Abstract
BACKGROUND:
Despite its widespread use, limited data on the validity of the Canadian Cardiovascular Society angina (CCSA) classification relative to other measures of functional status have been reported.
OBJECTIVE:
To assess the validity of the CCSA classification by comparing it with the Duke Activity Status Index (DASI) and evaluate its prognostic significance with respect to long-term mortality.
METHODS:
The study population consisted of 1407 patients who underwent cardiac catheterization between 1992 and 1996. The median follow-up period was 9.7 years (interquartile range 6.1 to 11.1 years) and the mortality status as of December 31, 2004 was available for all patients.
RESULTS:
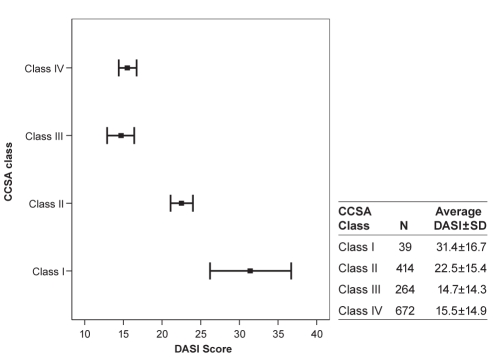
The first three CCSA classes were inversely related to the DASI. The mean (± SD) scores were as follows: class I, 31.4±16.7; class II, 22.5±15.4; class III, 14.7±14.3; and class IV, 15.5±14.9 (P<0.01). Increasing CCSA class was associated with increased long-term mortality, even after adjusting for baseline characteristics. Chest pain course was also an important modulator of mortality among class III and IV patients; one-year mortality rates were 8.1% among unstable patients compared with 4.8% among patients with stable or progressing course.
CONCLUSION:
CCSA classes I to III were inversely related to DASI scores and linearly associated with mortality. The similarity in outcomes among class III and IV patients is probably explained by the confounding effect of the stability of the patients’ symptoms. The higher mortality risk among class III and IV patients with an unstable course provides impetus for a revised CCSA definition incorporating this information.
Keywords: Angina, Functional status, Outcomes
Abstract
HISTORIQUE :
Malgré l’usage généralisé de la classification de l’angine de la Société canadienne de cardiologie (ASCC), on possède peu de données sur sa validité.
OBJECTIF :
Évaluer la validité de la classification de l’ASCC par rapport à l’indice d’état d’activité de Duke (IÉAD) et en évaluer la signification pronostique par rapport à la mortalité à long terme.
MÉTHODOLOGIE :
La population à l’étude se composait de 1 407 patients qui avaient subi un cathétérisme cardiaque entre 1992 et 1996. La période de suivi médiane était de 9,7 ans (plage interquartile de 6,1 à 11,1 ans) et au 31 décembre 2004, on connaissait le statut de mortalité de tous les patients.
RÉSULTATS :
Les trois premières classes d’ASCC étaient inversement proportionnelles à l’IÉAD. Les indices moyens (±ÉT) s’établissaient comme suit : classe I, 31,4±16,7; classe II, 22,5±15,4; classe III, 14,7±14,3 et classe IV 15,5±14,9 (P<0,01). La classe d’ASCC croissante s’associait à une mortalité accrue à long terme, même après rajustement des caractéristiques de départ. L’évolution des douleurs thoraciques était un modulateur important de la mortalité chez les patients de classe III et IV. Les taux de mortalité au bout d’un an étaient de 8,1 % chez les patients instables par rapport 4,8 % chez les patients stables ou à l’évolution progressive.
CONCLUSION :
Les classes I à III d’ASCC étaient inversement proportionnelles aux IÉAD et étaient associées linéairement à la mortalité. La similarité des issues chez les patients de classes III et IV s’explique probablement par l’effet confusionnel de la stabilité des symptômes des patients. Le risque de mortalité plus élevé chez les patients de classes III et IV à l’évolution instable incite à réviser la définition d’ASCC afin de l’y incorporer.
