How did the register come about?
The Copenhagen School Health Records Register (CSHRR) is a database of health examination information on more than 350 000 schoolchildren who ever attended school in the central municipality of the capital city of Denmark. For longer than 100 years, school-based health care has been provided to children in Copenhagen,1 and from the 1930s, the material was systematically recorded on individual health cards. The CSHRR results from the retrieval and computerization of data from every health card. Information from the register can be used on its own and it can also be linked to a variety of health registers and other cohort studies in Denmark.
In the early 1980s, an effort was made to locate the cards when researchers wanted to examine childhood exposures in a cohort of severely obese Danish draftees.2–5 Locating these records was a large undertaking, as previously the cards had been found only for a small number of subjects.6–8 Retrieving the cards was a challenge because they were stored in boxes under the attic eaves of an old tall school building. The necessary cards were retrieved and computerized for the draftee study, but recognizing their tremendous research potential, efforts were made to ensure they were properly archived. Fortunately, this realization occurred just in time—the cards were slated for destruction. The Cancer Registry, run by the Danish Cancer Society, rescued the records and they are now preserved in the Copenhagen Municipal Archives. In the 25 years following the initial study on the draftees, a systematic computerization of information on schoolchildren in Copenhagen born from 1930 to 1983 was undertaken in phases depending on available resources. The process is ongoing, and records from recent school years are added as they become available.
Who is in the register?
The CSHRR is based on the population of 350 445 children born from 1930 to 1983 who ever attended school in the municipality of Copenhagen. A unique feature of the register is that it contains virtually every school child from this time period from public and private schools. Although children who attended private schools were only included from 1947 and onwards, as <4% of children attended private schools before this time, very few were not seen by the health services.9 It is noteworthy that private schools in Denmark, unlike in many other countries, are substantially funded by the state (up to 85% of costs) and are not necessarily only for children from well-off families.10 Additionally, as non-traditional schooling methods such as home schooling were, and remain, very rare in Denmark, few children were educated outside of the formal school system.9 Therefore, the register can be considered virtually complete with regard to the inclusion of Copenhagen's schoolchildren.
During the large number of school years included in the CSHRR, there were slight variations in the ages at which children entered and exited school. Throughout this time period, children entered school at 5–7 years of age,11 but they left school at different ages because the length of compulsory education changed. From 1814, children had to remain in school until the seventh grade, which corresponds to ∼13–14 years of age. In 1972, a law was passed requiring that children remain in school until the ninth grade, or 15–16 years of age.12 By the time it was officially changed, however, it reflected a trend towards longer educations and did not substantially increase the numbers of students remaining in school until this grade.12 As a result of these legislative changes, children were consistently in school from the ages of 7 to 13 years throughout the majority of the time period covered by the register, and up to the age of 15 years from 1960s onwards.
What time period does the sample cover?
The cohort includes children who were born during a significant portion of the 20th century. The history of Copenhagen during these years can be divided into six phases: 1930–35: the mid-inter-war period; 1935–39: the late inter-war period; 1940–45: the occupation; 1946–52: the reconstruction; 1953–72: the social expansion (when the welfare state was established) and 1973–84: the new departure and crises period (characterized by large political and governmental changes, oil crises and a recession).13,14 The impact of World War II on Denmark during the occupation period bears closer scrutiny.
In contrast with many other European countries, German forces occupied Denmark with a minimum of violence.15,16 In sharp contrast with the well-known Dutch Famine in The Netherlands,17 there was very little loss of life in Denmark and supplies were not blockaded.15,16 Although certain food items, fuel and clothing were rationed, all Danes, regardless of economic circumstances, were able to afford and obtain a full diet.11 In fact, for many, the rationing system meant that they ate a healthier diet than before the war, which is supported by a reduction in the number of dental caries among the population.11 We have also demonstrated that there was a negligible impact on the growth of children attending school during the war years.18 These results contrast with documented deficits in childhood growth in countries that were severely affected by the war including Finland,18 France,19 The Netherlands19 and Norway,20,18 among others.
How were the data collected?
