Abstract
Although coagulase-negative staphylococci (C-NS) have been implicated in certain human infections, they are generally regarded as contaminants, and their clinical significance is questioned. To assess their role as pathogens, we studied 205 isolates of C-NS from wounds and body fluids (blood, urine, pleural and peritoneal fluids, etc.). Patient's charts were reviewed, and, by using strict criteria, a determination was made regarding the clinical significance of these isolates. The organisms were then identified to determine whether certain species of C-NS were associated with specific infections. S epidermidis sensu stricto accounted for 81% of the C-NS isolated. The frequencies of other species were: S. haemolyticus (6%), S. hominis (5%), S. capitis (4%), S. warneri (3%), and others (1%). Only two isolates were novobiocin resistant; neither was identified as S. saprophyticus. By using our criteria, 22% of the C-NS were considered to be clinically significant, and the majority of these (93%) was S. epidermidis. The most common source of the clinically relevant C-NS isolates was wounds. These data suggest that identification of C-NS species other than S. epidermidis may be of limited value in predicting clinical significance.
Full text
PDF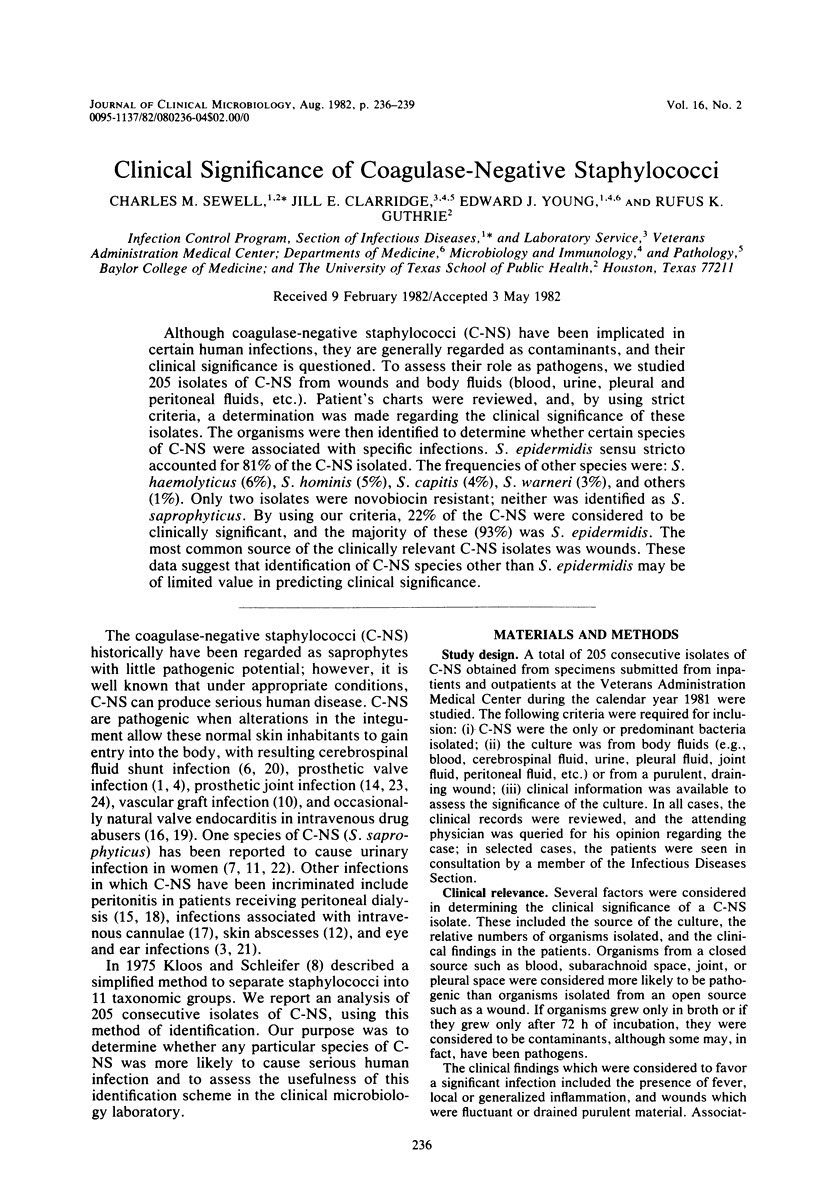
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amoury R. A., Bowman F. O., Jr, Malm J. R. Endocarditis associated with intracardiac prostheses. Diagnosis, management, and prophylaxis. J Thorac Cardiovasc Surg. 1966 Jan;51(1):36–48. [PubMed] [Google Scholar]
- Brun Y., Fleurette J., Forey F. Micromethod for biochemical identification of coagulase-negative staphylococci. J Clin Microbiol. 1978 Nov;8(5):503–508. doi: 10.1128/jcm.8.5.503-508.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feigin R. D., Shackelford P. G., Campbell J., Lyles T. O., Schechter M., Lins R. D. Assessment of the role of Staphylococcus epidermidis as a cause of otitis media. Pediatrics. 1973 Oct;52(4):569–576. [PubMed] [Google Scholar]
- Jordan P. A., Iravani A., Richard G. A., Baer H. Urinary tract infection caused by Staphylococcus saprophyticus. J Infect Dis. 1980 Oct;142(4):510–515. doi: 10.1093/infdis/142.4.510. [DOI] [PubMed] [Google Scholar]
- Kloos W. E., Schleifer K. H. Simplified scheme for routine identification of human Staphylococcus species. J Clin Microbiol. 1975 Jan;1(1):82–88. doi: 10.1128/jcm.1.1.82-88.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liekweg W. G., Jr, Greenfield L. J. Vascular prosthetic infections: collected experience and results of treatment. Surgery. 1977 Mar;81(3):335–342. [PubMed] [Google Scholar]
