Abstract
Objective
The recent obesity epidemic has been accompanied by a parallel growth in chronic sleep deprivation. Physiologic studies suggest sleep deprivation may influence weight through effects on appetite, physical activity, and/or thermoregulation. This work reviews the literature regarding short sleep duration as an independent risk factor for obesity and weight gain.
Methods
A literature search was conducted for all articles published between 1966 and January 2007 using the search “sleep” AND (“duration” OR “hour” OR “hours”) AND (“obesity” OR “weight) in the MEDLINE database. Additional references were identified by reviewing bibliographies and contacting experts in the field. Studies reporting the association between sleep duration and at least one measure of weight were included.
Results
Thirty-six publications (31 cross-sectional, 5 prospective, and 0 experimental) were identified. Findings in both cross-sectional and cohort studies of children suggested short sleep duration is strongly and consistently associated with concurrent and future obesity. Results from adult cross-sectional analyses were more mixed with 17 of 23 studies supporting an independent association between short sleep duration and increased weight. In contrast, all 3 longitudinal studies in adults found a positive association between short sleep duration and future weight. This relationship appeared to wane with age.
Discussion
Short sleep duration appears independently associated with weight gain, particularly in younger age groups. However, major study design limitations preclude definitive conclusions. Further research with objective measures of sleep duration, repeated assessments of both sleep and weight and experimental study designs that manipulate sleep are needed to better define the causal relationship of sleep deprivation on obesity.
Keywords: sleep, sleep duration, sleep deprivation, risk factor, weight
Introduction
Over the past several decades, the prevalence of obesity has grown to epidemic proportions. Concurrent with this rise in weight has been a similar epidemic of chronic sleep deprivation. According to annual surveys done by the National Sleep Foundation, by 1998 only 35% of American adults were obtaining 8 hours of sleep and that number had fallen to 26% by 2005.1
Evidence has grown over the past decade supporting a role for short sleep duration as a novel risk factor for weight gain and obesity. A number of causal pathways linking reduced sleep with obesity have been posited based on experimental studies of sleep deprivation. Chronic partial sleep deprivation causes feelings of fatigue which may lead to reduced physical activity.2, 3 Sleep deprivation may also have neurohormonal effects that increase caloric intake.4 Because of the rapidly accelerating prevalence of sleep deprivation, any causal association between short sleep durations and obesity would have substantial importance from a public health standpoint. We performed a systematic review of the literature to assess the present evidence suggesting sleep deprivation may represent a novel risk factor for weight gain and obesity.
Methods
Relevant original articles were identified by searching the MEDLINE database (National Library of Medicine, Bethesda, MD) of articles published between 1966 and August 2006 examining the relationship between sleep duration and weight gain, obesity or both. The primary search was performed using the keywords “sleep” AND (“duration” OR “hour” OR “hours”) AND (“obesity” OR “weight”). A subsequent search was also performed using medical subheading (MeSH) terms. The searches were repeated in January 2007 to identify any new publications. Bibliographies of retrieved articles were reviewed and experts in the field were contacted to further identify relevant works. Articles were restricted to studies conducted in humans presenting original research. Where data from the same cohort were presented in more than one article, only the report that most directly analyzed the sleep-weight association was included. All abstracts obtained from this search were screened. Relevant articles were obtained and evaluated for presentation of data regarding the association between sleep duration and at least one measure of weight (e.g. BMI, BMI z-score, weight) either cross-sectionally or longitudinally. A meta-analysis was attempted, but the degree of heterogeneity among study designs, particularly with respect to the measure of association and the definition of short sleep duration, was prohibitive, and therefore a more qualitative assessment is presented. Greater weight is given to large studies, prospective cohort studies, and studies which objectively assessed sleep durations. Because of differences in the sleep requirements of children and adults, these groups are considered separately. Where results were presented graphically, authors were contacted to obtain the numeric data.3, 5, 6
Results
The keyword search initially identified a total of 1013 citations. After screening through abstracts for relevance, 36 articles of potential relevance were identified. The MeSH search identified an additional 5 articles. Fifteen articles were excluded because though both sleep duration and weight data were collected, the association between these two factors was not assessed. Another 5 articles were excluded for presentation of data overlapping with another report, leaving 21 articles. Ten investigations were added after the original extraction from review of references and expert contact. The updated search in January 2007 identified 44 additional citations of which 5 were relevant for this synthesis. Thus 36 studies were included in this analysis. Of these, 31 are cross-sectional studies, two are prospective cohort studies, and three report both cross-sectional and prospective findings. No experimental studies with weight as an outcome were identified. There are 13 studies examining the association between sleep duration and weight in pediatric populations and 23 studies of adults.
Cross-sectional studies in children
Eleven studies were identified which assessed the cross-sectional association between sleep duration and weight in children (Table 1). All 11 works reported a positive association between short sleep duration and increased obesity. For the most part, obesity was defined by age-adjusted thresholds of BMI which was directly measured while sleep duration was typically obtained from questionnaires completed by parents. Because sleep requirements change through childhood, definitions of short sleep duration varied greatly based on the age of the cohort being studied.
Table 1.
Cross-sectional studies of sleep duration and weight in children.