Clinical history is the foundation of the diagnosis and clinical management of coronary artery disease (CAD) (1). In this context, the Canadian Cardiovascular Society angina (CCSA) classification is a time-honoured and useful tool for quantifying physical activity thresholds at which angina occurs (2). Higher CCSA class has also recently been correlated with mortality outcomes, illustrating the enduring value of a classification devised three decades ago (3). While its practicality and ease of use are well known, limited data on the validity of the CCSA classification have been reported (4–8). One form of construct validation would be to correlate the CCSA classification with other methods of quantifying exertional symptoms such as a graded exercise test. However, the results of exercise tests may differ from ordinary activities of daily living in which the patient controls his or her own rate of walking or stair climbing. Correlating the CCSA class with ischemic jeopardy on myocardial scintigraphy or echocardiographic imaging may also not be very useful because ischemic jeopardy and severity of symptoms do not always correlate.
Given these limitations, we assessed the construct validity of the CCSA classification by comparing it with another established validated instrument, the Duke Activity Status Index (DASI). The DASI is a self-administered questionnaire that incorporates four major activity domains: personal care, ambulation, household tasks, and sexual function and recreation (9). The primary objective of the present study was to examine the correlation between CCSA classification and the DASI. The prognostic significance of the CCSA classification was also investigated by examining its association with long-term mortality.
Methods
Patient population
Data collected as part of the Mediators of Social Support (MOSS) study were used to conduct the analysis. The study was described in detail previously (10) and was designed to evaluate the relationship between psychosocial and behavioural factors and outcomes in patients with CAD. Patients with suspected or known CAD referred for a coronary angiographic study at Duke University Medical Center (Durham, North Carolina, USA) between January 1992 and January 1996 were enrolled in the study (n=2885). All MOSS study patients who reported chest pain during the six weeks before cardiac catheterization were included in the study. The presenting chest pain was categorized as typical or atypical angina that was either stable, progressing (defined as a clinically significant increase in the frequency, severity or duration of chest pain) or unstable (defined as severe or prolonged episodes of chest pain at rest, leading to immediate admission to the coronary care unit to rule out a myocardial infarction and for medical management to control symptoms). Patients with congenital heart disease, previous percutaneous coronary interventions (PCIs), repeat coronary angiographic study during the same hospital admission, heart transplant patients and non-English speakers were excluded from the study. Patients were contacted by mail and with a follow-up telephone call at six months, one year and annually every year following catheterization. The identification information (eg, name, social security number) for patients who could not be contacted was submitted annually to the National Death Index (NDI) to assess mortality status. The most current search of the NDI database for the present patient cohort was on December 31, 2004. Therefore, a patient was considered to be alive if they were contacted via mail or telephone, or if no match was found in the 2004 NDI search.
Data
A description of the CCSA classification and the DASI are provided in Tables 1 and 2. The DASI, a patient-reported measure of functional capacity, is a questionnaire-based analogue of the exercise stress test and has been validated against maximal oxygen uptake measured at exercise among patients with CAD. Each unit increase in maximal oxygen uptake is equal to 0.43×DASI+9.6 (9). DASI scores range from 0 to 58, with higher scores reflecting better functional status. Data on CCSA class were recorded by physicians in the catheterization laboratory. The DASI scores were collected independently from the collection of clinical data, including CCSA class. All study data were collected before the angiographic study.
TABLE 1.
Definitions of the Canadian Cardiovascular Society angina (CCSA) classification and the Duke Activity Status Index
| CCSa classification | |
|---|---|
| Class I | Ordinary physical activity does not cause angina, such as walking and climbing stairs. Angina with strenuous or rapid or prolonged exertion at work or recreation |
| Class II | Slight limitation of ordinary activity. Walking or climbing stairs rapidly, walking uphill, walking or stair climbing after meals, or in cold, or in wind, or under emotional stress or only during the few hours after awakening. Walking more than two blocks on level and climbing more than one flight of ordinary stairs at a normal pace and in normal conditions |
| Class III | Marked limitation of ordinary physical activity. Walking one or two blocks on the level and climbing one flight of stairs in normal conditions and at normal pace |
| Class IV | Inability to carry on a physical activity without discomfort – angina syndrome may be present at rest |
Data from reference 2
TABLE 2.
