Abstract
The present report describes a 67-year-old woman with a mobile aortic valve lesion discovered by transesophageal echocardiography performed in the setting of abdominal pain. Definitive identification of the lesion was not possible by transesophageal echocardiography alone. Pathological examination of the excised lesion led to the diagnosis of papillary fibroelastoma (PFE). PFEs are rare benign tumours that primarily affect cardiac valves. Because left-sided PFEs are associated with a high risk of systemic embolization including cerebral ischemia and myocardial infarction, they require preventive surgical correction. The present case of PFE is reviewed for a better understanding of its pathology.
Keywords: Aortic valve, Cardiac tumour, Echocardiography, Embolism, Papillary fibroelastoma
Abstract
Le présent rapport décrit le cas d’une femme de 67 ans ayant une lésion mobile de la valve aortique découverte par échocardiographie transœsophagienne effectuée en raison de douleurs abdominales. Il n’a pas été possible de dépister la lésion avec certitude au moyen de l’échocardiographie seulement. L’examen pathologique de la lésion excisée a permis de diagnostiquer un fibroélastome papillaire (FÉP). Les FÉP sont des tumeurs bénignes rares qui touchent surtout les valves cardiaques. Puisque les FÉP gauches s’associent à un risque important d’embolisation systémique, y compris l’ischémie cérébrale et l’infarctus du myocarde, ils nécessitent une chirurgie correctrice préventive. Les auteurs analysent le présent cas de FÉP pour mieux en comprendre la pathologie.
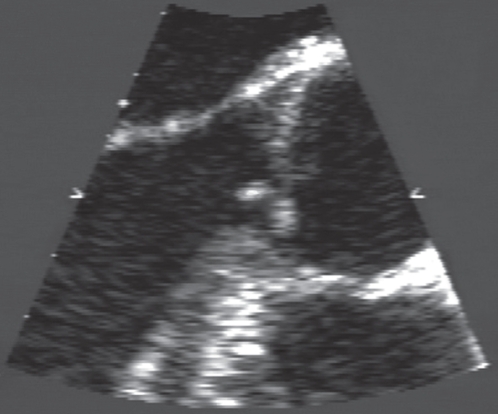
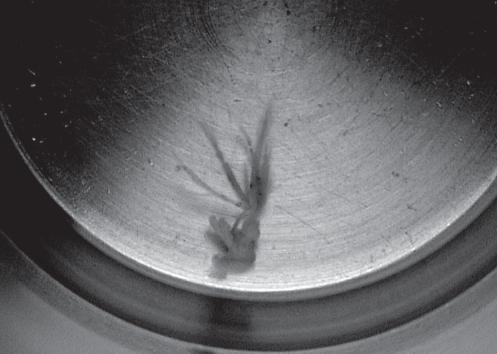
A 67-year-old woman was referred to the Institut Universitaire de Cardiologie et de Pneumologie de Québec (Québec, Québec) for transesophageal echocardiography to eliminate an embolism of cardiac origin. One week before the patient’s transfer, she had a consultation for abdominal pain. Her medical history was noncontributory and her physical examination was normal. A computed tomography scan showed a limited splenic infarct. Thrombophlebitis of the lower limbs with secondary paradoxical embolism was ruled out. An electrocardiogram showed normal sinus rhythm. Transthoracic echocardiography showed only minimal mitral regurgitation. Transesophageal echocardiography showed a mobile mass, 6 mm in length on the aortic valve that was attached to the extremity of the right coronary cusp and fluttered in the left ventricular outflow tract (Figure 1). Distinction between a tumour or a vegetation was not possible. Hemocultures were negative. The splenic infarct was best explained by peripheral embolism related to the aortic valve lesion. The lesion was surgically removed, leaving the valve intact. On gross pathological evaluation, the lesion consisted of a delicate white mass that was 6 mm in size and resembled a sea anemone when immersed in water (Figure 2). Microscopically, it showed delicate avascular fronds of fibrous and elastic tissue lined with endothelial cells. No thrombus was identified. These features were interpreted as diagnostic of papillary fibroelastoma (PFE).
Figure 1).
Transesophageal echocardiography showing a mobile mass, 6 mm in length, on the aortic valve that was attached to the extremity of the right coronary cusp and fluttered in the left ventricular outflow tract
Figure 2).