In 1897, a school health system of doctors was introduced in Copenhagen because many children showed signs of poor hygeine.1 The primary task of the school health system was to ensure good sanitary conditions, reduce infectious diseases and improve the general health of the children in the schools. As the years went by, the system expanded and children were given full health examinations on a yearly basis.1,21 Supporting this practice, which already prevailed by the school year of 1936, a law was passed in 1947 requiring every child to be examined by at least once a year by a doctor. The law was revised in 1972, and this resulted in fewer examinations. In 1983, it was changed again, and it stipulated that children only had to be measured at school entry or if they had special health needs. Nevertheless, in Copenhagen the policy was to continue offering an examination at school exit. In 1995, a measurement at school exit was again required. Changes in these laws only affected the number of measurements available per child, and not the number of children in the register.
Parents or guardians accompany the child to the first health examination at school entry. At the examinations, the children are given a full health check and the results are recorded in their health card. The health cards changed during the years included in the CSHRR, but the manner of recording height and weight remained unchanged. Birth weight was recorded for children born after 1936. A parent (typically the mother) reported it at the first school health examination. During much of this period, mothers were instructed to bring cards or health books in which doctors, midwives or public health nurses had recorded birth weight. Nonetheless, the period of recall was short (<8 years) and as other reports show, this method is fairly accurate over much longer periods,22,23 it is fair to assume the values are reasonable.
School physicians and nurses performed the height and weight measurements.1 During the majority of the period covered by the register, children were measured without shoes and either naked or wearing underwear. Only after 1973 was light clothing permitted. The measurements were performed using equipment provided by the school health service. Each school had its own schedule for performing the exams; some opted to measure all children on one day, whereas others had individual examinations. Nonetheless, at all schools, if a child was absent on the day of the exam, he or she was measured at another time.
A key feature of the register is that it contains a personal identification number for the children. From April 1, 1968 onwards, The Danish Central Office of Civil Registration (Det Centrale Personregister) assigned an identification number to every citizen. It is known as the central person registration number (CPR number).24 It consists of 10 digits; the first six indicate the day, month and year of birth and the last digit denotes the sex of the person. Children attending school in 1968 and thereafter had the number recorded on their health card.
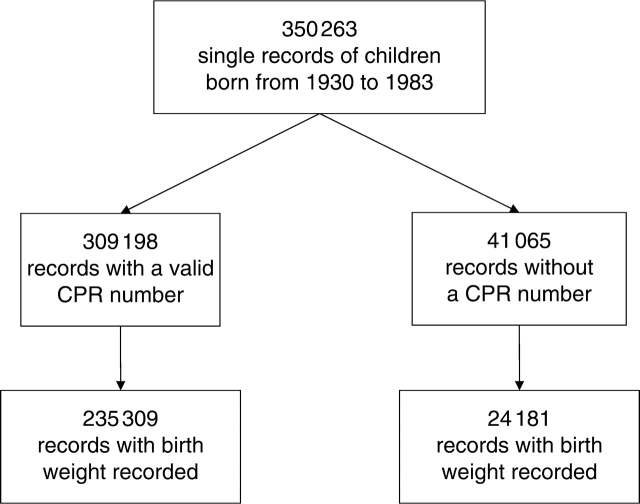
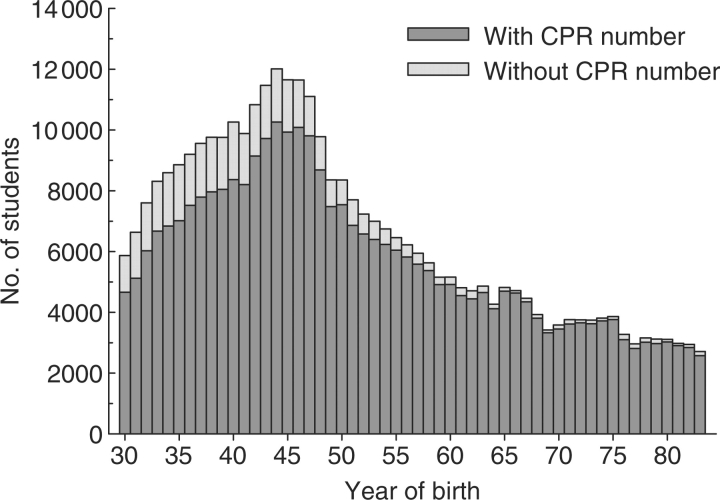
Identification numbers were also obtained for children who did not have them recorded on their health cards. Based on the subjects’ forename(s) and surname, sex and date of birth, matches were obtained with the entire CPR register. A series of algorithms were applied to determine the validity of the matches. A conservative approach was used to ensure that only the valid matches were retained. As a result, identification numbers were identified for 309 198 (88%) of children (Figure 1). CPR numbers were not identified for subjects who died or emigrated before 1968 (thus a number was never issued). Therefore, subjects born in the earliest part of the cohort are more likely to be missing CPR numbers compared with subjects born later (Figure 2). These identification numbers allow for linkages with various other registers and studies in Denmark.
