Abstract
Crystalline lithium phthalocyanine (LiPc) can be used to sense oxygen. To enhance biocompatibility/stability of LiPc, we encapsulated LiPc in Teflon AF (TAF), cellulose acetate (CA), and polyvinyl acetate (PVAc) (TAF, previously used to encapsulate LiPc, was a comparator). We identified water-miscible solvents that don’t dissolve LiPc crystals, but are solvents for the polymers, and encapsulated crystals by solvent evaporation. Oxygen sensitivity of films was characterized in vitro and in vivo. Encapsulation did not change LiPc oximetry properties in vitro at anoxic conditions or varying partial pressures of oxygen (pO2). EPR linewidth of encapsulated particles was linear with pO2, responding to pO2 changes quickly and reproducibly for dynamic measurements. Encapsulated LiPc was unaffected by biological oxidoreductants, stable in vivo for four weeks. Oximetry, stability and biocompatibility properties of LiPc films were comparable, but both CA and PVAc films are cheaper, and easier to fabricate and handle than TAF films, making them superior.
Keywords: Oximetry, Electron Paramagnetic Resonance, Lithium pthalocyananine, Spin probes, EPR
1 Introduction
Abnormal oxygen concentration is implicated in many pathophysiological conditions including ischemic diseases, reperfusion injury, and oxygen toxicity (Kulkarni et al. 2007; Kutala et al. 2007). A noninvasive technique to accurately and repetitively measure tissue oxygenation would find broad applications in clinical and basic research. Accurate, real-time oximetry could also improve clinical management in multiple disease states and conditions including cancer, transplantation, cardiovascular disease and wound healing.
Many methods are available to measure oxygen concentration, but none is completely satisfactory (Springett and Swartz 2007; Vikram et al. 2007). Nonetheless, electron paramagnetic resonance (EPR)-based oximetry, using paramagnetic crystalline (particulate) probes, has distinct advantages (Gallez and Swartz 2004; Swartz 2004). Advantages of particulate probes for EPR oximetry include: (1) their ability to report partial pressure of oxygen (pO2), rather than dissolved oxygen concentration or oxygen saturation; (2) their ability to measure tissue oxygen without consuming it, and (3) their capacity for high resolution oximetry at low pO2. Particulate probes show a single-line EPR spectrum that is highly exchange-narrowed (Ilangovan et al. 2004a, b; Ilangovan et al. 2002a; Liu et al. 1993; Pandian et al. 2003b). Linewidth is sensitive to the concentration of molecular oxygen showing a linear relationship to pO2. Lithium phthalocyanine (LiPc) probes are widely used reporters of oxygen concentration and depend on their micro- to nanoscale crystalline morphologies for their oximetry properties (Ilangovan et al. 2000b; 2001; 2004a, b; 2000a, b; Liu et al. 1993; Sostaric et al. 2006). Other particulate paramagnetic spin probes used in oximetry include derivatives of lithium phthalocyanine and napthalocyanine (Bratasz et al. 2006; 2007; Fujii et al. 2007; Kutala et al. 2004; Pandian et al. 2003a, b; 2005; 2006a, b; 2007; Pandian and Kuppusamy, unpublished results; Wisel et al. 2007) and carbon blacks (Lan et al. 2004). However, biocompatibility, long-term in vivo stability, and oxygen responsiveness of some particulate probes are compromised over time in vivo (Jiang et al. 2001), and encapsulation into biocompatible polymeric matricies has been pursued to mitigate these limitations, (Gallez et al. 1999; He et al. 2001).
The simplest method for LiPc polymer encapsulation is solvent evaporation. Oximetry properties of the LiPc is dependent on its crystalline structure (Sugimoto et al. 1986), so the solvent must not dissolve the LiPc crystals. We report novel solvent/polymer systems for LiPc encapsulation resulting from systematic screening polymer/LiPc solubilities. We investigated multiple solvents and polymeric materials beyond those already reported in the literature (Gallez et al. 1999; He et al. 2001; Jiang et al. 2001; Dinguizli et al 2006), to broaden the choice of polymers that might be used for LiPc encapsulation. This will allow investigators to consider polymer parameters (cost, handling properties and mechanical properties, etc.) in design and optimization of implantable/retrievable oximetry films. We present analysis of various solvents and polymers for their suitability for encapsulation of LiPc; we also present in vitro and in vivo evaluation of oximetry properties of encapsulated LiPc particles, and demonstrate multi-week stability of oximetry properties of encapsulated LiPc.
2 Materials and methods
2.1 Materials
Lithium phthalocyanine (LiPc) radical was synthesized and characterized in our laboratory (Ilangovan et al. 2000a; Ilangovan et al. 2000b) (Fig. 1). N-methyl-2-pyrrolidone (NMP), tetrahydrofurfuryl alcohol (THFA), ethylene glycol dimethyl ether (EGDE), ethyl lactate (EtL), dimethyl sulfoxide (DMSO), glycerol formal (GF), Fluorinert FC-40, Fluorinert FC-77, hexaflurobenzene (HFB), polyviny-lacetate (PVAc), cellulose acetate (CA), Teflon AF 2400 (TAF), polyvinyl formal, cellulose acetate butyrate and polyvinylchloride were purchased from Sigma (St. Louis, MO, USA).
Fig. 1.
