. All patients received low dose warfarin, aspirin and plavix for 6 months and then the warfarin was discontinued.
RESULTS
There was no blood leak out of the proximal anastomotic site and no problem was encountered at device release. All patients received a left internal thoracic artery to revascularize the left anterior descending coronary artery, in 30 patients the radial artery was anastomosed as a T graft to the left internal mammary artery. A total of 70 vein grafts were used and all proximal vein graft anastomoses were done with the aortic connector system. Two vein grafts were anastomosed as T grafts to other vein grafts. 49 vein grafts were anastomosed to the posterior descending artery, 5 to a diagonal branch, 13 to an obtuse marginal, 14 to a postero-lateral branch. The mean vein loading time on the connector system was 6.5±1.0 min. All vein grafts were patent at the end of the procedure. Flow measurements were 95.05±2.96 mL/min for single vein grafts.
In the immediate postoperative period, no stenosis in the grafted saphenous vein was observed by either angiography (n=22) or 3D CT (n=46). 6 months follow up was done with 59 patients either by angiography (n=7) or by 3-D CT (n=52). Of these patients, five showed graft stenosis in the midportion (Fig. 1, 2) and three in the ostium (Fig. 3).
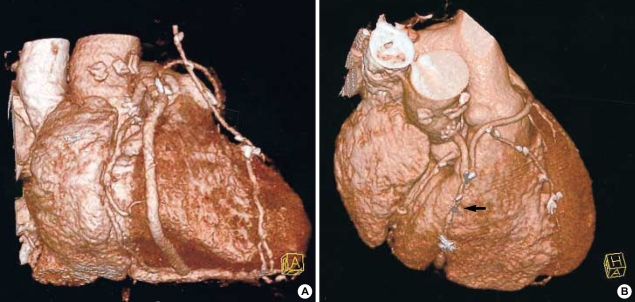
Fig. 1.
Serial images of 3-D CT at immediate and 6-months postoperatively in 65-yr old man. Note the patent saphenous vein including aortic connector site (A) and the severe stenosis in the midportion of the saphenous vein (arrow) (B). But proximal site is widely patent.
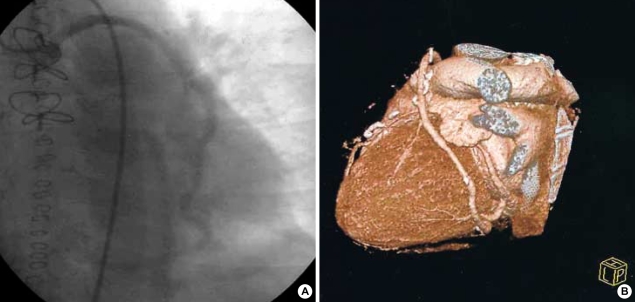
Fig. 2.
Immediate postoperative coronary angiogram (A) shows patent graft, whereas diffuse, but very mild narrowing in the mid-portion of graft is observed 6 months later on follow-up image (B).
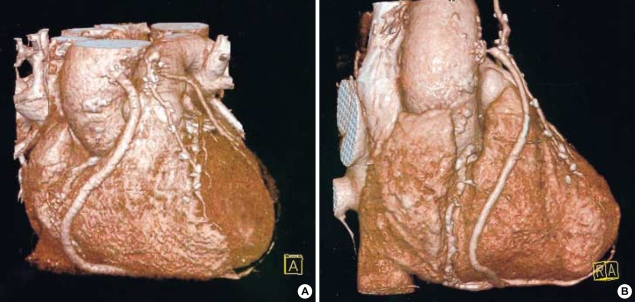
Fig. 3.
Severe proximal ostial graft narrowing is observed on 6-month follow-up images of a 75 yr old man (B), which is contrast to Fig. 1, 2 in that other portion of the graft is saved. However it was widely patent at the previous study (A).
No patients presented with postoperative neurologic complications such as stroke, delirium, and an impaired level of consciousness or with a major neuropsychological deficits or operative mortality. No patient was re-explored due to postoperative bleeding, and no complications such as acute renal failure, infection, perioperative myocardial infarction (PMI) occurred. As for the remaining 9 patients, 6 are waiting for their 6-month follow up study and 3 refused additional study due to lack of subjective symptoms.