| First Author Country Year | Sample Size | Age Range or Mean | Population Source | Weight Measure | Sleep Measure | Potential Confounders Addressed | Pattern of Association |
|---|---|---|---|---|---|---|---|
| Locard10 France 1992 | 1,031 | 5 | 202 schools | Measured BMI | 1 question to parents | Age, ethnicity, SES, TV viewing, breastfeeding, parental obesity, maternal age, single parent | Short SD associated with increased obesity risk. |
| Ben Slama13 Tunisia 2002 | 167 | 6–10 | Primary schools in Ariana district | Measured BMI | 1 question to parents | None | Short SD associated with increased obesity risk. |
| Von Kries9 Germany 2002 | 6,862 | 5–6 | School entry physicals | Measured BMI, body fat mass | Bedtime/wake-time questions to parents | Age, maternal smoking, SES, physical activity, TV viewing, diet, breastfeeding, snacking, birthweight, parental obesity, single parent | Short SD associated with increased obesity risk. |
| Sekine7 Japan 2002 | 8,274 | 6–7 | Birth cohort in Toyama | Measured BMI | 1 question to parents | Age, sex, physical activity, TV viewing, snacking, regular breakfast | Short SD associated with increased obesity risk. |
| Gupta14 USA 2002 | 383 | 11–16 | Heartfelt Study | Measured BMI, percent body fat | 24 hr actigraphy | Age, sex, ethnicity, Tanner stage | Short SD associated with increased obesity risk. |
| Benefice15 Senegal 2004 | 40 | 13–14 | Niakhar district | Measured BMI, triceps skinfold | 72–96 hr accelerometry | Age, sex, ethnicity, physical activity, height, season | Inverse association between SD and BMI. |
| Giugliano12 Brazil 2004 | 165 | 6–10 | Private school | Measured BMI, percent body fat | 1 question to parents | None | Inverse association between SD and percent body fat. |
| Knutson16 USA 2005 | 4,486 | 17 | NLSAH | Measured BMI | 1 question to child | Age, sex, ethnicity, SES, physical activity | Short SD associated with increased overweight risk in boys but not girls. |
| Padez8 Portugal 2005 | 4,511 | 7–9 | Primary schools | Measured BMI | Weekday/weekend questions to parents | Age, sex | Short SD associated with increased obesity risk. |
| Chaput11 Canada 2006 | 422 | 5–10 | 14 schools | Measured BMI | 1 question to parents | Age, sex, SES, physical activity, TV viewing, breastfeeding, regular breakfast, parental obesity, single parent | Short SD associated with increased overweight risk. |
| Chen17 Taiwan 2006 | 656 | 13–18 | 7 schools | Measured BMI | 1 question to child (frequency of adequate sleep - SD at least 6–8 hours on weekdays) | Age, sex | Low frequency of adequate sleep associated with increased obesity risk. |
Estimates provided with 95% confidence intervals in parentheses. BMI: body mass index; SD: sleep duration; OR: odds ratio; NLSAH: National Longitudinal Study of Adolescent Health; SES: socioeconomic status; TV: television.
The largest pediatric cohort to date is a Japanese birth cohort of 8,274 children assessed between the ages of 6 and 7.7 Compared to children with a sleep duration of 10 hours or more, the odds ratios (ORs) for obesity were 1.49, 1.89, and 2.89 for sleep durations of 9–10, 8–9, or fewer than 8 hours respectively. A study of 4,511 Portuguese schoolchildren aged 7–9 reported similar findings.8 Compared to a sleep duration of11 hours or more, the ORs for obesity were 2.27 and 2.56 for sleep durations of 9–10 hours and 8 hours respectively.
Two studies have analyzed data from children undergoing health screens at school enrollment. A study of 6,645 German children aged 5–6 years found the ORs for obesity were 1.18 and 2.22 for sleep durations of 10.5–11.0 hours and less than 10.5 hours respectively compared to 11.5 hours or more.9 A similar study of 1,031 French five-year olds found the OR for obesity was 1.4 for a sleep duration less than 11 hours.10
Three smaller studies have examined a broader range of grade school children. A study of 422 Canadian children ages 5–10 found that compared to a sleep duration of 12 hours or more, the ORs for obesity were 1.42 and 3.45 for sleep durations of 10.5–11.5 hours and 10 or fewer hours.11 Two small case-control studies of children ages 6–10 years, one from Brazil and one from Tunisia, reported similar findings. Giugliano et al reported obese children had 31 minutes shorter sleep duration than normal weight children but no significant difference was found between overweight and normal weight children.12 Ben Slama et al found 58% of obese children had a sleep duration less than 8 hours compared to only 11% of non-obese children.13
Four studies have examined the relationship between sleep duration and weight in adolescents. Two of these studies though small, were notable for using objective measures of sleep habits. Measuring sleep duration with wrist actigraphy over a 24-hour period in 383 children aged 11–16, Gupta et al reported one of the strongest associations between short sleep duration and obesity, with the odds of obesity increasing 5-fold for every hour reduction in sleep duration.14 Benefice et al using an accelerometer worn near the hip to assess sleep over 3–4 days in 40 Senegalese girls aged 13–14 years observed sleep duration was reduced by 6.85 min for every 1 kg/m2 increase in BMI.15 This work was notable for demonstrating a sleep-weight relationship in a non-obese population mean BMI was only 16.9 kg/m2. The other adolescent reports included one of 4,486 American teens (mean age 16.6 years) which found short self-reported sleep duration predicted both higher BMI z-score and overweight among boys. However, no relationship was found in girls.16 A study of 656 Taiwanese teenagers (mean age 15.0 years) found the frequency of obtaining a sleep duration of at least 6–8 hours was inversely correlated with obesity risk.17
The consistent findings from studies spanning five continents suggest the reported associations are independent of ethnicity though no formal assessment of effect modification by race has been reported. Several studies suggest boys may be more susceptible to sleep loss than girls. Sekine et al found the OR for obesity associated with a sleep duration less than 8 hours compared to greater than 10 hours was 5.5 in boys and 2.1 in girls.7 Similarly, Chaput et al found the OR for obesity associated with a sleep duration of 10 or fewer hours as opposed to 12 or more hours was 5.7 in boys and 3.2 in girls.11 Knutson et al found the risk of being overweight increased 10% for each hour reduction in sleep duration among boys, while no significant effect was found among girls.16
A few studies have attempted to identify the causal pathway linking sleep duration to obesity. Von Kries et al found no relationship between sleep habits and caloric intake obtained from a food frequency questionnaire.9 Gupta et al using actigraphy and Benefice et al using accelerometry to estimate activity levels each found no relationship between sleep duration and physical activity.14, 15
Cross-sectional studies in adults
Nineteen studies have focused on the cross-sectional relationship between sleep duration and weight in adults (Table 2). The findings have been less consistent than the pediatric literature. Eleven studies reported a clear association between short sleep duration and increased weight and two studies reported mixed findings with an association found in one gender but not the other. Five studies reported no association between short sleep duration and increased weight while one found short sleep duration was associated with reduced weight. In addition, six studies have found evidence that long sleep durations are also associated with increased weight resulting in a U-shaped curve between sleep duration and weight. In general, obesity has been defined as a BMI ≥ 30 kg/m2 based on either measured or self-reported height and weight. Habitual sleep duration has been typically obtained via questionnaire.
Table 2.