Duke Activity Status Index
| Activity | Weight |
|---|---|
| 1. Could you take care of yourself, that is, eating, dressing, bathing, and using the toilet? | 2.75 |
| 2. Could you walk indoors, such as around your house? | 1.75 |
| 3. Could you walk a block or two on level ground? | 2.75 |
| 4. Could you climb a flight of stairs or walk up a hill? | 5.50 |
| 5. Could you run a short distance? | 8.00 |
| 6. Could you do light work around the house like dusting or washing the dishes? | 2.70 |
| 7. Could you do moderate work around the house like vacuuming, sweeping floors, or carrying in groceries? | 3.50 |
| 8. Could you do heavy work around the house like scrubbing floors or lifting or moving heavy furniture? | 8.00 |
| 9. Could you do yard work like raking leaves, weeding or pushing a power mower? | 4.50 |
| 10. Could you have sexual relations? | 5.25 |
| 11. Could you participate in moderate recreational activities like golf, bowling, dancing, doubles tennis, or throwing a baseball or football? | 6.00 |
| 12. Could you participate in strenuous sports like swimming, singles tennis, football, basketball, or skiing? | 7.50 |
Data from reference 9
Statistical analysis
Means and SDs, as well as medians and interquartile ranges, are presented for continuous variables. Values were compared across CCSA classes using ANOVA and nonparametric Kruskal-Wallis tests, respectively. Categorical variables are presented as percentages, and comparisons were made using χ2 tests. Overall DASI scores and their individual components across CCSA categories were examined. Kaplan-Meier analysis was used to generate one-year, five-year and eight-year survival curves, and log-rank statistics were used to examine whether unadjusted survival differed across the CCSA classes. A backward stepwise Cox proportional hazard model was developed to examine the impact of CCSA on long-term mortality. The following variables were included in the model: demographic variables (age, sex, race and income), clinical history including all comorbidities, number of diseased coronary vessels, left ventricular ejection fraction and chest pain characteristics (course, type and CCSA classification). A modified c index was used to assess the discriminatory power of the model (11).
RESULTS
A total of 2230 patients reported chest pain during the six weeks before the coronary angiographic study. CCSA was not coded for 823 of these patients. Patients with missing CCSA data included those presenting with symptoms unrelated to exertion or with acute coronary syndromes. Characteristics of patients with and without CCSA data are summarized in Table 3.
TABLE 3.
Baseline characteristics among patients with and without Canadian Cardiovascular Society angina (CCSA) class data
| Variable | Patients with CCSA data (n=1407) | Patients without CCSA data (n=823) | P |
|---|---|---|---|
| Baseline demographics | |||
| Age, years, mean ± SD | 62.9±10.8 | 62.8±11.2 | 0.90 |
| Women, % | 29.2 | 39.6 | <0.01 |
| Caucasian, % | 82.2 | 79.0 | 0.07 |
| Poverty*, % | 24.0 | 28.9 | 0.01 |
| Medical history, % | |||
| Hypertension | 59.5 | 63.2 | 0.09 |
| Diabetes | 27.2 | 28.6 | 0.52 |
| Smoking | 67.0 | 68.5 | 0.48 |
| Previous myocardial infarction | 43.9 | 55.7 | <0.01 |
| Peripheral arterial disease | 14.0 | 14.5 | 0.80 |
| Stroke | 12.7 | 12.4 | 0.90 |
| Congestive heart failure | 20.3 | 22.2 | 0.28 |
| Coronary and left ventricular angiographic findings | |||
| Diseased coronary vessels, n | 2.2 | 2.1 | <0.01 |
| Ejection fraction, % | 54.8 | 52.1 | <0.01 |
| Treatment, % | |||
| PTCA within 30 days | 26.8 | 30.1 | 0.10 |
| CABG within 30 days | 36.1 | 28.6 | <0.01 |
Defined as household income ≤$10,000 (1992 to 1996 US$). CABG Coronary artery bypass graft surgery; PTCA Percutaneous transluminal coronary angioplasty
Baseline characteristics overall and by CCSA class are presented in Table 4. The risk profile defined by the presence of risk factors and other vascular diseases increased significantly across the angina classes. In addition, women and patients with lower socioeconomic status reported higher CCSA classes. Patients with higher CCSA classes also had a higher number of episodes per week and their chest pain course was more likely to be worsening or unstable. There were no significant differences in rates of PCI or coronary artery bypass graft surgery (CABG) within 30 days across the CCSA classes.
