Abstract
Introduction
The present study reports on the prevalence of smoke-free homes, the characteristics of participants who adopted a smoke-free home policy, and the association between smoke-free homes and subsequent predictors of smoking cessation.
Methods
Data are reported on 4,963 individuals who originally participated in the Community Intervention Trial for Smoking Cessation between 1988 and 1993 and completed follow-up surveys in 2001 and 2005. The relationship between home smoking policy and smoking behavior was examined with a multivariate regression model.
Results
Among those who were smokers at the 2001 follow-up, the percentage reporting that no smoking was allowed in their home increased from 29% in 2001 to 38% in 2005. Smokers most likely to adopt smoke-free home policies between 2001 and 2005 were males, former smokers, and those who had lower levels of daily cigarette consumption (among those who continued to smoke), those with higher annual household incomes, and those with no other smokers in the household. Some 28% of smokers with smoke-free homes in 2001 reported that they had quit smoking by 2005 compared with 16% of those who allowed smoking in their homes (odds ratio [OR] = 1.7, 95% CI = 1.4–2.2), and baseline quitters with smoke-free homes also were less likely to relapse (OR = 0.6, 95% CI = 0.4–0.8).
Discussion
Smoke-free homes are becoming more prevalent, and they are a powerful tool not only to help smokers stop smoking but also to help keep those who quit from relapsing back to smoking.
Introduction
The recent surgeon general's report concluded that secondhand smoke causes disease and death in children and nonsmoking adults (U.S. Department of Health and Human Services [USDHHS], 2006), and household smoking restrictions are encouraged to protect these individuals. Such restrictions may have an indirect public health benefit by promoting smoking cessation among smokers. The relationship between smoke-free worksite policies and increased cessation behavior is well established (Bauer, Hyland, Li, Steger, & Cummings, 2005; Fichtenberg & Glantz, 2002); however, the potential role of smoke-free home policies on smoking behavior has received much less attention. A handful of cross-sectional studies in adults have examined the association between smoke-free homes and smoking behavior and found that rules that prohibit smoking in the home are associated with fewer cigarettes smoked per day (Gilpin, White, Farkas, & Pierce, 1999), more interest in quitting (Gilpin et al., 1999), reduced smoking behavior (Clark et al., 2006), as well as reduced relapse among smokers who have quit (Gilpin et al., 1999). However, cross-sectional studies cannot clarify whether the smoke-free policy precedes the change in smoking behavior or if smokers who quit, then adopt a smoke-free home policy.
A prospective, population-based study on this topic by Borland et al. (2006) found that intentions to quit at baseline and quitting activity in the 7-month follow-up period were associated with implementing home smoking bans during that period. Also, the presence of bans at baseline was associated with significantly greater proportions of quit attempts, and success among those who tried, at follow-up. Other longitudinal studies have demonstrated associations between home smoking bans and reduced cigarette consumption (Farkas, Gilpin, Distefan, & Pierce, 1999; Shields, 2005), increased quit attempts (Farkas et al., 1999; Pizacani et al., 2004), prolonged time to relapse (Pizacani et al., 2004), lower rates of relapse (Farkas et al., 1999), and increased smoking cessation (Shields, 2007; Shopland, Anderson, & Burns, 2006). The two most consistent correlates of having a smoke-free home policy are the presence of young children and not having any other smokers in the home (Borland et al., 2006; Gilpin et al., 1999; Merom & Rissel, 2001).
The present study aimed to add to the literature on the relationship between smoke-free home policy implementation and subsequent smoking behavior using data from a large, prospective population-based sample of U.S. current and former smokers interviewed between 2001 and 2005. The study had the following three goals: (a) to describe the level and rate of smoke-free home policy adoption, (b) to examine the characteristics of participants who implemented a smoke-free home policy, and (c) to assess the relationship between having a smoke-free home policy at baseline and predictors of cessation in smokers and relapse in former smokers.
Methods
Data source
The data analyzed here come from people who originally participated in the Community Intervention Trial for Smoking Cessation (COMMIT) study conducted between 1988 and 1993 and who were subsequently reinterviewed in 2001 and 2005. A detailed description of the COMMIT study design has been reported previously (COMMIT Research Group, 1995; National Cancer Institute, 1995). In brief, the study was a matched-pair, randomized trial of 22 small to medium communities in 10 states or provinces in the United States and Canada. In 1988, random-digit–dialed, cross-sectional telephone surveys regarding adult smoking behaviors were conducted, and all participants were smokers (defined as having smoked 100 cigarettes in their lifetime and currently smoking at the time of interview). These smokers were interviewed again in 1993, and all U.S. subjects who finished both the 1988 and 1993 surveys were interviewed again in 2001 and 2005 when questions about home smoking policies were added to the surveys. Participants were aged 25–64 years at baseline, and sample sizes were 22,046 in 1988, 12,435 in 1993, 6,603 in 2001, and 4,963 in 2005. By 2005, the remaining sample contained 2,268 current smokers and 2,695 former smokers. Those who were current smokers in 2001 were more likely to be lost to follow-up if they were male or if they had lower income or had less education. Only the data from 2001 and 2005 were used in the present study because measures of smoke-free home policies were not collected from the entire cohort in the 1988 or 1993 surveys.
