Abstract
Objectives
To characterize and assess sign-out practices among internal medicine house staff, and to identify contributing factors to sign-out quality.
Design
Prospective audiotape study
Setting
Medical wards of an acute teaching hospital
Participants
Eight internal medicine house staff teams
Measurements
Quantitative and qualitative assessments of sign-out content, clarity of language, environment, and factors affecting quality and comprehensiveness of oral sign-out.
Results
Sign-out sessions (N=88) contained 503 patient sign-outs. We collected complete written sign-outs accompanying 50/88 sign-out sessions (57%). Median duration of sign-out was 35 seconds (IQR 19–62) per patient. The combined oral and written sign-outs described clinical condition, hospital course and whether or not there was a task to be completed for 184/298 (62%) of patients. Least commonly conveyed was patient’s current clinical condition, described in 249/503 (50%) of oral sign-outs and 117/306 (38%) of written sign-outs. Most patient sign-outs (298/503, 59%) included no questions from the sign-out recipient (median 0, IQR 0–1). Five factors were associated with a higher rate of oral content inclusion: familiarity with the patient, sense of responsibility for the patient, only one sign-out per day, presence of a senior resident, and a comprehensive written sign-out. Omissions and mischaracterizations of data were present in 22% of sign-outs repeated in a single day.
Conclusions
Sign-outs are not uniformly comprehensive and include few questions. Our findings suggest that several changes may be required to improve sign-out quality, including standardizing key content, minimizing sign-outs that do not involve the primary team, templating written sign-outs, emphasizing the role of sign-out in maintaining patient safety, and fostering a sense of direct responsibility for patients among covering staff.
Introduction
Miscommunication during transfers of responsibility for hospitalized patients is common and can result in harm.1–9 Indeed, one fifth of malpractice claims against internal medicine house staff involve poorly-conducted transfers.7 Nonetheless, transfers in care are routine and becoming more frequent with resident work-hour restrictions.10 Growing awareness of problematic transfers has led to calls for improving the safety and efficacy of handoffs,11–17 including a requirement by the Joint Commission that institutions standardize handoff processes.18
Guidelines for safe and effective handoffs have now been proposed by some experts and organizations.19–25 These recommend that sign-outs include key content, are allotted adequate time for questions, clearly convey which patients are seriously ill or clinically unstable, be supervised by senior staff, include up-to-date information and take place in a quiet setting that minimizes distractions.19–25
Little is known about adherence to such recommendations in clinical practice because direct observation of oral and written sign-outs among physicians has rarely been performed. Furthermore, the degree of individual practice variability and the predictors of high quality sign-out are largely unknown. Direct observation of existing practices is needed in order to identify areas needing improvement, generate motivation for change and prioritize interventions. Accordingly, we conducted a mixed methods direct observation study to characterize and assess sign-out practices among internal medicine house staff.
Methods
Study design and sample
The design of this study has been previously described.5 Briefly, we audiotaped oral sign-outs conducted among 8 internal medicine house staff teams at one hospital over two periods in the spring of 2006, collected the accompanying written sign-outs, and interviewed all post-call and night float house staff the post-call morning. Sign-outs and interviews were transcribed and the transcripts redacted of identifying information. Teams comprised two residents and two interns. Each intern-resident pair was on call once every four days. During on-call days, one intern remained in the hospital overnight to care for all the patients on the team. Six teams employed a night float system; two did not (Figures 1 and 2).
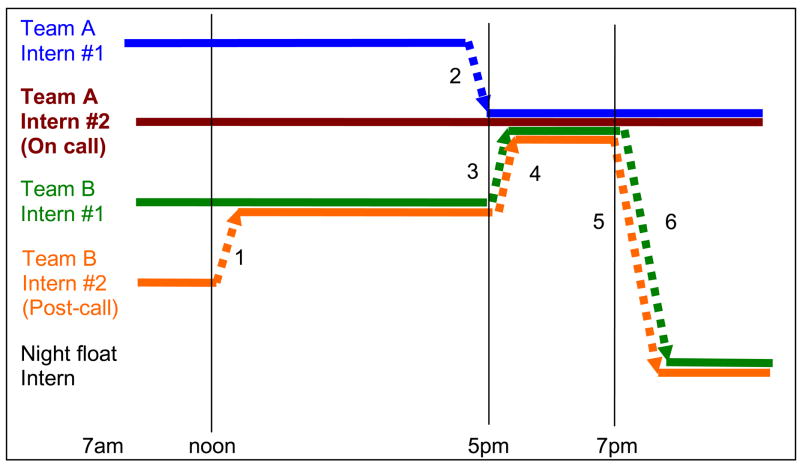
Figure 1.
Schema of weekday sign-out pattern for teams with night float. At the start of the day each intern cares for a group of patients, represented by a colored line. Each sign-out is numbered and is represented by a dotted line towards the intern receiving care of that group of patients. Approximate time of day at which each sign-out occurs is indicated along the bottom of the figure. At noon the post-call intern signs out to his or her co-intern. At 5pm the on-call intern receives sign-out from his or her co-intern, as well as from the two interns of his or her “sister team” (here, Team B). The on-call intern in turns signs-out some patients to the night float intern at 7pm. The tape recorder in this study was carried by the on-call intern. Thus sign-out #1, which did not involve the on-call intern, was not eligible for inclusion in the study.