Molecular structure of lithium phthalocyanine (LiPc) radical and polymer films Teflon AF 2400 (TAF), polyvinyl acetate (PVAc) and cellulose acetate (CA)
2.2 Solvent solubility screening tests for LiPc and polymeric materials
The LiPc particulate spin probes were exposed to different biocompatible, water-miscible organic solvents (NMP, THFA, EGDE, EtL, DMSO, GF FC-40, FC-77 and HFB) for water-insoluble biomedical polymeric materials (cellulose acetate, poly vinyl acetate, polyvinyl formal and Teflon AF 2400). The solvents were used as is or mixed with water (90:10, v/v solvent:water, respectively). Aliquots of LiPc (5 mg) were incubated for at least 24 h at room temperature in 200 µL of each solvent to determine LiPc solubility. LiPc was considered insoluble if, at the end of 24 h, LiPc crystals were still present and the solvent remained uncolored by dissolved LiPc (LiPc is blue in color). For the polymers, 0.5 ml of each solvent was incubated with 0.025 g of polymer (for PVA 0.048 g was used) at room temperature for up to 4 h with occasional vortexing. Polymers were considered soluble if solid polymer was no longer detectable after incubation. Teflon AF 2400 was prepared at 2.5 wt.%. The contents of the tubes were left standing for possible dissolution of the polymeric materials.
2.3 Preparation of films/membranes doped with oxygen-sensing particles
The oximetry particle-loaded membranes were fabricated by solution-casting on precleaned glass slides (flat or concave), followed by evaporation of the solvent for the polymer at room temperature or at 75°C. Prior to casting, the test LiPc particles were dispersed manually as uniformly as possible into polymer solutions. Solvent evaporation was carried out under three environmental conditions: room temperature, fume hood air draft and oven at 75°C. Regardless of solvent evaporation conditions used, all LiPc polymer membranes were kept in the oven overnight to assure complete solvent evaporation.
2.4 EPR measurements
The EPR measurements were carried out using a Bruker X-band (9.8 GHz) spectrometer (Bruker Instruments, Karlshrue, Germany) equipped with a TM110 cavity. Polymer-encapsulated probes were placed in a 4-mm quartz tube, open at both ends, and inserted into the TM110 cavity for spectral acquisition. The LiPc microcrystals were precalibrated for EPR oximetry as reported (Pandian et al. 2003b; 2006b). The peak-to-peak widths of polymer membrane-encapsulated probes relative to un-encapsulated particulate probes under anoxic condition, as well as various pO2, were measured.
2.5 Implantation of polymer-encapsulated spin probes in gastrocnemius muscle of mice
Mice were anesthetized by isoflurane respiration (1.5% isoflurane/air) delivered through a nose cone; 2 × 2 mm films of polymer-encapsulated LiPc cast as described was implanted subcutaneously in the gastrocnemius muscle of normal leg. In vivo EPR measurements of polymer-encapsulated probes in mice were made at least 48 h after the implantation.
2.6 Animal studies
Female C3H mice supplied through the Frederick Cancer Research Center, Animal Production Unit (Frederick, MD, USA) were used in the present work. The animals were received at 6 weeks of age and housed five per cage in climate-controlled rooms and allowed food and acidified water ad libitum. The animals were on average 50-days old at the time of experimentation and weighed 22–28 g. Experiments were conducted according to the principles outlined in the Guide for the Care and Use of Laboratory Animals prepared by the Institute of Laboratory Animal Resources, National Research Council.
2.7 In vivo EPR measurements in mice
The EPR measurements were carried out on anesthetized mice using an L-band (1.32 GHz) spectrometer (Magnettech, Berlin, Germany) and a topical (surface loop) resonator (Ilangovan et al. 2004a, b). Anesthesia was maintained during the measurements with continuous delivery of 1.5% isoflurane/air mixture using a veterinary anesthesia system (Vasco Anesthesia, Pro Tech Medical Inc., Hazel Crest, IL, USA). The flow rate of the breathing gas mixture was maintained at 2.0 L/min. A thermistor rectal probe was used to monitor body temperature. The body temperature was maintained at 37±1°C using an infrared lamp.
3 Results
3.1 Solvents and polymers
Most of the solvents tested are widely used in the pharmaceutical industry in drug formulation (NMP, THFA, EGDE, EtL, DMSO, and GF) and are therefore widely regarded as biocompatible (Mottu et al. 2000; Pole 2008). Unfortunately, TAF is insoluble in all of them, so we used the solvents FC-40, FC-77 and HFB, all less widely used in biomedical applications, but all known to dissolve TAF.
Polymeric encapsulation can enhance the in vivo stability of oxygen sensing particulates as has been demonstrated by polymer encapsulation of unstable paramagnetic carbon based oximetry materials (He et al. 2001). CA, PVAc, and TAF all have long histories of biomedical use, and high oxygen-permeability coefficients (Dinguizli et al. 2006; Liang et al. 1998; Novoa et al. 2005). Structures of these polymers are shown in Fig. 1.
TAF is a random copolymer of tetrafluoroethylene and 2,2-bis(trifluoromethyl)-4,5-difluoro-l,3-dioxole (Zhao et al. 2005), and exhibits superior chemical stability associated with fluoropolymers (such as PTFE) but with much higher oxygen permeability (exhibiting amongst the highest permeability of any polymer to the “permanent” gases hydrogen, oxygen, nitrogen and carbon dioxide (Merkel et al. 1999). Accordingly, TAF is widely used in gas sensing and filtration systems, and is biocompatible (used in contact lens, Werner et al. 1999). Cellulose is the most abundant naturally occurring polysaccharide, formed out of glucose-based repeat units, connected by 1,4-beta-glucosidic linkages. Biomaterials based on cellulose and cellulose acetate are used in semipermeable membrane devices in hemofiltration and hemodialysis membranes (for renal dialysis), in diffusion-controlling or bioseparation membranes, in membranes for protein immobilization in biosensors, in coating materials for drugs and drug-releasing scaffolds, in in vitro hollow fiber perfusion systems, in cell-culturing and tissue-engineering scaffolds and in contact lens among other biomedical applications (Entcheva et al. 2004; Ke et al. 2006; Kung and Yang 2006). PVAc is used as a coating for drugs and drug-releasing coatings for implants, as in controlled drug release as from drug-eluting vascular stents (Strübing et al. 2007).