Cross-sectional studies of sleep duration and weight in adults.
| Author Country Year | Sample Size | Age Range or Mean | Population Source | Weight Measure | Sleep Measure | Potential Confounders Addressed | Pattern of Association |
|---|---|---|---|---|---|---|---|
| Gortmaker56 USA 1990 | 712 | --- | Harvard School of Public Health | Reported BMI | 1 sleep question | None | No association between SD and BMI. |
| Vioque35 Spain 2000 | 1,772 | ≥ 15 | Health and Nutritional Survey of Valencia | Measured BMI | 1 sleep question | Age, sex, smoking, SES, marital status, physical activity, TV viewing | Short SD associated with increased obesity risk. |
| Shigeta34 Japan 2001 | 453 | 53 | Hospital clinic | Measured BMI | 1 sleep question | None | Short SD associated with increased obesity risk. |
| Heslop18 UK 2002 | 6,797 | 35–64 | Work places in Scotland | Measured BMI | 1 sleep question | Age, sex | Short SD associated with higher BMI in men but not women. |
| Kripke5 USA 2002 | 1,116,936 | 33–102 | American Cancer Society volunteers | Reported BMI | 1 sleep question | Sex | Inverse linear association between SD and BMI in men, U- shaped association in women. |
| Tamakoshi19 Japan 2004 | 104,010 | 40–79 | Japan Collaborative Cohort Study | Reported BMI | 1 sleep question | Sex | Short SD associated with lower BMI. |
| Amagai20 Japan 2004 | 11,325 | 19–93 | Jichi Medical School Cohort Study | Measured BMI | Bedtime/wake-time questions | Sex | No association between SD and BMI. |
| Cournot26 France 2004 | 3,127 | 32–62 | VISAT study | Measured BMI | Bedtime/wake-time questions | Age, sex, smoking, SES, marital status, physical activity, TV viewing, shiftwork, naps, age at menarche, parity, menopause, medications | Short SD associated with higher BMI in women but not men. |
| Ohayon30 Europe 2004 | 8,091 | 55–101 | Random sampling in 7 European countries | Reported BMI | Night-time/daytime sleep questions | Age, sex, smoking, alcohol, caffeine, SES, physical activity, depression, anxiety, stress, medical disorders, insomnia | No association between short night-time SD and BMI but positive association between long night-time SD and underweight. |
| Taheri27 USA 2004 | 1,024 | 53 | Wisconsin Sleep Cohort Study | Measured BMI | 6 day Sleep Diary | Age, sex | U-shaped association between SD and BMI. |
| Bjorkelund22 Sweden2005 | 1,462 | 38–60 | Population-based cohort of Gothenburg | Measured BMI, WHR | 1 sleep question | Sex | Inverse association between SD and both BMI and WHR. |
| Ohayon31 France 2005 | 1,026 | ≥ 60 | Population-based cohort of Paris | Reported BMI | Night-time/daytime sleep questions | Age, sex, smoking, alcohol, caffeine, SES, physical activity, depression, anxiety, stress, medical disorders, insomnia, sleepiness, cognition, social supports | Short night-time SD associated with increased BMI category. No association between total SD and BMI category. |
| Singh23 USA 2005 | 3,158 | 18–65 | Population-based cohort of Detroit | Reported BMI | Weekday/weekend sleep questions | Age, sex, ethnicity, alcohol, medical disorders, OSA | Short SD associated with increased obesity risk. |
| Vorona33 USA 2005 | 924 | 18–91 | 4 Primary Care Clinics | Measured BMI | Weekday/weekend sleep questions | Sex, sleep disorders | Short SD associated with increased BMI category. |
| Gottlieb21 USA 2006 | 5,910 | 40–100 | Sleep Heart Health Study | Measured BMI | Weekday/weekend sleep questions | None | U-shaped association between SD and BMI. |
| Kohatsu28 USA 2006 | 990 | 48 | Employed adults in rural Iowa | Measured BMI | 1 sleep question | Age, sex, alcohol, SES, physical activity, depression, OSA | Inverse association between SD and BMI. |
| Lauderdale32 USA 2006 | 669 | 35–49 | CARDIA Study | Measured BMI (3 y prior to sleep assessment) | 72 hr actigraphy | Age, sex, ethnicity, smoking, alcohol, SES, physical activity, OSA, shiftwork, bedpartner, children | No association between SD and BMI. |
| Moreno24 Brazil 2006 | 4,878 | 40 | Male truck drivers in Sao Paulo | Measured BMI | 1 sleep question | Age, sex, smoking, alcohol, illicit drugs, medical disorders, OSA | Short SD associated with increased obesity risk. |
| Chaput29 Canada 2007 | 740 | 21–64 | Quebec Family Study | Measured BMI, WHR, skinfold thicknesses, body fat mass | 1 sleep question | Age, sex, physical activity | U-shaped association between SD and obesity risk. |
| Ko25 China 2007 | 4,793 | 17–83 | Hong Kong union members | Measured BMI, waist circumference | 1 sleep question | Age, sex, smoking, alcohol, medical disorders, work time | Inverse association between SD and both BMI and waist circumference. |
Estimates provided with 95% confidence intervals or p-values in parentheses if available. BMI: body mass index; WHR: waist-hip ratio; SD: sleep duration; OR: odds ratio (unless otherwise specified, all odds ratios are for obesity; CARDIA: Coronary Artery Risk Development in Young Adults; SES: socioeconomic status; TV: television; OSA: obstructive sleep apnea.