Outcome measures: smoke-free home policy
In the 2001 and 2005 surveys, participants were asked, “What are the smoking rules or restrictions in your household, if any? Would you say… smoking is never allowed in the house, smoking is sometimes allowed, smoking is allowed in some rooms only, or there are no rules about smoking in the house?” Those who responded that “smoking is never allowed in the house” were considered to have a smoke-free home. Those who responded with any of the other three choices were combined into a single category and considered not to have a smoke-free home. We considered the 2001 reported home smoking policy as well as the change in policy between 2001 and 2005 in the analysis. The home smoking policy variable is considered as an outcome for the analyses presented in Table 1 and as the main predictor variable for the analyses presented in Table 2.
Table 1.
Characteristics of those adopting a smoke-free home policy by 2005 among smokers in 2001 who allowed smoking in their homes
| 95% CI |
|||||
| Sample size | Percent adopted | Relative riska | Lower | Upper | |
| Overall | 1,873 | 19 | |||
| Sex | |||||
| Female | 1,126 | 17 | 1.0 | Referent | |
| Male* | 748 | 21 | 1.4 | 1.1 | 1.7 |
| Age, years (2001) | |||||
| <45 | 394 | 19 | 1.0 | Referent | |
| 45–54 | 739 | 20 | 1.1 | 0.8 | 1.5 |
| 55–64 | 502 | 18 | 1.0 | 0.7 | 1.4 |
| 65+ | 235 | 17 | 1.1 | 0.7 | 1.8 |
| Race | |||||
| White | 1,682 | 19 | 1.0 | Referent | |
| Black | 72 | 11 | 0.5 | 0.2 | 1.1 |
| Hispanic | 85 | 20 | 0.8 | 0.5 | 1.5 |
| Other | 33 | 12 | 0.5 | 0.2 | 1.4 |
| Income (2001) | |||||
| <US$15,000 | 134 | 16 | 1.0 | Referent | |
| $15,000–$37,500 | 429 | 15 | 1.0 | 0.6 | 1.8 |
| $37,501–$60,000 | 595 | 20 | 1.5 | 0.9 | 2.5 |
| >$60,000* | 610 | 23 | 1.9 | 1.1 | 3.2 |
| Refused/do not know | 103 | 12 | 0.7 | 0.3 | 1.6 |
| Education, years (1988) | |||||
| <12 | 219 | 17 | 1.0 | Referent | |
| 12 | 437 | 19 | 1.0 | 0.7 | 1.6 |
| 13–15 | 839 | 19 | 0.9 | 0.6 | 1.4 |
| 16+ | 373 | 18 | 0.7 | 0.4 | 1.1 |
| Number of cigarettes smoked per day (2001) | |||||
| 25+ | 529 | 16 | 1.0 | Referent | |
| 15–24* | 811 | 19 | 1.3 | 1.0 | 1.8 |
| 5–14 | 413 | 20 | 1.3 | 0.9 | 2.0 |
| <5* | 115 | 30 | 2.0 | 1.2 | 3.5 |
| Time to first cigarette, min (2001) | |||||
| <10 | 639 | 17 | 1.0 | Referent | |
| 10–30 | 686 | 17 | 1.0 | 0.7 | 1.3 |
| 31–60 | 298 | 20 | 1.0 | 0.7 | 1.5 |
| >60 | 243 | 28 | 1.5 | 1.0 | 2.3 |
| Other household smokers (2001) | |||||
| ≥1 | 665 | 17 | 1.0 | Referent | |
| 0* | 1,209 | 20 | 1.4 | 1.1 | 1.8 |
Note. The percentages adopting a smoke-free policy presented in this table differ from those shown in Figure 1 because these results are restricted to the subpopulation of smokers who did not have a smoke-free home policy in 2001, whereas the data in Figure 1 are among all smokers.
Results from a logistic regression controlling for sex, age, race, income, education, amount smoked, time to first cigarette, and other household smokers.