Figure 1.
Description of the CSHRR cohort. Personal identification numbers (CPR numbers) were identified for >88% (n = 309 198) of the sample. Birth weight, due primarily to procedural reasons, was available for a subset of the cohort
Figure 2.
Numbers of children in the CSHRR, with and without personal identification numbers (CPR numbers), by year of birth
What variables are computerized?
The sheer size of the register meant that only the most crucial information was computerized; any added digit would have to be read and typed more than 350 000 times. The building up of the register focused on childhood body size, so even though the cards contain health data, only essential personal information and anthropometric measurements were computerized (Table 1). The register currently contains >2.7 million computerized measurements.
Table 1.
Information available in the Copenhagen School Health Records in versions of the records from the birth years of 1930–83a
| Information recorded in the health records on a nearly continuous basis |
||
|---|---|---|
| Currently computerized | Available | |
| General information | Name | Address |
| Sex | Paternal and/or maternal occupation | |
| Date of birth | School name(s) | |
| Personal identification number (CPR number)b | ||
| Date of the examination (month, year) | ||
| Birth and early infancy | Birth weight (g)c | Birth order |
| Number of siblings | ||
| Anthropometric variables | Weight (kg), Height (cm) | |
| Physical examination | Age at menarche | |
| Hearing | ||
| Vision | ||
| Illnesses/conditions | Colour blindness | |
| Involuntary urination | ||
| Mental condition | ||
| Infectious diseases | Chicken pox | |
| Measles | ||
| Mumps | ||
| Pertussis | ||
| Rubella | ||
| Vaccination status | BCG | |
| Diptheria/tetanus/polio/pertussis | ||
| Smallpoxd | ||
aOther information about the children's health is contained in the records, just not on a continuous basis throughout this time period.
bRecorded on the health card for children attending school in 1968 and onwards, and identified for children in school prior to this time.
cRecorded from the birth year of 1936 and onwards.
dDiscontinued as of April 1, 1977.
Birth weight was computerized, if possible. It was not recorded for children born prior to 1936, and its entry on the cards was phased in from the school year of 1942 so it is not available for children from the earliest part of the cohort. An examination of children with missing birth weight did not reveal an obvious pattern of missing data,25 but it remains a possibility that it is somehow an indicator of a disadvantaged background. Up to 12 measurements of childhood height and weight were entered, with the restriction that measurements needed to be at least 3 months apart. The doctors and nurses recorded the heights and weights with a great attention to detail; heights were recorded to the nearest half-centimetre and weights were recorded to the nearest 100 g.
What other variables are available?
Currently, a case–cohort sampling design has been implemented to obtain further information on the children.5 Even though childhood anthropometry is the focus of the register, the school health examinations covered many aspects of the child health and well being, and this information was recorded on the health cards (Table 1). The case–cohort design optimizes retrieval of this other information for use in studies. In this strategy, a pre-defined, multi-purpose sub-cohort is selected.26 It can be used in multiple studies, which contrasts with the more familiar case–control sampling scheme in which the controls can only be used in one study.26 The case–cohort sampling scheme maximizes statistical power, and the confidence intervals for analyses on rare outcomes are only slightly broader than those from a full-cohort analysis.27,26 For common outcomes, the confidence intervals are similar to those obtained from a full cohort analysis.26,27
The sub-cohort in the CSHRR consists of a 5% sample of each sex by year of birth. All children born on the first of the month are included, and then the sample is enriched up to 5% by a random sample of the remaining children. Children born on the first of the month are included to benefit from future linkage potentials with records from the Copenhagen Municipal Archives. Records are retained there from numerous sources for all citizens born on the first of the month. The case sampling is performed on a project-specific basis.
