Abstract
BACKGROUND
New recommendations suggest that the 2000 Centers for Disease Control and Prevention (CDC) growth charts and body mass index (BMI) for age be used for Canadian children. Little information is available on how often growth parameters are documented in hospital settings.
OBJECTIVE
To determine the frequency of documentation of growth parameters in the medical records of a tertiary care paediatric hospital.
METHODS
A prospective, 14-day audit of 491 charts of children seen in the emergency department (ED) or admitted to a ward was performed to determine the frequency of documentation of height/length, weight, head circumference, BMI or weight for height, and presence of growth charts. Similar data were sought from the most recent clinic visit for all ward charts.
RESULTS
Growth parameters, aside from weight, were infrequently documented in the medical record. Height/length was documented in no ED charts and in 42% of ward charts. BMI or weight for height were almost never found, and growth charts were present in only 23% of ward charts, one clinic chart and one ED chart.
CONCLUSIONS
Rates of documentation of growth parameters in the teaching hospital setting were unacceptably low. Implementation of the use of the 2000 CDC growth charts will require not only education regarding BMI but also steps to encourage more regular measurement of height and use of shared growth charts in all areas of the hospital. A simple conceptualization framework for health care providers to use as a counselling tool is presented.
Keywords: Audit, Body mass index, Green zone, Growth, Growth chart
Abstract
HISTORIQUE
Selon de nouvelles recommandations, les courbes de croissance et d’indice de masse corporelle (IMC) selon l’âge, créées en 2000 par les Centers for Disease Control and Prevention (CDC), devraient être utilisées pour les enfants canadiens. Il existe peu d’information sur la fréquence de la documentation des paramètres de croissance en milieu hospitalier.
OBJECTIF
Déterminer la fréquence de la documentation des paramètres de croissance dans les dossiers médicaux d’un hôpital pédiatrique de soins tertiaires.
MÉTHODOLOGIE
La vérification prospective pendant 14 jours de 491 dossiers d’enfants vus à l’urgence ou hospitalisés a été effectuée pour déterminer la fréquence de la documentation de la taille, du poids, de la circonférence crânienne, de l’IMC ou du poids par rapport à la taille ainsi que la présence des courbes de croissance. À l’égard de tous les dossiers d’hospitalisation, des données similaires ont été recherchées pour la visite clinique la plus récente.
RÉSULTATS
À part le poids, les paramètres de croissance sont rarement documentés dans les dossiers médicaux. La taille était documentée dans 42 % des dossiers d’hospitalisation, mais dans aucun dossier de l’urgence. L’IMC ou le poids par rapport à la taille n’étaient pratiquement jamais précisés, et les courbes de croissance n’étaient incluses que dans 23 % des dossiers d’hospitalisation, dans un dossier clinique et dans un dossier de l’urgence.
CONCLUSIONS
Les taux de documentation des paramètres de croissance sont bas et ce, à un niveau inacceptable pour un hôpital d’enseignement. Pour implanter l’usage des courbes de croissance des CDC de 2000, il faudra non seulement prévoir une formation à l’égard des IMC, mais également poser des gestes pour favoriser la prise plus régulière des mesures de taille et l’usage de courbes de croissance communes dans tous les secteurs de l’hôpital. Une simple structure de conceptualisation conçue pour que les dispensateurs de soins utilisent les courbes comme outil de counseling est présentée.
In March 2004, the Canadian Paediatric Society (CPS) published a position statement regarding the use of growth charts for the assessment and monitoring of growth in Canadian infants and children (1). The statement acknowledged the pre-eminent role of growth assessment in defining health and nutritional status in children and recommended the use of the 2000 Centers for Disease Control and Prevention (CDC) growth charts as the growth reference. Body mass index (BMI) for age was recommended for general use as a screen for overweight in children aged two to 20 years (1). This is similar to recent recommendations of the American Academy of Pediatrics to calculate and plot BMI once a year in all children (2).
