Abstract
Background/Objectives:
The use of multimicronutrient (MMN) supplementation to reduce the burden of anaemia in non-pregnant women of reproductive age has been little studied, particularly in Africa. The objective of the study was to evaluate haematological outcomes in non-pregnant, rural Gambian women of reproductive age, receiving daily MMN supplements for one-year.
Subjects/Methods:
The study in 293 women aged from 17 to 45 years old was nested within a double-blind, randomised placebo-controlled trial of periconceptional MMN supplementation [ISRCTN 13687662], using the United Nations International Multiple Micronutrient Preparation (UNIMMAP), received daily for one year or until conception. Red cell parameters and free erythrocyte protoporphyrin concentration were measured at baseline and after 12-months in those women who did not conceive.
Results:
Anaemic women (haemoglobin concentration <12g/dL) were more likely to be older and in economic deficit at baseline. Mean change in haemoglobin concentration was +0.6±1.4g/dL in the intervention arm and −0.2±1.2g/dL in the placebo arm (p<0.001). After supplementation with MMN the relative risk of anaemia (<12g/dL) was 0.59 (0.46, 0.76) compared to placebo. Anaemic subjects at baseline showed an increase in mean haemoglobin from 10.6g/dL to 11.8g/L (p<0.001) after MMN supplementation.
Conclusion:
MMN supplementation should be considered as a strategy for improving the micronutrient and haematological status of non-pregnant women of reproductive age.
Keywords: anaemia, non-pregnant women, micronutrients, supplementation, Gambia
INTRODUCTION
Many women in low-income countries suffer from sub-optimal micronutrition as a consequence of eating diets which are often low in animal-source foods and which do not meet dynamic micronutrient requirements throughout the reproductive lifecycle (Bartley et al 2005). Although iron deficiency is the commonest cause of nutritional morbidity worldwide (Stoltzfus 2003), in women of reproductive age concurrent deficiencies of vitamins A, C, B and folate also frequently occur and all contribute to an increased anaemia risk (Huffman SL et al 1998). The prevention of multiple micronutrient deficiencies as a strategy to reduce the risk of prenatal anaemia has been little studied and attention has tended to focus instead on iron supplementation during pregnancy, with conflicting results (Reveiz et al 2007) . There are few large intervention trials of multiple micronutrient supplementation in non-pregnant women of reproductive age and none have been conducted in Africa.
In The Gambia, as in other parts of sub-Saharan Africa, seasonal multiple micronutrient deficiencies are common (Bates et al 1984, Powers and Bates 1987), and maternal anaemia and its sequelae remain frequent problems, particularly in rural areas (Powers and Bates 1987, Topley 1968). In order to assess the effectiveness of MMN supplementation in anaemia prevention in rural Gambian women, we analysed a sub-sample of participants enrolled as part of a large MMN, placebo-controlled supplementation trial.
MATERIALS/SUBJECTS AND METHODS
Study design and intervention
The current study was nested within the Periconceptional Multimicronutrient Supplementation Trial (PMMST) [ISRCTN 13687662], based in 31 rural Gambian villages of Kiang West under demographic surveillance by the UK Medical Research Council field station in Keneba and which ran between February 2005 and June 2008. Between March and July 2006, resident females aged 17-45y were identified from the demographic database and pre-randomised to receive daily supplementation with UNIMMAP or placebo. For ease of administration in the field, randomisation was to one of four colour-coded groups (2 for intervention; 2 for placebo), stratified by age. Researchers were blinded to subject allocation scheme and subjects and field staff knew only the colour-coded allocation groups. UNIMMAP is a balanced preparation of 15 vitamins and minerals formulated by an Expert Committee of the United Nations Children's Fund, World Health Organization and the United Nations University, primarily for use by pregnant and lactating women. The composition of UNIMMAP is shown in Table 1 (UNICEF/WHO/UNU 1999). Eligible females were invited to attend a recruitment clinic where informed consent was sought in writing from individuals or guardians, in the cases of girls under 18-years old. Consenting non-pregnant women who were menstruating, not breastfeeding an infant, not using contraception or not severely anaemic (haemoglobin concentration < 7g/dL) were included in the trial. Exclusions were referred for clinical management as required. Women received 30 tablets according to their allocated intervention group and were instructed to take one tablet daily. They were also asked to attend weekly supplementation clinics held in their own villages when they were re-supplied with supplements. Compliance with supplementation was assessed by pill counts (compliance factor=ratio of the number of tablets apparently consumed / number of days enrolled in study). Information on morbidity and menstrual patterns was also recorded at these visits. Subjects were asked to notify fieldworkers of suspected pregnancy and following confirmation of pregnancy by study midwives, women were instructed to stop supplementation and no further supplements were issued. These women received a standard antenatal preparation of 60mg elemental iron and 250μg of folic acid daily. They were followed in the antenatal study clinic at regular intervals until delivery. Women who did not conceive while enrolled in PMMST, had received at least one year of MMN supplementation or placebo and were still resident in the selected villages in Kiang West, were eligible for inclusion in the current study. Data collection for the current study took place between July and August 2007.