DISCUSSION
Many patients undergoing CABG suffer from perioperative cerebrovascular events (1-5%) and neurocognitive dysfunction (33-83%) (12, 13). Moreover, it is well known that aortic manipulation and clamping may potentially cause plaque and debris embolization, leading to adverse neurologic outcomes. So availability of a sutureless proximal anastomotic device is viewed as having the potential to reduce procedural time and the risk of cerebral microemboli during CABG.
The symmetry bypass system was developed for the anastomosis of vein grafts to the aorta during CABG without manipulating the aorta and used in either on- or off-pump procedures. It consists of an aortic cutter and an aortic connector for attaching the proximal end of the vein graft to the aortotomy without using sutures. To use the system, the vein is loaded onto a transfer sheath of the aortic connector, guided to the end of the sheath where it is then pierced by several hooks around the vein graft circumference (1, 2). Previous studies have shown a mean loading time for the vein onto the aortic connector of 4.6-7.7 min with a device deployment time to complete mechanical anastomosis of less than 1 min (14). The Symmetry connector device thus has the potential to reduce operative time and perioperative neurologic sequelae.
Since gaining FDA approval in May 2001, more than 30,000 Symmetry Aortic Connector systems have been used and emerging reports have established safety of this device and the overall patency rates appear to be equivalent to historic suture-mediated anastomosis control although large randomized trials are lacking.
However, early bypass graft failures have been reported with some patients requiring redo CABG, or revascularization by percutaneous intervention and stenting (15). In addition there was also intraoperative fatal complications resulted in the deaths of two patients (7). Donsky and associates described two cases of acute thrombotic occlusion of the aortic ostia and hypothesized that this complication may have a similar pathophysiology to that of acute stent thrombosis (8). Carrel et al. also decided to interrupt the use of the Aortic Connector system for the following reasons. 1) The recruitment of the patients was difficult. 2) The rate of stenosis observed was not acceptable, similar to that observed in the early days of intracoronary stenting. 3) A new generation of St. Jude proximal connectors that eliminate the major disadvantages of the present device have been released for investigational purposes (14).
In immediate post-operative coronary angiograms or 3-D CT, we failed to observe evidence of connector site stenosis or occlusion, although these have been reported by others. However, in the 6-month follow-up study, we identified 3 cases of ostial saphenous vein graft stenosis and the graft stenosis in the midportion or in the entire length of the saphenous vein graft in 5 patients in which the ostial site was widely patent.
In order to use the aortic connector system, a saphenous vein must be harvested without any surrounding tissue, which has high collagen content and may thus act as a buffer against pulsatile stress with the adventitia. Tsui et al. suggested preservation of the adventitia as well as surrounding fat by harvesting with a 'no-touch' might improve vein graft patency with integrity of endothelium and nitric oxide synthase (15). Furthermore, saphenous vein, which is harvested with skeletonized pattern, would be slid over a transfer sheet thus facilitating the loading process on the release tube. At this point care must be taken to ensure that the vein is adequately humidified and that it is transferred smoothly.
The fate of bypassed graft depends on many factors, including technical faults in harvesting, handling and fashioning the conduits; thrombosis, myointimal hyperplasia, fibrosis and a rapidly progressing variety of atherosclerosis (16). And it is difficult to prove scientifically whether stenosis in the midportion was caused by endothelial damage during the manipulation of the saphenous vein before deploying or by the remodeling process according to native coronary artery flow, or by the progression of atherosclerosis of the grafted saphenous vein. And before concluding thrombotic complications were the direct results of one or more defects in the Symmetry system, several factors regarding a condition recognized to be a prothrombotic state of the each patient must be considered. However we cautiously hypothesize these observations may suggest possible mechanical trauma during disengagement of the delivery sheath and the deployment might cause endothelial damage in any portion of the loaded vein in which perivascular tissue had been already stripped off or at least it might facilitate the progression of the early graft intimal hyperplasia leading to graft failure. And to our knowledge, no reports have appeared describing the graft stenosis in the midportion with wide patent ostium since the introduction of ACS.
When the ACS is used, the proximal anastomosis must be performed first; that is not common to all surgeons. Furthermore a bulldog clamp has to be used to clamp the graft once the anastomosis has been performed. We also hypothesize this may damage the endothelium of the graft especially when the saphenous vein is clamped under arterial pressure.