The largest studies reporting on the association between sleep duration and weight were designed as prospective cohort studies to examine the effects of a wide range of behaviors on health outcomes and were not specifically designed to study sleep duration.5, 18–20 Furthermore, data on the cross-sectional association between sleep duration and weight in these cohorts were presented as part of analyses designed to assess sleep duration as a predictor of mortality and so focused on the potential of weight to confound the sleep – mortality association. As a result, only the marginal associations between sleep duration and BMI were computed. The largest of these studies was a survey by the American Cancer Society of over 1.1 million individuals.5 This study found a U-shaped association between sleep duration and BMI among women with the minimum at 7 hours and a monotonic trend in men such that longer sleep durations were associated with a lower BMI. Comparing a sleep duration of 4 hours to 7 hours, women had a 1.39 kg/m2 greater BMI and men had a 0.57 kg/m2 greater BMI. The next largest study was a Japanese cohort of over 100,000 individuals.19 This is the only study to find short sleep durations associated with reduced weight. Mean BMI in those with sleep durations ≤ 4, 5, 6, and 7 hours were 22.2, 22.6, 22.9 and 22.7 kg/m2 for men and 22.6, 22.9, 22.9, and 22.9 kg/m2 for women. A second Japanese cohort of over 10,000 individuals found no association between sleep duration and weight.20 On the other hand, a Scottish study of 6,797 individuals found mean BMI was 0.3 kg/m2 greater among men with a sleep duration less than 7 hours compared to 7–8 hours.18 Two other studies considered weight as a secondary outcome. The Sleep Heart Health Study, in studying the association of sleep duration with hypertension, found a U-shaped association between sleep duration and weight with BMI 0.7 kg/m2 and 0.4 kg/m2 greater in those with sleep durations less than 6 hours and 6–7 hours compared to 7–8 hours.21 A Swedish study of sleep duration and diabetes found sleep duration was inversely correlated with both BMI (r=−0.06) and waist-hip ratio (r=−0.08).22
Two studies using population-based sampling techniques have directly assessed the relationship between short sleep duration and obesity in middle-aged populations. The larger studied 3,158 adults and found an inverse association between sleep duration and obesity with a minimum risk associated with a sleep duration of 8–9 hours.23 Compared to this group, the ORs for obesity were 1.85, 1.49, 1.24, and 1.09 for sleep durations ≤ 5, 5–6, 6–7, and 7–8 hours. A second study of 1,772 Spanish subjects found a similar association with the odds of obesity 39% greater in those with a sleep duration of 6 or fewer hours compared to a sleep duration of 7 hours.
Several studies have examined the sleep – weight association in working populations. A survey of 4,878 Brazilian truck drivers found a sleep duration less than 8 hours per day was associated with a 24% greater odds of obesity.24 Similarly, a survey of 4,793 Hong Kong union members found an inverse correlation between sleep duration and BMI (r=−0.037, p=0.02).25 This relationship was almost exclusively observed in men. In contrast, a French study of 3,127 workers found that while no association between sleep duration and weight was found in men, among women, those with a sleep duration of 6 hours or less had a 0.63 kg/m2 greater mean BMI than those with longer sleep durations.26 In a study of 1,024 government workers in Wisconsin, a U-shaped association was found using sleep duration based on sleep diaries.27 In multivariate modeling, the minimum BMI corresponded to a sleep duration of 7.7 hours. A cross-sectional study of 990 employed adults in Iowa found that BMI was 0.42 kg/m2 greater for each hour reduction in sleep duration.28
Analysis of a Canadian family-based cohort supports the presence of a U-shaped relationship between sleep duration and obesity.29 The ORs for obesity were 1.63 and 1.51 in women with sleep durations of 5–6 hours and 9–10 hours compared to 7–8 hours. The corresponding values in men were 1.72 and 1.18. Similar associations were found between sleep duration and waist-hip ratio, body fat mass, and skinfold thicknesses.
Two reports have specifically examined the association between sleep duration and weight in geriatric cohorts. Both were designed to define normative sleep habits in the elderly and considered weight as a predictor of sleep duration. The first study recruited 8,091 individuals over the age of 55 from 7 European nations.30 Obesity did not predict being in the lowest 5th percentile of sleep durations. A study of 1,026 French subjects over 60 found those with a BMI > 27 kg/m2 were 3.6 times more likely to report nocturnal sleep duration in the lowest 5th percentile than those with BMI of 20–25 kg/m2.31 However, the obese were also more likely to report daytime naps so that no association existed between total sleep duration and obesity.
Only one study of adults has examined the sleep – weight relationship using an objective measure of sleep duration. Lauderdale et al investigated predictors of sleep duration in 669 individuals and used 72-hr actigraphy to assess average sleep duration.32 In multivariate analysis, the study found a weak inverse correlation between sleep duration and BMI that was not statistically significant.
Two studies have examined the association between sleep habits and weight in clinic populations. Among 924 Americans attending a primary care clinic, sleep duration was longest in those with BMI < 25 kg/m2.33 In a study of 453 Japanese clinic patients, the odds of obesity was nearly double in those with a sleep duration less than 6 hours.34
Overall, the cross-sectional data in adults suggest short sleepers are heavier though the findings are much less consistent than the pediatric data. Several reports have noted a U-shaped association between sleep duration and weight in adults with the lowest BMI associated with a sleep duration of 7–8 hours.5, 21, 27, 29 If this relationship is truly U-shaped, studies that force a linear relationship in modeling the sleep – weight association would underestimate the true effect of short sleep duration and might explain the negative findings in some studies. Ethnic differences in susceptibility to sleep deprivation may also explain the disparate findings as 2 of the 3 Japanese studies were negative. Although no study has directly examined differential susceptibility by ethnicity, several studies have noted that both obesity and sleep deprivation are more common among African-Americans than Caucasians.23, 32 Findings on differences in gender susceptibility have been mixed. While several studies suggested a greater vulnerability in women,5, 26, 29, 33 at least two reports found an association between short sleep duration and obesity existed only in men.18, 25
In terms of understanding the mechanism of any sleep – weight association, four of the studies finding an association between short sleep duration and obesity found this association could not be explained by differences in physical activity.18, 26, 29, 35 In addition, one of the negative studies also found no relationship between sleep duration and physical activity.32 None of the studies assessed caloric intake. However, two studies examined biomarkers that may be relevant to appetite. Short sleep durations were associated with suppressed leptin levels in both the Quebec Family Study and the Wisconsin Sleep Cohort Study after adjusting for obesity.27, 29 Short sleep durations were also associated with elevated ghrelin levels in the Wisconsin cohort.27
Prospective cohort studies
Only two studies have examined the longitudinal relationship between sleep duration and weight in children (Table 3). A British birth cohort of 8,234 children found a monotonic relationship between sleep duration reported by parents at 38 months of age and obesity at age 7 with odds ratios of 1.45, 1.35, and 1.04 for children having sleep durations < 10.5, 10.5–10.9, and 11.0–11.9 hours compared to 12 or more hours.36 A smaller birth cohort of 150 children also found short sleep duration as reported by parents at ages 3–5 predicted overweight at age 9.5.37 Those who became overweight had a sleep duration about 30 minutes less than those who were normal weight at follow-up. Although both studies adjusted for birth weight and weight gain in the first months of life, neither assessed weight at the time of the sleep assessments.