Table 1.
Composition of the United Nations International Multiple Micronutrient Preparation (UNIMMAP)
| Micronutrient | Dose* |
|---|---|
| Vitamin A | 800RE |
| Vitamin D | 200IU |
| Vitamin E | 10mg |
| Vitamin C | 70mg |
| Vitamin B1 | 1.4mg |
| Vitamin B2 | 1.4mg |
| Niacin | 18mg |
| Vitamin B6 | 1.9mg |
| Vitamin B12 | 2.6mg |
| Folic Acid | 400μg |
| Iron | 30mg |
| Zinc | 15mg |
| Copper | 2mg |
| Selenium | 65μg |
| Iodine | 150μg |
Doses are based on US/Canadian recommended daily allowances in pregnancy(UNICEF/WHO/UNU 1999).
Permission for this study was obtained from the London School of Hygiene and Tropical Medicine Ethics Committee and the Gambian Government/MRC Joint Ethics Committee. The parent-trial was subjected to the scrutiny of an independent Data Safety and Monitoring Board and operated under the auspices of Good Clinical Practice guidelines (MRC 1999). MRC Keneba offers free primary health care to anyone who consults, in collaboration with the Gambian Government Lower River Divisional Health Team. Apart from the structured clinical contacts outlined (during which subjects were given transport and a meal) no additional benefits were provided to trial participants.
Study location and population
Kiang West is a semi-arid area of savannah-scrubland with a rural population of 14 000 people, predominantly of the Mandinka tribe. HIV status was not assessed during this study but national sentinel data from antenatal clinics indicates a HIV prevalence of around 1% (Schim van der Loeff et al 2003). The sub-sample was drawn from 12 of the original 31 villages, chosen on the grounds of their larger size and easier accessibility. They included the core research villages of the Keneba, Kanton Kunda and Manduar and 9 of the villages to the east and west of Keneba. This provided a broad yet manageable sample frame from within the original trial cohort, given the logistical constraints under which the current study was carried out. Consenting subjects who were present in the village on an allotted day were recruited. Anthropometry and blood samples were collected from participants during village visits
Sample size
Mean recruitment haemoglobin for the PMMST study was 11.7 g/dL, (SD 1.5 g/dL) for a population of 1156. A sample of 150 for each trial arm was required in order to detect a change in haemoglobin of 0.5 g/dL between study arms with 5% significance and 80% power.
Data and sample collection
Individual informed consent was obtained in the local language by Gambian MRC fieldworkers. A thumbprint was requested from women who were unable to write. An information sheet in English was provided for women to take away. A questionnaire assessing marital status and socioeconomic status was carried out. Economic situation was assessed by ownership of radio and/or bicycle and information on perceived economic status. Participants were asked whether they considered the household's economic situation in the preceding year to have been always in deficit, occasionally deficit, balanced or surplus. A household was categorised as in ‘economic deficit’ if the subject answered either always deficit or occasionally deficit (Hyder et al 2004). A one-week dietary history, menstrual and medical history was completed for each subject. A stool sample was requested and sterile universal containers provided at the study visit following the trial. At initial recruitment within the main study baseline stool samples had not been collected. Venous blood was placed in EDTA, sedivette and serum tubes (Sarstedt Monovette, UK). Height was measured to the nearest cm using a stadiometer (Seca Leicester, UK), and weight to the nearest 100 g using an electronic scale (Tanita, USA). Mid-upper arm circumference (MUAC) was measured at the mid-point of the left arm using standard tapes (TALC, UK). Data were double entered into the MRC Keneba database (MS Access, Microsoft, USA).
Laboratory analysis
Haematological analysis included haemoglobin concentration, white blood cell count, mean cell volume (MCV), mean cell haemoglobin (MCH), reticulocyte count (Cel-Dyn 3700 Analyser, Abbott Diagnostics, USA and Medonic CA530, Clinical Diagnostic Solutions, Inc., USA), and zinc protoporphyrin concentration (ZnPP) (AVIV ZP Hematofluorometer Model 206, Analis Scientific Instruments, Belgium). The erythrocyte sedimentation rate (ESR) (Sarstedt, UK) and C-reactive protein (CRP) (Vitros system 250, Johnson & Johnson, USA) were measured. Malaria blood films were prepared and stained with giemsa stain and 100 microscopic fields examined to determine parasite count. Wet stool samples were prepared for examination by light microscopy for the presence of helminths.