Table 1 and Table 2 summarize the solubility of LiPc and our selected biomedical polymers in various solvents. With the exception of TAF-specific solvents, all the solvents listed are widely used in biomedical settings. We identified multiple, water-miscible solvents that do not dissolve LiPc, but do dissolve biomedical polymeric materials. Cellulose acetate (CA) and polyvinyl acetate (PVAc), are more commonly used in biomedical applications either polyvinyl formyl (PVF) or cellulose acetate butyrate (CAB). Therefore, we pursued CA and PVAc as LiPc encapsulation matricies. Teflon AF 2400 (TAF) has been previously reported as an encapsulating matrix for LiPc (Dinguizli et al 2006), so we used TAF-encapsulated LiPc as a comparator to CA and PVAc encapsulated LiPc.
Table 1.
Solubility of LiPc crystals selected organic solvents
| Solvent systems in which LiPc was insoluble | Solvent systems in which LiPc was soluble |
|---|---|
| 90% Tetrahydrofurfuryl alcohol (THFA):10% H2O, v/v | N-methyl-2-pyrrohdone (NMP) |
| Ethylene glycol dimethyl ether (EGDE) | Dimethyl sulfoxide (DMSO) |
| Ethyl lactate (EtL); 90% Dimethylsulfoxide (DMSO):10% H2O | Tetrahydrofurfuryl alcohol (THFA) |
| Glycerol formal (GF) | 90% N-methyl-2-pyrrolidone (NMP):H2O, v/v |
| 90% Glycerol formal (GF):10% H2O, v/v | – |
Table 2.
Solubility of selected biomedical, polymers in solvents of Table 1
| Celllulose acetate (CA) | Polyvinyl acetate (PVAc) | Teflon AF 2400 (TAF) |
|---|---|---|
| 90% N-methyl-2-pyrrolidone (NMP):H2O, v/v | 90% N-methyl-2-pyrrolidone (NMP):H2O, v/v | Flurinert FC-77 |
| Glycerol formal | Glycerol formal | Flurinert FC-40 |
| 90% glycerol formal: 10% H2O, v/v | 90% glycerol formal:H2O, v/v | Hexa-fluro benzene |
| 90% Dimethyl sulfoxide (DMSO):10% H2O, v/v | 90% Dimethyl sulfoxide DMSO):10% H2O, v/v | – |
| Tetrahydrofurfuryl alcohol (THFA) | Tetrahydrofurfuryl alcohol (THFA) | – |
| Ethylene glycol dimethyl ether (EGDE) | 90%Tetrahydrofurfuryl alcohol (THFA): 10% H2O, v/v | – |
| Ethyl lactate (EtL) | Ethylene glycol dimethyl ether (EGDE) | – |
| – | Ethyl lactate (EtL) | – |
LiPc is not detectably soluble in these solvents
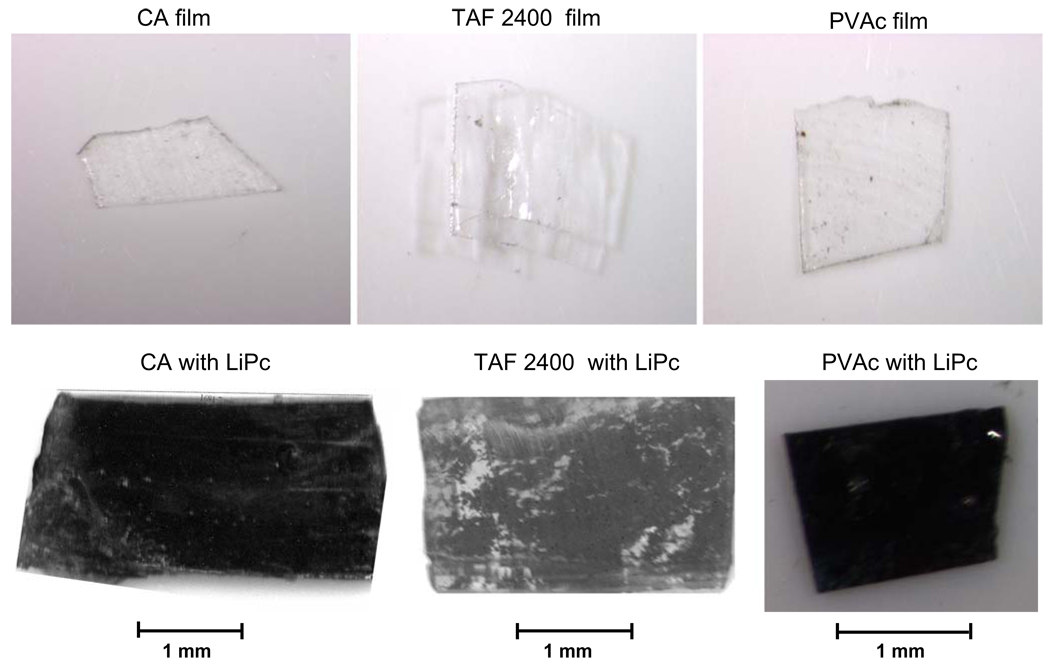
Native TAF, CA, and PVAc films are all colorless and optically transparent (Fig. 2). Embedding LiPc in polymers produced dark purple polymeric films (Fig. 2). To assure complete coverage of the encapsulated LiPc probes within the polymeric matrix, multiple layers (2–3) of polymer were applied.
Fig. 2.