There is, however, little information on how often growth parameters are currently documented in hospital settings. One audit of medical records from paediatric specialty clinics from 1973 in a university medical centre found that growth charts were deficient in 45% of cases (3). An audit of emergency room charts in 1997 found that children were weighed before drugs were prescribed in only two of 100 cases (4). A recent survey of community paediatricians in North Carolina, USA, revealed that although the use of BMI for age was more likely to lead to the identification of weight problems, most paediatricians still used a combination of weight and height charts, a practice that may lead to underestimation of childhood overweight (5).
The introduction of new growth charts provides an opportunity to examine our approach to alterations in normal growth. While the prevalence of growth problems such as short stature has not increased, the prevalence of children who are overweight or at risk for overweight in Canada has risen and become a major public health concern (6). Routine measurement using accurate techniques, an appropriate growth reference and BMI for age form the basis for approaching this problem. Health care professionals then require tools to assist them in addressing the pressing issues of assisting families to maintain or achieve a healthy BMI. Before the introduction of the 2000 CDC growth charts at the IWK Health Centre, Halifax, Nova Scotia, we undertook an audit of the frequency of documentation of growth parameters in hospital charts. In the present paper, we report the results of the audit and present the “Green Zone”, a conceptual framework we have developed for health care providers that links the importance of healthy eating, healthy activity and BMI.
METHODS
A prospective audit of documentation of growth parameters and use of growth charts was performed in three areas of the IWK Health Centre, a tertiary care children’s hospital, over 14 consecutive days from March 24 to April 6, 2004. Audits were performed in the emergency department (ED) and three inpatient wards (two medical, one surgical) after permission was obtained from health services managers in each area. Staff members were blinded to the purpose of the audit to avoid changes in their practice. In the ED, at least 25 charts were reviewed each day, selected by beginning at different points in the alphabet and proceeding sequentially. Due to the consistency of findings in the ED, no further charts were audited after 12 days. Charts of patients admitted from the ED were not reviewed in the ED. Charts from admissions to the selected wards over a 14-day period were reviewed by one of the authors (HJ), usually within 20 h to 48 h of admission. The goal was to review the charts of all patients admitted to the selected wards on the day following admission of the patient; however, this was not always achieved because charts were not always available for review. Transcription of the weight from the ED was not accepted as documentation of weight for inpatient wards. For ward admissions, medical record charts were also reviewed to audit the most recent visit to any clinic in the health centre. The clinic data, therefore, came from a wide variety of sources, including general paediatrics, specialty medicine and surgery clinics.
Information extracted included the age of the patient and whether documentation of height/length, weight, head circumference, heart rate, respiratory rate, temperature, blood pressure, and a growth chart or documented percentiles appeared on the chart. Measured heights and weights were also recorded. Charts were excluded from the audit if there was a significant barrier to accurate measurement, such as critical illness or immediate postoperative state, or if charts could not be located at the time of the audit.
All data was entered into and analyzed using Epi Info 2002 (CDC, USA). Data were analyzed using frequency and 95% CIs. Head circumference measurements were analyzed only for children younger than two years of age. Fisher’s exact test was used to compare rates of documentation between the medical and the surgical wards. Using height/length and weight extracted from the chart, height, weight, BMI for age and weight for height, percentiles and z-scores were calculated using the Epi Info 2002 NutStat program using the 2000 CDC reference.
RESULTS
A total of 491 charts were reviewed (415 ED, 16 surgical ward and 60 medical ward charts). This represents 34% of all ED visits, 33% of surgical ward admissions and 74% of medical ward admissions during the study period. The median age of patients was 3.88 years (range 0.01 to 18.8 years) and 44% were female. In total, 33.9% of patients were younger than two years of age, 23.9% were from 2.0 to 4.99 years, 18.8% were from 5.0 to 9.99 years, and 23.5% were 10 years or older. Ten per cent of charts (n=51) were classified as inappropriate for measurement and were excluded from the following analyses. There were no differences in the rates of documentation of weight (P=0.32), height/length (P=0.27), head circumference (P=0.43) or presence of growth charts (P=0.22) between the medical and surgical wards; therefore, data from all wards are reported together.