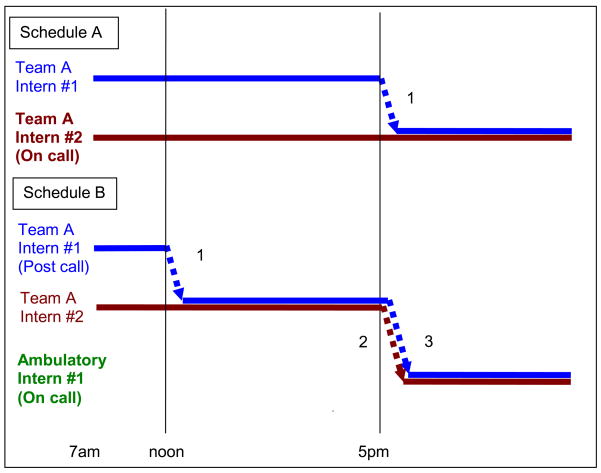
Figure 2.
Schema of weekday sign-out pattern for teams without night float. At the start of the day each intern cares for a group of patients, represented by a colored line. Each sign-out is numbered and is represented by a dotted line towards the intern receiving care of that group of patients. Approximate time of day at which each sign-out occurs is indicated along the bottom of the figure. On days when a member of the team is on call (Schedule A), one intern signs out patients to the on-call intern at about 5pm. On days when no members of the team are on call (Schedule B), an ambulatory intern arrives at 5pm to assume care of both interns’ patients, receiving two sign-out lists at that time. Earlier in the day, the post-call intern had signed out to the co-intern. The tape recorder in this study was carried by the on-call intern. Thus sign-out #1 in Schedule B, which did not include the on-call intern, was not eligible for inclusion in the study.
Like most U.S. hospitals,10 there was no sign-out curriculum or training for house staff. The Human Investigation Committee of Yale Medical School approved the study and granted a Health Insurance and Portability and Accountability Act waiver to permit audiotaping. Signed informed consent was obtained from all participating house staff and medical students.
Measures
We characterized sign-outs along three dimensions – content, clarity of language and surrounding environment – using both quantitative and qualitative analytic techniques. We also recorded the level of training of those present and the relationship of the sign-out provider to the patients (i.e. their own patients or a sister team’s patients).
We characterized content by measuring the prevalence in the written and oral sign-outs of recommended key elements: code status, current clinical condition, hospital course and tasks to complete.5, 19–25 Based on a separate analysis of problems resulting from these sign-out sessions, we also evaluated the prevalence of statements about anticipatory guidance and events to take place that night.5 For the subsets of patients where anticipatory guidance were provided or tasks were assigned, we measured the frequency with which plans of action and, separately, rationales were also provided.5 For example, “If he sundowns, what works best is trazodone 25, because he’s had adverse reactions to Haldol” was coded as an anticipatory guidance statement with both a plan and a rationale. We defined current clinical condition as any statement about the patient’s recent health state (vital signs, symptoms, physical examination findings, and laboratory values), stability (“doing fine,” “waiting for rehabilitation”) or trajectory (“improving”). We defined hospital course as any statement about events since admission, new events of the day or the duration of hospitalization.
At least two study investigators (T.M. and L.I.H. or L.W.) independently assessed the presence or absence of each key content item, coded as binary variables. Disagreements were resolved by negotiated consensus. Of 10 kappa scores calculated, 1 was below 0.5 (Kappa 0.47 for hospital course between two investigators), 4 were between 0.5 and 0.7, and 5 were above 0.7.
We qualitatively described language patterns of providers and recipients. We also quantified recipients’ repeat-back statements and questions. When calculating frequency of “repeat-back” behavior by sign-out recipients, we included every repetition, including summary statements such as, “So, basically, if anything happens, I’m going to call in GI and renal and the MICU.”
To evaluate the sign-out environment, we counted the number of interruptions by pagers or other staff that resulted in a break in the sign-out conversation. In addition, one investigator (L.I.H.) qualitatively assessed background as silent, having quiet background noise, having moderate background noise or having noise loud enough to interfere with conversation.
Analysis
We used descriptive statistics generated by SAS 9.1.2 (SAS Institute, Cary, North Carolina) to characterize quantitative outcome measures (key content inclusion, sign-out duration, interruptions, repeat-back statements and questions).
In order to assess important features of sign-out content and language patterns, and to explore factors affecting sign-out, we conducted a qualitative analysis. This analysis employed a mixed deductive-inductive approach26 and began with an initial code list based on previous studies of healthcare communication.1, 8, 27–33 At least two study investigators (T.M. and L.I.H. or L.W.) independently reviewed each transcript. After each transcript, these investigators met to review the transcripts and codes together, eliminating or refining codes as needed. Disagreements were resolved by negotiated consensus. We continued this process until thematic saturation had been achieved and no new codes were being generated. Each transcript was then independently recoded by two investigators using the final code structure and reviewed by the group, with disagreements resolved by consensus. We used Atlas.ti 5.0 (GmbH, Berlin, Germany) to facilitate qualitative analysis.
Two of the factors revealed by qualitative analysis to affect sign-out content and the amount of discussion among participants were the provider’s familiarity with patients and provider’s level of training (intern vs. resident). We converted these into quantitative predictors by scoring them as categorical variables. We then assessed the statistical association between these two factors and rates of sign-out content and discussion, using generalized models with provider as a random effect and the predictor of interest as a fixed effect to account for clustering of sign-outs within providers. All statistical tests were conducted using a two-tailed p value of .05 for significance.