Table 3.
Prospective cohort studies of sleep duration and weight.
| Author Country Year Follow-up Time |
Sample Size |
Baseline Age |
Population source |
Measure of weight |
Measure of Sleep | Potential Confounders Addressed |
Cross-sectional Relationship | Longitudinal Relationship |
|---|---|---|---|---|---|---|---|---|
| Agras37 USA 2004 6.5 years | 150 | 3 | Birth cohort from San Francisco | Measured BMI | 1 sleep question to parents each year over 3 years | Age, ethnicity, SES, physical activity, TV viewing, diet, breastfeeding, eating behaviors, birthweight, parental obesity, parental attitudes towards eating and weight, temperatment, parental age | Not assessed. | Short SD associated with increased overweight risk. |
| Hasler38 Switzerland 2004 13 years | 496 | 27 | Zurich Cohort Study | Reported BMI | 3 sleep questions (bedtime, wake-time, and sleep latency) at 4 time points | Age, sex, smoking, SES, physical activity, eating behaviors, parental obesity, depression | Short SD associated with increased obesity risk. | Short SD associated with increased obesity risk. |
| Gangwisch6 USA 2005 9 years | 9,588 | 32–86 | NHANES | Measured & reported BMI | 1 sleep question | Age, sex, ethnicity, smoking, alcohol, SES, physical activity, depression, insomnia, sleepiness | U-shaped association between SD and obesity risk. | Short SD associated with increased obesity risk. |
| Reilly36 UK 2005 4 years | 8,234 | 3 | ALSPAC | Measured BMI | 1 sleep question to parents | Age, sex, maternal smoking, SES, TV viewing, diet, birthweight, parental obesity | Not assessed. | Short SD associated with increased obesity risk. |
| Patel3 USA 2006 16 years | 68,183 | 45–65 | Nurses Health Study | Reported BMI | 1 sleep question | Age, sex, smoking, alcohol, caffeine, SES, physical activity, diet, medical disorders, OSA, shiftwork, menopause, medications | U-shaped association between SD and obesity risk. | Short SD associated with increased obesity and weight gain risk. |
All estimates provided with 95% confidence intervals in parentheses. BMI: body mass index; SD: sleep duration; OR: odds ratio; HR: hazard ratio; NHANES: National Health and Nutrition Examination Survey; ALSPAC: Avon Longitudinal Study of Parents and Children; SES: socioeconomic status; TV: television; OSA: obstructive sleep apnea.
Three studies have examined the longitudinal relationship between sleep duration and weight in adults. The largest was an analysis of 68,183 women ages 45–65 in the Nurses Health Study followed for 16 years.3 Questionnaire response regarding sleep duration was obtained at baseline and self-reported weights were obtained at baseline and every 2 years subsequently. Cross-sectionally, a U-shaped association was found with minimum weight in those having a sleep duration of 7 hours. Longitudinally, a modest association between short sleep duration and weight gain was found. Adjusting for differences in baseline weight, weight gain was 1.14 kg and 0.71 kg greater over 16 years among those with sleep durations ≤ 5 and 6 hours compared to 7 hours. The hazard ratios for obesity were 1.15 and 1.06 for sleep durations ≤ 5 and 6 hour respectively while the hazard ratios for a 15 kg weight gain were 1.28 and 1.10.
An analysis of 9,588 participants in the NHANES study used measured heights and weights at baseline but relied on self-reported weights at subsequent timepoints.6 At baseline, a U-shaped association was found between sleep duration and BMI with the minimum at 7 hours. The strength of the sleep – obesity relationship appeared to wane with age such that the odds ratios for obesity associated with a sleep duration of 4 hours or fewer relative to 7 hours were 3.21, 1.81, and 1.71 among those ages 32–49, 50–67, and 68–86. Because the strongest cross-sectional association was in the youngest tertile, longitudinal analyses were only reported in this subgroup. Over nine years, a linear relationship between sleep duration and weight gain was found with those having a sleep duration of 4 hours or fewer gaining 1.46 kg/m2 and those having a sleep duration of 10 hours or more gaining only 0.08 kg/m2. Individuals with a sleep duration less than 5 hours were twice as likely to be obese after nine years compared to those with a sleep duration of 7 hours.
Hasler et al followed 496 27-year olds in the Zurich Cohort Study over 13 years.38 Height and weight were self-reported while sleep duration was calculated from questions regarding bedtime, wake-time, and sleep latency. These questions were asked at four separate times. In cross-sectional analyses, the association between a sleep duration less than 6 hours and obesity was found to weaken with increasing age. The odds ratios were 7.4, 8.1, 4.7, and 1.1 at ages 27, 29, 34, and 40. In longitudinal modeling, the rate of change of BMI was found to have a monotonic relationship with sleep duration such that those with a sleep duration less than 5 hours gained weight at a rate of nearly 0.4 kg/m2/year while those with a sleep duration more than 9 hours actually lost weight. Interestingly, sleep duration appeared to be more strongly associated with BMI at the prior time point than concurrent or future BMI. For example, the ORs for a sleep duration less than 6 hours at age 29 were 11.8 with obesity at age 27, 8.1 with obesity at age 29, and 4.6 with obesity at age 34.
Overall, the prospective studies have been consistent in finding an increased risk of weight gain and obesity in those with short sleep durations. Several of these studies attempted to assess causal pathways. While the Nurses Health Study found short sleep duration was associated with reduced physical activity, adjustment for these differences did not affect the magnitude of the sleep - weight association.3 Similarly, associations found in the Zurich Cohort Study and NHANES persisted in models that incorporated physical activity.6, 38 Two studies used food frequency questionnaires to estimate total caloric intake as well as intakes of particular food groups.3, 36 In addition, one study performed a quantitative assessment of 24-hour caloric intake.37 None of these studies found the relationship between sleep duration and weight was weakened by controlling for dietary differences.
