Abstract
Although abdominal bloating is one of the most bothersome symptoms experienced by patients with functional dyspepsia (FD), therapeutic drugs to relieve abdominal bloating have not been established. We investigated the Kampo (Chinese herbal) medicine, Hangekobokuto (Banxia-houpo-tang, HKT) for patients with FD from the standpoint of bowel gas retention. The bowel gas volume calculated from a plain abdominal radiogram (gas volume score, GVS) in FD patients was significantly higher than that in healthy subjects. Two week administration of HKT in the FD patients showed a significant decrease of GVS. Furthermore, gastrointestinal symptoms, especially symptoms of abdominal pain, indigestion and constipation, all of which are closely related to abdominal bloating, improved significantly in FD patients after the administration of HKT. These results suggest that HKT improves abdominal bloating accompanied by the reduction of bowel gas in FD patients.
Keywords: abdominal bloating, aerophagia, functional dyspepsia, functional gastrointestinal disorders, herbal medicine, prokinetics
Introduction
Functional dyspepsia (FD) is one of the most common diseases in advanced countries (1–3). Among the various gastrointestinal symptoms FD causes (4–6), abdominal bloating is one of the most bothersome. Several factors, such as bowel gas retention and abnormal sensitivity of the intestinal wall, are considered to play a role in making patients experience the sensation of abdominal bloating (7). However, the exact pathogenesis is still not clear, and therapeutic drugs to relieve the complaint have thus not yet been established.
To date, many Kampo medicines have shown efficacy for the relief of symptoms in dyspeptic patients (8). Rikkunshito was proved to be effective against FD by double-blind RCT for the first time. In an earlier study, we reported that Hangekobokuto (Banxia-houpo-tang, HKT) increased the gastric emptying rate in FD patients, and that gastrointestinal symptoms improved significantly, suggesting that HKT acts as a prokinetic agent (9).
We investigated HKT for patients with FD from the standpoint of bowel gas retention, because HKT is classically considered one of the representative formulations to improve abdominal bloating, which includes an excess of abdominal gas in its pathophysiology.
Methods
Subjects
Twenty asymptomatic healthy volunteers [all men, mean age 35.4 years (26–49)] and 30 patients with FD [12 men and 18 women, mean age 54.5 years (25–85)] were enrolled. HKT was evaluated for bowel gas in 20 healthy volunteers and 19 [6 men and 13 women, mean age 50.2 years (25–85)] of the 30 FD patients. The diagnosis of FD was determined on the basis of international criteria (6). All the FD patients were classified as ‘post-prandial distress syndrome’. None of the participants used medication that could affect gastrointestinal motility for over 2 weeks before the examinations. All participants provided informed consent before participating in this study.
Preparation of HKT
HKT is composed of the five drugs shown in Table 1. We used freeze-dried extracts of HKT, TJ-16 (Tsumura Co., Tokyo, Japan) and the three-dimensional HPLC profile of the methanol solution of TJ-16 described previously (7). The daily dose for adults is 7.5 g, and was administered orally three times a day before each meal.
Table 1.
Constituents of Hangekobokuto
| Pinelliae tuber | 6 g |
| Hoelen | 5 g |
| Magnoliae cortex | 3 g |
| Perillae herba | 2 g |
| Zingiberis rhizoma | 1 g |
Study Protocol
We administered HKT to patients with FD, as well as to healthy subjects for 2 weeks. Before and after this administration, we evaluated bowel gas volume calculated from a plain abdominal radiogram (10). Briefly, plain abdominal radiographs in the supine position taken in the fasting state in the morning were digitized and transmitted to the computer. After the region of bowel gas was identified, its outline was traced on the monitor. The total area for the region of bowel gas (gas in stomach was excluded) was determined as the pixel value on images by using Scion Image Beta version 4.02. The ratio of the quantity of bowel gas to the pixel value in the region surrounded by a horizontal line tangential to the suprasymphysary margin, a horizontal line tangential to the uppermost diaphragm and the most lateral line tangential to the right and left costal arches was defined as GVS. We also assessed the gastrointestinal symptoms of the FD patients using the gastrointestinal symptom rating scale (GSRS) as a questionnaire (11). Our protocol was approved by the ethical committee in Oriental Medicine Research Center of the Kitasato Institute.