Microscope image of polymer matricies TAF 2400 (TAF), PVAc and CA with and without LiPc spin probes. The LiPc particulates were dispersed uniformly into the polymer solution, followed by evaporation of the polymer solvent to obtain LiPc probe-encapsulated membranes. Uniform dark color of LiPc-containing films reflects uniformly distribution of LiPc in TAF or CA or PVAc
3.2 In vitro EPR characterization
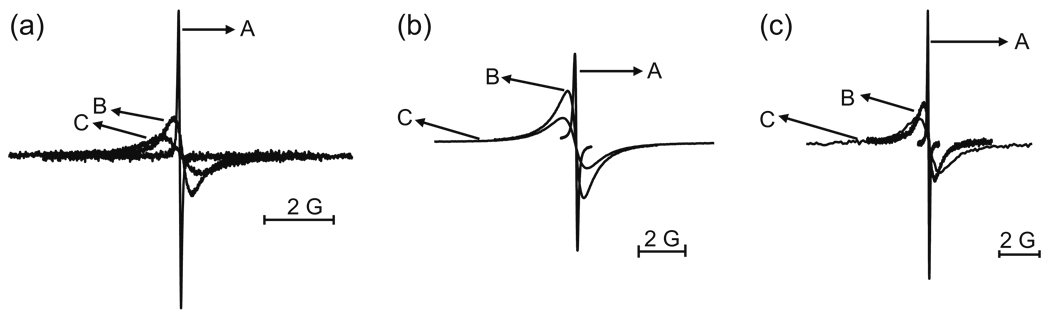
EPR spectra were determined at room temperature, and each encapsulated LiPc formulation exhibited a single-line EPR spectrum similar to that of uncoated LiPc microcrystals (Fig. 3). Under anoxic (0 mmHg of oxygen) conditions, peak-to-peak widths were virtually identical for all encapsulated LiPc (Table 3). Moreover, oxygen sensitivity of uncoated LiPc polymer and polymer embedded LiPc preparations were not significantly different (Table 3).
Fig. 3.
EPR spectra of LiPc particulates encapsulated in (a) TAF 2400, (b) PVAc and (c) CA films. The spectra obtained under 100% N2 (A, anoxic conditions), in the presence of 10% O2/90% N2 (B), and 20.9% O2/79.1% N2 (C) are shown
Table 3.
EPR and Oxygen sensing properties of polymer membrane-coated lithium phthalocyanine (LiPc)
| Polymer | Solvent | Anoxic (0 mmHg of oxygen) (G) | Oxygen sensitivity (mG/mmHg) |
|---|---|---|---|
| TAF | Hexaflurobenzene | 0.07±0.015 | 6.17±0.33 |
| CA | Tetrahydrofurfuryl alcohol (THFA) | 0.07±0.01 | 6.48±0.37 |
| CA | 90% glycerol formal (GF):H2O, v/v | 0.07±0.01 | 6.48±0.28 |
| PVAc | 90% THFA: 10% H2O, v/v | 0.07±0.01 | 6.55±0.23 |
| N/A (uncoated LiPc) | N/A | 0.07±0.01 | 6.62±0.3 |
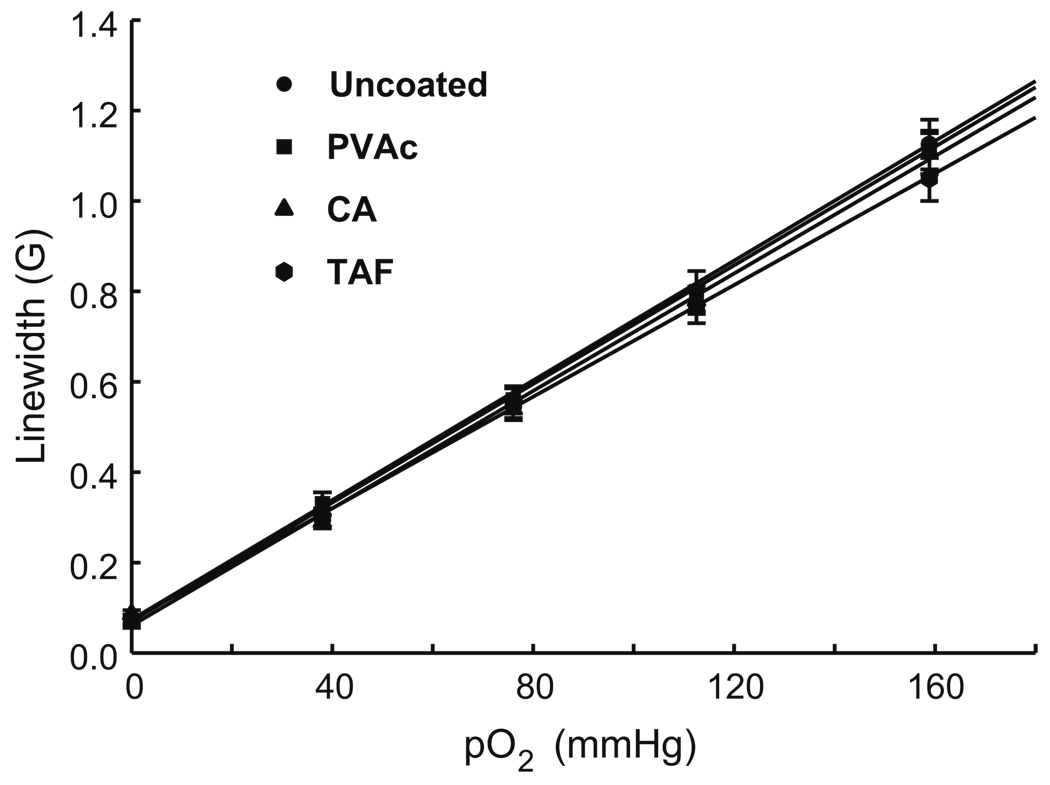
LiPc was encapsulated in one polymer (CA) using two different solvents, though the oximetry properties of the CA films were identical regardless of the difference in their synthesis (Table 3). For uncoated LiPc and for all polymer-encapsulated LiPc, EPR linewidth increased linearly with pO2 (Fig. 4). The relationship between pO2 and linewidth was essentially identical in all cases. Thus, the in vitro oximetry properties of LiPc were unchanged by exposure to any solvent or polymer embedding conditions tested.