Discussion
Overall, the published literature supports the presence of an association between sleep duration and weight. However, substantial differences in study designs including whether sleep duration was modeled as a cause or consequence of obesity preclude direct comparisons across studies or quantitative synthesis through meta-analysis. Differences in definitions of normal and short sleep durations also varied substantially across studies. Among children, short sleep duration was defined anywhere from less than 8 hours to less than 11 hours per night while definitions of normal sleep duration ranged from at least 8 hours to more than 12 hours.10, 13 A 6 year old with 9 hours of sleep could be classified as having short, intermediate, or long sleep duration depending on the study.7, 9, 13 Even in studies of adults where greater consensus regarding sleep needs exists, the definitions of normal sleep duration ranged greatly across studies from at least 6 hours to at least 9 hours.34, 35
Despite this variability in defining exposure, across the 13 pediatric studies, results were fairly uniform: short sleep duration was positively associated with increased weight. The findings among adult studies were more mixed. This may in part reflect a more complex relationship between sleep duration and weight in this age group with many studies reporting a U-shaped cross-sectional association. Some of the negative results may therefore be due to the fact that in these studies, long sleepers were not specifically separated from normal sleepers. Interestingly, both the NHANES and Nurses Health Study found a positive association between long sleep durations and obesity assessed simultaneously but no association with future obesity, suggesting the cross-sectional relationship might be due to reverse causation or residual confounding.3, 6 Potential mechanisms for an association between long sleep duration and obesity, whether causal or not, include depression, low socioeconomic status, and societal isolation.39
The robust pediatric data as well as the negative findings in the two studies focusing on geriatric cohorts suggest the relationship between sleep duration and weight may weaken with age. Data from prospective studies support this hypothesis.6, 38 In the Zurich Cohort Study, the cross-sectional relationship between sleep duration and weight weakened as participants aged. In the NHANES population, the association between short sleep duration and weight was most apparent in the youngest tertile. Thus, overall, the literature suggests short sleep duration may represent an independent risk factor for weight gain and obesity particularly in children and younger adults.
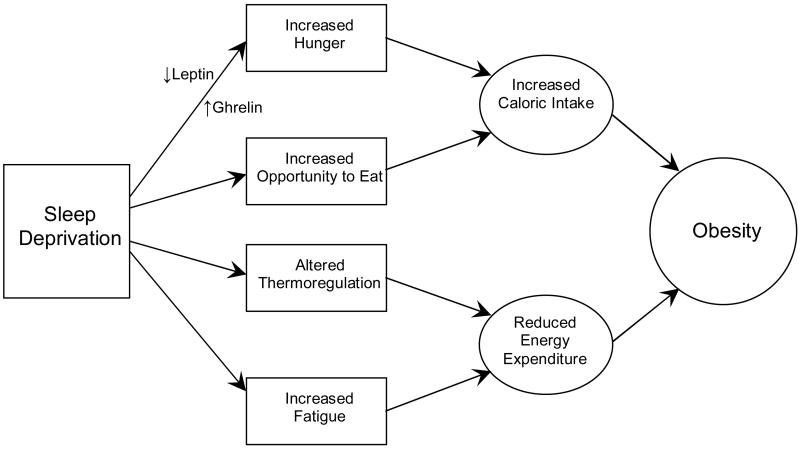
A number of causal pathways linking short sleep duration with obesity have been suggested based on experimental studies of sleep deprivation (Figure 1). One mechanism by which sleep deprivation might predispose to weight gain is by increasing caloric intake. Total sleep deprivation experiments in animals have consistently found sleep deprivation produces hyperphagia.40 Partial sleep deprivation experiments in humans suggest a similar effect. Comparing 4 hours of sleep opportunity per night to 10 hours over a period of 2 days, both hunger and appetite scores on a visual analog scale were elevated by sleep deprivation.4 Furthermore, these increases were particularly notable for high fat and high carbohydrate foods. These changes corresponded with elevations in serum ghrelin and reductions in serum leptin suggesting sleep deprivation may impact peripheral regulators of hunger. A study restricting sleep for six consecutive days found a similar reduction in leptin that persisted throughout the 24 hour day.41 Alternatively, some have argued that in an environment where food is readily available, curtailed sleep may simply represent an increased opportunity to eat especially if most of wake-time is spent in sedentary activities such as watching television where snacking is common.42 In the epidemiologic literature, those studies that attempted to quantify caloric intake found no relationship between sleep duration and dietary consumption.3, 9, 36, 37 However, two epidemiologic studies have demonstrated that short sleepers have reduced levels of leptin and elevated levels of ghrelin study supporting an effect of short sleep durations on appetite regulation.27, 29
Figure 1.
Potential mechanisms by which sleep deprivation may predispose to obesity.
Chronic partial sleep deprivation also clearly leads to feelings of fatigue.2 This tiredness may lead to reductions in physical activity. In fact, cross-sectional studies in children have found short sleep durations to be associated with increased television viewing and reduced participation in organized sports.9, 10 In the Nurses’ Health Study and Nurses’ Health Study 2, short sleep durations were associated with reduced reported physical activity.3, 39 None of the epidemiologic studies that assessed physical activity found differences in activity could explain the sleep-weight association. Similarly, none of the studies that assessed television viewing found the sleep – obesity relationship could be explained by this factor.7, 9–11, 35–37 Finally, studies of acute sleep deprivation in humans have found a drop in core body temperature, suggesting sleep loss may impact energy expenditure through thermoregulation.43 No epidemiologic study of sleep duration to date has assessed thermoregulation. However, a recent study found no association between reported sleep duration and total energy expenditure measured using doubly labeled water.44
Despite the general consistency in the presence of a sleep – weight association, there are important limitations in the current literature that limit the ability to definitively conclude that short sleep duration causes accelerated weight gain. One concern is the rarity of objective measurements of sleep duration. Although polysomnography is infeasible in large cohorts and the recording instrumentation may itself interfere with sleep, other methods of objectively measuring sleep exist. Wrist actigraphy uses a monitor the size of a wristwatch to measure motion in the arm and has been validated against polysomnography.45, 46 Unfortunately, only two studies of sleep duration and obesity to date have utilized actigraphy and both used recording times that were too short to incorporate variability across the week.14, 32 Most studies have relied on questionnaires to assess sleep. However, the wording of these questions varies greatly across studies and few questions have been validated. The Nurses Health Study question is one of the few exceptions; in a subgroup of the cohort, this question showed good correlation (r=0.79) with one week of sleep diaries.47 However, the correlation between sleep diaries and actigraphy has been moderate at best (r=0.57 for nocturnal sleep and r=0.48 for daytime sleep).48 In addition, many studies asked only about nocturnal sleep which may substantially underestimate sleep duration in populations where napping or shift-work is common. The importance of this problem is demonstrated by the study by Ohayon et al where short nocturnal sleep durations were associated with obesity but no association was found with overall sleep duration because the obese were more likely to nap during the day.31 The large night to night variability in sleep duration may also lead to substantial measurement error. Of particular concern is the fact that sleep habits vary greatly between weekdays and weekends. Several studies have reported sleep duration is 0.6 hours longer on average on weekends.1, 32 These differences are even larger in those who have more severe sleep restriction during the week. It is unclear how accurately individuals are able to average their sleep habits over weekdays and weekends to answer a single question about usual sleep habits.
