Abstract
This investigation evaluated the effect of continuous milrinone infusion on right ventriclular (RV) function during off-pump coronary artery bypass graft (OPCAB) surgery in patients with reduced RV function. Fifty patients scheduled for OPCAB, with thermodilution RV ejection fraction (RVEF) <35% after anesthesia induction, were randomly allocated to either milrinone (0.5 µg/kg/min) or control (saline) group. Hemodynamic variables and RV volumetric data measured by thermodilution method were collected as follows: after anesthesia induction (T1); 10 min after heart displacement for obtuse marginal artery anastomosis (T2); after pericardial closure (T3). Cardiac index and heart rate increased and systemic vascular resistance significantly decreased in milrinone group at T2. Initially lower RVEF of milrinone group was eventually comparable to control group after milrinone infusion. RVEF did not significantly change at T2 and T3 in both groups. RV end-diastolic volume in milrinone group consistently decreased from the baseline at T2 and T3. Continuous infusion of milrinone without a bolus demonstrated potentially beneficial effect on cardiac output and RV afterload in patients with reduced RV function during OPCAB. However, aggressive augmentation of intravascular volume seems to be necessary to maximize the effect of the milrinone in these patients.
Keywords: Milrinone; Ventricular Function, Right; Thermodilution; Coronary Artery Bypass, Off-pump
INTRODUCTION
Off-pump coronary artery bypass graft (OPCAB) surgery is now universally performed as an operative treatment of ischemic heart disease. Hemodynamic derangements ranging from mild to moderate hypotension to circulatory collapse can be induced by heart displacement to expose the target vessels for anastomosis. Several investigators have demonstrated that biventricular mechanical dysfunction contributes to the development of these consequences and an impaired right ventriclular (RV) function plays a pivotal role, especially during anastomosis of posterior branches (1-5). The patients with preoperatively reduced RV function could be prone to become hemodynamically unstable during OPCAB and supportive methods for RV can have beneficial hemodynamic effects. RV support by means of mechanical assist device was demonstrated to stabilize the hemodynamic profiles during heart displacements in an animal model (4). However, installation of such device may not be so feasible in patients with respect to the invasiveness and cost-effectiveness of the procedure.
Milrinone, phosphodiesterase III inhibitor, has been known to be an excellent inotropic agent with less myocardial O2 consumption than other sympathomimetics (6, 7) and to improve RV function and reduce pulmonary vascular resistance (PVR) in an animal model of pulmonary hypertension (8). Moreover, pharmacologic support with milrinone was also associated with an improved hemodynamic profile in patients undergoing OPCAB (9).
The aim of this investigation was to evaluate the effect of continuous milrinone infusion on hemodynamic profile and RV function, which were measured continuously with thermodilution pulmonary artery (PA) catheter during OPCAB in patients with reduced RV function.
MATERIALS AND METHODS
Patients' preparation
After institutional review board approval, this study was prospectively performed in 50 patients with right ventricular ejection fraction (RVEF) <35% measured by the thermodilution method and written informed consent was obtained from all patients. No patient with any of the following conditions was included; significant preoperative hepatic or renal dysfunction; thrombocytopenia or coagulopathy; supraventricular tachyarrhythmias; significant ventricular arrhythmias; preoperative history of receiving inotropic agents; single coronary artery disease. Originally, 96 patients who had been anticipated to have compromised RV function with elevated RV systolic pressure (>30 mmHg) measured by preoperative transthoracic echocardiography (10) were planned to be included in this investigation and randomly allocated to either milrinone or control group using sealed envelope system. Forty six patients demonstrated a thermodilution RVEF ≥35% after induction of anesthesia and were excluded and thus, 50 patients (24 in the control group and 26 in the milrinone group) were finally enrolled for this study.