Fig. 4.
Effect of oxygen concentration (pO2) on the peak-to-peak EPR linewidth of LiPc particulates encapsulated in PVAc, CA and TAF 2400 (TAF) films. The linewidth increases linearly with pO2 in the range 0 to 160 mmHg (corresponding to 0–20.9% oxygen at 1 atmospheric pressure) with an anoxic linewidth of 70 mG and slope (oxygen sensitivity) of 6.42±0.3 mG/mmHg. There was no significant difference in the oxygen sensitivities of the preparations. Oxygen sensitivities of polymer-encapsulated LiPc are in Table 3
We were concerned that air bubbles in oximetry films might interfere with accurate oxygen measurements and found that solvent evaporation at higher temperature (at 75°C) was more likely to produce films containing air bubbles. Therefore, solvent evaporation was routinely performed at lower (ambient) temperature. The slower evaporation rate at room temperature also allowed us to remove any visible bubbles with a needle before the solvent evaporation was complete.
3.3 In vivo oximetry
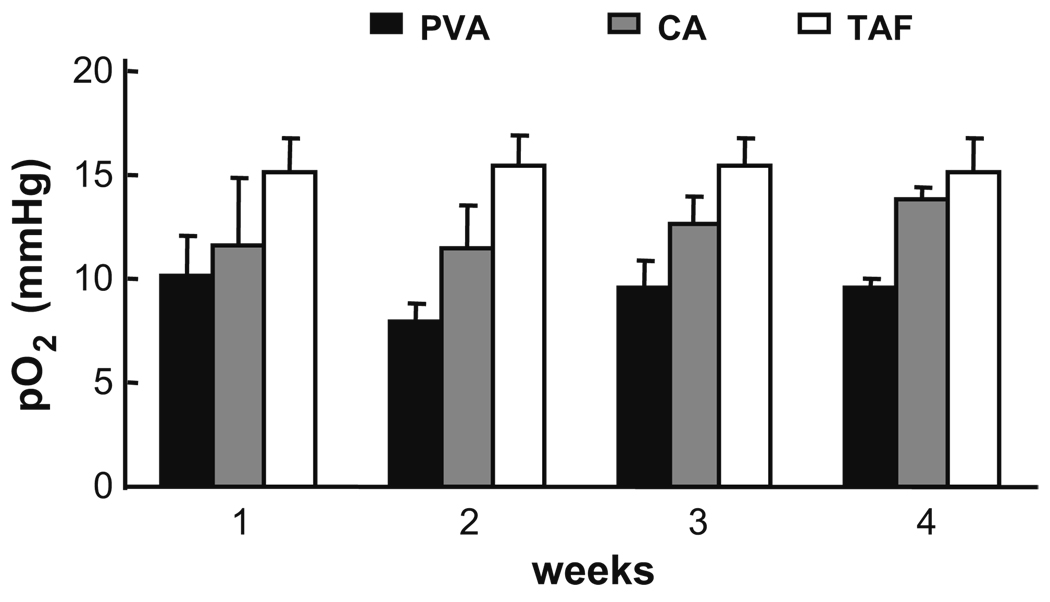
Oxygen sensitivity of uncoated LiPc particles has limited stability in vivo (Liu et al. 1993). To evaluate long term in vivo stability of polymer-encapsulated LiPc, we implanted encapsulated probes in the gastrocnemius muscle of mice and measured pO2 in the same animals for a month (Fig. 5). pO2 under normal blood flow conditions for TAF, CA and PVAc were 15.5±1.5, 12. 2±1.1, 9.8±0.8 mmHg, respectively. These values are within the range of previously reported, EPR-determined normoxic pO2 values in gastrocnemius muscle (normoxia at about 10–25 mmHg, Ilangovan et al. 2004a, b, 2002a, b, 2001). As previously described with LiPc crystals implanted in murine gastrocnemius muscle (Ilangovan et al. 2001), constriction of blood flow to the leg by tying down the limb for 5 min with an elastic band resulted in rapid decrease in measured pO2 for all three films (data not shown). Furthermore, surgically retrieved LiPc-containing polymer films exhibited identical in vitro oximetry properties to those they exhibited prior to implantation (data not shown).
Fig. 5.
Long-term stability of oximetry by polymer-encapsulated LiPc, in vivo. The implanted Polymer films encapsulating LiPc particles were surgically implanted in the gastrocnemius muscle (upper hind leg) of C3H mice (one mouse/film). Oximetry was performed weekly for 4 weeks. All encapsulated particulates remain are oxygen responsive in vivo tissues for 4 weeks
4 Discussion
The potential utility of in vivo oximetry in various human disease states is large, but also largely unsatisfied by current technology. To the end of translating EPR oximetry to the clinic, we demonstrate the feasibility of encapsulating LiPc oximetry crystals in multiple matrices using multiple polymer–solvent pairs. The polymers and solvents used did not significantly alter LiPc oximetry properties. EPR linewidth of encapsulated crystals remained linear with pO2, with slopes similar to that of unencapsulated LiPc. While in vitro oximetry properties were not significantly altered by encapsulation, it stabilized the crystals in vivo. LiPc crystals in TAF, CA and PVAc films were resistant to a panel of common biologic oxidoreductants, and, unlike unencapsulated LiPc, retained their oximetry properties during multi-week in vivo implantation experiments (Liu et al. 1993, Jiang et al. 2001, Gallez et al. 1999; He et al. 2001). As we discuss below, the new polymer formulations offer advantages over earlier TAF oximetry films.
Beyond enhancing in vivo stability, polymer encapsulation also renders other potentially advantageous properties to LiPc crystals, especially in light of the fact that toxicology, inflammatory and immunogenicity properties of LiPc have not been fully elucidated. Encapsulation in biomedical polymers sequesters the oximetry compound from tissue, thereby minimizing the potential for adverse toxicological events in patients. The effectiveness of partition between encapsulated crystals and the biologic system provided by the polymer depends on the polymer not breaking or eroding in vivo, so as to expose LiPc crystals. Barrier function of the polymers thus depends on mechanical properties of the films, which, differ between different polymers (see below).