Information from other computerized sources
The unique personal identification number is the key to linking children in the CSHRR to a large number of national registers on vital statistics, health, economic and social conditions. Thus far, four key national registers have been linked to the cohort. The first national register is the CPR register which contains basic vital statistics.24 The second register is the Hospital Discharge Diagnosis Register (Landspatientregister).28 Established in 1977, it contains information about operations and procedures they received and discharge diagnoses from the visit. From 1995 onwards, outpatient admissions have also been recorded. The third register is the National Cancer Register (Cancerregisteret). Established in 1943, it contains validated information on the type, location and treatment given for cases of cancer.29 Finally, the Cause of Death register (Dødsårsregister) has been linked.30 It contains information about mode of death and up to four diagnoses about the causes of death, which are coded according to International Classification of Disease criteria (version 8 prior to 1994, version 10 thereafter).
The CPR number allows for linkages with numerous other registers in Denmark. These include the Fertility Database,31 the Prescription Medicine Register,32 the Psychiatric Central Register,33 the Twin Register34 and registers from the National Board of Statistics,35 among others. Additionally, because of the CPR number, linkages are also possible with a number of cohort studies that have been conducted throughout Denmark during the last 50 years.
What are the main strengths and weaknesses?
Major strengths of this cohort stem from its extreme size, its population-based nature and the linkage possibilities it offers. The large number of subjects provides great statistical power that allows for investigations of both common and rare outcomes with a high degree of precision. As the cohort is population-based, there is minimal selection bias due to such factors as socioeconomic status. Combined with the complete follow-up obtained on the 88% of the cohort that had a CPR number, analyses on this cohort produce results with a high degree of internal validity. The linkage possibilities to national registers and other studies within Denmark afforded by the identification number make this cohort relevant for numerous types of studies, and especially for those in the area of life-course research.
Other strengths lie in the information contained in the records and in the long time span covered by the cohort. Birth weight was available for the majority of the cohort, and it was reported while the children were young. Doctors and nurses measured the children's body size, and their attention to detail is evident in their careful recordings of it. Since the records still exist, it is always possible to verify an unusual value. The longitudinal nature of the measurements also provided the opportunity for an internal validation by plotting growth curves for the children and examining them for anomalies. Additionally, many of the cohort members have now reached middle age and beyond, so investigations of diseases that only manifest later in life are possible.
As this is an extremely large register-based cohort, a weakness is that little information is available on potentially confounding variables. It was not possible to computerize the entire health card due to time and financial constraints. Nonetheless, as the records are stored in an archive, it is possible to retrieve them and obtain information on a project-specific basis. External validation studies on anthropometric measurements in the CSHRR are not possible because Danish registers on these items simply do not exist for the time period it covers.
In the majority of the cohort, information was not recorded about ethnicity. It can be assumed that nearly all of the subjects in the cohort from the birth years of 1930–83 are of European origin. Immigration from non-Western countries was uncommon prior to the late 1960s, and although it increased after this time, the numbers were very low until 1980s.36 Even in 1980, <3.1% of the overall population in Copenhagen was of non-Western origin.37 Since this time, however, the ethnic composition of schoolchildren in Copenhagen has changed dramatically, and now 24% are of non-European origin.38 Information about ethnicity is noted in records (and is computerized) from the birth year of 1984 onwards. The number of children in the CSHRR has declined since 1940s. In addition to a decreasing birth rate in Denmark, the decline also reflects a movement of many young families to the suburbs outside of the Copenhagen municipality.39 Even with these limitations, which are common to all register-based cohorts, the unique qualities of the CSHRR make it an invaluable resource for research.
What are key findings from this cohort?
Research from this cohort has contributed extensively to the understanding of the early origins of disease. In particular, important contributions have been made in the areas of the development and course of obesity, how the epidemic developed and its long-term health consequences.