Monitoring and anesthetic techniques
The patients were premedicated with intramuscular morphine 0.05-0.1 mg/kg given 1 hr before the induction of anesthesia. When the patient arrived in the operating theater, 5-lead electrocardiogram (ECG) electrodes were attached, and leads II and V5 with ST segment trend analysis were monitored. Direct arterial pressure monitoring was performed by 20-gauge radial artery cannulation. A thermodilution PA catheter (Swan-Ganz CCOmbo V CCO/SvO2/CEDV Model 775HF75®, Edwards Lifesciences, Irvine, CA, U.S.A.) was placed through the right internal jugular vein. The PA catheter was interfaced with the monitoring device (Vigilance®, Edwards Lifesciences, Irvine, CA, U.S.A.) and the Vigilance® monitor was also connected to the ECG signal output port of the patient monitor (CMS®, Hewlett-Packard, Andover, Mass., U.S.A.) with slave cable.
Anesthesia was induced with midazolam 2, 3 mg, sufentanil 1.5-2 µg/kg and rocuronium 0.6 mg/kg. After endotracheal intubation, ventilation was controlled artificially to maintain an end-tidal CO2 of 4.6-5.3 kPa. Anesthesia was maintained with continuous infusion of sufentanil 0.2-0.3 µg/kg/hr and intermittent inhalation of isoflurane 0.2-0.6% in medical oxygen/air mixture (FiO2 0.6). Vecuronium 2-4 mg/hr was infused to maintain muscle paralysis. After induction, isosorbide dinitrate 0.3-0.5 µg/kg/min was continuously infused throughout the operation. Transesophageal echocardiography (TEE) probe was inserted and both ventricular functions were continuously monitored. Central body temperature measured with PA catheter was tried to keep around 36.0℃. An average of 1,000-1,500 mL fluid was administered intravenously during graft vessel harvesting.
OPCAB techniques
After internal mammary artery dissection, heparin 1 mg/kg was given to maintain an activated clotting time (ACT) ≥250 sec during the anastomoses. To elevate the cardiac apex and expose the lateral wall, 2-cm-wide fabric tape was sutured to the posterior aspect of the pericardial reflection between the right and left pulmonary veins. With pericardial tape, the heart was displaced in various directions and angles along the target vessel for exposure. Tissue stabilizer (Octopus Tissue Stabilizing System®, Medtronic, Minneapolis, MN, U.S.A.) was applied to immobilize the target coronary territory. Anastomoses had been continuously performed without returning the heart to the neutral position. When the beating heart was displaced for anastomoses, the patient was placed in a 10-20° head-down tilt position and norepinephrine 0.03-0.05 µg/kg/min was given intermittently to maintain the mean arterial pressure (MAP) ≥60-65 mmHg. In case of left anterior descending (LAD) coronary artery anastomosis, an intracoronary shunt (Flo-Thru®, Synovis Innovations, St. Paul, MN, U.S.A.) was inserted to maintain downstream coronary flow but, other coronary branches were snared during anastomoses.
Collection of hemodynamic variables
After the induction of anesthesia, hemodynamic variables and RV volumetric data were collected as the baseline values (T1). These variables include heart rate (HR), MAP, mean pulmonary arterial pressure (MPAP), central venous pressure (CVP), pulmonary capillary wedge pressure (PCWP), cardiac index (CI), mixed venous saturation (SvO2), RVEF, stroke volume index (SVI), systemic and pulmonary vascular resistance indices (SVRI and PVRI, respectively), and RV end-diastolic and end-systolic volume indices (RVEDVI and RVESVI, respectively) which are displayed, calculated and indexed by the Vigilance® monitor. With these values, right ventricular stroke work index (RVSWI) was calculated. After sternotomy, infusion of milrinone 0.5 µg/min/kg (milrinone group) or the equivalent volume of saline (control group) was started and maintained throughout the OPCAB procedures. Nurses unconcerned in this study prepared solutions, and surgeons and anesthesiologists involved in this study were not aware of the patient's group until the end of the study. The variables were recorded 10 min after the displacement and immobilization of the heart with tissue stabilizer for obtuse marginal artery (OM) anastomosis (T2) and after pericardial closure (T3).
Statistic analysis
Values are expressed as the number of patients for discrete variables or mean±SD for continuous variables. Differences of discrete variables between the two groups were evaluated by χ2-test. Independent sample t-tests were performed to compare the continuous variables between the two groups at each time point. The changes of the variables from T1 within each group were evaluated by paired t-tests. A p<0.05 was considered statistically significant. To prevent increasing type I error from the repeated comparisons, Bonferroni's correction for multiple comparisons was performed where appropriate. Statistical software package running on a personal computer (SPSS 11.0, SPSS Inc., Chicago, IL, U.S.A.) was used for statistical analyses.