Given the lack of interventional trial data, another concern in inferring short sleep duration promotes obesity is the possibility of reverse causation. Obesity increases the risk of medical conditions such as osteoarthritis, gastroesophageal reflux, asthma, and heart failure that can disrupt sleep and lead to insomnia.49–52 Obesity is the strongest risk factor for obstructive sleep apnea which has as its hallmark disruption of sleep.53 Several studies have attempted to control for these co-morbidities by including the presence of these diseases as covariates in multivariate modeling.3, 23, 24, 28, 32, 33 Another argument against reverse causation comes from the positive findings in pediatric studies where the prevalence of co-morbid disorders related to obesity are rare. Whether obesity has an effect on sleep independent of its medical complications is unclear, but the data suggest any effect is in the opposite direction. Inflammation associated with obesity may lead to the release of soporific cytokines producing longer sleep durations.54 A mouse model of diet-induced obesity supports the notion that obesity increases sleep duration.55
The positive findings from all five longitudinal studies support the contention that short sleep duration causes weight gain rather than vice versa. However, only one study made repeated measurements of sleep to consider the opposite causal relationship.38 In that study, weight was a better predictor of future sleep duration than sleep duration was of future weight. This suggests the causal direction may be reversed, although the findings may also be explained by a waning effect of sleep duration on weight with aging.
The possibility of residual confounding is another concern. Conditions that have been associated with both short sleep durations and obesity and might therefore bias measures of the effect of sleep duration on weight include medical disorders such as chronic pain syndromes as well as psychiatric disorders such as depression. Such conditions may limit an individual’s ability to be physically active as well as interfere with sleep continuity. In addition, many medications can adversely affect both weight and sleep duration. Several studies have attempted to measure and control for co-morbid medical and psychiatric disorders as well as medication use through multivariate analysis.3, 6, 24, 28, 38 Because the Zurich Cohort Study was designed to investigate psychiatric outcomes, detailed assessments of depressive symptoms were performed and the sleep – weight association was found to be independent of depression.38 Again, findings from pediatric cohorts where co-morbidity and medication use are rare argue against the observed sleep – weight association being due to confounding from medical or psychiatric disease.
Socioeconomic status may also confound the sleep-weight relationship. People of lower socioeconomic status may have less favorable sleep environments, work longer hours, and work less desirable hours such as rotating or overnight shifts resulting in poor sleep. Low income has been associated with reduced sleep durations.32 However, many studies have adjusted for socioeconomic status in multivariate analyses and have found the sleep-weight association persisted.6, 9–11, 16, 26, 28, 35–38
The prevalence of chronic partial sleep deprivation has increased dramatically in the past half century, in parallel with the growing epidemics of overweight and obesity. Currently, 40% of American adults report obtaining less than 7 hours of sleep.1 In this systematic review, findings from many cross-sectional investigations as well as five prospective cohort studies suggest short sleep duration may be a novel and independent risk factor for weight gain and obesity, particularly in younger populations. Clearly, however, further research, particularly from large prospective cohort studies with objective measurement of sleep habits and repeated measures of both sleep duration and weight, is needed to more definitively establish a causal link and to better define the magnitude of any causal effect. In addition, further physiologic studies in both human and animal models are needed to better define the pathways by which sleep curtailment might impact weight regulation. In the end, controlled trials will be needed to assess the potential for sleep-promoting interventions to combat the obesity epidemic.
Acknowledgments
This work was supported by NIH research grants HL081385, DK58845, P30 DK46200, and CA87969 as well as the American Heart Association.
References
- 1.2005 Sleep in America Poll. Washington: National Sleep Foundation; 2005. [Google Scholar]
- 2.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 3.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–54. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spiegel K, Tasali E, Penev P, Van Cauter E. Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141:846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 6.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 7.Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between short sleeping hours and childhood obesity: results of the Toyama Birth Cohort Study. Child Care Health Dev. 2002;28:163–70. doi: 10.1046/j.1365-2214.2002.00260.x. [DOI] [PubMed] [Google Scholar]
- 8.Padez C, Mourao I, Moreira P, Rosado V. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr. 2005;94:1550–7. doi: 10.1080/08035250510042924. [DOI] [PubMed] [Google Scholar]
- 9.von Kries R, Toschke AM, Wurmser H, Sauerwald T, Koletzko B. Reduced risk for overweight and obesity in 5- and 6-y-old children by duration of sleep--a cross-sectional study. Int J Obes Relat Metab Disord. 2002;26:710–6. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 10.Locard E, Mamelle N, Billette A, Miginiac M, Munoz F, Rey S. Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes Relat Metab Disord. 1992;16:721–9. [PubMed] [Google Scholar]
- 11.Chaput JP, Brunet M, Tremblay A. Relationship between short sleeping hours and childhood overweight/obesity: results from the ‘Quebec en Forme’ Project. Int J Obes (Lond) 2006;30:1080–5. doi: 10.1038/sj.ijo.0803291. [DOI] [PubMed] [Google Scholar]
- 12.Giugliano R, Carneiro EC. Factors associated with obesity in school children. J Pediatr (Rio J) 2004;80:17–22. [PubMed] [Google Scholar]
- 13.Ben Slama F, Achour A, Belhadj O, Hsairi M, Oueslati M, Achour N. [Obesity and life style in a population of male school children aged 6 to 10 years in Ariana (Tunisia)] Tunis Med. 2002;80:542–7. [PubMed] [Google Scholar]