*Statistically significant at the 5% level.
Table 2.
Relative risk (RR) of cessation-related outcomes in 2005 by smoke-free home status in 2001
| Smoke-free home (2001) | ||||||||||
| Overall |
No |
Yes |
95% CI |
|||||||
| Sample | Outcome | Sample size | % | Sample size | % | Sample size | % | RR | Lower | Upper |
| All smokers in 2001 | Quita* | 2,622 | 19 | 1,879 | 16 | 742 | 28 | 1.7 | 1.4 | 2.2 |
| Quit attempt* | 2,622 | 64 | 1,879 | 62 | 742 | 71 | 1.5 | 1.3 | 1.9 | |
| Continuing smokers, 2001–2005 | Use of NRT/bupropionb* | 2,122 | 39 | 1,585 | 37 | 536 | 42 | 1.5 | 1.2 | 1.9 |
| Decrease in cigarettes per dayc | 2,122 | 42 | 1,580 | 42 | 534 | 41 | 1.2 | 0.9 | 1.4 | |
| Former smokers in 2001 | Relapsedd* | 2,341 | 7 | 950 | 9 | 1,390 | 6 | 0.6 | 0.4 | 0.8 |
Note. aIn the analyses of quitting and quitting-related outcomes, results from a logistic regression controlling for smoke-free homes in 2001, sex, age, race, income, education, amount smoked, time to first cigarette, and other smokers in the household. The reference group is homes where smoking is allowed. Quitting was assessed with the question “Do you smoke cigarettes now?” Quit attempts were assessed with the question “Since 2001, how many times have you made a serious attempt to quit smoking?”
Use of nicotine replacement therapy (NRT) was calculated by combining responses to questions about use of NRT since 2001: “Since 2001, have you used…?”
Decrease in cigarettes per day was calculated with the difference between the number of cigarettes smoked per day in 2001 and in 2005.
In the analysis of relapse, results from a logistic regression controlling for smoke-free homes in 2001, sex, age, race, income, education, and other smokers in the household. The reference group is homes where smoking is allowed. Relapse was defined as a response of yes to the question “Do you smoke cigarettes now?” among those who did not smoke in 2001.
*Statistically significant at the 5% level.
Outcome measures: smoking behavior
Five predictors of cessation were examined among those who were smokers in 2001: (a) quit attempts, defined as the self-report of one or more “serious attempts to quit smoking since 2001”; (b) use of medication designed to assist in smoking cessation (report of using a nicotine patch, nicotine gum, nicotine inhaler, nicotine nasal spray, nicotine lozenges, or bupropion since 2001); (c) reductions in cigarettes per day among continuing smokers, defined as the difference between the number of cigarettes smoked per day in 2001 and in 2005; (d) successful cessation among those who attempted to quit, defined as report of not smoking cigarettes at least 6 months prior to the 2005 survey; and (e) overall smoking cessation, defined as report of not smoking cigarettes at least 6 months prior to the 2005 survey.
In addition, relapse to smoking was examined among those who were successful quitters in 2001 and who were currently smoking at the time of the 2005 interview.
Independent variables
Independent variables examined in the analysis included the following: age in 2001 (<45, 45–54, 55–64, 65+ years), gender (male or female), race/ethnicity (White, non-Hispanic; Black, non-Hispanic; Hispanic; and other), annual household income in 2001 (<US$15,000; $15,000–$37,500; $37,501–$60,000; >$60,000), education in 1988 (<12, 12, 13–15, 16+ years), number of cigarettes smoked per day in 2001 (≥25, 15–24, 5–14, or <5), time to first cigarette after waking in 2001 (<10, 10–30, 31–60, >60 min), and number of other smokers in the household in 2001 (0, ≥1).
Data analyses
SPSS version 14.0 was used for all analyses. Home smoking policies in 2001 and 2005 and smoking behavior were assessed with descriptive statistics. Logistic regression was used to assess the association between the independent variables measured in 2001 and the adoption of a smoke-free home policy between 2001 and 2005 as well as to assess the association between home smoking policies in 2001 and subsequent cessation or relapse indicators while controlling for the independent variables noted above. Survey weights were calculated to weight the data to the age, gender, race/ethnicity, and community distribution of the 2001 sample. Analyses were conducted with both weighted and unweighted data with similar results, and only the weighted results are presented.