RESULTS
Demographic data
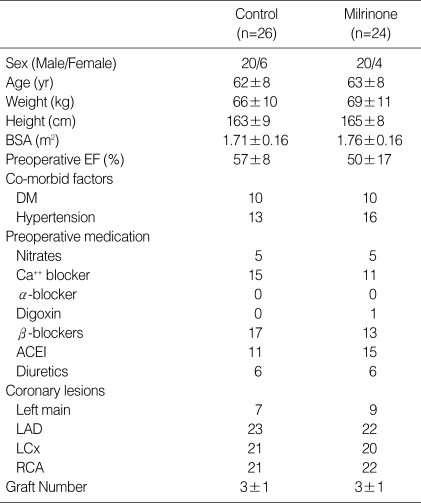
The two groups were not significantly different in the patients' characteristics (Table 1). All patients enrolled in this investigation successfully underwent OPCAB without emergent conversion to cardiopulmonary bypass and inotropic support other than milrinone.
Table 1.
Patients' characteristics
Data are expressed as number of patients or mean±SD.
BSA, body surface area; EF, ejection fraction; DM, diabetes mellitus; Ca++ blockers, calcium channel blockers; ACEIs, angiotensin-converting enzyme inhibitors; LAD, left anterior descending coronary artery; LCx, left circumflex artery; RCA, right coronary artery.
Comparisons of the variables between the two groups
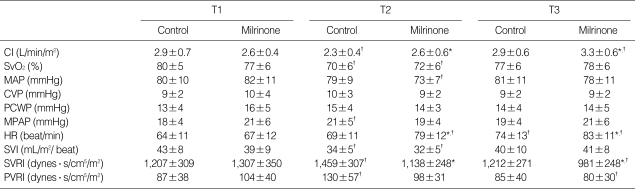
Alterations of hemodynamic variables and RV volumetric data during OPCAB procedures are shown in Table 2 and 3, respectively. After the induction of anesthesia (T1), the two groups were comparable in the whole variables, except that RVEF was lower in the milrinone group (p=0.015). CI and HR were higher and SVRI was lower in the milrinone group than the control group at T2 (p=0.013, 0.011 and 0.001, respectively) and T3 (p=0.009, 0.016 and 0.004, respectively). Remaining variables were comparable between the two groups at T2 and T3. The amounts of intravenous fluid infused, blood products transfused and the dose of norepinephrine infused during the surgery were comparable between the groups.
Table 2.
Alterations of hemodynamic variables during OPCAB
Data are expressed as mean±SD. *p<0.05, compared to Control; †p<0.05, compared to T1.
OPCAB, off-pump coronary artery bypass graft surgery; T1, after induction of anesthesia; T2, during obtuse marginal artery anastomosis; T3, after pericardial closure; CI, cardiac index; SvO2, mixed venous oxygen saturation; MAP, mean arterial pressure; CVP, central venous pressure; PCWP, pulmonary capillary wedge pressure; MPAP, mean pulmonary arterial pressure; HR, heart rate; SVI, stroke volume index; SVRI, systemic vascular resistance index; PVRI, pulmonary vascular resistance index.
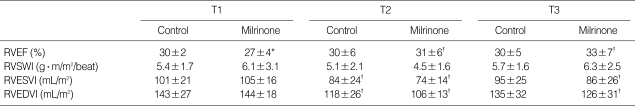
Table 3.
Alterations of RV volumetric data during OPCAB
Data are expressed as mean±SD. *p<0.05, compared to Control; †p<0.05, compared to T1.
OPCAB, off-pump coronary artery bypass graft surgery; T1, after induction of anesthesia; T2, during obtuse marginal artery anastomosis; T3, after pericardial closure; RVEF, right ventricular ejection fraction; RVSWI, right ventricular stroke work index; RVESVI, right ventricular end-systolic volume index; RVEDVI, right ventricular end-diastolic volume index.