- 14.Gupta NK, Mueller WH, Chan W, Meininger JC. Is obesity associated with poor sleep quality in adolescents? Am J Hum Biol. 2002;14:762–8. doi: 10.1002/ajhb.10093. [DOI] [PubMed] [Google Scholar]
- 15.Benefice E, Garnier D, Ndiaye G. Nutritional status, growth and sleep habits among Senegalese adolescent girls. Eur J Clin Nutr. 2004;58:292–301. doi: 10.1038/sj.ejcn.1601781. [DOI] [PubMed] [Google Scholar]
- 16.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 17.Chen MY, Wang EK, Jeng YJ. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health. 2006;6:59. doi: 10.1186/1471-2458-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–14. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 19.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–4. [PubMed] [Google Scholar]
- 20.Amagai Y, Ishikawa S, Gotoh T, et al. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14:124–8. doi: 10.2188/jea.14.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 22.Bjorkelund C, Bondyr-Carlsson D, Lapidus L, et al. Sleep disturbances in midlife unrelated to 32-year diabetes incidence: the prospective population study of women in Gothenburg. Diabetes Care. 2005;28:2739–44. doi: 10.2337/diacare.28.11.2739. [DOI] [PubMed] [Google Scholar]
- 23.Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: A population-based study. J Clin Sleep Med. 2005;1:357–363. [PubMed] [Google Scholar]
- 24.Moreno CR, Louzada FM, Teixeira LR, Borges F, Lorenzi-Filho G. Short Sleep Is Associated with Obesity among Truck Drivers. Chronobiol Int. 2006;23:1295–303. doi: 10.1080/07420520601089521. [DOI] [PubMed] [Google Scholar]
- 25.Ko GT, Chan JC, Chan AW, et al. Association between sleeping hours, working hours and obesity in Hong Kong Chinese: the ‘better health for better Hong Kong’ health promotion campaign. Int J Obes (Lond) 2007;31:254–60. doi: 10.1038/sj.ijo.0803389. [DOI] [PubMed] [Google Scholar]
- 26.Cournot M, Ruidavets JB, Marquie JC, Esquirol Y, Baracat B, Ferrieres J. Environmental factors associated with body mass index in a population of Southern France. Eur J Cardiovasc Prev Rehabil. 2004;11:291–7. doi: 10.1097/01.hjr.0000129738.22970.62. [DOI] [PubMed] [Google Scholar]
- 27.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kohatsu ND, Tsai R, Young T, et al. Sleep duration and body mass index in a rural population. Arch Intern Med. 2006;166:1701–5. doi: 10.1001/archinte.166.16.1701. [DOI] [PubMed] [Google Scholar]
- 29.Chaput JP, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec Family Study. Obesity. 2007;15:253–261. doi: 10.1038/oby.2007.512. [DOI] [PubMed] [Google Scholar]
- 30.Ohayon MM. Interactions between sleep normative data and sociocultural characteristics in the elderly. J Psychosom Res. 2004;56:479–86. doi: 10.1016/j.psychores.2004.04.365. [DOI] [PubMed] [Google Scholar]
- 31.Ohayon MM, Vecchierini MF. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28:981–9. [PubMed] [Google Scholar]
- 32.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 33.Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005;165:25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 34.Shigeta H, Shigeta M, Nakazawa A, Nakamura N, Yoshikawa T. Lifestyle, obesity, and insulin resistance. Diabetes Care. 2001;24:608. doi: 10.2337/diacare.24.3.608. [DOI] [PubMed] [Google Scholar]
- 35.Vioque J, Torres A, Quiles J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. Int J Obes Relat Metab Disord. 2000;24:1683–8. doi: 10.1038/sj.ijo.0801434. [DOI] [PubMed] [Google Scholar]
- 36.Reilly JJ, Armstrong J, Dorosty AR, et al. Early life risk factors for obesity in childhood: cohort study. Bmj. 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: a prospective study from birth to 9.5 years. J Pediatr. 2004;145:20–5. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 38.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27:661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 39.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rechtschaffen A, Bergmann BM. Sleep deprivation in the rat by the disk-over-water method. Behav Brain Res. 1995;69:55–63. doi: 10.1016/0166-4328(95)00020-t. [DOI] [PubMed] [Google Scholar]
- 41.Spiegel K, Leproult R, L’Hermite-Baleriaux M, Copinschi G, Penev PD, Van Cauter E. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71. doi: 10.1210/jc.2004-1003. [DOI] [PubMed] [Google Scholar]
- 42.Sivak M. Sleeping more as a way to lose weight. Obes Rev. 2006;7:295–6. doi: 10.1111/j.1467-789X.2006.00262.x. [DOI] [PubMed] [Google Scholar]
- 43.Shaw PJ. Thermoregulatory Changes. In: Kushida CA, editor. Sleep Deprivation: Basic Science, Physiology, and Behavior. New York: Marcel Dekker; 2005. pp. 319–338. [Google Scholar]
- 44.Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. Jama. 2006;296:171–9. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- 45.Jean-Louis G, von Gizycki H, Zizi F, et al. Determination of sleep and wakefulness with the actigraph data analysis software (ADAS) Sleep. 1996;19:739–43. [PubMed] [Google Scholar]
- 46.Jean-Louis G, von Gizycki H, Zizi F, Spielman A, Hauri P, Taub H. The actigraph data analysis software: I A novel approach to scoring and interpreting sleep-wake activity. Percept Mot Skills. 1997;85:207–16. doi: 10.2466/pms.1997.85.1.207. [DOI] [PubMed] [Google Scholar]
- 47.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 48.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–83. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- 49.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 50.Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo CA., Jr Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med. 2006;354:2340–8. doi: 10.1056/NEJMoa054391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13. doi: 10.1056/NEJMoa020245. [DOI] [PubMed] [Google Scholar]
- 52.Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–8. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 53.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 54.Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab. 1997;82:1313–6. doi: 10.1210/jcem.82.5.3950. [DOI] [PubMed] [Google Scholar]
- 55.Jenkins JB, Omori T, Guan Z, Vgontzas AN, Bixler EO, Fang J. Sleep is increased in mice with obesity induced by high-fat food. Physiol Behav. 2006;87:255–62. doi: 10.1016/j.physbeh.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 56.Gortmaker SL, Dietz WH, Jr, Cheung LW. Inactivity, diet, and the fattening of America. J Am Diet Assoc. 1990;90:1247–52. 1255. [PubMed] [Google Scholar]