Both Cell-dyn and Medonic CA530 analysers were used for processing of haematological samples due to a technical fault with the Cell-dyn machine. The correlation coefficient between the results for the two machines was 0.96 (p<0.001).
Statistical analysis
Data was blinded until completion of the analysis, which was performed on an intention-to-treat basis. Data were processed and analysed using SPSS for Windows v15. Log transformation was used for non-normal distributions. Anaemia was defined as hemoglobin concentration less than 12 g/dL (UNICEF/WHO/UNU 2001). Mean haemoglobin concentration change (baseline to follow-up) was compared between treatment groups with analysis of covariance. Variables which did not require adjustment for baseline values were compared using an independent t-test for continuous variables, Wilcoxon ranksum for non normally distributed variables (CRP) and a chi-squared test of proportions for categorical variables. The odds ratio (OR) and relative risk (RR) for anaemia in relation to MMN supplement, age and ESR were computed using logistic regression. Differences were considered significant at p<0.05.
RESULTS
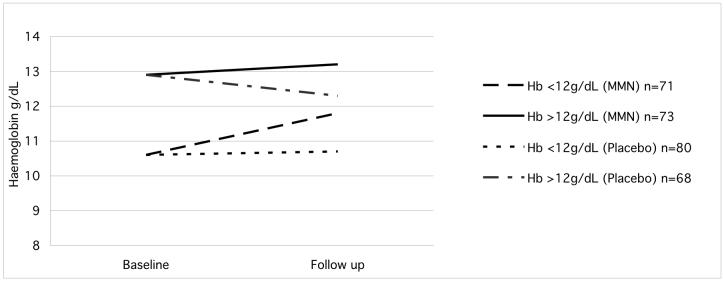
Of 1156 women recruited for the original trial 421 were considered to be eligible for the current study according to the criteria above. Of these 293 subjects were identified and recruited (Figure 1). Subjects who could not be traced by the field teams or who did not attend after direct invitation were not recruited (n=128). Baseline characteristics of recruited (n=293) and non-recruited (n=128) women are summarised in Table 2. Untraced women were more likely to be nulliparous, to have lower mean anthropometric indices and were more likely to have received formal schooling. There were no differences in haematological parameters. Baseline characteristics of the intervention and placebo groups were not different except for total white cell concentration at baseline (Table 3). The estimate of compliance did not differ between treatment groups (MMN: 0.96 ± 0.18; placebo: 0.92 ± 0.19, p=0.15). The mean time of follow up was similar in both groups (MMN: 14.1 ± 1.2 months, placebo 14.0 ± 1.2 months). Baseline predictors of anaemia, after adjustment (Table 4), included older age OR= 2.01 (1.16, 3.48) and economic deficit OR=1.98 (1.21, 3.25).
Figure 1.
Trial Profile: subjects entering PMMST and further enrolment into the haematological sub-study
Table 2.
Characteristics of recruited and non-recruited eligible subjects prior to intervention period
| Untraced Women n=128 |
Traced Women n=293 |
p value | |
|---|---|---|---|
|
| |||
| Characteristics | |||
| Age (yrs) | 25.2±7.9 | 32.4±8.7 | <0.001 |
| BMI (kg/m2) | 21.1±3.2 | 22.3±4.4 | 0.03 |
| Weight (kg) | 54.6±9.5 | 57.1±11.5 | 0.007 |
| MUAC (mm) | 259.5±28.6 | 268.9±37.9 | 0.012 |
| Proportion nulliparous 1 | 0.66(0.58,0.74) | 0.30(0.25,0.35) | <0.001 |
| Formal schooling1 (proportion) | 0.33(0.24,0.41) | 0.10(0.07,0.13) | <0.001 |
| Meat or fish eaten (d/wk) | 3.9±2.0 | 4.5±1.8 | 0.04 |
| Haemoglobin2 (g/dL) | 11.9±1.5 | 11.7±1.5 | 0.18 |
| MCV2 (fl) | 80.6±8.02 | 81.7±7.91 | 0.22 |
| MCH2 (pg) | 27.6±3.3 | 27.9±3.28 | 0.30 |
| ZnPP2,3 (μmol/mol heme) | 97.9(87.5,109.3) | 87.9(79.3,97.3) | 0.09 |
| Malaria film positive4 (no) | 0 | 3 | 0.89 |
| Totalwhite cells (×109/L) | 5.19±1.21 | 4.87±1.33 | 0.02 |
| Reticulocyte2 % | 1.64±0.68 | 1.58±0.52 | 0.30 |
Proportions and 95% confidence intervals given, Chi test performed
Only 127 in untraced group and 292 in traced group baseline haematological samples not being available
Geometric means
Only 127 in untraced group and 283 in traced group baseline samples not being available
Table 3.