The barrier provided by polymeric films mitigates potential toxicity, but as non-self materials, oximetry films are expected to induce foreign body responses (inflammatory cell infiltrates, fibrous capsule formation). Foreign body responses to implants are largely unavoidable with current technology, and in fact, do occur with oximetry films. Over a month of film intramuscular implantation, a mild foreign body response occurs, with thin fibrous capsule formation and a limited cellular infiltrate (Meenakshisundaram et al., manuscript in preparation). Despite this, all of the films tested here retained consistent oxygen and induced hypoxia responses in vivo over time.
As a practical matter, unencapsulated micro/nanoscale LiPc crystals cannot be conveniently removed from tissue after implantation. Polymer encapsulation makes it possible to surgically implant and retrieve oximetry films, again, minimizing prolonged systemic exposure to LiPc itself, and therefore minimizing toxicological risks. Perhaps more importantly for evaluation of the impact of encapsulation on LiPc oximetry in vivo, encapsulation allows oximetry films to be characterized before implantation, implanted, then removed from tissue for re-characterization.
The oximetry properties of films after retrieval from tissue were identical to their properties pre-implantation, indicating that intermediate length exposure to the in vivo environment does not detectably degrade their properties. That said, we do not know how long continuous oximetry could be performed from a single LiPc oximetry film. Implant biodegradation does not seem to be a major issue, but perhaps under some conditions, a fibrous capsule could be produced that would provide a significant diffusional barrier to oxygen, and therefore impair oxygen sensing. Still, failure to detect change in oxygen sensitivity/responsiveness over a month in vivo suggests that very long-term oximetry may be possible with the films described here.
Oximetry readings from TAF, CA, and PVAc films remained in normoxic ranges for the duration of the in vivo experiment, except during limb-ligation induced, transient hypoxia challenges. For each film, measured oxygen levels were consistent, but not identical between films. The rank order of sensed oxygen levels was highest with TAF film, followed by CA film, and lowest with PVAc film. Oximetry differences between films might reflect differential properties of each polymer, or might be due to variances in oxygenation in individual tissue sites. The ability to remove the films and recharacterize them after a month in vivo allows us to discriminate between these possibilities. Three observations argue that differences in measured oxygen reflect oxygenation in the individual animals with film implants.
First, the in vitro oximetry properties of the three films are identical prior to implantation, with less than 5% difference in their oxygen sensitivities. Second, all of the polymer oximetry films, when retrieved and retested ex vivo, had the same oximetry properties they had prior to implantation. Third, we have demonstrated comparable variability in normal blood flow conditions (also measured with LiPc crystals) in murine gastrocnemius muscle as observed here (Ilangovan et al. 2001, 2004a, b, 2002a, b). Similar variability in muscle normoxic pO2 has been reported with animal activity, between individual animals (Masumoto et al. 2005), with specific anesthesia regimens (Baudelet and Gallez 2004) and, in a rabbit model, between contralateral sites of single animals (Grinberg et al. 2004). Since results for TAF, CA, PVAc encapsulated LiPc crystals fall within previously measured normal pO2 ranges, and the in vitro oximetry properties of all three films are so similar, the explanation for the rank order of pO2 measured by the three polymer encapsulated LiPc microcrystals in Fig. 5 is likely the result of animal to animal or implant site to implant site variation.
From the standpoint of oximetry properties per se, TAF, CA and PVAc encapsulated LiPc are equivalent. We suspect that many other oxygen permeable polymers could be used to produce functional oximetry films, providing the polymers are oxygen permeable and are soluble in solvents that will not dissolve LiPc crystals, eliminating the oxygen sensitivity of the compound. Table 1 and Table 2 identify multiple specific polymer/solvent systems that could be used for LiPc oximetry films, and Fig. 3–Fig. 5 and Table 3 document the oximetric equivalence of several of the resultant films. Additionally, though we did not test the oximetry properties of films made using them, both polyvinyl formal and cellulose acetate butyrate polymers are oxygen permeable, soluble in multiple of the solvents we identified that do not dissolve LiPc crystals (data not shown), and so potentially could be used to make oximetry films. It seems likely that from the standpoint of oximetry properties, any solvent that does not dissolve LiPc crystals might be useful for making oximetry films. This suspicion is buttressed by the equivalence of CA LiPc film oximetry properties whether they are made using solvents THFA and GF (Table 3). The CA films are essentially identical in this respect, despite being made with different solvents. Still, this should not suggest that there are no rational reasons to prefer one polymer/solvent system over another.
For instance, both CA and PVAc are much less expensive than TAF. TAF also has significant restrictions on its in vivo use mandated by its manufacturer. Moreover, solvents for TAF (FC-40, FC-77 and HFB) are seldom used in in vivo applications, so the safety of those solvents and films processed using them is less well established than for CA and PVAc films. Aside from safety concerns, the solubility of TAF in those solvents is limited. Low concentrations of polymer in the solvents made producing TAF films by solvent evaporation considerably more tedious than producing CA or PVAc films. TAF films were typically thinner and more brittle than CA or PVAc films, making them hard to handle without breaking them. In our experience, there is a much greater likelihood that TAF films might break on manipulation (implantation or surgical retrieval or other handling) than either CA or PVAc films. TAF films might also break during in vivo use. Breakage could diminish the barrier function of the polymer, potentially exposing LiPC to the tissue environment. Furthermore, the fragility of the TAF films creates uncertainty that the film is intact after implantation, or if the entire film has been retrieved.