An early series of studies used data from the merge between a subset of the CSHRR and a cohort of male Danish draftees to investigate early life risk factors for obesity in young adulthood and its social consequences. Compared with non-obese draftees, the obese men were disadvantaged in terms of intelligence2,3 and eventual attained social class.4 These differences were independent of parental social class, suggesting that some aspect of obesity impaired their abilities. Investigations into the childhood growth of these obese men revealed that, contrary to expectations, most were not obese in childhood, although the risk of becoming an obese young man increased exponentially over the entire range of body mass index (BMI; kg/m2) in childhood.5 Findings from these studies suggested that to really understand the origins of obesity an investigation of the entire cohort of schoolchildren was required.40 Until this became possible, studies investigating causes of obesity were conducted in a population of adoptees who were also in the CSHRR. The strength of the genetic influence on BMI was already fully expressed by 7 years of age.41 These studies suggest that an interplay between genetic and environmental factors leads to obesity in adulthood as well as its social consequences.
Capitalizing on the wide range of years included in this cohort, trend studies have investigated the development of the obesity epidemic among children. Overweight and obesity developed in three phases among Danish school boys42,43 and girls.43 Yet, surprisingly during these years, the birth weight distribution changed very little44,25 and the positive association between birth weight and childhood obesity remained stable.44 A comparison between obesity trends among boys and draftees showed they were similar only when expressed by year of birth (as opposed to calendar year of measurement), suggesting that factors early in life contribute to the later development of obesity.45 Further, by supplementing the register with special data on a subset of Copenhagen schoolchildren in the 2003 school year, it was demonstrated that the prevalence of obesity has continued to rise.46 From these studies, a unique picture of the development of the obesity epidemic has emerged.
Several investigations have examined the long-term health implications of birth weight and body size in childhood. Larger size at birth is associated with breast cancer in women47,48 as well as most other cancers.49 Birth weight is also associated with all-cause mortality, but the association is U-shaped such that both low and high birth weights increase the risk of death.25 When childhood body size was investigated, the study on breast cancer found that women who were tall in childhood or who achieved their peak growth at an early age had a higher risk.48 In an investigation of childhood BMI and adult coronary heart disease, significant linear associations between childhood body size and heart disease were identified. For example, among boys each Z-score increase in BMI at 13 years of age was associated with a 17% greater risk of heart disease in adulthood.50 Taken together, these studies demonstrate that birth weight and body size in childhood have long-lasting effects on disease later in life.
Subsets of the cohort have been used in diverse areas of research investigating other topics such as Hodgkin's disease,6–8 testicular cancer,51 multiple sclerosis,52 childhood growth during World War II,18 blood pressure,53,54 lung function in adulthood55 and statistical methodologies to describe growth.56
How do I find out more about the cohort?
The contact person is T.I.A.S., E-mail: tias@ipm.regionh.dk.
Funding
J.L.B. is supported by a National Institutes of Health Ruth L. Kirschstein National Research Service Award F32DK070491 from the National Institutes of Diabetes and Digestive and Kidney Diseases.
Acknowledgements
Anna-Lise Petersen and Marianne Zimmerman have contributed greatly to the data entry, and Claus Holst contributed to the logistics of building up the computerized database; we are appreciative of their tireless efforts. And finally, we are grateful for the hard work and dedication of the doctors and nurses from the Copenhagen Community Health Services. The computerization of information in the CSHRR has been supported by the Danish Medical Research Council, the Danish National Research Foundation, the Danish Heart Association and the Lundbeck Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Conflict of interest: None declared.