Characteristics of subjects at baseline and after intervention
| Characteristics | MMN | Placebo | |||
|---|---|---|---|---|---|
| Baseline n=145 |
After intervention n=1421 |
Baseline n=148 |
After intervention n=148 |
p2 | |
| Age (yrs) | 33 ±8.6 | - | 34 ±8.8 | - | - |
| Proportion nulliparous 3 | 0.35(0.27,0.43) | - | 0.25(0.18,0.32) | - | - |
| Formal schooling3 (proportion) | 0.12(0.06, 0.17) | - | 0.09(0.04,0.13) | - | - |
| Meat or fish eaten (d/wk) | 4.6 ±1.8 | - | 4.4 ±1.8 | - | - |
| No of months in study | 14.1±1.2 | - | 14.0±1.2 | - | - |
| Malaria film positive4 (no) | 0 | 0 | 3 | 0 | - |
| BMI (kg/m2) | 22.4 ±5.0 | 23 ±5.2 | 22.1 ±3.8 | 22.6 ±4.2 | 0.49 |
| Weight (kg) | 57.4 ±12.1 | 59.0 ±12.9 | 56.7 ±10.9 | 58.0 ±11.8 | 0.49 |
| MUAC (mm) | 269.7 ±41.2 | 280.1 ±44.0 | 267.8 ±34.6 | 275.1 ±37 | 0.30 |
| Haemoglobin (g/dL) | 11.7 ±1.5 | 12.3 ± 1.1 | 11.6 ±1.5 | 11.5±1.4 | <0.001 |
| MCV (fl) | 81.2 ±8.5 | 81.9 ±6.2 | 82.1 ±7.3 | 80.6 ±7.2 | <0.001 |
| MCH (pg) | 27.8 ±3.5 | 32.0 ±3.9 | 28.1 ±3.1 | 32.0 ±4.4 | 0.76 |
| ZnPP5,6 (μmol/mol heme) | 89.5(86.0,93.0) | 54.0(52.2,56.8) | 86.4(82.8,90.0) | 72.2(68.5,75.9) | <0.001 |
| Totalwhite cells (×109/L) | 5.02±1.30 | 5.03 ±2.1 | 4.71±1.35 5.03 ±2.1 | 4.50 ±2.0 | 0.08 |
| Reticulocyte % | 1.64 ± 0.62 | 1.60 ±0.56 | 1.51 ± 0.40 | 1.56 ±0.41 | 0.04 |
| ESR7 (mm/hr) | - | 22 ±13.5 | - | 26 ±15.5 | 0.028 |
| CRP 9 | - | 0 | - | 0 | 0.73 |
142 samples as baseline sample not available for one subject, and 2 subjects did not have samples taken at follow up
Analysis of covariance unless otherwise stated. P-values refer to change in mean values between baseline and after intervention and not to the absolute values that are given in the table
Proportions and 95% confidence intervals given, Chi test performed
Fishers exact test
Only 144 subjects in MMN group at baseline as one sample not available
Geometric means given
Only 147 samples in placebo group due a to clotted sample
Student t-test
Non-parametric tests, Wilcoxon ranksum, median values quoted
Table 4.
Predictors of haemoglobin <12g/dL at baseline
| Odds Ratio (CI) | p | Adjusted Odds Ratio (CI) | p | |
|---|---|---|---|---|
| Age >35 yrs | 2.37 (1.54, 3.80) | <0.001 | 2.01 (1.16, 3.48) | 0.012 |
| Nulliparous | 0.48 (0.2, 0.80) | 0.005 | 0.74 (0.40, 1.32) | 0.29 |
| Economic deficit | 2.05 (1.27, 3.33) | 0.04 | 1.98 (1.21, 3.25) | 0.007 |
| MUAC (<21cm) | 1.22 (0.27, 5.54) | 0.799 | ||
| Meat (> once a week) | 0.53 (0.19, 1.50) | 0.23 | ||
| No formal schooling | 1.75 (0.81, 3.77) | 0.16 |
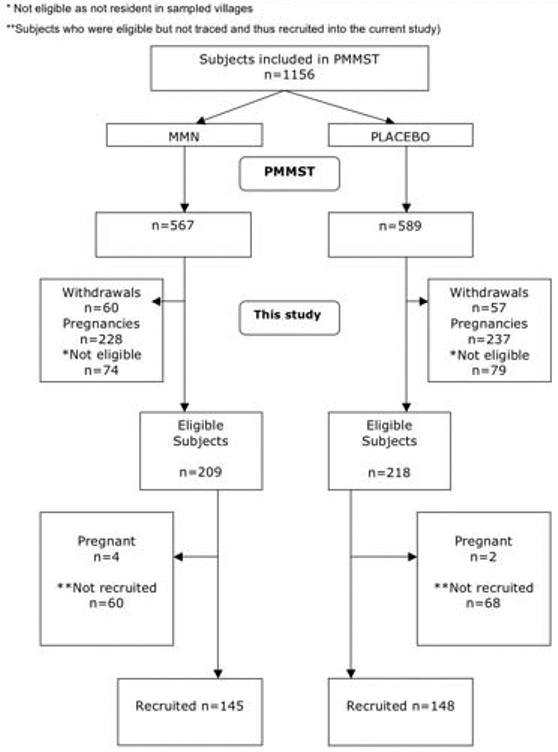
Following the intervention period mean haemoglobin concentration was higher in women receiving micronutrients (MMN: 12.3±1.1g/dL, placebo: 11.5±1.4g/dL) with a mean change in haemoglobin concentration of +0.6±1.4g/dL (MMN) and −0.2±1.2g/dL (placebo) (p<0.001). The increase in haemoglobin concentration in the intervention group relative to placebo was more marked in women who were anaemic at the start of the study (Figure 2). Although age and economic deficit were predictors of anaemia at baseline, in a sub analysis these groups did not respond differently to supplementation. Table 3 includes the haematological findings at follow up. Supplementation was associated with increased haemoglobin concentration and MCV and reduced ZnPP concentration (all p<0.001). The reduction in reticulocyte count was marginally significant (p=0.04). ESR was also noted to be lower in the MMN group than in the placebo group (22±13.5mm/hr versus 26±15.5mm/hr, p=0.02). Raised ESR values (>20mm/hr) were less frequent in supplemented women OR 0.71 (0.55, 0.91).