Results
Study sample
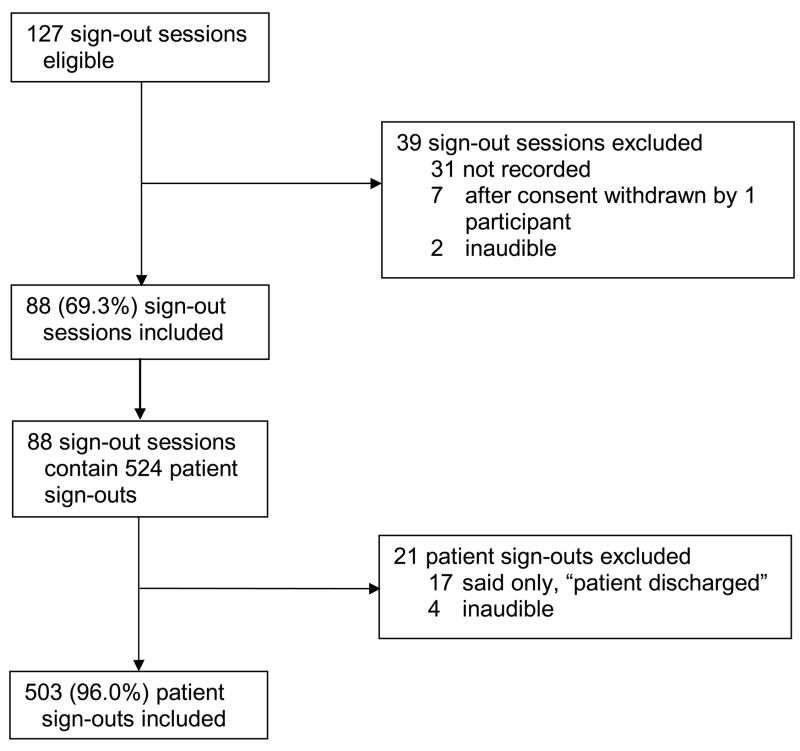
Our final study sample included 88 of 127 eligible sign out sessions (Figure 3). Twenty-four house staff conducted a mean of 3.7 ± 2.5 sign-out sessions each, and 20 house staff received a mean of 4.4 ± 4.3 sign-out sessions each. The sample included 503 individual patient sign-outs. We collected patient lists with handwritten addenda for 77/88 sign-out sessions (87.5%) and medication lists accompanying 53/88 sign-out sessions (60.2%); we obtained both for 50 of the 88 sign-out sessions (57%). We interviewed recipients of 84 of the 88 recorded sign-out sessions (95.5%). Characteristics of the study sample are shown in Table 1. A summary of the sign-out dimensions we assessed is shown in Table 2 and described in more detail in the following sections.
Figure 3.
Flow diagram of study participants
Table 1.
Characteristics of sign-out sessions
| Sign-out characteristics | Proportion of total sample (N=88) N (%) |
|---|---|
| Degrees of separation of sign-out from the primary team | |
| 0 (Within primary team) | 18 (20.5) |
| 1 (Primary team to sister team) | 34 (38.6) |
| 2 (Sister team to night float) | 36 (40.9) |
|
| |
| Relationship of provider to patients | |
| Own patients | 48 (54.6) |
| Another intern’s patients | 40 (45.4) |
|
| |
| Year of training of provider | |
| Sub-intern | 13 (14.7) |
| Intern | 58 (65.9) |
| Resident* | 17 (19.3) |
|
| |
| Gender of provider | |
| Male | 41 (46.6) |
| Female | 47 (53.4) |
|
| |
| Location of sign-out | |
| Conference room | 26 (29.6) |
| Nursing station | 37 (42.1) |
| Emergency department | 18 (20.5) |
includes any sign-out with resident present, even if not presenting information
Table 2.
Dimensions and range of sign-out processes
| Dimension | High quality | Low quality |
|---|---|---|
| Content | Comprehensive | Missing elements |
| Concise | Overshort or overlong | |
| Interactive | One-way | |
| Language clarity | More clear | Less clear |
| Concrete | Vague | |
| Closed-loop | Open-ended | |
| Environment | Quiet, no interruptions | Loud, numerous interruptions |
Sign-out content: Providers
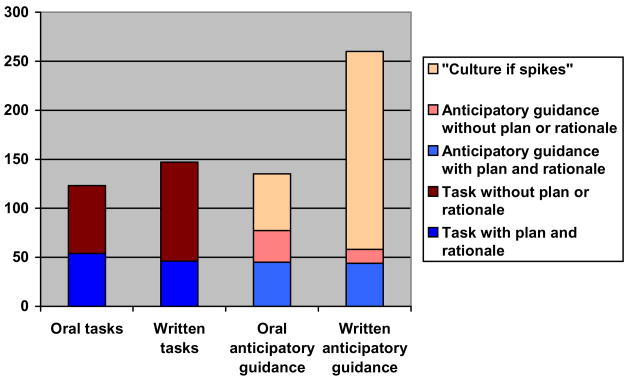
Oral sign-out sessions lasted a median of 245 seconds (IQR 154–373), or a median of 35 seconds per patient (IQR 19–62). Sign-outs typically did not contain the full range of key elements evaluated (Table 3). Figure 4 illustrates the frequency with which information about tasks to be performed and anticipatory guidance was provided in oral and written form.