Results
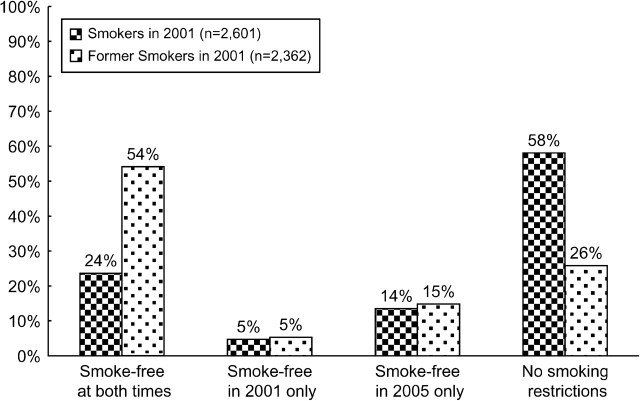
As shown in Figure 1, 14% of all smokers and 15% of all former smokers in 2005 adopted a smoke-free home policy. Only 5% of both current and former smokers eliminated their earlier smoke-free policy by 2005. Overall, only 24% of smokers in 2001 reported a smoke-free home in both 2001 and 2005, whereas 54% of the former smokers in 2001 reported the same.
Figure 1.
Smoke-free home status from 2001 to 2005 among smokers in 2001 (N = 2,601). Respondents were asked, “What are the smoking rules or restrictions in your household”, if any? Those who responded, “smoking is sometimes allowed,” “smoking is allowed in some rooms only,” or “there are no rules about smoking in the house” were not considered to have a smoke-free home. Those who responded, “smoking is never allowed in the house” were considered to have a smoke-free home.
When limiting analyses to smokers in 2001 who had no restrictions, 19% implemented a smoke-free home policy by 2005. Factors significantly associated with implementing a smoke-free home policy were male gender (relative risk [RR] = 1.4, 95% CI = 1.1–1.7), annual income greater than $60,000, compared with those making less than $15,000 (RR = 1.9, 95% CI = 1.1–3.2), smoking fewer than 5 cigarettes/day (RR = 2.0, 95% CI = 1.2–3.5), and the presence of no other smokers in the household (RR = 1.4, 95% CI = 1.1–1.8; Table 1).
Table 2 displays the results showing the relationship between having a smoke-free home in 2001 and smoking behavior in 2005. Among baseline smokers, smoke-free home policies were significantly associated with making a quit attempt (RR = 1.5, 95% CI = 1.3–1.9) and with quitting (RR = 1.7, 95% CI = 1.4–2.2). Among baseline smokers who continued to smoke, smoke-free home policies were significantly associated with increased use of medication designed to assist in smoking cessation (RR = 1.5, 95% CI = 1.2–1.9) but were not associated with reductions in number of cigarettes smoked per day. Among former smokers in 2001, those with a smoke-free home policy in 2001 were significantly less likely to relapse to smoking compared with those who still allowed smoking in their homes (RR = 0.6, 95% CI = 0.4–0.8).
Discussion
Using a longitudinal design, the present study showed that both current and former smokers increasingly adopted smoke-free home policies and that these policies increased cessation and decreased relapse. Furthermore, in the study sample, the prevalence of smoke-free homes increased between 2001 and 2005 and the strongest correlates of having a household smoking ban was lack of other smokers in the home, higher income, lower daily cigarette consumption, and male gender.
Other cross-sectional studies have consistently shown an association between the presence of smoke-free home policies and an increase in cessation, but the relationship between the onset of these smoking rules and time to cessation has not been clear (Clark et al., 2006; Gilpin et al., 1999). A prospective study looking at home smoking policies and subsequent smoking cessation found a 30% increase in the rate of subsequent quit attempts and nearly double the smoking cessation rate (Borland et al., 2006). Although the present results closely mirror these findings, our paper adds to the literature by documenting that smoke-free home policies are associated with greater use of medications that assist in cessation among current smokers and lower rates of relapse among former smokers.
The characteristics of those implementing a smoke-free home also were consistent with the literature. The most consistent correlate from the literature was the presence of nonsmokers in the household, particularly young children, a finding replicated in our study. Gilpin et al. (1999) reported that Blacks were less likely to report a smoke-free home policy. We observed a borderline statistically significant relationship with this variable, but our sample size was considerably smaller than the one reported by Gilpin et al. We also replicated the finding of Gilpin et al. that males and lighter smokers were more likely to have a smoke-free home policy and replicated the finding of Borland et al. (2006) of higher income as a predictor of smoke-free home policy adoption. Although our paper focused on the outcome of adopting a smoke-free home policy rather than the cross-sectional presence of a home policy, the data were examined in both ways and the results were qualitatively identical—a finding replicated by Borland et al.