Due to reports of early connector site stenosis or occlusion (6-8), we have started a very aggressive post-operative anti coagulation regimen. We used to start warfarin and an antiplatelet agent (aspirin and clopidogrel) for first 6 months to reduce the possibility of acute thrombosis at the proximal connector site and then discontinue coumadine and clopidogrel but continue aspirin. Even though the effect of the use of warfarin and clopidogrel on the absence of an early connector site stenosis in our study has to be more thoroughly evaluated, we understand that the pathophysiology of acute thrombosis at the proximal connector site may be similar to that seen in acute stent thrombosis (14). And we also observed 3 cases of ostial stenosis at the 6-month follow up, so, we would strongly recommend the use of warfarin and clopidogrel more aggressively postoperatively even more than 6 months.
The Symmetry aortic connector system has several potential advantages over the traditional suturing method. First, the time required to perform the anastomosis is reduced which might shorten recovery time. Second, minimizing aortic manipulation may reduce the risk of embolic events and thus reduce the incidence of neurologic complications (18, 19).
In this study we could not observe any neurologic problems in these patients whereas there were 1.5% cerebrovascular events in the other group of patients to whom we did not apply the ACS during the same period, although ACS was selectively used to the patients with pre-existing high risks.
However, although we assume that the potential benefits of the Symmetry device will outweigh the rare occurrences of device-related complications, when the ascending aorta is not diseased and until new safer anastomotic devices are introduced, we suggest the cautious use of it and will continue to prefer aortic side-clamping and hand-sewn anastomosis.
References
- 1.Mack MJ, Emery RW, Ley LR, Cole PA, Leonard A, Edgerton JR, Dewey TM, Magee MJ, Flavin TS. Initial experience with proximal anastomoses performed with a mechanical connetor. Ann Thorac Surg. 2003;75:1866–1871. doi: 10.1016/s0003-4975(03)00024-9. [DOI] [PubMed] [Google Scholar]
- 2.Calafiore AM, Bar-El Y, Vitolla G, Giammarco G, Teodori G, Iaco AL, D'Alessandro S, Mauro MD. Early clinical experience with a new sutureless anastomotic device for proximal anastomosis of the saphenous vein to the aorta. J Thorac Cardiovasc Surg. 2001;121:854–858. doi: 10.1067/mtc.2001.112829. [DOI] [PubMed] [Google Scholar]
- 3.Hornik L, Tenderich G, Minami K, Fassbender D, Schulz TO, Beinert B, Koerfer R. First experience with the St. Jude medical inc. Symmetry bypass system (Aortic Connector System) J Thorac Cardiovasc Surg. 2003;125:414–417. doi: 10.1067/mtc.2003.137. [DOI] [PubMed] [Google Scholar]
- 4.Eckstein FS, Bonilla LF, Englberger L, Immer FF, Berg TA, Schmidli J, Carrel TP. The St. Jude Medical symmetry aortic connector system for proximal vein graft anastomoses in coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2002;123:777–782. doi: 10.1067/mtc.2002.119695. [DOI] [PubMed] [Google Scholar]
- 5.Antona C, Scrofani R, Lemma M, Vanelli P, Mangini A, Danna P, Gelpi G. Assessment of an aortosaphenous vein graft anastomotic device in coronary surgery: clinical experience and early angiographic results. Ann Thorac Surg. 2002;74:2101–2105. doi: 10.1016/s0003-4975(02)04039-0. [DOI] [PubMed] [Google Scholar]
- 6.Traverse JH, Mooney MR, Pedersen WR, Madison JD, Flavin TF, Kshettry VR, Henry TD, Eales F, Joyce LD, Emery RW. Clinical, angiographic, and interventional follow-up of patients with aorticsaphenous vein graft connectors. Circulation. 2003;108:452–456. doi: 10.1161/01.CIR.0000080916.84077.C0. [DOI] [PubMed] [Google Scholar]