Table 3.
Frequency with which content applicable to every patient was mentioned during patient sign-out
| Content | Oral or written (N=299) | Oral sign-out (N=503) N (%) | Written sign- out (N=299) N (%) |
|---|---|---|---|
| Whether or not there are any tasks to complete | 299 (100) | 351 (69.8) | 297 (99.3) |
| Code status | 291 (97.3) | 146 (29.0) | 291 (97.3) |
| Hospital course* | 281 (94.0) | 405 (80.5) | 241 (80.6) |
| Current clinical condition† | 200 (66.9) | 249 (49.5) | 116 (38.8) |
| Clinical condition AND hospital course AND whether tasks to complete | 186 (62.2) | 135 (26.8) | 91 (30.4) |
any description of any event occurring since hospitalization
any description of symptoms, vital signs, physical exam, laboratory/procedure results, or clinical stability
Figure 4.
Bar graph of information about tasks and anticipatory guidance presented in oral and written form. “Culture if spikes [a high temperature]” is a particular type of anticipatory guidance routinely hand-written on this institution’s written sign-out sheets.
Sign-outs did not have to be lengthy in order to be comprehensive. Appendix A shows a 42 second sign-out that included name, age, gender, code status, principal diagnosis, past medical history, hospital course, events of the day, medications, clinical condition and overnight tasks.
Sign-out content: Recipients
During the 503 oral patient sign-outs, recipients asked 363 clarifying questions, made 28 suggestions, expressed 9 disagreements, and provided 46 repeat-back statements. Most patient sign-outs (298/503, 59.2%) included no questions at all (median 0, IQR 0–1). For example, here the sign-out recipient accepts a brief sign-out about a potentially ill patient without probing for any information about the patient’s respiratory status, medication regimen or oxygen requirements:
[Provider]: “This woman is a new person with COPD exacerbation. Severe COPD. Not really much going on. The resident ordered ambulatory O2 sat, just to pass on to the tomorrow morning people, just so they know.”
[Recipient]: “OK.”
“But nothing to do.”
When recipients did express a disagreement or offer a suggestion, they typically did so only indirectly. In this example, an intern was receiving sign-out about a patient with an International Normalized Ratio (INR) of 12 and disagreed with the plan, which was to give fresh frozen plasma (FFP):
[Provider]: “So they’ve been giving her FFP, and then they have an 8pm INR. And she was on Coumadin for unknown reasons.”
[Recipient]: “Why are they giving her FFP? Is she bleeding?”
[Provider]: “She’s not, and I think it was so high that they wanted to reverse it. So, it really was really high when she… Let me see what it was exactly.”
[Recipient]: “That’s interesting, because FFP is not very long-lasting.”
[Provider]: “I don’t know why they… vitamin K might have been something that they could have done.”
[Recipient]: “Yeah.”
The recipient indicates her disagreement with the plan by saying gently, “That’s interesting,” rather than more overtly questioning the team’s judgment.
Clarity of sign-out language
We characterized sign-out language along a spectrum from least to most clear. Unclear language was vague, left decisions to the sign-out recipient, and/or did not specify who had responsibility for tasks. Clear language was concrete, was prescriptive about actions to be taken overnight, and/or clearly assigned responsibility for tasks.
These differing language styles were most evident during parts of sign-out that dealt with anticipatory guidance and tasks to be performed overnight. For example, one diabetic patient came in with hypoglycemia from a medication overdose. Her intern gave the following vague anticipatory guidance in oral and written form to the covering intern: “If the nurse calls you with increased sugars, can you start insulin?” In the absence of specific instructions, the covering intern decided upon a suboptimal regimen of a long-acting insulin without any as-needed bolus insulin.
Unclear language also did not convey an explicit assignment of responsibility, such as in these examples: “We just have to make sure he gets out of bed,” and “there’s a GI note.” Such ambiguity occasionally led recipients not to recognize an intended assignment. One resident, for example, signed out an alcoholic patient with tachycardia by commenting, “if [his anxiety] does seem more like withdrawal, please feel free to treat that as such” without assigning an explicit task such as, “please check on this patient tonight for signs of withdrawal.” The written sign-out further confused the picture by omitting the patient’s alcohol history and noting that the patient had received “0.5 mg of iv ativan for panic attack and increased HR.” There was no note of the possibility of withdrawal. The patient suffered an acute decompensation that night after going untreated for several hours.
By contrast, clear language was concrete, included detailed guidance and clearly assigned responsibility for actions, as in this example:
“And then his blood pressure, if it’s greater than 165/105, you can push 40 of iv labetalol or 10–20 of hydralazine iv. And then he has scheduled labetalol, and that should be given to him unless he’s really hypotensive, like less than 100/60 is what they’ve had.”
The instructions were also detailed on the written sign-out. The following morning the intern who received the sign-out specifically commented that
“[the patient] was hypertensive; I had good instructions in terms of how to handle that, and what the goals were… The additional information in terms of what to do with him was helpful.”
Recipients also used concrete, closed loop language patterns. For example, here a recipient clarifies who has responsibility to check results of a radiologic exam:
[Provider]: “Neck CT is ordered, and I guess it got done today. I didn’t see anything in the computer, but the neck CT is to - in the setting of cervical lymphadenopathy and a breast mass, concern for malignancy…”
[Recipient]: “OK. Is the neck CT something that needs follow-up?”
[Provider]: “No, I think it won’t change management tonight.”