In the immediate case, these considerations cause us to prefer both CA or PVAc to TAF films for oximetry in vivo. In a broader sense, they illustrate how designers of oximetry implants can legitimately consider properties of the polymers in their design choices. Having a choice of encapsulating polymers, as we provide here, allows multiple parameters such as cost, chemical surface functionalities, rigidity, manufacturing handling, polymer wear and storage properties, among others, to be considered to optimize oximetry implants for clinical use.
Acknowledgement
The study was supported by NIH grant EB 004031.
Contributor Information
Edward Eteshola, Department of Biomedical Engineering, The Ohio State University, Columbus, OH 43210, USA; Davis Heart & Lung Research Institute, The Ohio State University, 473 West 12th Avenue, Room: 305, Columbus, OH 43210, USA.
Ramasamy P. Pandian, Center for Biomedical EPR Spectroscopy and Imaging, The Ohio State University, Columbus, OH 43210, USA Department of Internal Medicine, The Ohio State University, Columbus, OH 43210, USA; Davis Heart & Lung Research Institute, The Ohio State University, 473 West 12th Avenue, Room: 305, Columbus, OH 43210, USA.
Stephen C. Lee, Davis Heart & Lung Research Institute, The Ohio State University, 473 West 12th Avenue, Room: 305, Columbus, OH 43210, USA, e-mail: lee.1996@osu.edu Department of Biomedical Engineering, The Ohio State University, Columbus, OH 43210, USA.
Periannan Kuppusamy, Center for Biomedical EPR Spectroscopy and Imaging, The Ohio State University, Columbus, OH 43210, USA; Department of Internal Medicine, The Ohio State University, Columbus, OH 43210, USA; Davis Heart & Lung Research Institute, The Ohio State University, 473 West 12th Avenue, Room: 305, Columbus, OH 43210, USA.
References
- Baudelet C, Gallez B. Magn. Reson. Imaging. 2004;22(7):905–912. doi: 10.1016/j.mri.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Bratasz A, Pandian RP, Ilangovan G, Kuppusamy P. Adv. Exp. Med. Biol. 2006;578:375–380. doi: 10.1007/0-387-29540-2_58. [DOI] [PubMed] [Google Scholar]
- Bratasz A, Pandian RP, Deng Y, Petryakov S, Grecula JC, Gupta N, Kuppusamy P. Magn. Reson. Med. 2007;57(5):950–959. doi: 10.1002/mrm.21212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinguizli M, Jeumont S, Beghein N, He J, Walczak T, Lesniewski PN, Hou H, Grinberg OY, Sucheta A, Swartz HM, Gallez B. Biosens. Bioelectron. 2006;21(7):1015–1022. doi: 10.1016/j.bios.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Entcheva E, Bien H, Yin L, Chung CY, Farrell M, Kostov Y. Biomaterials. 2004;25(26):5753–5762. doi: 10.1016/j.biomaterials.2004.01.024. [DOI] [PubMed] [Google Scholar]
- Fujii H, Itoh K, Pandian RP, Sakata M, Kuppusamy P, Hirata H. Magn. Reson. Med. Sci. 2007;6(2):83–89. doi: 10.2463/mrms.6.83. [DOI] [PubMed] [Google Scholar]
- Gallez B, Swartz HM. NMR Biomed. 2004;17(5):223–225. doi: 10.1002/nbm.913. [DOI] [PubMed] [Google Scholar]
- Gallez B, Jordan BF, Baudelet C. Magn. Reson. Med. 1999;42(1):193–196. doi: 10.1002/(sici)1522-2594(199907)42:1<193::aid-mrm25>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- Grinberg OY, Hou H, Grinberg SA, Moodie KL, Demidenko E, Friedman BJ, Post MJ, Swartz HM. Physiol. Meas. 2004;25(3):659–670. doi: 10.1088/0967-3334/25/3/006. [DOI] [PubMed] [Google Scholar]
- He J, Beghein N, Ceroke P, Clarkson RB, Swartz HM, Gallez B. Magn. Reson. Med. 2001;46(3):610–614. doi: 10.1002/mrm.1234. [DOI] [PubMed] [Google Scholar]
- Ilangovan G, Zweier JL, Kuppusamy P. J. Phys. Chem. B. 2000a;104(40):9404–9410. [Google Scholar]
- Ilangovan G, Zweier JL, Kuppusamy P. J. Phys. Chem. B. 2000b;104(17):4047–4059. [Google Scholar]
- Ilangovan G, Li H, Zweier JL, Kuppusamy P. J. Phys. Chem. B. 2001;105(22):5323–5330. [Google Scholar]
- Ilangovan G, Manivannan A, Li H, Yanagi H, Zweier JL, Kuppusamy P. Free Radic. Biol. Med. 2002a;32(2):139–147. doi: 10.1016/s0891-5849(01)00784-5. [DOI] [PubMed] [Google Scholar]
- Ilangovan G, Pal R, Zweier JL, Kuppusamy P. J. Phys. Chem. B. 2002b;106(46):11929–11935. [Google Scholar]
- Ilangovan G, Bratasz A, Li H, Schmalbrock P, Zweier JL, Kuppusamy P. Magn. Reson. Med. 2004a;52(3):650–657. doi: 10.1002/mrm.20188. [DOI] [PubMed] [Google Scholar]
- Ilangovan G, Zweier JL, Kuppusamy P. J. Magn. Reson. 2004b;170(1):42–48. doi: 10.1016/j.jmr.2004.05.018. [DOI] [PubMed] [Google Scholar]