References
- 1.Koch J. Skolelægens arbejde i København gennem 75 år [The work of school doctors in Copenhagen during 75 years] Københavns Kommuneskole. 1972;65:765–67. [Google Scholar]
- 2.Sørensen TIA, Sonne-Holm S, Christensen U. Cognitive deficiency in obesity independent of social origin. Lancet. 1983;1:1105–6. doi: 10.1016/s0140-6736(83)91940-2. [DOI] [PubMed] [Google Scholar]
- 3.Sørensen TIA, Sonne-Holm S. Intelligence test performance in obesity in relation to educational attainment and parental social class. J Biosoc Sci. 1985;17:379–87. doi: 10.1017/s002193200001590x. [DOI] [PubMed] [Google Scholar]
- 4.Sonne-Holm S, Sørensen TIA. Prospective study of attainment of social class of severely obese subjects in relation to parental social class, intelligence, and education. Br Med J (Clin Res Ed) 1986;292:586–89. doi: 10.1136/bmj.292.6520.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sørensen TIA, Sonne-Holm S. Risk in childhood of development of severe adult obesity: retrospective, population-based case-cohort study. Am J Epidemiol. 1988;127:104–13. doi: 10.1093/oxfordjournals.aje.a114770. [DOI] [PubMed] [Google Scholar]
- 6.Andersen E, Isager H. Pre-morbid factors in Hodgkin's disease. II. BCG-vaccination status, tuberculosis, infectious diseases, tonsillectomy, and appendectomy. Scand J Haematol. 1978;21:273–77. [PubMed] [Google Scholar]
- 7.Isager H, Andersen E. Pre-morbid factors in Hodgkin's disease. I. Birth weight and growth pattern from 8 to 14 years of age. Scand J Haematol. 1978;21:250–5. doi: 10.1111/j.1600-0609.1978.tb00360.x. [DOI] [PubMed] [Google Scholar]
- 8.Isager H, Larsen S. Pre-morbid factors in Hodgkin's disease III. School contact between patients. Scand J Haematol. 1980;25:158–64. doi: 10.1111/j.1600-0609.1981.tb01381.x. [DOI] [PubMed] [Google Scholar]
- 9.Københavns Statistiske Kontor. Statistik Årbog [Statistical Yearbook]. Copenhagen: Copenhagen Statistical Office; 1930–1991. [Google Scholar]
- 10.Danish Centre for International Cooperation and Mobility in Education and Training. The Danish Education System. 2nd edn. Copenhagen: CIRIUS; 2006. p. 11. [Google Scholar]
- 11.Københavns Kommunalbestyrelse. Københavns Kommune 1940–1955 [The Municipality of Copenhagen 1940-1945]. Copenhagen: S.L. Møllers; 1957. [Google Scholar]
- 12.Nissen HS. Landet Blev by [Urbanisation of the countryside]. Copenhagen: Glydendals, Politiken; 1991. [Google Scholar]
- 13.Hansen SA, Henriksen I. Sociale Brydninger 1914–39 [Social strife 1914–39]. Copenhagen: Glydenal; 1980. [Google Scholar]
- 14.Hansen SA, Henriksen I. Velfærdsstaten 1940–78 [The welfare state 1940-78]. Copenhagen: Gyldenal; 1980. [Google Scholar]
- 15.Kaarsted T. Krise og Krig 1925–1950 [Crisis and war 1925–1950]. Copenhagen: Gyldendal og Politikens; 1991. [Google Scholar]
- 16.Nielsen N. Verdenshistorie og Danmarkshistorie til 1945. Fra Industrialisering til Verdenskrigene [History of the World and Denmark until 1945. From Industrialization to the World Wars]. Horsens: Åløkke; 1996. [Google Scholar]
- 17.Stein Z. Famine and Human Development: The Dutch Hunger Winter of 1944–1945. New York: Oxford University Press; 1975. [Google Scholar]