Environment
Interruptions by staff (N=13) and answering pages (N=10) occurred in 17 sign-out sessions (19%). In those sessions with interruptions, the median was 1 (range 1 to 4). Background was generally quiet to moderately loud and we observed only one instance of background noise being overwhelming enough to interfere with the sign-out process.
Factors affecting oral sign-out content
Since written sign-outs were developed and passed on from person to person they usually remained similar for each sign-out session of the day. By contrast, oral sign-outs varied substantially from session to session. Analysis revealed five main factors affecting the content of oral sign-out and/or the amount of discussion among participants. These factors were: familiarity with patients, sense of responsibility for patients, sequential sign-outs, experience, and comprehensiveness of the written sign-out.
Familiarity with patients
Lack of familiarity with patients was correlated with an increased likelihood of content omissions by providers. Interns signing out other interns’ patients were significantly less likely to provide information about the patient’s current clinical condition (mean 43.2% of patients vs. 57.3%, p=.007), and were less likely to provide anticipatory guidance (0.42 statements per patient vs. 0.56, p=.02) compared with interns signing out their own patients. Similarly, interns signing out other interns’ patients were often uncertain about the information they did provide. For example, in this case an intern signing out a sister team’s patient is uncertain about the patient’s clinical condition and treatment:
“[The patient] presented with acute renal failure secondary to obstruction that’s resolved. And I think his renal status has resolved. I don’t know if he’s getting Flomax, probably something like that.”
Sense of responsibility
Sign-out recipients tended on the whole to defer to the primary team’s interpretations and plans rather than actively participate in managing care. Night float interns, for example, asked half as many questions about patients than interns receiving sign-out about patients on their own team (0.57 questions per patient vs. 1.24, p<.001). One factor in this conservativism was a sense among on-call physicians that they were “just covering,” rather than an integral part of the patient’s care. As a covering intern recounts in a post-call interview:
Intern: “I told [a family member with questions], could you please come [back] in the morning. I’m not your doctor, and I don’t have any idea of what they are going to talk about.”
Interviewer: “That must have been unsatisfying.”
Intern: “It was not unsatisfying. You know, I just told them that I’m covering for night, so I really don’t know what is the nature of the discussion.”
Sequential sign-outs
The night float system exacerbated unfamiliarity and limited responsibility because the night float arrived after the primary teams had already gone home. Patients were thus signed out first to an on-call intern, who shortly thereafter signed them out again to the night float intern. The on-call intern was typically not familiar with the patients and had little sense of primary responsibility for them; the same was true of the night float. Furthermore, in the second sign-out, providers had to recall and repeat information that had been rapidly presented in the sign-out hours earlier. Important clinical information from the first sign-out was omitted or mischaracterized in 46 of 211 second sign-outs – a rate of 22%.
These omissions and mischaracterizations were rarely recognized by sign-out recipients unless they resulted in patient harm. Several examples are shown in Table 4.
Table 4.
Omissions and mischaracterizations in sequential sign-outs
| Sequential sign-out problem | Representative example |
|---|---|
| Omission [in italics] |
First sign-out: “Mrs. [Name] is this woman that came in with… painless jaundice. And…she went and had an EUS today and they found a pancreatic mass. And so they did brushings, and stuff, of that. They were not able to stent it with ERCP. So a couple of things with her is that something happened during the procedure; they said submucosal contrast or something. And I don’t understand what that is, but they said if she has an increase in pain or spikes a fever, they said low threshold for CT of her belly and calling them. I started her on cipro iv and that’s it. She’s on clears.” Second sign-out: “Mrs. [Name]. She’s got obstructive jaundice. She was found to have a mass. They said it wasn’t able to be stented but I think they sent a biopsy. So there’s nothing to do tonight.” |
| Mischaracterization [in italics] |
First sign-out: “Mr. [Name]. He’s a patient with hemarthrosis, hemophilia. He’s been pretty stable painwise… So, it’s basically just pain control with some Dilaudid, 4q3.” Second sign-out: “Mr. [Name] is a 32-year old gentleman who came in with a hemarthrosis, I believe of his knee. So he’s been doing fine, hasn’t required any pain meds.” |
| Uncertainty |
[Provider]: “This person I don’t remember anything. It’s important that [the written sign-out] jogs my memory, because then I remember what I’m supposed to tell you. [reading from written sign-out] Alcohol abuse, intoxicated patient, fell, puncture wound on right side. With possible brachial plexus injury? I remember nothing, I’m sorry.” [Recipient]: “That’s ok.” [Provider]: “It looks like there’s nothing to do, but I’m sorry, I remember nothing about this patient.” [Recipient]: “OK. So it looks like he’s a high risk for withdrawing sometime today I guess?” [Provider]: “Yeah. OK. Sorry.” |
Experience and supervision
Sign-out sessions conducted in the presence of a senior resident differed in several ways from those that only included interns. For example, they were more likely to include information about patient’s current clinical condition (63.4% of patient sign-outs vs. 46.0%, p=.008) and to include a plan of action and a rationale with anticipatory guidance statements (58.1% of statements vs. 32.2%, p=.046). Of the key tasks recommended for sign-out, assessing the patient’s clinical condition and providing anticipatory guidance are perhaps most dependent on clinical experience. We did not observe any inhibitory effect of resident presence on willingness of junior staff to ask questions or express uncertainty. For example, sign-out recipients asked as many questions when there was a senior resident present as without (mean 0.66 with resident vs. 0.85 without, p=.38).