Figure 2.
Comparison of haemoglobin change in MMN and placebo groups in relation to baseline haemoglobin concentration
There were no differences in anthropometric indices (BMI, weight, and MUAC) between the two groups (Table 3). No subjects had malaria parasitaemia at follow-up. Median CRP was 0 mg/L for both groups and there were no differences in proportion of women with a raised CRP (>10g/L) in either group. Only one stool sample showed hookworm infection.
At baseline, anaemia prevalence was 50.7% (MMN group) and 54.1% (placebo group). Following supplementation these were 36% and 62% respectively, generating RR=0.59 (0.46, 0.76) for anaemia in the MMN group. Anaemia was less frequent in the MMN group (p<0.001) and more frequent in older women (p=0.01) and there was no significant interaction between age and intervention group.
There were no significant differences in combined or system-specific morbidity profiles between study groups (data not shown).
DISCUSSION
To our knowledge this is the first African trial to evaluate the effect of multiple micronutrient supplementation on red cell parameters and iron status among non-pregnant women of reproductive age. Twelve months of daily MMN supplementation significantly improved haemoglobin concentration in this group of women. The associated decrease in ZnPP concentration and increased MCV in supplemented women suggests that the iron content of the supplements underpinned the improved haematological profile, while the differences in reticulocyte count suggest a reduction in red cell turnover among MMN supplemented women. Anaemia prevalence was almost halved in supplemented women and anaemic women showed the greatest increase in haemoglobin concentration following supplementation (+1.2g/dL). This would be expected as subjects who are iron-depleted use iron more effectively than those who are iron-replete (Moriarty-Craige et al 2004).
ESR was measured in this study. ESR is a non-specific, indirect measurement of plasma acute-phase protein and systemic inflammatory status that is known to correlate with haemoglobin and plasma fibrinogen concentrations (Kanfer and Nicol 1997). It is influenced by the size, shape, and number of erythrocytes, as well as by other plasma constituents such as immunoglobulins (Brigden 1999, Gabay and Kushner 1999). Interpretation of the effect of supplementation on ESR is complex (Breckenridge and Okpanachi 1976) but the reduction in ESR following supplementation could indicate a ameliorating effect of MMN on systemic inflammation. However, there was no direct evidence that CRP concentration was affected by micronutrient supplementation. More detailed studies of inflammatory markers and MMN supplementation are required in order to understand their roles in the aetiology of anaemia in this population of women, particularly in areas of high malarial endemicity.