- 18.Angell-Andersen E, Tretli S, Bjerknes R, et al. The association between nutritional conditions during World War II and childhood anthropometric variables in the Nordic countries. Ann Hum Biol. 2004;31:342–55. doi: 10.1080/03014460410001685304. [DOI] [PubMed] [Google Scholar]
- 19.Markowitz SD. Retardation in growth of children in Europe and Asia during World War II. Hum Biol. 1955;27:258–73. [PubMed] [Google Scholar]
- 20.Brundtland GH, Liestol K, Walloe L. Height, weight and menarcheal age of Oslo schoolchildren during the last 60 years. Ann Hum Biol. 1980;7:307–22. doi: 10.1080/03014468000004381. [DOI] [PubMed] [Google Scholar]
- 21.Jensen S. Under Fælles Ansvar. Københavns Historie, 1900–45 [Common responsibility: History of Copenhagen, 1900–1945]. Copenhagen: Gyldendal; 1981. [Google Scholar]
- 22.Krebs L, Langhoff-Roos J, Weber T. Breech at term–mode of delivery? A register-based study. Acta Obstet Gynecol Scand. 1995;74:702–6. doi: 10.3109/00016349509021178. [DOI] [PubMed] [Google Scholar]
- 23.Walton KA, Murray LJ, Gallagher AM, Cran GW, Savage MJ, Boreham C. Parental recall of birthweight: a good proxy for recorded birthweight? Eur J Epidemiol. 2000;16:793–96. doi: 10.1023/a:1007625030509. [DOI] [PubMed] [Google Scholar]
- 24.Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull. 2006;53:441–49. [PubMed] [Google Scholar]
- 25.Baker JL, Olsen LW, Sørensen TIA. Weight at birth and all-cause mortality in adulthood. Epidemiology. 2008;19:197–203. doi: 10.1097/EDE.0b013e31816339c6. [DOI] [PubMed] [Google Scholar]
- 26.Prentice RL, Self SG, Mason MW. Design options for sampling within a cohort. In: Moolgavkar SH, Prentice RL, editors. Modern Statistical Methods in Chronic Disease Epidemiology. New York: Wiley-Interscience; 1986. p. 282. [Google Scholar]
- 27.Prentice RL. A case-cohort design for epidemiologic cohort studies and disease prevention trials. Biometrika. 1986;73:1–11. [Google Scholar]
- 28.Andersen TF, Madsen M, Jorgensen J, Mellemkjær L, Olsen JH. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull. 1999;46:263–68. [PubMed] [Google Scholar]
- 29.Storm HH, Michelsen EV, Clemmensen IH, Pihl J. The Danish Cancer Registry–history, content, quality and use. Dan Med Bull. 1997;44:535–39. [PubMed] [Google Scholar]
- 30.Juel K, Helweg-Larsen K. The Danish registers of causes of death. Dan Med Bull. 1999;46:354–57. [PubMed] [Google Scholar]
- 31.Knudsen LB. The Danish fertility database. Dan Med Bull. 1998;45:221–25. [PubMed] [Google Scholar]
- 32.Gaist D, Sorensen HT, Hallas J. The Danish prescription registries. Dan Med Bull. 1997;44:445–48. [PubMed] [Google Scholar]
- 33.Munk-Jorgensen P, Mortensen PB. The Danish psychiatric central register. Dan Med Bull. 1997;44:82–84. [PubMed] [Google Scholar]
- 34.Skytthe A, Kyvik K, Holm NV, Vaupel JW, Christensen K. The Danish twin registry: 127 birth cohorts of twins. Twin Res. 2002;5:352–57. doi: 10.1375/136905202320906084. [DOI] [PubMed] [Google Scholar]
- 35.Statistics Denmark. [(Accessed 27 March, 2008)];Research. 2008 Available at: http://www.dst.dk/HomeUK/ForSale/Research.aspx.
- 36.Nannestad P. Immigration as a challenge to the Danish welfare state. Eur J Polit Econ. 2004;20:755–67. [Google Scholar]
- 37.Statistics Denmark. [(Accessed 27 March, 2008)];Statbank Denmark. 2008 Available at: www.dst.dk.