Written sign-out comprehensiveness
The content of the oral sign-out was also affected by the comprehensiveness of the written sign-out, which served as a cue and a memory aid. Incomplete written sign-outs were particularly problematic during sequential sign-out sessions, in which the providers did not know the patients and were more reliant on the written sign-out. In this example, the written sign-out includes just the patient’s name and demographic information, which proves unhelpful to the person providing the second sign-out of the day:
“Mr. [Name], I guess he’s a guy who’s been here for a while. [pause, flipping through written sign-out packet] He’s definitely been here a few times. [long pause] Yeah, I really don’t know the story on him.”
In this case the lack of information on the written sign-out contributed to a correspondingly incomplete oral sign-out.
Discussion
This study of oral and written sign-outs about medicine inpatients found that key clinical information was available just two thirds of the time in either the oral or written sign-out. Less than one third of oral patient sign-outs or written patient sign-outs included the minimum content of: the current clinical state of the patient, any description of the hospital course and a statement as to whether or not there were tasks to be performed overnight. Furthermore, vague and open-ended language was common, while 22% of sign-outs conducted in sequence mischaracterized or omitted information from the previous sign-out. Although in theory oral communication provides an opportunity for interactive dialogue to correct unclear or omitted information, in practice we observed that questions, suggestions, disagreements and read-back were relatively rare. These gaps in information flow during the sign-out process highlight the substantial potential for near misses and medical errors due to transfers of care.
An important feature of our data is that these content omissions were neither random, nor solely dependent on individual skill, but rather were systematically affected by broader structural and cultural conditions: the organization and infrastructure of the hospital, norms about autonomy and responsibility, and the collective understanding of the purpose of sign-out.
A major organizational factor in sign-out quality was the design of the coverage schedule to require two sequential sign-outs in the span of a few hours. This arrangement, a common response to the need to limit resident work hours,34 increased the complexity of the sign-out process and thus the opportunity for error.35 The sequential nature of the sign-outs also meant that sign-outs to the night float, who cared for the patient most of the night, were most often performed by covering physicians unfamiliar with the patients. Providers unfamiliar with patients they were signing out were less likely to include key clinical information than the patients’ primary team members, and were frequently unable to answer recipients’ questions.
The hospital’s information technology infrastructure also affected sign-out quality. Because the institution lacked a fully-templated written sign-out, some written sign-outs contained scant information. In turn, this reduced the comprehensiveness of the oral sign-out, which depended on the written sign-out as a memory aid. Both the night float system and the IT infrastructure were institutional-level factors that embedded obstacles to comprehensive information transfer in the sign-out process, despite great individual efforts to work around these obstacles (such as by providing detailed handwritten annotations every day to the computer-generated sign-out).
Organizational culture was no less important. At this institution, the norm was to have interns sign out without residents present. Consequently, most sign-out sessions did not incorporate senior residents’ greater clinical experience. When senior residents were involved, sign-outs were more likely to include important information such as the clinical condition of the patient. Finally, sign-out recipients were generally passive rather than active participants in patient care. This may have resulted from a culture of deference and reluctance to criticize colleagues36 combined with a misconception of sign-out as a one-way transfer of information, not as a moment to reflect critically upon the primary team’s diagnoses, actions and plans. The vulnerability of transitions to error was thus increased because recipients did not take full advantage of opportunities to clarify confusing statements, ask for plans or anticipatory guidance, and make suggestions.
Our direct observation study confirms results of earlier interview studies, which found that omitted content was common, language was unstructured and informal, written sign-outs were outdated, night float was problematic, and covering doctors were often uncertain about patient care decisions when covering overnight.1, 4, 8, 9, 27, 37–39 We did not, however, find evidence to support some contextual factors affecting communication that have been noted in other studies. Reluctance to criticize authority and a desire to impress more senior staff have been described as interfering with good sign-out communication.8 We did not observe any marked effect of hierarchy, perhaps because few sign-outs involved senior residents, and even these did not involve staff more than one or two years senior to interns. Likewise, high workload, interruptions and background distractions have been shown to interfere with good communication;8, 28 these were not evident factors in this analysis, perhaps because each sign-out session was relatively brief. Coiera and colleagues, for example, observed an interruption by call or page on average every 18.5 minutes;28 the average sign-out session in this study was less than 5 minutes.
Our study was limited by the nature of the observation; because we had only audiotapes, we were not able to capture non-verbal communication and cues that might have revealed other factors contributing to sign-out quality. In addition, several participants commented that the presence of the tape recorder led to more comprehensive sign-outs than were typical. The measures we used to measure quality were derived from a separate analysis of these data5 and expert opinion,19–25 and have not otherwise been proven to correlate with patient safety. The study was conducted at one institution in one specialty and may not be generalizable to other institutions, call structures, written sign-out formats and specialties. The timing of the study – late spring – meant both that interns had more experience, but also that residents were less often present to supervise. Finally, the limited number of sign-outs involving residents may have reduced our ability to observe effects of hierarchy and experience, and the limited number of interruptions prevented us from assessing the effect of environment.