As shown in Table 1, weight was the most frequently documented growth parameter, while BMI or weight for height and growth charts were infrequently documented. For charts with growth parameters available, percentiles and z-scores were calculated by the authors following the audit. Height z-scores (n=31) ranged from −4.38 to 2.14, with 13% (n=4) falling below −2. Weight z-scores (n=386) ranged from −4.22 to 5.76, with 2.6% falling below −2.0 and 8.5% falling above 2.0. This information is difficult to interpret without corresponding height data. Weight for height or BMI for age could be calculated in only 35% (n=32) of ward and clinic charts, and it fell more than two standard deviations from the mean in two cases. The BMI z-scores ranged from −1.27 to 2.54 (10th to 99th percentiles).
TABLE 1.
Documentation of growth parameters by location
| Location | ED (n=378) | Ward (n=62) | Clinic (n=30) |
|---|---|---|---|
| Height/length, % (n) | 0 | 41.9 (26) | 23.3 (7) |
| Weight, % (n) | 88.9 (336) | 71.0 (44) | 40.0 (12) |
| Head circumference*, % (n) | 0 | 54.5 (18) | N/A |
| BMI/weight for height, % (n) | 0 | 0 | 6.7 (2) |
| Growth chart, % (n) | 0.3 (1) | 22.6 (14) | 3.3 (1) |
For cases younger than two years of age (n=33). BMI Body mass index; ED Emergency department; N/A Not available
DISCUSSION
In this tertiary care university medical centre, rates of documentation of growth parameters were surprisingly and unacceptably low. One previous study (3) at another institution from the 1970s found growth charts present in just over one-half of paediatric subspecialty clinic charts, indicating that the level of documentation has not improved over time. When children are ill enough to be hospitalized, one would expect growth assessment to be part of the routine history and physical examination. For the ward charts, only a weight documented from the ward scale was accepted because weights in the ED are frequently taken without removing shoes and street clothes. This may have underestimated the percentage of patients for whom weights were available; however, we felt that for inpatients who may require accurate serial weights, documentation on the ward scale was important. BMI, weight for height and growth charts were found in very few ward charts, even when height was measured. Because most paediatricians assess appropriateness of weight using a combination of the weight and height percentiles (5), this finding suggests that the nutritional status of the patients was not objectively assessed in the majority of cases. This is of concern given that 20% to 30% of children admitted to a tertiary care children’s hospital may have acute or chronic malnutrition (7) and given the rising incidence of overweight in Canadian children (6). In addition, the absence of readily accessible growth charts in the child’s permanent hospital record makes tracking of weight, height and BMI over time difficult.
In the ED, weight was documented in most patients, unlike in one previous report from the United Kingdom (4). Heights, and hence BMIs, or weights for height were never documented in the ED. This may have been due, in part, to a lack of a measuring board and stadiometer. However, before this audit, there had been no request for such equipment to be placed in the ED, suggesting that the value and importance of height and BMI or weight for height as part of a standard health assessment has been overlooked in this setting for some time. It could be argued that given the rapid turnover of patients with acute illness, these measurements are not the health care priority at the time. However, just as a simple blood pressure measurement can detect unsuspected hypertension, measuring height and weight and calculating BMI for age can indicate nutritional excess or inadequacy and the need for intervention.
Regular measuring and charting of height and weight is generally recommended as part of the routine health assessment of children (8). While single measurements are helpful, the best information is derived from serial measurements over time. When children attend a tertiary care paediatric hospital and are not measured, an opportunity has been lost to document health information that may be important in future health assessments, particularly because many children may see a family physician or paediatrician infrequently. It also represents a lost opportunity to educate families about growth and reinforce the importance of healthy eating and activity levels.