Comparisons of the variables within each gr
CI reduced at T2 compared to T1 in control group, but it was comparable at T2 and increased at T3 from T1 in milrinone group. SvO2 and SVI reduced in both groups at T2 compared to values at T1. MAP was lower in milrinone group at T2 and MPAP was higher in control group compared to values at T1. HR increased in milrinone group at T2 and in both groups at T3 compared to values at T1. SVRI and PVRI increased in control group at T2, but reduced in milrinone group at T3 compared to values at T1. RVEF significantly increased in milrinone group at T2 and T3 compared to values at T1. RVSWI demonstrated no significant changes throughout the procedures in each group. RVESVI and RVEDVI decreased in control group at T2 and in milrinone group at T2 and T3 compared to values at T1.
During the procedures, no significant change was observed in ST segment analysis or cardiac rhythm. No newly developed regional wall motion abnormality and valvular insufficiency were seen on TEE during and after OPCAB procedures.
DISCUSSION
In the patients with reduced RV function, continuous infusion of milrinone during OPCAB improved CI and RVEF measured by thermodilution method. In regard to the RVEF, however, definite improvement over the control group was not observed in the milrinone group and it seemed to have resulted from inadequate preload augmentation.
Several investigations on animals and patients had revealed that RV dysfunction from mechanical compression was an important cause of the hemodynamic instability during OPCAB (1-5). The degree of heart displacement is often intensified when the vessels on the posterior aspect (e.g. OM artery) are exposed.
Milrinone, a well-known inodilator, had been demonstrated to decrease PVR and to improve RV function in both animal and human investigations (6-9, 11, 12). Therefore, milrinone was supposed to exert beneficial effects on RV hemodynamics in patients undergoing OPCAB in this study. Since the therapeutic responses to intravenous milrinone had been reported to partly depend on the pre-treatment hemodynamic status (13), patients with thermodilution RVEF <35% were selected and the hemodynamic variables were measured during OM anastomosis. Previously it was reported that RVEF and CI were reduced during OM anastomosis and the increase in RV afterload was discussed as the possible cause (14).
In this study, milrinone was obviously demonstrated to improve cardiac output during OM anastomosis as well as after completion of coronary anastomoses. Milrinone prevented PVRI increment that occurred in the control group during OM anastomosis and even reduced PVRI below the baseline value after pericardial closure. As RVEF is inversely correlated with RV afterload (15), RV function was expected to be improved in concordance with reduced RV afterload with milrinone. In fact, RVEF, which was significantly lower in the milrinone group than in the control group at baseline, increased to be comparable with that in the control group after milrinone infusion. Milrinone, however, failed to improve RVEF on that of the control group in this study and it was likely to be attributed to following factors. Firstly, the inadequate augmentation of RV preload in the milrinone group might contribute to the result. In spite of the relatively large amount of fluid administered and head-down tilt position, RVEDVI consistently reduced from the baseline after milrinone infusion. This, as well as the increased CO in the milrinone group, is presumed to be the result of the uncompensated vasodilatory effect of milrinone. Preload reduction would also be complicated with administration of nitrate agents with additive vasorelaxation effect (16). Given normal or near-normal RV afterload, preload is the determinant for the RV performance (17). Milrinone has been demonstrated to have beneficial hemodynamic effects only in heart failure patients with an adequate preload (18). Therefore, maintenance of sufficient intravascular volume seems to be crucial for beneficial effect of milrinone on RV function during OPCAB. Secondly, Gründeman et al. reported that RV dysfunction and concomitant hemodynamic instability are due to direct compression of the RV during coronary artery anastomosis (2). Thus, mechanical compression of the RV during anastomosis might be another limitation for milrinone to exert significant effect on RV function.
In this study, milrinone increased CI and reduced SVR, which might be associated with improved left heart function. Since left and right heart functions are closely related, improved left ventricular function with milrinone could affect RV function and the result of this study.