Our findings have important implications for efforts to improve sign-out. Many recommendations for improving communication between providers focus on ensuring that sign-out includes key information.19–21 Information transfer is clearly lacking in current practice and efforts such as standardization of oral and written content are vital. Nonetheless, because multiple factors beyond individual performance affect the likelihood with which key information is included, focusing on individuals is not sufficient.40 Asking a sign-out provider always to mention the patient’s clinical condition, for example, is of limited value if 1) the provider is not familiar with the patient, 2) the provider lacks the clinical experience to recognize and transmit a worrisome change of condition and is not supervised by anyone with more experience, 3) the second in a series of providers forgets what the first one said because the night float system requires multiple handoffs in a row, or 4) the recipient does not demand the information when it is missing because cultural norms emphasize deference and prevent listeners from considering themselves an integral part of the patient’s care team. Thus, reducing structural and cultural obstacles to good sign-out will be important additions to existing efforts to standardize sign-out communication.24, 33, 41
Handoffs serve a number of purposes beyond the transfer of clinical information, including teaching, promotion of team cohesion, emotional support, socialization, maintenance of social order, and error detection.29–31, 42, 43 On occasion these goals conflict, as when promotion of team cohesion is prioritized over error detection, so questioning is discouraged. Yet the multitude of purposes served by sign-out is also an advantage. The socialization and training aspects of sign-out, for example, could be harnessed to foster the development and maintenance of a sign-out culture that prioritizes and enhances patient safety.39 The team-building component of sign-out could be reconfigured from a model in which the sign-out recipient is someone who just “holds the fort,” to a model in which all sign-out participants are equal members of a team bearing equal responsibility for the patient. Such a reframed sign-out culture would help promote a “new” professionalism, defined not as the duty to stay with the patient at all times but as the duty to ensure the best care for the patient no matter who is in the hospital.16
Conclusion
In summary, we found that sign-outs are not uniformly comprehensive and often include problematic communication styles. The quality of sign-out communication is affected by social relationships among providers, a sense of responsibility for patients, familiarity with patients, participants’ clinical experience, and the sequential nature of many sign-outs. To improve quality, not only should key information be systematically included, but sign-outs that do not involve the primary team should be minimized, written sign-outs should be templated, the role of sign-out in maintaining patient safety should be emphasized, and a sense of direct responsibility for patients should be fostered among covering staff.
Acknowledgments
Dr. Horwitz was affiliated with the Robert Wood Johnson Clinical Scholars Program and was supported by the Department of Veterans Affairs during the time the work was conducted. Dr. Bradley is supported by the Catherine and Patrick Donaghue Medical Research Foundation Investigator award. Neither the Department of Veterans Affairs, the Catherine and Patrick Donaghue Medical Research Foundation, nor the Robert Wood Johnson Foundation had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review and approval of the manuscript. Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank the house staff who agreed to participate in the study.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in QSHC and any other BMJPGL products to exploit all subsidiary rights, as set out in our licence (http://qhc.bmj.com/ifora/licence.pdf)
Biography
Dr. Horwitz was affiliated with the Robert Wood Johnson Clinical Scholars Program and was supported by the Department of Veterans Affairs during part of the time this work was conducted. Dr. Bradley is supported by the Catherine and Patrick Donaghue Medical Research Foundation Investigator award.
References
- 1.Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–407. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (in-hospital handover of care): a prospective survey. Qual Saf Health Care. 2008;17:6–10. doi: 10.1136/qshc.2006.019273. [DOI] [PubMed] [Google Scholar]
- 3.Chassin MR, Becher EC. The wrong patient. Ann Intern Med. 2002;136:826–833. doi: 10.7326/0003-4819-136-11-200206040-00012. [DOI] [PubMed] [Google Scholar]
- 4.Gandhi TK. Fumbled handoffs: one dropped ball after another. Ann Intern Med. 2005;142:352–358. doi: 10.7326/0003-4819-142-5-200503010-00010. [DOI] [PubMed] [Google Scholar]
- 5.Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. Consequences of inadequate sign-out for patient care. Arch Intern Med. 2008;168:1755–1760. doi: 10.1001/archinte.168.16.1755. [DOI] [PubMed] [Google Scholar]
- 6.Shojania KG, Fletcher KE, Saint S. Graduate medical education and patient safety: a busy--and occasionally hazardous--intersection. Ann Intern Med. 2006;145:592–598. doi: 10.7326/0003-4819-145-8-200610170-00008. [DOI] [PubMed] [Google Scholar]
- 7.Singh H, Thomas EJ, Petersen LA, Studdert DM. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167:2030–2036. doi: 10.1001/archinte.167.19.2030. [DOI] [PubMed] [Google Scholar]
- 8.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79:186–194. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Williams RG, Silverman R, Schwind C, et al. Surgeon information transfer and communication: factors affecting quality and efficiency of inpatient care. Ann Surg. 2007;245:159–169. doi: 10.1097/01.sla.0000242709.28760.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166:1173–1177. doi: 10.1001/archinte.166.11.1173. [DOI] [PubMed] [Google Scholar]
- 11.Gosbee J. Communication among health professionals. BMJ. 1998;316:642. doi: 10.1136/bmj.316.7132.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mukherjee S. A precarious exchange. N Engl J Med. 2004;351:1822–1824. doi: 10.1056/NEJMp048085. [DOI] [PubMed] [Google Scholar]
- 13.Okie S. An elusive balance--residents’ work hours and the continuity of care. N Engl J Med. 2007;356:2665–2667. doi: 10.1056/NEJMp078085. [DOI] [PubMed] [Google Scholar]
- 14.Philibert I, Leach DC. Re-framing continuity of care for this century. Qual Saf Health Care. 2005;14:394–396. doi: 10.1136/qshc.2005.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sithamparanathan M. That’s all I got handed over. BMJ. 2006;332:496. [Google Scholar]
- 16.Van Eaton EG, Horvath KD, Pellegrini CA. Professionalism and the shift mentality: how to reconcile patient ownership with limited work hours. Arch Surg. 2005;140:230–235. doi: 10.1001/archsurg.140.3.230. [DOI] [PubMed] [Google Scholar]
- 17.Stevens DP. Handovers and Debussy. Qual Saf Health Care. 2008;17:2–3. doi: 10.1136/qshc.2007.025916. [DOI] [PubMed] [Google Scholar]
- 18.Joint Commission on Accreditation of Healthcare Organizations. [Accessed June 3, 2007];Critical Access Hospital and Hospital National Patient Safety Goals. 2007 http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/07_hap_cah_npsgs.htm.