A lesion consisting of a delicate white mass that was 6 mm in length and resembled a sea anemone when immersed in water
DISCUSSION
The incidental discovery of an aortic valve mass is not a rare phenomenon (1). Correct identification is crucial because some lesions require surgical correction. Vegetations caused by endocarditis, Lambl’s excrescences, PFEs and other valve tumours are classically considered, while aortic valve fenestration (AVF) bridging strand rupture is rarely mentioned (2). PFE is a benign cardiac tumour that accounts for three-fourths of all cardiac valve tumours (3). PFE predominates in adults and is particularly frequent between the fourth and eighth decades of life. The precise etiology of this lesion is not known. Few cases are congenital but most cases are believed to be acquired (3). These tumours are small, highly papillary and pediculated. PFE has a characteristic flower-like appearance, with multiple papillary fronds attached to the endocardium by a short pedicle. Because papillary fronds are best visualized when immersed in physiological saline, this tumour is often compared with a sea anemone. Organized thrombi can occasionally be present on the surface of a PFE. The size of this tumour varies greatly, but the majority of PFEs are approximately 10 mm at the greatest dimension (3). This benign tumour derives from normal components of the endocardium. In more than 80% of cases, PFEs are located on the cardiac valves, but they arise from anywhere within the heart. PFEs may arise from the free edge of the valve, although a PFE is more frequently attached to the middle portion of the valve. PFEs occurring on the atrioventricular valves usually arise from the atrial aspect of the endocardium, whereas tumours on the semilunar valves affect either side of the valve with equal predilection. In adults, the aortic valve is mostly involved. PFEs are usually solitary but can sometimes be multiple. Most patients with cardiac PFEs are asymptomatic, but disabling symptoms may occur. There are various clinical presentations, including embolization, cardiac or obstructive symptoms. Presentation is determined by many factors including tumour location, size and growth rate. It is not clear whether embolization is more likely the result of associated thrombi or from the tumour itself (4). Possible manifestations include myocardial infarction, sudden death, cerebral ischemic attack, heart failure, syncope, pulmonary embolism and peripheral embolism (4). PFEs arising from the aortic valve have been implicated in sudden death of otherwise healthy young individuals. Transient or complete obstruction of the ostium of the left or right coronary artery is the proposed mechanism to explain the lethal issue (3,5). Conduction system disturbances and complete atrioventricular conduction block have also been reported (3). Atrioventricular valve PFEs can cause obstruction of left or right ventricle filling, resulting in recurrent pulmonary edema and right heart failure (3). Most PFEs are discovered incidentally by transthoracic echocardiography. Echocardiography usually demonstrates a small, mobile and echodense mass. It can be pediculated or sessile, valvular or endocardial, and may prolapse or flutter into cardiac chambers (1). The differential diagnosis includes thrombi, vegetations, valvular calcifications, Lambl’s excrescences, AVF and other cardiac tumours. Useful diagnostic features to distinguish PFE from other valvular masses include clinical presentation, size, location and mobility assessed by echocardiography (3). Unlike PFE, Lambl’s excrescences are filiform fronds that occur frequently along the line of valve closure and are often multiple (1). When contemplating a diagnosis of PFE, one should always remember to include AVF bridging strand rupture as a possible alternative explanation. Myxomas most commonly occur in the left atrium, with a pedicle attached near the fossa ovalis and are predominantly solitary tumours. In a review of 725 cases of PFE (3), 21 patients (3%) died. Tumour mobility was the only independent predictor of cardiac death or nonfatal embolization. PFEs are amenable to simple surgical excision with minimal morbidity and mortality (4). Surgery is the treatment of choice for symptomatic PFE and is now recommended even in asymptomatic patients, especially if the lesion is present on the left side (1). Prophylactic anticoagulation should be initiated at diagnosis. However, none of these recommendations are based on randomized controlled data (1). Careful follow-up with clinical and echocardiographic evaluation is warranted.
REFERENCES
- 1.Hicks KA, Kovach J, Frishberg DP, et al. Echocardiographic evaluation of papillary fibroelastoma: A case report and review of the literature. J Am Soc Echocardiogr. 1996;9:353–60. doi: 10.1016/s0894-7317(96)90152-2. [DOI] [PubMed] [Google Scholar]
- 2.Bourgault C, Couture C, Martineau A, Dagenais F, Sénéchal M. Incidental mobile aortic valve lesion: A case of aortic valve fenestration. J Heart Valve Dis. 2007;16:692–4. [PubMed] [Google Scholar]
- 3.Gowda RM, Khan IA, Nair CK, et al. Cardiac papillary fibroelastoma: A comprehensive analysis of 725 cases. Am Heart J. 2003;146:404–10. doi: 10.1016/S0002-8703(03)00249-7. [DOI] [PubMed] [Google Scholar]
- 4.Georghiou Georgios P, Shapira Y, Stamler A, et al. Surgical excision of papillary fibroelastoma for known or potential embolization. J Heart Valve Dis. 2005;14:843–7. [PubMed] [Google Scholar]
- 5.Bussani R, Silvestri F. Sudden death in a woman with fibroelastoma of the aortic valve chronically occluding the right coronary ostium. Circulation. 1999;100:2204. doi: 10.1161/01.cir.100.21.2204. [DOI] [PubMed] [Google Scholar]