The thermodilution PA catheter used in the current investigation continuously measured RVEF and volumetric parameters. RVEF values measured by this catheter were approved to have significant reproducibility and correlation with other methods (19, 20). However, this parameter has limitations in monitoring RV function because RVEF is load-dependent. Significant alterations in RV preload would interfere with the efficacy of RVEF measured with the thermodilution catheter to evaluate RV function. TEE has been known to be an effective monitoring tool for wall motion and volume status in cardiac patients, (21) and employing additional echocardiographic indices could be more helpful to delineate the change of RV function with milrinone infusion. Monitoring RV function with TEE, however, during distal coronary anastomosis in every patient would be impossible because of displacement and elevation of the heart during that period.
To reduce the risk of hypotension, milrinone was infused without a bolus dose (9). Continuous infusion without a bolus was reported to demonstrate hemodynamic effects within 30 min from the start of infusion (22). In the present study, it took more than an hour to begin the coronary anastomosis after starting milrinone infusion and significant changes in hemodynamic parameters including CI, HR, SVRI and PVRI could be a proof of therapeutic plasma concentration of milrinone.
In conclusion, continuous infusion of milrinone was demonstrated to improve CI and RV afterload and have potentially beneficial effect on RV function in the patients with reduced RV function during OPCAB. Adequate augmentation of intravascular volume could be helpful to accomplish definite hemodynamic effect of milrinone administration in these patients.
Footnotes
This study was not supported by any research grants.
References
- 1.Grundeman PF, Borst C, van Herwaarden JA, Mansvelt Beck HJ, Jansen EW. Hemodynamic changes during displacement of the beating heart by the Utrecht Octopus method. Ann Thorac Surg. 1997;63:S88–S92. doi: 10.1016/s0003-4975(97)00339-1. [DOI] [PubMed] [Google Scholar]
- 2.Grundeman PF, Borst C, Verlaan CW, Meijburg H, Moues CM, Jansen EW. Exposure of circumflex branches in the tilted, beating porcine heart: echocardiographic evidence of right ventricular deformation and the effect of right or left heart bypass. J Thorac Cardiovasc Surg. 1999;118:316–323. doi: 10.1016/S0022-5223(99)70222-9. [DOI] [PubMed] [Google Scholar]
- 3.Nierich AP, Diephuis J, Jansen EW, Borst C, Knape JT. Heart displacement during off-pump CABG: how well is it tolerated? Ann Thorac Surg. 2000;70:466–472. doi: 10.1016/s0003-4975(00)01561-7. [DOI] [PubMed] [Google Scholar]
- 4.Porat E, Sharony R, Ivry S, Ozaki S, Meyns BP, Flameng WJ, Uretzky G. Hemodynamic changes and right heart support during vertical displacement of the beating heart. Ann Thorac Surg. 2000;69:1188–1191. doi: 10.1016/s0003-4975(99)01437-x. [DOI] [PubMed] [Google Scholar]
- 5.Mathison M, Edgerton JR, Horswell JL, Akin JJ, Mack MJ. Analysis of hemodynamic changes during beating heart surgical procedures. Ann Thorac Surg. 2000;70:1355–1360. doi: 10.1016/s0003-4975(00)01590-3. [DOI] [PubMed] [Google Scholar]
- 6.Kikura M, Levy JH, Michelsen LG, Shanewise JS, Bailey JM, Sadel SM, Szlam F. The effect of milrinone on hemodynamics and left ventricular function after emergence from cardiopulmonary bypass. Anesth Analg. 1997;85:16–22. doi: 10.1097/00000539-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Monrad ES, Baim DS, Smith HS, Lanoue AS. Milrinone, dobutamine, and nitroprusside: comparative effects on hemodynamics and myocardial energetics in patients with severe congestive heart failure. Circulation. 1986;73:III168–III174. [PubMed] [Google Scholar]