Borland et al. (2006) reported that smokers who lived in a community in which smoking was prohibited in bars were significantly more likely to implement smoke-free home policies. Our ability to replicate this finding was limited because only California had a smoke-free bar law in force at the beginning of the study. We did, however, examine a model that included respondents’ worksite smoking policy in 2001 as a crude proxy for public smoking restrictions. This model showed a nonsignificant RR for smoke-free home policy adoption for those reporting completely smoke-free worksites at baseline (RR = 0.9, 95% CI = 0.9–1.6). We did not include this variable in the models presented here because it reduced the sample size considerably (to only employed participants). Subsequent studies should be able to confirm or refute the finding of Borland et al. that public smoking policies can directly influence the home smoking policies.
The strengths of the present analysis include the long-term follow-up, large sample size, and the fact that it is population based. Its principal potential limitation is that only 23% of the original cohort recruited in 1988 completed an interview in 2005. To examine this issue further, we weighted the 2005 sample to the baseline age, gender, race/ethnicity, and community distribution of the 2001 sample. Another limitation is that the COMMIT sample is not nationally representative and is skewed toward older, heavier smokers. As a result, the findings may not be generalizable to a younger or lighter smoking population; however, the impact of smoke-free homes on quitting behavior in the general population, which is younger and less nicotine dependent than the sample used in the present study, may be even larger than observed here because lighter smokers were more likely to implement smoke-free home policies.
In conclusion, smoke-free homes are becoming more prevalent, and the results from the present study show that they are a powerful tool that both promotes cessation and helps prevent relapse.
Funding
The COMMIT study was conducted between 1988 and 1993 and was funded by the National Cancer Institute (NCI). The 2001 follow-up survey of the COMMIT cohort also was funded by the NCI, through the State and Community Tobacco Control Interventions Research Initiative (CA86225). The 2005 survey was funded by NCI (CA100802).
Declaration of Interests
None declared.
Supplementary Material
References
- Bauer JE, Hyland A, Li Q, Steger C, Cummings KM. A longitudinal assessment of the impact of smoke-free worksite policies on tobacco use. American Journal of Public Health. 2005;95:1024–1029. doi: 10.2105/AJPH.2004.048678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: Findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15:42–50. doi: 10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark PI, Schooley MW, Pierce B, Schulman J, Hartman AM, Schmitt CL. Impact of home smoking rules on smoking patterns among adolescents and young adults. Preventing Chronic Disease. 2006;3:1–13. Retrieved December 5, 2007, from http://www.cdc.gov/pcd/issues/2006/apr/05_0028.htm. [PMC free article] [PubMed] [Google Scholar]
- COMMIT Research Group. Community Intervention Trial for smoking sessation (COMMIT): I. Cohort results from a four-year community intervention. American Journal of Public Health. 1995;85:183–192. doi: 10.2105/ajph.85.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas AJ, Gilpin EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviors. Tobacco Control. 1999;8:261–265. doi: 10.1136/tc.8.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behavior: Systematic review. British Medical Journal. 2002;325:188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin EA, White MM, Farkas AJ, Pierce JP. Home smoking restrictions: Which smokers have them and how they are associated with smoking behavior. Nicotine & Tobacco Research. 1999;1:53–62. doi: 10.1080/14622299050011261. [DOI] [PubMed] [Google Scholar]
- Merom D, Rissel C. Factors associated with smoke-free homes in NSW: Results from the 1998 NSW Health Survey. Australia and New Zealand Journal of Public Health. 2001;25:339–345. doi: 10.1111/j.1467-842x.2001.tb00590.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Community-based intervention for smokers: The COMMIT field experience. Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health, Nation Cancer Institute; 1995. (NIH Publication No. 95-4028). Smoking and tobacco control monograph 6. [Google Scholar]
- Pizacani BA, Martin DP, Stark MJ, Koepsell TD, Thompson B, Diehr P. A prospective study of household smoking bans and subsequent cessation related behavior: The role of stage of change. Tobacco Control. 2004;13:23–28. doi: 10.1136/tc.2003.003038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields M. The journey to quitting smoking. Health Reports. 2005;16(3):19–36. [PubMed] [Google Scholar]
- Shields M. Smoking bans: Influence on smoking prevalence. Health Reports. 2007;18(3):9–24. [PubMed] [Google Scholar]
- Shopland DR, Anderson CM, Burns DM. Association between home smoking restrictions and changes in smoking behavior among employed women. Journal of Epidemiology and Community Health. 2006;60(Suppl. 2):44–50. doi: 10.1136/jech.2006.045724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2006. (OSG Publication No. O2NLM: WA 754 H4325 2006) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.