- Jiang H, Beghei N, Clarkson RB, Swartz HM, Gallez B. Phys. Med. Biol. 2001;46(12):33239–33239. doi: 10.1088/0031-9155/46/12/317. [DOI] [PubMed] [Google Scholar]
- Ke R, Xu Y, Wang Z, Khan SU. Environ. Sci. Technol. 2006;40(12):3906–3911. doi: 10.1021/es060493t. [DOI] [PubMed] [Google Scholar]
- Kulkarni AC, Kuppusamy P, Parinandi N. Antioxid. Redox Signal. 2007;9(10):1717–1730. doi: 10.1089/ars.2007.1724. [DOI] [PubMed] [Google Scholar]
- Kung FC, Yang MC. Colloids Surf. B Biointerfaces. 2006;47(1):36–42. doi: 10.1016/j.colsurfb.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Kutala VK, Parinandi NL, Pandian RP, Kuppusamy P. Antioxid. Redox Signal. 2004;6(3):597–603. doi: 10.1089/152308604773934350. [DOI] [PubMed] [Google Scholar]
- Kutala VK, Khan M, Angelos MG, Kuppusamy P. Antioxid. Redox Signal. 2007;9(8):1193–1206. doi: 10.1089/ars.2007.1636. [DOI] [PubMed] [Google Scholar]
- Lan M, Beghein N, Charlier N, Gallez B. Magn. Reson. Med. 2004;51(6):1272–1278. doi: 10.1002/mrm.20077. [DOI] [PubMed] [Google Scholar]
- Liang XZ, Zhang Y, Lunte CE. J. Pharm. Biomed. Anal. 1998;16(7):1143–1152. doi: 10.1016/s0731-7085(97)00204-5. [DOI] [PubMed] [Google Scholar]
- Liu KJ, Gast P, Moussavi M, Norby SW, Vahidi N, Walczak T, Wu M, Swartz HM. Proc. Natl. Acad. Sci. USA. 1993;90(12):5438–5442. doi: 10.1073/pnas.90.12.5438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masumoto K, Takasugi S-i, Hotta N, Fujishima K, Iwamoto Y. Eur. J. Appl. Physiol. 2005;94(1–2):54–61. doi: 10.1007/s00421-004-1288-x. [DOI] [PubMed] [Google Scholar]
- Merkel TC, Bondar V, Nagai K, Freeman BD, Yampolskii YP. Macromol. 1999;32:8427–8440. [Google Scholar]
- Mottu F, Gailloud P, Massuelle D, Rufenacht DA, Doelker E. Biomaterials. 2000;21(8):803–811. doi: 10.1016/s0142-9612(99)00243-4. [DOI] [PubMed] [Google Scholar]
- Novoa GG, Heinämäki J, Sabir M, Osmo A, Antonio IC, Alberto SP, Yliruusi J. Eur. J. Pharm. Biopharm. 2005;59:343–350. doi: 10.1016/j.ejpb.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Pandian RP, Kutala VK, Parinandi NL, Zweier JL, Kuppusamy P. Arch. Biochem. Biophys. 2003a;420(1):169–175. doi: 10.1016/j.abb.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Pandian RP, Parinandi NL, Ilangovan G, Zweier JL, Kuppusamy P. Free Radic. Biol. Med. 2003b;35(9):1138–1148. doi: 10.1016/s0891-5849(03)00496-9. [DOI] [PubMed] [Google Scholar]
- Pandian RP, Kutala VK, Liaugminas A, Parinandi NL, Kuppusamy P. Mol. Cell. Biochem. 2005;278(1–2):119–127. doi: 10.1007/s11010-005-6936-x. [DOI] [PubMed] [Google Scholar]
- Pandian RP, Dang V, Manoharan PT, Zweier JL, Kuppusamy P. J. Magn. Reson. 2006a;181(1):154–161. doi: 10.1016/j.jmr.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Pandian RP, Kim Y, Woodward PM, Zweier JM, Manoharan PT, Kuppusamy P. J. Mater. Chem. 2006b;16(36):3609–3618. [Google Scholar]
- Pandian RP, Dolgos M, Dang V, Sostaric JZ, Woodward PM, Kuppusamy P. Chem. Mater. 2007;19(14):3545–3552. [Google Scholar]
- Pole DL. J. Pharm. Sci. 2008;97(3):1071–1088. doi: 10.1002/jps.21060. [DOI] [PubMed] [Google Scholar]
- Sostaric JZ, Pandian RP, Weavers LK, Kuppusamy P. Chem. Mater. 2006;18(17):4183–4189. [Google Scholar]
- Springett R, Swartz HM. Antioxid. Redox Signal. 2007;9(8):1295–1301. doi: 10.1089/ars.2007.1620. [DOI] [PubMed] [Google Scholar]
- Strübing S, Metz H, Mäder K. Eur. J. Pharm. Biopharm. 2007;66:13–119. doi: 10.1016/j.ejpb.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Sugimoto H, Mori M, Masuda H, Taga T. J. Chem. Soc. Chem. Commun. 1986:962–963. [Google Scholar]
- Swartz HM. Antioxid. Redox Signal. 2004;6(3):677–686. doi: 10.1089/152308604773934440. [DOI] [PubMed] [Google Scholar]
- Vikram DS, Zweier JL, Kuppusamy P. Antioxid. Redox Signal. 2007;9(10):1745–1756. doi: 10.1089/ars.2007.1717. [DOI] [PubMed] [Google Scholar]
- Werner L, Legeais JM, Nagel MD, Renard G. J. Biomed. Mater. Res. 1999;46(3):347–354. doi: 10.1002/(sici)1097-4636(19990905)46:3<347::aid-jbm6>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Wisel S, Chacko SM, Kuppusamy ML, Pandian RP, Khan M, Kutala VK, Burry RW, Sun B, Kwiatkowski P, Kuppusamy P. Am. J. Physiol. 2007;292(3):H1254–H1261. doi: 10.1152/ajpheart.01058.2006. [DOI] [PubMed] [Google Scholar]
- Zhao H, Zhang J, Wu N, Zhang X, Crowley K, Weber AG. J. Am. Chem. Soc. 2005;127:15112–15119. doi: 10.1021/ja052875p. [DOI] [PubMed] [Google Scholar]