- 38.Rangvid B. Living and learning separately? Ethnic segregation of school children in Copenhagen. Urb Stud. 2007;44:1329–54. [Google Scholar]
- 39.Illeris S. How did the Population in the Copenhagen Region Change, 1960–2002? Cities in Transition. Ljubljana: Slovenia; 2004. pp. 405–21. [Google Scholar]
- 40.Sørensen TIA. Obesity in the Scandinavian countries: prevalence and developmental trends. Acta Med Scand Suppl. 1988;723:11–16. doi: 10.1111/j.0954-6820.1987.tb05923.x. [DOI] [PubMed] [Google Scholar]
- 41.Sørensen TIA, Holst C, Stunkard AJ. Childhood body mass index–genetic and familial environmental influences assessed in a longitudinal adoption study. Int J Obes Relat Metab Disord. 1992;16:705–14. [PubMed] [Google Scholar]
- 42.Thomsen BL, Ekstrom CT, Sørensen TIA. Development of the obesity epidemic in Denmark: cohort, time and age effects among boys born 1930-1975. Int J Obes Relat Metab Disord. 1999;23:693–701. doi: 10.1038/sj.ijo.0800907. [DOI] [PubMed] [Google Scholar]
- 43.Bua J, Olsen LW, Sørensen TIA. Secular trends in childhood obesity in Denmark during 50 years in relation to economic growth. Obesity. 2007;15:977–85. doi: 10.1038/oby.2007.603. [DOI] [PubMed] [Google Scholar]
- 44.Rugholm S, Baker JL, Olsen LW, Schack-Nielsen L, Bua J, Sørensen TIA. Stability of the association between birth weight and childhood overweight during the development of the obesity epidemic. Obes Res. 2005;13:2187–94. doi: 10.1038/oby.2005.271. [DOI] [PubMed] [Google Scholar]
- 45.Olsen LW, Baker JL, Holst C, Sørensen TIA. Birth cohort effect on the obesity epidemic in Denmark. Epidemiology. 2006;17:292–95. doi: 10.1097/01.ede.0000208349.16893.e0. [DOI] [PubMed] [Google Scholar]
- 46.Pearson S, Olsen LW, Hansen B, Sørensen TIA. Increase in overweight and obesity amongst Copenhagen schoolchildren, 1947–2003. Ugeskr Laeger. 2005;167:158–62. [PubMed] [Google Scholar]
- 47.Ahlgren M, Sørensen TIA, Wohlfahrt J, Haflidadottir A, Holst C, Melbye M. Birth weight and risk of breast cancer in a cohort of 106,504 women. Int J Cancer. 2003;107:997–1000. doi: 10.1002/ijc.11481. [DOI] [PubMed] [Google Scholar]
- 48.Ahlgren M, Melbye M, Wohlfahrt J, Sørensen TIA. Growth patterns and the risk of breast cancer in women. N Engl J Med. 2004;351:1619–26. doi: 10.1056/NEJMoa040576. [DOI] [PubMed] [Google Scholar]
- 49.Ahlgren M, Wohlfahrt J, Olsen LW, Sørensen TIA, Melbye M. Birth weight and risk of cancer. Cancer. 2007;110:412–19. doi: 10.1002/cncr.22773. [DOI] [PubMed] [Google Scholar]
- 50.Baker JL, Olsen LW, Sørensen TIA. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–37. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prener A, Hsieh CC, Engholm G, Trichopoulos D, Jensen OM. Birth order and risk of testicular cancer. Cancer Causes Control. 1992;3:265–72. doi: 10.1007/BF00124260. [DOI] [PubMed] [Google Scholar]
- 52.Bager P, Nielsen NM, Bihrmann K, et al. Childhood infections and risk of multiple sclerosis. Brain. 2004;127(Pt 11):2491–47. doi: 10.1093/brain/awh283. [DOI] [PubMed] [Google Scholar]
- 53.Schack-Nielsen L, Holst C, Sørensen TIA. Blood pressure in relation to relative weight at birth through childhood and youth in obese and non-obese adult men. Int J Obes Relat Metab Disord. 2002;26:1539–46. doi: 10.1038/sj.ijo.0802166. [DOI] [PubMed] [Google Scholar]
- 54.Gamborg M, Byberg L, Rasmussen F, et al. Birth weight and systolic blood pressure in adolescence and adulthood: meta-regression analysis of sex- and age-specific results from 20 Nordic studies. Am J Epidemiol. 2007;166:634–45. doi: 10.1093/aje/kwm042. [DOI] [PubMed] [Google Scholar]
- 55.Bua J, Prescott E, Schack-Nielsen L, et al. Weight history from birth through childhood and youth in relation to adult lung function, in Danish juvenile obese and non-obese men. Int J Obes (Lond) 2005;29:1055–62. doi: 10.1038/sj.ijo.0802998. [DOI] [PubMed] [Google Scholar]
- 56.Petersen JH. A Conditional Bivariate Reference Curve with an Application to Human Growth. Copenhagen: University of Copenhagen; 2005. [Google Scholar]