TABLE 4.
Baseline characteristics by Canadian Cardiovascular Society angina (CCSA) class
| Variable | Overall (n=1407) | Class I (n=39) | Class II (n=424) | Class III (n=265) | Class IV (n=679) | P |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age, years, mean ± SD | 63±11 | 64±10 | 62±11 | 64±10 | 63±11 | 0.14 |
| Women, % | 29.2 | 12.8 | 17.7 | 33.6 | 35.6 | <0.01 |
| Caucasian, % | 82.2 | 87.2 | 83.3 | 86.0 | 79.7 | 0.09 |
| Poverty*, % | 24.0 | 10.5 | 15.1 | 25.3 | 29.7 | <0.01 |
| Medical history, % | ||||||
| Hypertension | 59.5 | 43.6 | 55.0 | 60.8 | 62.7 | 0.01 |
| Diabetes | 27.2 | 7.7 | 24.1 | 26.4 | 30.6 | <0.01 |
| Smoking | 67.0 | 59.0 | 70.3 | 61.5 | 67.6 | <0.01 |
| Previous myocardial infarction | 43.9 | 38.5 | 38.2 | 43.4 | 48.0 | 0.07 |
| Peripheral arterial disease | 14.0 | 5.1 | 9.2 | 15.1 | 17.1 | 0.013 |
| Stroke | 12.7 | 12.8 | 7.1 | 11.7 | 16.5 | <0.01 |
| Congestive heart failure | 20.3 | 12.8 | 12.5 | 26.4 | 23.1 | <0.01 |
| Coronary and left ventricular angiographic findings, mean ± SD | ||||||
| Diseased coronary vessels, n | 2.2±0.9 | 2.0±0.9 | 2.2±0.8 | 2.2±0.9 | 2.2±0.9 | 0.72 |
| Ejection fraction, % | 54.8±15 | 58.2±13 | 56.8±14 | 53.6±16 | 53.9±15.3 | <0.01 |
| Chest pain characteristics | ||||||
| Type, % | 0.08 | |||||
| Typical† | 79.3 | 59.0 | 79.7 | 79.2 | 80.6 | |
| Atypical‡ | 20.5 | 41.0 | 20.3 | 20.8 | 19.4 | |
| Frequency§, mean ± SD | 7.6±10.4 | 2.5±3.0 | 4.7±6.1 | 7.0±6.7 | 9.9±13.1 | <0.01 |
| Course, % | <0.01 | |||||
| Stable | 18.6 | 50.0 | 35.4 | 11.9 | 9.9 | |
| Progressing¶ | 34.3 | 31.6 | 40.3 | 49.0 | 26.3 | |
| Unstable** | 45.3 | 18.4 | 24.3 | 39.1 | 63.9 | |
| Duration of symptoms, months, mean ± SD | 70.9±88.8 | 65.6±90.3 | 65.0±85.6 | 67.9±83.2 | 76.2±92.7 | 0.20 |
| Treatment (30-day), % | ||||||
| Percutaneous transluminal coronary angioplasty | 26.8 | 20.5 | 25.0 | 26.8 | 28.3 | 0.52 |