- Marsik F. J., Brake S. Species identification and susceptibility to 17 antibiotics of coagulase-negative staphylococci isolated from clinical specimens. J Clin Microbiol. 1982 Apr;15(4):640–645. doi: 10.1128/jcm.15.4.640-645.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson F. P., Brown C. S. The McKee-Farrar total hip replacement. Preliminary results and complications of 368 operations performed in five general hospitals. J Bone Joint Surg Am. 1972 Mar;54(2):257–275. [PubMed] [Google Scholar]
- Popovich R. P., Moncrief J. W., Nolph K. D., Ghods A. J., Twardowski Z. J., Pyle W. K. Continuous ambulatory peritoneal dialysis. Ann Intern Med. 1978 Apr;88(4):449–456. doi: 10.7326/0003-4819-88-4-449. [DOI] [PubMed] [Google Scholar]
- Rubin J., Rogers W. A., Taylor H. M., Everett E. D., Prowant B. F., Fruto L. V., Nolph K. D. Peritonitis during continuous ambulatory peritoneal dialysis. Ann Intern Med. 1980 Jan;92(1):7–13. doi: 10.7326/0003-4819-92-1-7. [DOI] [PubMed] [Google Scholar]
- Sapira J. D. The narcotic addict as a medical patient. Am J Med. 1968 Oct;45(4):555–588. doi: 10.1016/0002-9343(68)90172-1. [DOI] [PubMed] [Google Scholar]
- Schoenbaum S. C., Gardner P., Shillito J. Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis. 1975 May;131(5):543–552. doi: 10.1093/infdis/131.5.543. [DOI] [PubMed] [Google Scholar]
- Valenton M. J., Brubaker R. F., Allen H. F. Staphylococcus epidermidis (albus) endophthalmitis. Report of two cases after cataract extraction. Arch Ophthalmol. 1973 Feb;89(2):94–96. doi: 10.1001/archopht.1973.01000040096004. [DOI] [PubMed] [Google Scholar]
- Wallmark G., Arremark I., Telander B. Staphylococcus saprophyticus: a frequent cause of acute urinary tract infection among female outpatients. J Infect Dis. 1978 Dec;138(6):791–797. doi: 10.1093/infdis/138.6.791. [DOI] [PubMed] [Google Scholar]
- Wilson P. D., Jr, Amstutz H. C., Czerniecki A., Salvati E. A., Mendes D. G. Total hip replacement with fixation by acrylic cement. A preliminary study of 100 consecutive McKee-Farrar prosthetic replacements. J Bone Joint Surg Am. 1972 Mar;54(2):207–236. [PubMed] [Google Scholar]
- Wilson P. D., Jr, Salvati E. A., Aglietti P., Kutner L. J. The problem of infection in endoprosthetic surgery of the hip joint. Clin Orthop Relat Res. 1973 Oct;(96):213–221. [PubMed] [Google Scholar]