Statistical Analysis
Data were expressed as mean ± SE. The statistical significance of the differences between measurements made before and after the administration of HKT was assessed using the Wilcoxon signed rank test, and differences between the two groups were assessed using the Mann–Whitney U-test. A P-value <0.05 was regarded as significant.
Results
HKT Decreases GVS in FD Patients but not in Healthy Subjects
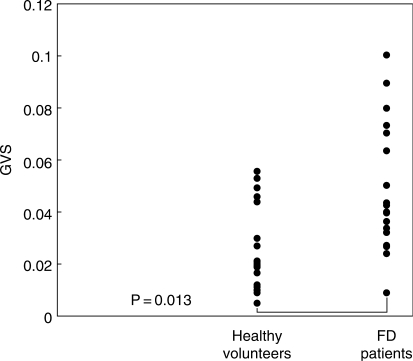
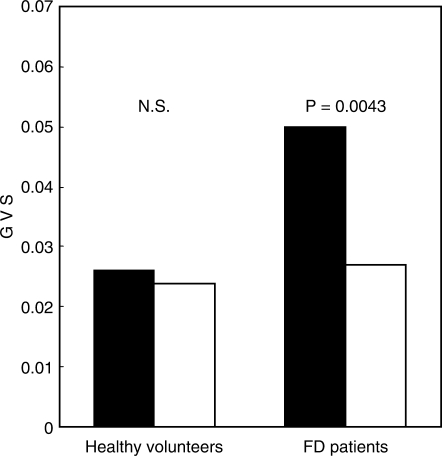
The GVS in FD patients (0.050 ± 0.006) was significantly higher than that in the healthy subjects (0.026 ± 0.004) (Fig. 1). The GVS in FD patients showed a significant decrease (0.027 ± 0.005) after 2 weeks of medication with HKT. In contrast, there was no significant change (0.024 ± 0.003) in the GVS of the healthy volunteers (Fig. 2).
Figure 1.
Comparison of gas volume score (GVS) between healthy volunteers and patients with functional dyspepsia (FD).
Figure 2.
Effect of Hangekobokuto on gas volume score (GVS) of healthy volunteers and patients with functional dyspepsia (FD). Black columns: mean GVS before administration of HKT. White columns: mean GVS after administration of HKT.
HKT Improves Gastrointestinal Symptoms in FD Patients
The gastrointestinal symptoms of FD patients as expressed by the GSRS total score showed significant improvement after HKT treatment (from 2.48 ± 0.14 to 2.08 ± 0.11, P = 0.0019). The GSRS symptom scores for five categories except diarrhea also showed a significant decrease, especially in the score for indigestion with high positivity (Table 2).
Table 2.
Changes in gastrointestinal symptoms of patients with functional dyspepsia after administration of Hangekobokuto
| GSRS score |
|||
|---|---|---|---|
| Before | After | P-value | |
| Total | 2.48(±0.14) | 2.08(±0.11) | 0.0019 |
| Reflux | 2.53(±0.24) | 1.98(±0.15) | 0.0090 |
| Abdominal pain | 2.35(±0.17) | 2.00(±0.14) | 0.0090 |
| Indigestion | 2.80(±0.23) | 2.34(±0.22) | 0.00056 |
| Diarrhea | 1.75(±0.17) | 1.58(±0.17) | NS |
| Constipation | 2.81(±0.25) | 2.33(±0.18) | 0.017 |
GSRS, gastrointestinal symptom rating scale.