| Coronary artery bypass graft surgery | 36.1 | 38.5 | 38.2 | 36.6 | 34.5 | 0.63 |
Defined as household income ≤$10,000 (1992 to 1996 US$);
Classical history of angina pectoris with the expected finding of significant atherosclerotic heart disease. In general, it should be reproducibly precipitated by increased cardiac workload (usually exercise), located appropriately (chest or arm), visceral in quality and relieved promptly after removal of the precipitating factors or the use of nitroglycerin;
Symptoms are possibly or probably due to myocardial ischemia, although the symptoms are not consistent with classical angina;
Defined as the number of episodes per week during the six weeks before coronary angiography;
Defined as a clinically significant increase in the frequency, severity or duration of chest pain;
Defined as a very unstable anginal pain pattern, usually with severe or prolonged episodes of chest pain at rest, leading to immediate admission to the coronary care unit to rule out a myocardial infarction and for medical management to control pain
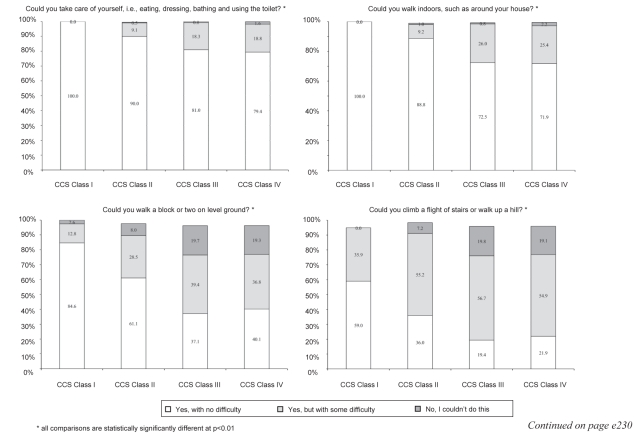
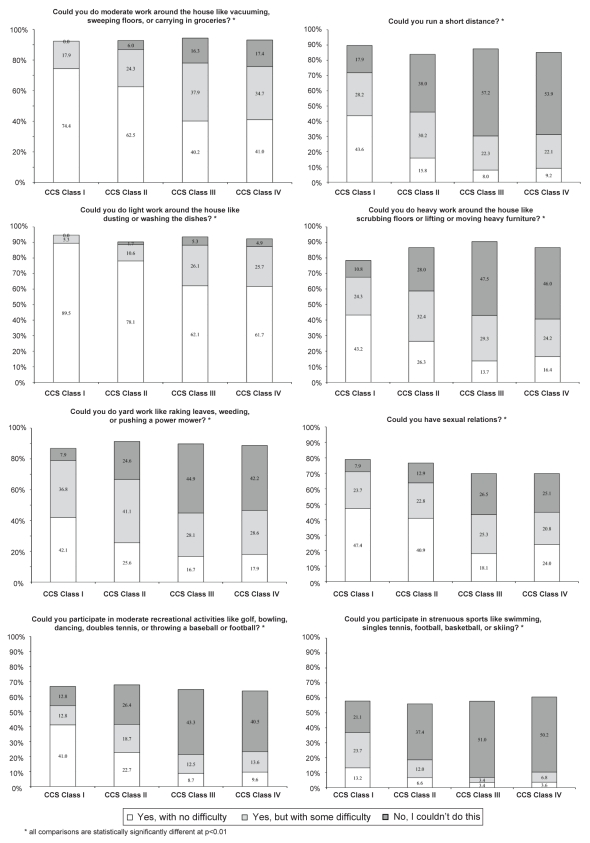
CCSA class and the overall baseline DASI score were negatively correlated; ie, higher angina class patients had lower scores (Pearson correlation of −0.23, P<0.01). The overall DASI score by CCSA class is presented in Figure 1. CCSA class I patients had the highest baseline DASI scores (31.4±16.7) and class III patients had the lowest (14.7±14.3). CCSA class IV patients had similar DASI scores to class III patients (15.5±14.9). The correlation between individual components of the DASI and CCSA class are presented in Appendix 1. Difficulty in performing activities of daily living increased significantly with increasing CCSA class.
Figure 1).