Another concern that is highlighted by the results of this audit relate to the health centre’s function as a teaching institution. If growth parameters are not being measured and growth charts are not being used, then appropriate paediatric assessments are not being modelled for medical students and other trainees.
The results of this audit show that when introducing the 2000 CDC growth charts into our health centre, we will need to do more than provide the new charts and education around BMI. The question of why growth parameters are being documented so infrequently must be asked. Although we did not assess this issue in our audit, discussion of the results among our colleagues suggested some reasons, including perceived lack of time or relevance to the immediate health concern, lack of equipment and unclear delineation of roles. This is being addressed in our health centre by rewriting the hospital policy on growth assessment and linking the implementation of the new policy with the introduction of the 2000 CDC growth charts. Measurement equipment in all areas of the hospital is being reviewed to ensure ease of access to the appropriate equipment. In addition, promotion of the importance of documenting growth parameters is being highlighted in various forums, including grand rounds, trainee teaching sessions, and nursing in-services and orientations.
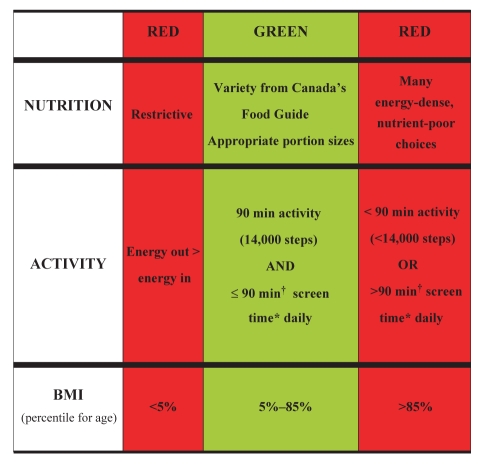
Another concern raised was a lack of tools to constructively address deviations from the normal range of BMI for age if they are detected. This concern led us to develop the concept of the “Green Zone” (Figure 1). Interpreting these data in the context of the Green Zone may help to clarify and highlight the relevance and importance of these measurements and the discussion of healthy eating and activity to staff, patients and families.
Figure 1.
Green Zone for Healthy Active Living – Children and Youth. *Screen time: television, video, video games and recreational computer; †60 min or less for preschoolers. BMI Body mass index
We feel it is essential that counselling regarding BMI be linked to both healthy eating and healthy activity levels. In addition to objective measurements of height and weight, a child’s level of activity and quality of diet must be taken into consideration when assessing health. The Green Zone tool is used to conceptualize this approach to health and points out that to be at either extreme of the spectrum in any one parameter (ie, in a red zone) is unhealthy. It includes green zones that encompass healthy levels of activity (9,10), acceptable levels of inactivity (9), healthy amounts and types of food, and a healthy range for BMI (1). On either side of this green zone are red zones that identify unhealthy amounts of activity (either too little or too much), unhealthy food choices in volume and quality, and unhealthy BMIs, either below the 5th percentile or above the 85th percentile (1). Within the red zones, there is variability such that BMI values in the overweight range (between the 85th and 95th percentiles) are associated with risk, but these risks may be lower than for those with a BMI above the 95th percentile. Similarly, a child who achieves 45 min of daily activity is better off than one who walks for 10 min a day. A child who regularly participates in 90 min of activity each day but also is consuming a diet high in energy-dense, nutrient-poor choices with a BMI in the 90th percentile would be in the green zone for activity and in the red zone for diet and BMI. Using this tool, counselling may be focused on changes in diet while encouraging maintenance of activity. It is important to emphasize that even those children with a BMI in the green zone may fall within the red zone for diet or activity or both, indicating that they, too, are at risk for health problems (9,11). Conversely, a child who is in the red zone for BMI but after careful assessment is shown to be in the green zones for diet and activity may be at a lower health risk and should be encouraged to continue with healthy eating and activity patterns.