The study was restricted to a sub-sample of geographically selected villages but this does not appear to have biased the results of the study, as the placebo and intervention groups were comparable at baseline. The high compliance, regular follow-up and long duration of our study further increases confidence in the findings. The placebo control group allowed for an absolute evaluation of the effects of micronutrients on haematological parameters. The primary analysis was powered to assess changes in haemoglobin concentration, which limited the scope of this study to the functional effect of MMN supplementation on nutritional anaemia. This outcome represented a simple, clinically relevant measure of composite micronutrient status, achievable within the time and resource constraints under which the nested study was carried out. However an analysis of the effects of supplementation on broader micronutrient status in this population would have been of interest and is a specified outcome in the main trial, which will be reported elsewhere. There was a low prevalence of malaria parasitaemia in the current study, which is likely to have been a consequence of cross-sectional sampling of partially immune adults early in the wet season, in an area of highly seasonal endemicity. Although there was no difference in the rate of clinical infection diagnosis between the two arms of the parent trial, longitudinal malaria exposure may have been an effect modifier or confounding variable in this study and ought to be assessed formally in future work.
Iron deficiency is an important risk factor for increased maternal mortality, low birth weight and preterm delivery (Brabin et al 2001) and the availability of calcium, iodine, folate and vitamins A and D may modulate fetal development (Bartley et al 2005). In order to achieve Millennium Development Goals, new strategies to address nutritional problems in women of reproductive age are required. Several recent studies in poorer countries have already demonstrated improved parameters of fetal growth and gestational length with various prenatal MMN supplementation regimen, although effects have been inconsistent and the mechanisms of action are unclear (Christian et al 2003) (Kaestel et al 2005) (Fawzi et al 2007). There are concerns about possible detrimental interactions between micronutrients combined within a single supplement but experimental data are sparse and the potential synergistic and positive effects of particular combinations should not be ignored (Sandstrom 2001). The timing of supplementation may likewise be a crucial factor (Owens and Fall 2008). For example, the fact that prenatal folate supplementation substantially reduces the risk of neural tube defect only if it is taken preconceptually is well known but improving vitamin A status before pregnancy has also been shown to have a dramatic and as yet unexplained effect on maternal morbidity and mortality (West et al 1999). Optimising the pre- and inter-pregnancy micronutritional status of women, particularly in low resource settings could be extremely beneficial (Allen 2000, Bartley et al 2005, Huffman SL et al 1998, Owens and Fall 2008) and may lead to improved subsequent maternal and pregnancy outcomes.
Previous studies in Mexico and Bangladesh have shown no additional benefit on haematological parameters when women of reproductive age and adolescents were given MMN compared to iron-folate supplements (Ahmed et al 2005, Moriarty-Craige et al 2004). The duration of supplementation in these studies was short, different MMN formulations were used and sample sizes were smaller than in the present study. Neither trial utilised a placebo-controlled design, limiting the interpretation of the study results. The present study achieved a greater improvement in haemoglobin concentration and a greater decline in the prevalence of anaemia compared to these previous reports. The findings from the Bangladesh study did however provide additional support for the use of combinations of micronutrients in preference to iron alone, as the prevalence of other nutrient deficiencies including folic acid, riboflavin and vitamin B12, A and C were also decreased in addition to improved values for haematological parameters (Ahmed et al 2005).
In Indonesia, the haemoglobin concentration of adolescent girls improved on supplementation with combinations of iron, folic acid, retinol and vitamin C, over placebo but did not respond better to daily rather that weekly supplementation, although serum ferritin increased more in the daily supplemented group (Angeles-Agdeppa et al 1997). The intervention period was only 3-months, compared with 12-months in the present study, and there was a high dropout rate.
A study of Bangladeshi adolescents receiving a micronutrient fortified beverage 6d/week reported haematological effects which were of a similar magnitude to those in the current study (Hyder et al 2007). An increase in serum retinol and improved anthropometric status (weight, height, BMI) in supplemented girls was also recorded (Hyder et al 2007), indicating the potential benefits of MMN supplementation for a risk group attempting to satisfy increased nutritional requirements for pubertal growth while commonly manifesting a substantial degree of undernutrition. It has frequently been suggested that adolescents should be the focus of targeted intervention strategies which aim to improve reproductive health particularly before first pregnancies (Leenstra et al 2007). Although the issue of supplementation in younger women is critical, they may be difficult to target over a long period of time and may not begin their reproductive lives proximal to the supplementation period.
The number of adolescents in the present study was small (n=23) and conclusions cannot readily be drawn concerning the haematological responses of this sub-group. By contrast, subjects were generally older, better nourished, multiparous and poorly educated. Two-thirds of untraced women were nulliparous compared with one third of the traced women, characterising a group of younger, more mobile but less reproductively-active women, akin to that in the Bangladeshi study (Hyder et al 2007).
We have rather shown that older, anaemic multiparae who are experiencing recurrent demands of pregnancy and lactation under seasonally adverse conditions (Anya 2004, Billewicz and McGregor 1981) clearly benefit from MMN supplementation. The findings of this study provide evidence of the efficacy of MMN supplementation and support its promotion in non-pregnant women as a means of optimising haematological and micronutrient status in between pregnancies, especially in relation to iron status. Community antenatal and paediatric clinics, which often already serve these populations, can readily be used to identify those at particular risk on finger-prick testing and target them for supplementation.