Correlation between Canadian Cardiovascular Society angina (CCSA) class and the Duke Activity Status Index (DASI) at baseline
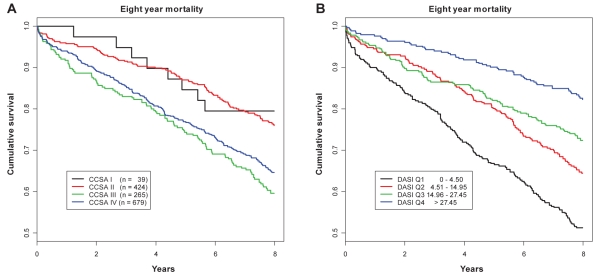
Figure 2 shows Kaplan-Meier long-term (eight-year) survival curves by CCSA class (Figure 2A) and quartiles of DASI (Figure 2B). Eight-year mortality rates were 20.5%, 24.1%, 40.4% and 35.3% (P<0.01) among class I, II, III and IV patients, respectively. There was also a significant inverse relationship between DASI scores and eight-year mortality: 48.7% in quartile 1, 35.5% in quartile 2, 27.6% in quartile 3 and 17.8% in quartile 4 (P<0.01).
Figure 2).
Survival by Canadian Cardiovascular Society angina (CCSA) class (A) and quartiles of the Duke Activity Status Index (DASI) (B)
CCSA class was a significant predictor of long-term mortality, after adjusting for other baseline characteristics (Table 5). Other factors associated with worse long-term prognosis were age, lower socioeconomic status, diabetes, smoking, congestive heart failure, chest pain course, number of diseased vessels and lower ejection fraction. The model performance was good with a c index value of 0.74. The mortality rate among patients who underwent revascularization (PCI or CABG) was significantly lower compared with patients who did not undergo revascularization within 30 days of cardiac catheterization (eight-year mortality rate among revascularized patients was 26.5% compared with 42% among nonrevascularized patients; P<0.01). Inclusion of revascularization status increased the model’s c index value to 0.75. Both PCI (hazard ratio 0.71; 95% CI 0.53 to 0.94) and CABG (hazard ratio 0.77; 95% CI 0.62 to 0.96) were associated with improved survival in this cohort of patients.
TABLE 5.
Baseline predictors of eight-year mortality
| Hazard ratio | Lower 95% CI | Upper 95% CI | P | |
|---|---|---|---|---|
| Age | 1.05 | 1.04 | 1.07 | 0.00 |
| Poverty* | 1.48 | 1.21 | 1.81 | 0.00 |
| Diabetes | 1.44 | 1.18 | 1.76 | 0.00 |
| Smoking | 1.43 | 1.16 | 1.76 | 0.00 |
| Congestive heart failure | 1.60 | 1.30 | 1.98 | 0.00 |
| CCSA class | ||||
| I† | 1.00 | 1.00 | 1.00 | 0.02 |
| II | 1.16 | 0.56 | 2.39 | |
| III | 1.77 | 0.85 | 3.68 | |
| IV | 1.37 | 0.67 | 2.82 | |
| Chest pain course | ||||
| Stable† | 1.00 | 1.00 | 1.00 | 0.04 |
| Progressing | 0.93 | 0.69 | 1.25 | |
| Unstable | 1.22 | 0.92 | 1.62 | |
| Number of diseased vessels | 1.25 | 1.10 | 1.42 | 0.00 |
| Left ventricular ejection fraction | 0.97 | 0.97 | 0.98 | 0.00 |
Defined as household income ≤$10,000 (1992 to 1996 US$);
Comparison group. CCSA Canadian Cardiovascular Society angina
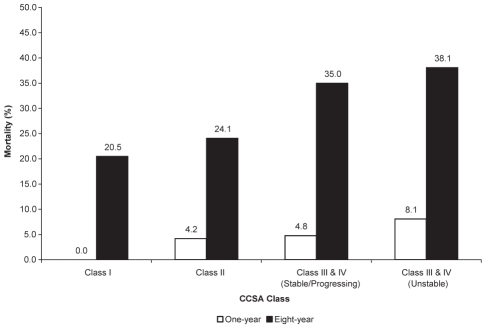
In the present population, 39.1% of class III and 63.9% of class IV patients had an unstable chest pain course. To examine the extent to which the stability of the symptoms modulated the prognostic power of the CCSA class, the class III and class IV patients were regrouped into class III and IV patients with stable or progressing course (n=414) and class III and IV patients with unstable course (n=530). One-year and eight-year mortality rates according to the new classification are presented in Figure 3. One-year mortality rates were 0% among class I, 4.2% among class II, 4.8% among class III and IV patients with stable or progressing symptoms, and 8.1% among class III and IV patients with unstable symptoms (P<0.01). Eight-year mortality rates were 20.5%, 24.1%, 35.0% and 38.1%, respectively, across the four groups.