When a child is found to be within one of the red zones, brief counselling interventions (12) and tools, such as nutritional or activity handouts, can be provided to assist the child and family to make choices that will move them toward the green zones for activity and nutrition, with a goal of maintaining better health and moving toward a healthier BMI. Resources are available from a variety of organizations including the CPS (Healthy Kids, Active Kids [<www.cps.ca/english/proadv/HAL/practicetools.htm>]), Health Canada (Canada’s Physical Activity Guide to Healthy Active Living [<www.paguide.com>]) and Dietitians of Canada (Eat Well, Play Well [<http://www.dietitians.ca/english/frames.html>]). It is important to note that change must be gradual; inactive children should be advised to start by increasing their current activity by 30 min per day, with at least 10 min of vigorous activity, and advance from there in 15 min increments monthly (9). Older children and teens may wish to use a pedometer or step counter and set goals to gradually increase their steps to 14,000 steps per day (10). For children who fall in the red zone for all three parameters, more aggressive interventions may need to be considered. We are in the process of carrying out further work to evaluate the application of the Green Zone concept, but on first pass, a number of health care providers in our centre have commented favourably on its utility.
ACKNOWLEDGEMENTS
The authors would like to thank the wards and emergency department at the IWK Health Centre who facilitated the performance of this audit. The authors would also like to thank Dr Noni MacDonald and the Healthy Eating Active Lifestyles Team at the IWK for their support and input.
REFERENCES
- 1.A collaborative statement from Dietitians of Canada, Canadian Paediatric Society, The College of Family Physicians of Canada and Community Health Nurses Association of Canada. Use of growth charts for assessing and monitoring growth in Canadian infants and children: Executive summary. Paediatr Child Health. 2004;9:171–3. doi: 10.1093/pch/9.3.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krebs NF, Jacobson MS American Academy of Pediatrics Committee on Nutrition. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 3.Meyers A. Audit of medical records from pediatric specialty clinics. Pediatrics. 1973;51:22–5. [PubMed] [Google Scholar]
- 4.Greig A, Ryan J, Glucksman E. How good are doctors at estimating children’s weight? J Accid Emerg Med. 1997;14:101–3. doi: 10.1136/emj.14.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perrin EM, Flower KB, Ammerman AS. Body mass index charts: Useful yet underused. J Pediatr. 2004;144:455–60. doi: 10.1016/j.jpeds.2004.01.047. [DOI] [PubMed] [Google Scholar]
- 6.Canadian Institute for Health Information . Canadian Population Health Initiative Summary Report: Improving the Health of Canadians. 2004 < http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=PG_39_E&cw_topic=39&cw_rel=AR_322_E> (Version current at August 2, 2005)
- 7.Hendricks KM, Duggan C, Gallagher L, et al. Malnutrition in hospitalized pediatric patients. Current prevalence. Arch Pediatr Adolesc Med. 1995;149:1118–22. doi: 10.1001/archpedi.1995.02170230072010. [DOI] [PubMed] [Google Scholar]
- 8.Needlman RD. Assessment of growth. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson Textbook of Pediatrics. 17th edn. Philadelphia: WB Saunders Company; 2004. pp. 58–62. [Google Scholar]
- 9.Canadian Paediatric Society, Advisory Committee on Healthy Active Living for Children and Youth. Healthy active living for children and youth. Paediatr Child Health. 2002;7:339–45. [Google Scholar]
- 10.Tudor-Locke C. Taking steps toward increased physical activity: Using pedometers to measure and motivate. President’s Council on Physical Fitness and Sports Research Digest. 2002;3:1–8. [Google Scholar]
- 11.World Health Organization. Diet, nutrition and the prevention of chronic diseases: Report of a joint WHO/FAP expert consultation. < http://www.who.int/dietphysicalactivity/publications/trs916/en/> (Version current at August 2, 2005)
- 12.Whitlock EP, Orleans CT, Pender N, Allan J. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am J Prev Med. 2002;22:267–84. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]