- 8.Chen EP, Bittner HB, Davis RD, Jr, Van Trigt P., 3rd Milrinone improves pulmonary hemodynamics and right ventricular function in chronic pulmonary hypertension. Ann Thorac Surg. 1997;63:814–821. doi: 10.1016/s0003-4975(97)00011-8. [DOI] [PubMed] [Google Scholar]
- 9.Kwak YL, Oh YJ, Shinn HK, Yoo KJ, Kim SH, Hong YW. Haemodynamic effects of a milrinone infusion without a bolus in patients undergoing off-pump coronary artery bypass graft surgery. Anaesthesia. 2004;59:324–331. doi: 10.1111/j.1365-2044.2004.03659.x. [DOI] [PubMed] [Google Scholar]
- 10.Feigenbaum H. Echocardiography. 5th ed. Philadelphia: Lea & Febiger; 1993. pp. 195–198. [Google Scholar]
- 11.Skoyles JR, Sherry KM. Pharmacology, mechanisms of action and uses of selective phosphodiesterase inhibitors. Br J Anaesth. 1992;68:293–302. doi: 10.1093/bja/68.3.293. [DOI] [PubMed] [Google Scholar]
- 12.Maslow AD, Regan MM, Schwartz C, Bert A, Singh A. Inotropes improve right heart function in patients undergoing aortic valve replacement for aortic stenosis. Anesth Analg. 2004;98:891–902. doi: 10.1213/01.ANE.0000107940.23783.33. [DOI] [PubMed] [Google Scholar]
- 13.Feneck RO The European Milrinone Multicentre Trial Group. Intravenous milrinone following cardiac surgery: II. Influence of baseline hemodynamics and patient factors on therapeutic response. J Cardiothorac Vasc Anesth. 1992;6:563–567. doi: 10.1016/1053-0770(92)90098-r. [DOI] [PubMed] [Google Scholar]
- 14.Kwak YL, Oh YJ, Jung SM, Yoo KJ, Lee JH, Hong YW. Change in right ventricular function during off-pump coronary artery bypass graft surgery. Eur J Cardiothorac Surg. 2004;25:572–577. doi: 10.1016/j.ejcts.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Burger W, Brinkies C, Illert S, Teupe C, Kneissl GD, Schrader R. Right ventricular function before and after percutaneous balloon mitral valvuloplasty. Int J Cardiol. 1997;58:7–15. doi: 10.1016/s0167-5273(96)02860-4. [DOI] [PubMed] [Google Scholar]
- 16.He GW, Yang CO, Gately H, Furnary A, Swanson J, Ahmad A, Floten S, Wood J, Starr A. Potential greater than additive vasorelaxant actions of milrinone and nitroglycerin on human conduit arteries. Br J Clin Pharmacol. 1996;41:101–107. doi: 10.1111/j.1365-2125.1996.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 17.Burger W, Jockwig B, Rucker G, Kober G. Influence of right ventricular pre- and afterload on right ventricular ejection fraction and preload recruitable stroke work relation. Clin Physiol. 2001;21:85–92. doi: 10.1046/j.1365-2281.2001.00300.x. [DOI] [PubMed] [Google Scholar]
- 18.Remme WJ, van Hoogenhuyze DC, Kruijssen HA, Pieper PG, Bruggeling WA. Preload-dependent hemodynamic effects of milrinone in moderate heart failure. Cardiology. 1992;80:132–142. doi: 10.1159/000174991. [DOI] [PubMed] [Google Scholar]
- 19.Vincent JL, Thirion M, Brimioulle S, Lejeune P, Kahn RJ. Thermodilution measurement of right ventricular ejection fraction with a modified pulmonary artery catheter. Intensive Care Med. 1986;12:33–38. doi: 10.1007/BF00315367. [DOI] [PubMed] [Google Scholar]
- 20.Urban P, Scheidegger D, Gabathuler J, Rutishauser W. Thermodilution determination of right ventricular volume and ejection fraction: a comparison with biplane angiography. Crit Care Med. 1987;15:652–655. doi: 10.1097/00003246-198707000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Chassot PG, van der Linden P, Zaugg M, Mueller XM, Spahn DR. Off-pump coronary artery bypass surgery: physiology and anaesthetic management. Br J Anaesth. 2004;92:400–413. doi: 10.1093/bja/aeh064. [DOI] [PubMed] [Google Scholar]
- 22.Baruch L, Patacsil P, Hameed A, Pina I, Loh E. Pharmacodynamic effects of milrinone with and without a bolus loading infusion. Am Heart J. 2001;141:266–273. doi: 10.1067/mhj.2001.111404. [DOI] [PubMed] [Google Scholar]