There is now a small but growing body of data supporting the efficacy of prenatal multi-micronutrients in improving selected perinatal outcomes of women and babies in resource-poor settings. Studies specifically utilising UNIMMAP benefit from and contribute to datasets based on a uniform and targeted intervention, facilitating the interpretation and reproducibility of their results. Future studies should compare placebo, iron-folate and UNIMMAP supplementation in order to assess the efficacy and effectiveness of pre- or inter-pregnancy supplementation on later maternal anaemia and pregnancy outcome, as well as the impact on broader micronutrient status and other functional outcomes in this vulnerable group.
ACKNOWLEDGEMENTS
The authors would like to thank the PMMST field team, especially Ms. Fatou Sossey (Senior Midwife) and Mr. Baba Jobarteh (Field Supervisor), and Dr. Sophie Moore (Head of Station, MRC Keneba) for their logistical support to the project. The study was funded from the programme grant to the MRC International Nutrition Group, London School of Hygiene and Tropical Medicine.
REFERENCES
- Ahmed F, Khan MR, Akhtaruzzaman M, Karim R, Marks GC, Banu CP, et al. Efficacy of twice-weekly multiple micronutrient supplementation for improving the hemoglobin and micronutrient status of anemic adolescent schoolgirls in Bangladesh. Am J Clin Nutr. 2005;82:829–835. doi: 10.1093/ajcn/82.4.829. [DOI] [PubMed] [Google Scholar]
- Allen LH. Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr. 2000;71:1280S–1284S. doi: 10.1093/ajcn/71.5.1280s. [DOI] [PubMed] [Google Scholar]
- Angeles-Agdeppa I, Schultink W, Sastroamidjojo S, Gross R, Karyadi D. Weekly micronutrient supplementation to build iron stores in female Indonesian adolescents. Am J Clin Nutr. 1997;66:177–183. doi: 10.1093/ajcn/66.1.177. [DOI] [PubMed] [Google Scholar]
- Anya SE. Seasonal variation in the risk and causes of maternal death in the Gambia: malaria appears to be an important factor. Am J Trop Med Hyg. 2004;70:510–513. [PubMed] [Google Scholar]
- Bartley KA, Underwood BA, Deckelbaum RJ. A life cycle micronutrient perspective for women's health. Am J Clin Nutr. 2005;81:1188S–1193S. doi: 10.1093/ajcn/81.5.1188. [DOI] [PubMed] [Google Scholar]
- Bates CJ, Villard L, Prentice AM, Paul AA, Whitehead RG. Seasonal variations in plasma retinol and carotenoid levels in rural Gambian women. Trans R Soc Trop Med Hyg. 1984;78:814–817. doi: 10.1016/0035-9203(84)90028-2. [DOI] [PubMed] [Google Scholar]
- Billewicz WZ, McGregor IA. The demography of two West African (Gambian) villages, 1951--75. J Biosoc Sci. 1981;13:219–240. doi: 10.1017/s0021932000013390. [DOI] [PubMed] [Google Scholar]
- Brabin BJ, Hakimi M, Pelletier D. An analysis of anemia and pregnancy-related maternal mortality. J Nutr. 2001;131:604S–614S. doi: 10.1093/jn/131.2.604S. discussion 614S-615S. [DOI] [PubMed] [Google Scholar]
- Breckenridge MA, Okpanachi E. The erythrocyte sedimentation rate in healthy North Nigerian university students. Afr J Med Med Sci. 1976;5:221–227. [PubMed] [Google Scholar]
- Brigden ML. Clinical utility of the erythrocyte sedimentation rate. Am Fam Physician. 1999;60:1443–1450. [PubMed] [Google Scholar]
- Christian P, Khatry SK, Katz J, Pradhan EK, LeClerq SC, Shrestha SR, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. Bmj. 2003;326:571. doi: 10.1136/bmj.326.7389.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawzi WW, Msamanga GI, Urassa W, Hertzmark E, Petraro P, Willett WC, et al. Vitamins and perinatal outcomes among HIV-negative women in Tanzania. N Engl J Med. 2007;356:1423–1431. doi: 10.1056/NEJMoa064868. [DOI] [PubMed] [Google Scholar]
- Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448–454. doi: 10.1056/NEJM199902113400607. [DOI] [PubMed] [Google Scholar]