Discussion
We demonstrated that the Kampo medicine HKT reduces bowel gas and improves gastrointestinal symptoms in FD patients. Koide et al. (10) reported that patients with irritable bowel syndrome (IBS) showed significantly higher GVS than normal volunteers. Even though, our controls were younger and all were male, the mean GVS of healthy volunteers was approximately equal to that of their original report. They also reported that GVS did not have an apparent correlation with the total colonic transit time, an index for colonic peristalsis. Therefore, GVS is considered a new marker of bowel function in humans. It is interesting that our data on GVS in patients with FD fell just between that of patients with IBS and the data on normal volunteers. Gastroenterologists currently argue that FD and IBS cannot be completely distinguished. In addition, a broader definition of functional gastrointestinal disorders has been proposed which includes these two disease entities (5). Common overlap between dyspeptic symptoms and IBS is also noticed in the Rome III criteria (6). Our data might reflect the common backgrounds of both FD and IBS. From this viewpoint, we now intend to investigate the possibilities of HKT for patients with IBS.
In a former investigation, we demonstrated that HKT improves gastric motility by measuring the gastric emptying rate using an ultrasonographic method (9). Several other reports also support prokinetic action in ingredients of HKT by animal experiments (12–14). Therefore, we consider it possible that prokinetic action might also work in the lower gastrointestinal tract. The anxiolytic effect of HKT in reducing bowel gas should also be considered. Magnoliae Cortex contains honokiol, which was reported to show an anxiolytic effect in animal experiments (15,16). Pinelliae Tuber is also reported to have an anxiolytic effect (12). Many of the patients with FD are considered to also suffer from anxiety, depression and autonomic nerve disturbance (17–19), which sometimes lead to the development of aerophagia due to psychological stress. HKT might attenuate mental stress and protect FD patients from aerophagia. The fact that there was no apparent change of GVS in healthy subjects may provide support for our hypothesis.
With regard to the subjective symptoms of FD patients, their gastrointestinal symptoms significantly improved after the administration of HKT, suggesting that HKT could be used as an agent for FD. It is noteworthy that the analysis of individual symptoms showed that indigestion markedly improved out of five individual symptoms categories. As mentioned before, HKT has often been prescribed for patients complaining of abdominal bloating or who show abdominal gas retention by physical examination. Thus these results are not surprising because complaints of abdominal bloating would be most related to this symptom category. In addition, these results help support the proposal that HKT is effective for this troublesome complaint in dyspeptic patients.
Finally, we were able to demonstrate the clinical efficacy of HKT to improve the gastrointestinal symptoms of patients with FD. The reduction of bowel gas may be a characteristic mechanism of action for HKT, making HKT a possible candidate for a therapeutic drug for FD, especially for patients with abdominal bloating.