- 19.British Medical Association, National Patient Safety Agency, NHS Modernisation Agency. Safe handover: safe patients. London, UK: British Medical Association; 2004. [Google Scholar]
- 20.University HealthSystem Consortium. UHC Best Practice Recommendation: Patient Hand Off Communication: White Paper. Oak Brook, IL: UHC; 2006. [Google Scholar]
- 21.McKean SCW. The Core Competencies in Hospital Medicine: Patient Handoff. J Hosp Med. 2006;1:83. doi: 10.1002/jhm.6. [DOI] [PubMed] [Google Scholar]
- 22.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80:1094–1099. doi: 10.1097/00001888-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257–266. doi: 10.1002/jhm.103. [DOI] [PubMed] [Google Scholar]
- 24.Horwitz LI, Moin T, Green ML. Development and Implementation of an Oral Sign-out Skills Curriculum. J Gen Intern Med. 2007;22:1470–1474. doi: 10.1007/s11606-007-0331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arora VM, Farnan JM. Care transitions for hospitalized patients. Med Clin North Am. 2008;92:315–324. viii. doi: 10.1016/j.mcna.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 27.Bomba DT, Prakash R. A description of handover processes in an Australian public hospital. Aust Health Rev. 2005;29:68–79. doi: 10.1071/ah050068. [DOI] [PubMed] [Google Scholar]
- 28.Coiera E, Tombs V. Communication behaviours in a hospital setting: an observational study. BMJ. 1998;316:673–676. doi: 10.1136/bmj.316.7132.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelly R. Goings-on in a CCU: an ethnomethodological account of things that go on in a routine hand-over. Nurs Crit Care. 1999;4:85–91. [PubMed] [Google Scholar]
- 30.Kerr MP. A qualitative study of shift handover practice and function from a socio-technical perspective. J Adv Nurs. 2002;37:125–134. doi: 10.1046/j.1365-2648.2002.02066.x. [DOI] [PubMed] [Google Scholar]
- 31.Lally S. An investigation into the functions of nurses’ communication at the inter-shift handover. J Nurs Manag. 1999;7:29–36. doi: 10.1046/j.1365-2834.1999.00095.x. [DOI] [PubMed] [Google Scholar]
- 32.Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13:330–334. doi: 10.1136/qshc.2003.008425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16:125–132. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 34.Yoon P, Steiner I, Reinhardt G. Analysis of factors influencing length of stay in the emergency department. Cjem. 2003;5:155–161. doi: 10.1017/s1481803500006539. [DOI] [PubMed] [Google Scholar]
- 35.Woods DD, Hollnagel E. Joint cognitive systems: Patterns in cognitive systems engineering. Boca Raton, FL: Taylor & Francis; 2006. [Google Scholar]
- 36.Eisenberg EM, Murphy AG, Sutcliffe KM, et al. Communication in emergency medicine: implications for patient safety. Communication Monographs. 2005;72:390–413. [Google Scholar]
- 37.Beach C, Croskerry P, Shapiro M. Profiles in patient safety: emergency care transitions. Acad Emerg Med. 2003;10:364–367. doi: 10.1111/j.1553-2712.2003.tb01350.x. [DOI] [PubMed] [Google Scholar]
- 38.Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents Report on Adverse Events and Their Causes. Arch Intern Med. 2005;165:2607–2613. doi: 10.1001/archinte.165.22.2607. [DOI] [PubMed] [Google Scholar]
- 39.Arora VM, Johnson JK, Meltzer DO, Humphrey HJ. A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care. 2008;17:11–14. doi: 10.1136/qshc.2006.018952. [DOI] [PubMed] [Google Scholar]
- 40.Patterson ES. Structuring flexibility: the potential good, bad and ugly in standardisation of handovers. Qual Saf Health Care. 2008;17:4–5. doi: 10.1136/qshc.2007.022772. [DOI] [PubMed] [Google Scholar]
- 41.Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf. 2006;32:167–175. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- 42.Behara R, Wears RL, Perry SJ, et al. Agency for Healthcare Research and Quality. Advances in Patient Safety: From Research to Implementation. Vol. 2. Rockville, MD: AHRQ; 2005. A conceptual framework for studying the safety of transitions in emergency care; pp. 309–321. [PubMed] [Google Scholar]
- 43.Sherlock C. The patient handover: a study of its form, function and efficiency. Nurs Stand. 1995;9:33–36. doi: 10.7748/ns.9.52.33.s34. [DOI] [PubMed] [Google Scholar]