- Huffman SL, Shumann J, ER Z. The case for promoting multiple vitamin/mineral supplements for women of reproductive age in developing countries. The LINKAGES Project. 1998 [Google Scholar]
- Hyder SM, Persson LA, Chowdhury M, Lonnerdal BO, Ekstrom EC. Anaemia and iron deficiency during pregnancy in rural Bangladesh. Public Health Nutr. 2004;7:1065–1070. doi: 10.1079/PHN2004645. [DOI] [PubMed] [Google Scholar]
- Hyder SM, Haseen F, Khan M, Schaetzel T, Jalal CS, Rahman M, et al. A multiple-micronutrient-fortified beverage affects hemoglobin, iron, and vitamin A status and growth in adolescent girls in rural Bangladesh. J Nutr. 2007;137:2147–2153. doi: 10.1093/jn/137.9.2147. [DOI] [PubMed] [Google Scholar]
- Kaestel P, Michaelsen KF, Aaby P, Friis H. Effects of prenatal multimicronutrient supplements on birth weight and perinatal mortality: a randomised, controlled trial in Guinea-Bissau. Eur J Clin Nutr. 2005;59:1081–1089. doi: 10.1038/sj.ejcn.1602215. [DOI] [PubMed] [Google Scholar]
- Kanfer EJ, Nicol BA. Haemoglobin concentration and erythrocyte sedimentation rate in primary care patients. J R Soc Med. 1997;90:16–18. doi: 10.1177/014107689709000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leenstra T, Kariuki SK, Kurtis JD, Oloo AJ, Kager PA, Ter Kuile FO. The effect of weekly iron and vitamin A supplementation on hemoglobin levels and iron status in adolescent schoolgirls in western Kenya. Eur J Clin Nutr. 2007 doi: 10.1038/sj.ejcn.1602919. [DOI] [PubMed] [Google Scholar]
- Moriarty-Craige SE, Ramakrishnan U, Neufeld L, Rivera J, Martorell R. Multivitamin-mineral supplementation is not as efficacious as is iron supplementation in improving hemoglobin concentrations in nonpregnant anemic women living in Mexico. Am J Clin Nutr. 2004;80:1308–1311. doi: 10.1093/ajcn/80.5.1308. [DOI] [PubMed] [Google Scholar]
- Owens S, Fall CH. Consequences of poor maternal micronutrition before and during early pregnancy. Trans R Soc Trop Med Hyg. 2008;102:103–104. doi: 10.1016/j.trstmh.2007.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers HJ, Bates CJ. Micronutrient deficiencies in the aetiology of anaemia in a rural area in The Gambia. Trans R Soc Trop Med Hyg. 1987;81:421–425. doi: 10.1016/0035-9203(87)90157-x. [DOI] [PubMed] [Google Scholar]
- Reveiz L, Gyte GM, Cuervo LG. Treatments for iron-deficiency anaemia in pregnancy. Cochrane Database Syst Rev. 2007:CD003094. doi: 10.1002/14651858.CD003094.pub2. [DOI] [PubMed] [Google Scholar]
- Sandstrom B. Micronutrient interactions: effects on absorption and bioavailability. Br J Nutr. 2001;85(Suppl 2):S181–185. [PubMed] [Google Scholar]
- Schim van der, Loeff MF, Sarge-Njie R, Ceesay S, Awasana AA, Jaye P, Sam O, et al. Regional differences in HIV trends in The Gambia: results from sentinel surveillance among pregnant women. AIDS. 2003;17:1841–1846. doi: 10.1097/01.aids.0000076303.76477.49. [DOI] [PubMed] [Google Scholar]
- Stoltzfus RJ. Iron deficiency: global prevalence and consequences. Food Nutr Bull. 2003;24:S99–103. doi: 10.1177/15648265030244S206. [DOI] [PubMed] [Google Scholar]
- Topley E. Common anaemia in rural gambia. II. Iron deficiency anaemia among women. Trans R Soc Trop Med Hyg. 1968;62:595–601. doi: 10.1016/0035-9203(68)90108-9. [DOI] [PubMed] [Google Scholar]
- UNICEF/WHO/UNU Composition of a multi-micronutrient supplement to be used in pilot programmes among pregnant women in developing countries. 1999 Report of an UNICEF/WHO/UNU workshop. [Google Scholar]
- UNICEF/WHO/UNU Iron Deficiency Anaemia Assessment, Prevention and Control: A guide for programme managers. 2001 [Google Scholar]
- West KP, Jr., Katz J, Khatry SK, LeClerq SC, Pradhan EK, Shrestha SR, et al. Double blind, cluster randomised trial of low dose supplementation with vitamin A or beta carotene on mortality related to pregnancy in Nepal. The NNIPS-2 Study Group. Bmj. 1999;318:570–575. doi: 10.1136/bmj.318.7183.570. [DOI] [PMC free article] [PubMed] [Google Scholar]