Figure 3).
Mortality rates across revised Canadian Cardiovascular Society angina (CCSA) class. All rates are significantly different across groups at P<0.01
DISCUSSION
The present study is one of the first to examine the validity of the CCSA classification in a large subset of patients by comparing it with a previously validated patient-reported functional status measure in addition to evaluating its prognostic value. We expected to find a significant inverse relationship between the CCSA classes and DASI scores. We observed this inverse relationship for patients with class I, II and III but not for those with class IV angina. Furthermore, we documented that an increased CCSA class – except for class IV – was associated with an increase in all-cause mortality.
There was, in general, a graded relationship between the CCSA classes from I to IV and the baseline risk factors and other vascular diseases; the only exception was that age was similar across the four groups. The rate of worsening angina significantly increased with increasing CCSA class from I to III. As expected from these observations, the relationship between the CCSA class I to III and the DASI scores was not only significant globally, but was also consistent for each of the 12 questions assessing functional impairment gradation based on either difficulty or total incapacity to accomplish the proposed activities (Appendix 1).
The result that CCSA class IV patients had similar DASI scores to patients assessed as CCSA class III was not unexpected. Although the patients in class IV tended to be at higher risk than those in class III according to baseline characteristics, they had a lower rate of worsening angina but a higher rate of unstable angina and more angina episodes per week. Patients with worsening angina may have remained more incapacitated during symptom assessment because patients with unstable angina would have received more intensive medical management, often as inpatients.
It is well known that survival in persons with or without well-established ischemic heart disease is related to exercise capacity; those achieving a high exercise performance have better survival than those with limited to low exercise capacity (12,13). Hemingway et al (3) reported that among 2849 consecutive angina patients with defined CAD by angiography, higher CCSA classes were linearly associated with all-cause mortality and nonfatal myocardial infarction during a 2.5-year follow-up period. This relationship was confirmed in our study for all-cause mortality during an eight-year follow-up period for class I, II and III patients. Our study also corroborates previous work by Naylor et al (14), suggesting that the stability of symptoms offers important prognostic information in this population. When class III and IV patients were reclassified according to the stability of their symptoms, we found that unstable patients had significantly higher mortality rates (8.1% at one year and 38.1% at eight years compared with stable patients (4.8% at one year and 35.0% at eight years).
Limitations
Our study has some limitations. The patients involved in the present study represent a select population undergoing coronary angiography at a single institution. However, the Duke University Medical Center is a high-volume, high-quality academic centre housing the Duke Database for Cardiovascular Disease (15), which is the largest, oldest and most comprehensive ongoing epidemiological database of patients undergoing cardiac catheterization. A second limitation is the absence of inter-rater and intrarater reliability. Because data on CCSA class were recorded by physicians in the catheterization laboratory, it is feasible that definitions were interpreted differently by different physicians. It is noteworthy, however, that Goldman et al (16) examined the reproducibility of the CCSA classification using the performance of 75 patients during a standard Bruce protocol exercise treadmill test as a reference. They compared the New York Heart Association class with the CCSA class and the specific activity scale, a functional measure based on the metabolic costs of specific activities. The CCSA class had a reproducibility of 73%, similar to the specific activity scale and higher than the 56% reproducibility rate of the New York Heart Association scale. A third limitation is that the small number of CCSA class I patients may increase the variability of the estimates.