- 7.Lahtinen J, Biancari F, Mosorin M, Heikkinen J, Rainio P, Juvonen TS, Lepojarvi M. Fatal complications after use of the symmetry aortic connetor in coronary artery bypass surgery. Ann Thorac Surg. 2004;77:1817–1819. doi: 10.1016/S0003-4975(03)01291-8. [DOI] [PubMed] [Google Scholar]
- 8.Donsky AS, Schussler JM, Donsky MS, Roberts WC, Hamman BL. Thrombotic occlusion of the aortic ostia of saphenous venous grafts early after coronary artery bypass grafting by using the Symmetry aortic connector system. J Thorac Cardiovasc Surg. 2002;14:397–399. doi: 10.1067/mtc.2002.124236. [DOI] [PubMed] [Google Scholar]
- 9.He GW. Verapamil plus nitroglycerin solution maximally preserves endothelial function of the radial artery: Comparison with papaverine solution. J Thorac Cardiovasc Surg. 1998;115:1321–1327. doi: 10.1016/S0022-5223(98)70215-6. [DOI] [PubMed] [Google Scholar]
- 10.He GW, Yang CG. Use of verapamil and nitroglycerin solution in preparation of radial artery for coronary grafting. Ann Thorac Surg. 1996;61:610–614. doi: 10.1016/0003-4975(95)00920-5. [DOI] [PubMed] [Google Scholar]
- 11.Mussa S, Guzik TJ, Black E, Dipp MA, Channon KM, Taggart DP. Comparative efficacies and durations of action of phenoxybenzamine, verapamil/nitroglycerin solution, and papaverine as topical antispasmodics for radial artery coronary bypass grafting. J Thorac Cardiovasc Surg. 2003;126:1798–1805. doi: 10.1016/s0022-5223(03)00943-7. [DOI] [PubMed] [Google Scholar]
- 12.Eckstein FS, Bonilla LF, Englberger L, Immer FF, Berg TA, Schmidli J, Carrel TP. Minimizing aortic manipulation during OPCAB using the symmetry aortic connector system for proximal vein graft anastomoses. Ann Thorac Surg. 2001;72:995–998. doi: 10.1016/s0003-4975(01)02965-4. [DOI] [PubMed] [Google Scholar]
- 13.Endo M, Benhameid O, Morin JF, Shennib H. Avoiding aortic clamping during coronary artery bypass using an automated anastomotic device. Ann Thorac Surg. 2002;73:1000–1001. doi: 10.1016/s0003-4975(01)03444-0. [DOI] [PubMed] [Google Scholar]
- 14.Carrel TP, Eckstein FS, Englberger L, Windecker S, Meier B. Pitfalls and key lessons with the symmetry proximal anastomotic device in coronary artery bypass surgery. Ann Thorac Surg. 2003;75:1434–1436. doi: 10.1016/s0003-4975(02)04839-7. [DOI] [PubMed] [Google Scholar]
- 15.Tsui JC, Souza DS, Filbey D, Bomfim V, Dashwood MR. Preserved endothelial integrity and nitric oxide synthase in saphenous vein grafts harvested by a 'no-touch' technique. Br J Surg. 2001;88:1209–1215. doi: 10.1046/j.0007-1323.2001.01855.x. [DOI] [PubMed] [Google Scholar]
- 16.Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hopper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996;28:616–626. doi: 10.1016/0735-1097(96)00206-9. [DOI] [PubMed] [Google Scholar]
- 17.Cline SL, Guduvalli A, Kalaria VG. Early osteal saphenous vein graft stenosis associated with the use of symmetry sutureless aortic proximal anastomosis device: successful percutaneous revascularization. Catheter Cardiovasc Interv. 2004;62:203–208. doi: 10.1002/ccd.20048. [DOI] [PubMed] [Google Scholar]
- 18.Dewey TM, Crumrine K, Herbert MA, Leonard A, Prince SL, Worley C, Edgerton JR, Magee MJ, Mack MJ. First-year outcomes of beating heart coronary artery bypass grafting using proximal mechanical connetors. Ann Thorac Surg. 2004;77:1542–1549. doi: 10.1016/j.athoracsur.2003.09.047. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe G, Takemura H, Tomita S, Nagamine H, Kamiya H, Kanamori T. Skeletonized radial artery graft with the St. Jude medical symmetry bypass system (Aortic Connector System) Ann Thorac Surg. 2004;77:1550–1552. doi: 10.1016/j.athoracsur.2003.10.012. [DOI] [PubMed] [Google Scholar]