References
- 1.Hirakawa K, Adachi K, Amano K, Katsube T, Ishihara S, Fukuda R, et al. Prevalence of non-ulcer dyspepsia in the Japanese population. J Gastroenterol Hepatol. 1999;14:1083–7. doi: 10.1046/j.1440-1746.1999.02012.x. [DOI] [PubMed] [Google Scholar]
- 2.Knill-Jones RP. Geographical differences in the prevalence of dyspepsia. Scand J Gastroenterol. 1991;182(Suppl):17–24. doi: 10.3109/00365529109109532. [DOI] [PubMed] [Google Scholar]
- 3.Talley NJ, Zinsmeister AR, Schleck CD, Melton LJ., 3rd Dyspepsia and dyspepsia subgroups: a population-based study. Gastroenterology. 1992;102:1259–68. [PubMed] [Google Scholar]
- 4.Talley NJ, Colin-Jones D, Koch KL, Nyren O, Stanghellini V. Functional dyspepsia. A classification with guidelines for diagnosis and management. Gastroenterol Int. 1991;4:145–60. [Google Scholar]
- 5.Talley N, Stanghellini V, Heading R. Functional gastroduodenal disorders. Gut. 1999;45(Suppl 2):1137–42. doi: 10.1136/gut.45.2008.ii37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–79. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 7.Azpiroz F, Malagelada JR. Abdominal bloating. Gastroenterology. 2005;129:1060–78. doi: 10.1053/j.gastro.2005.06.062. [DOI] [PubMed] [Google Scholar]
- 8.Terasawa K. Evidence-based reconstruction of Kampo medicine: Part-III – How should Kampo be evaluated? Evid Based Complement Alternat Med. 2004;1:219–22. doi: 10.1093/ecam/neh046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oikawa T, Ito G, Koyama H, Hanawa T. Prokinetic effect of a Kampo medicine, Hange-koboku-to (Banxia-houpo-tang), on patients with functional dyspepsia. Phytomedicine. 2005;12:730–4. doi: 10.1016/j.phymed.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Koide A, Yamaguchi T, Odaka T, Koyama H, Tsuyuguchi T, Kitahara H, et al. Quantitative analysis of bowel gas using plain abdominal radiograph in patients with irritable bowel syndrome. Am J Gastroenterol. 2000;95:1735–41. doi: 10.1111/j.1572-0241.2000.02189.x. [DOI] [PubMed] [Google Scholar]
- 11.Glise H, Hallerback B, Wiklund I. Quality of life: a reflection of symptoms and concerns. Scand J Gastroenterol. 1996;31(Suppl 221):14–7. doi: 10.3109/00365529609095545. [DOI] [PubMed] [Google Scholar]
- 12.Kasahara Y, Saito E, Hikino H. Pharmacological actions of Pinellia Tuber and Zingiber Rhizomes. Shoyakugaku Zasshi. 1983;37:73–83. [Google Scholar]
- 13.Koezuka Y, Honda G, Tabata M. An intestinal propulsion-promoting substance from Perilla frutescens and its mechanism of action. Planta Medica. 1985;51:480–2. [PubMed] [Google Scholar]
- 14.Yamahara J, Huang Q, Li Y, Xu L, Fujimura H. Gastrointestinal motility-enhancing effect of ginger and its active constituents. Chem Pharm Bull. 1990;38:430–1. doi: 10.1248/cpb.38.430. [DOI] [PubMed] [Google Scholar]
- 15.Kuribara H, Stavinoha WB, Maruyama Y. Behavioural pharmacological characteristics of honokiol, an anxiolytic agent present in extracts of Magnolia bark, evaluated by an elevated plus-maze test in mice. J Pharm Pharmacol. 1998;50:819–26. doi: 10.1111/j.2042-7158.1998.tb07146.x. [DOI] [PubMed] [Google Scholar]
- 16.Kuribara H, Kishi E, Hattori N, Yuzurihara M, Maruyama Y. Application of the elevated plus-maze test in mice for evaluation of the content of honokiol in water extracts of magnolia. Phytother Res. 1999;13:593–6. doi: 10.1002/(sici)1099-1573(199911)13:7<593::aid-ptr520>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 17.Alpers DH. Why should psychotherapy be a useful approach to management of patients with non-ulcer dyspepsia? Gastroenterology. 2000;119:869–71. doi: 10.1053/gast.2000.17840. [DOI] [PubMed] [Google Scholar]
- 18.Haug TT, Wilhelmsen I, Ursin H. What are the real problems for patients with functional dyspepsia? Scand J Gastroenterol. 1995;30:97–100. doi: 10.3109/00365529509093244. [DOI] [PubMed] [Google Scholar]
- 19.Talley NJ, Fung LH, Gilligan IJ, McNeil D, Piper DW. Association of anxiety, neuroticism, and depression with dyspepsia of unknown cause. A case-control study. Gastroenterology. 1986;90:886–92. doi: 10.1016/0016-5085(86)90864-4. [DOI] [PubMed] [Google Scholar]