CONCLUSION
CCSA classes I to III were inversely related to DASI scores in the present cohort and were significantly associated with long-term mortality. We therefore recommend the continued use of this simple instrument in both clinical practice and trials to risk stratify and manage patients with angina. The similarity in outcomes among class III and IV patients can likely be explained by the confounding effect of the stability of the patients’ symptoms. The higher mortality risk among class III and IV patients with an unstable course provides impetus for a revised CCSA definition incorporating this information.
APPENDIX 1. Relationship between individual Duke Activity Status Index (DASI) questions and Canadian Cardiovascular Society (CCS) angina classes
REFERENCES
- 1.Chun AA, McGee SR. Bedside diagnosis of coronary artery disease: A systematic review. Am J Med. 2004;117:334–43. doi: 10.1016/j.amjmed.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Campeau L. Grading of angina pectoris. Circulation. 1976;54:522–3. [PubMed] [Google Scholar]
- 3.Hemingway H, Fitzpatrick NK, Gnani S, et al. Prospective validity of measuring angina severity with Canadian Cardiovascular Society class: The ACRE study. Can J Cardiol. 2004;20:305–9. [PubMed] [Google Scholar]
- 4.Goldman L, Hashimoto B, Cook EF, Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: Advantages of a new specific activity scale. Circulation. 1981;64:1227–34. doi: 10.1161/01.cir.64.6.1227. [DOI] [PubMed] [Google Scholar]
- 5.Ho Ping Kong W, Llewellyn-Thomas H, Naylor CD. The internal logic of the Canadian Cardiovascular Society scale for grading angina pectoris: A first appraisal. Can J Cardiol. 1992;8:947–53. [PubMed] [Google Scholar]
- 6.Cox JL, Naylor CD, Johnstone DE. Limitations of Canadian Cardiovascular Society classification of angina pectoris. Am J Cardiol. 1994;74:276–7. doi: 10.1016/0002-9149(94)90372-7. [DOI] [PubMed] [Google Scholar]
- 7.Campeau L. The Canadian Cardiovascular Society grading of angina pectoris revisited 30 years later. Can J Cardiol. 2002;18:371–9. [PubMed] [Google Scholar]
- 8.Dagenais GR, Armstrong PW, Theroux P, Naylor CD, CCS Ad Hoc Committee for Revising the CCS Grading of Stable Angina Revising the Canadian Cardiovascular Society grading of stable angina pectoris after a quarter of a century of use. Can J Cardiol. 2002;18:941–4. [PubMed] [Google Scholar]
- 9.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (The Duke Activity Status Index) Am J Cardiol. 1989;64:651–4. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 10.Bosworth HB, Siegler IC, Brummett BH, et al. The association between self-reported health and mortality in a well-characterized sample of coronary artery disease patients. Medical Care. 1999;37:1226–36. doi: 10.1097/00005650-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Harrel FE, Lee KL, Mark DB. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 12.Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- 13.Dagenais GR, Rouleau JR, Christen A, Fabia J. Survival of patients with strongly positive exercise electrocardiogram. Circulation. 1982;65:452–7. doi: 10.1161/01.cir.65.3.452. [DOI] [PubMed] [Google Scholar]
- 14.Naylor CD, Baigrie RS, Goldman BS, et al. Assessment of priority for coronary revascularization procedures. Lancet. 1990;335:1070–4. doi: 10.1016/0140-6736(90)92640-4. [DOI] [PubMed] [Google Scholar]
- 15.Duke Heart Center<http://dukeheartcenter.org> (Version current at May 28, 2009).
- 16.Goldman L, Hashimoto B, Cook EF, Loscalzo A. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: Advantages of a new specific activity scale. Circulation. 1981;64:1227–34. doi: 10.1161/01.cir.64.6.1227. [DOI] [PubMed] [Google Scholar]