Abstract
Background
It has been shown before that when compared with the medial para-patellar approach, the mid-vastus approach for TKR results in less post-operative pain for patients and more rapid recovery of straight leg raise. As far as we are aware the post-operative length of stay of the two groups of patients has not been compared. We postulated that the reduced pain and more rapid recovery of straight leg raise would translate into an earlier, safe, discharge home for the mid-vastus patients compared with those who underwent a traditional medial para-patellar approach.
Methods
Twenty patients operated on by each of five established knee arthroplasty surgeons were evaluated prospectively with regard to their pre and post-operative range of movement, time to achieve straight leg raise post-operatively and length of post-operative hospital stay. Only one of the surgeons performed the mid-vastus approach, and the measurements were recorded by physiotherapists who were blinded as to the approach used on each patient.
Results
The results were analysed using a standard statistical software package, and although the mean length of stay was lower for the mid-vastus patients, the difference did not reach a level of significance (p = 0.13). The time taken to achieve straight leg raise post-operatively was significantly less in the mid-vastus group (p<0.001).
Conclusion
Although this study confirms previous findings that the mid-vastus approach reduces the time taken for patients to achieve straight leg raise, when compared with the medial para-patellar approach, on its own it does not translate into a significantly shorter length of hospital stay.
In order to reduce the length of post-operative hospital stay with an accelerated rehabilitation program for TKR, a multi-disciplinary approach is required. Patient expectations, GP support, physiotherapists and nursing staff all have a role to play and the mid-vastus approach, in permitting earlier straight leg raising, significantly contributes to this.
INTRODUCTION
Total knee arthroplasty (TKA) is a very commonly performed, major orthopaedic procedure, and accounts for a large proportion of elective inpatient bed-days. The pressure to improve productivity and efficiency of orthopaedic units is seemingly inexorable and the reduction of post-operative inpatient stay is a constant target to help reduce the pressure on beds.
Inpatient stay and consequently the timing of discharge after TKA is influenced by a variety of pre-operative, operative and post-operative factors.1 We wanted to know if a simple modification to the operative technique could significantly reduce the length of in-patient stay after TKA in this hospital.
Historically the medial para-patellar approach has been the most popular approach to the knee for TKA.2 This involves making a sagittal incision in the quadriceps tendon proximal to its insertion into the patella. More recently the mid-vastus approach has gained in popularity.3 This does not involve disruption of the quadriceps tendon. An elegant study by White et al in 1999,4 showed that all other factors being equal, this approach led to reduced post-operative pain and analgesia requirements and a more rapid recovery of straight leg raise when compared to the medial para-patellar approach.
Post-operative length of stay of the two approaches has not been compared. We postulated that the reduced post-operative pain and more rapid recovery of movement with the mid-vastus approach would translate into an earlier, safe, discharge home for these patients compared with those patients who underwent a traditional medial para-patellar approach.
METHOD
In our prospective, blinded study, twenty consecutive patients operated on by each of five established knee arthroplasty surgeons were evaluated for several parameters. Each of the 100 patients had measurements taken for pre and post-operative range of movement, time taken to regain a straight leg raise and the number of postoperative days spent in hospital prior to discharge.
The exclusion criteria were dementia, patients who were unable to comply with having the measurements taken and those patients who were unable to undertake the standard post-operative physiotherapy regime. Patients, who had significant co-morbidities that might otherwise delay their discharge, or whose discharge was delayed by the time taken to set up appropriate home care packages, were also excluded.
The post-operative physiotherapy regime was the standard extension type regime employed in our institution. This involves incremental increases in the degree of flexion in the post-operative period. The aim is to achieve 90 degrees of flexion prior to discharge, although if steady improvement is being made patients can be allowed home before reaching this milestone. In these cases, more intensive, supervised physiotherapy is arranged on an out-patient basis.
All measurements and data were recorded on a standard pro-forma (Figure 1) by physiotherapists working on the elective orthopaedic unit. Although the physiotherapist recorded who the operating surgeon was in each case, they were blinded as to which approach was used on each patient.
Figure 1.
Sample of patient reference label.
Out of the five study surgeons, one performed the mid-vastus approach in every case and the other four all used the traditional medial para-patellar approach.
The mid-vastus approach was performed according to the technique described by Engh et al. The distal portion of the arthrotomy is identical to the traditional medial para-patellar approach. When the superomedial pole of the patella is reached the arthrotomy turns medially to divide the vastus medialis obliquus in line with its fibres for not more than 4 cm. In this way the quadriceps mechanism is not violated.
In each case a tourniquet was used as was regional anaesthesia in the form of sciatic and femoral nerve blocks.
The results were analysed using the Minitab 14 statistics package.
RESULTS
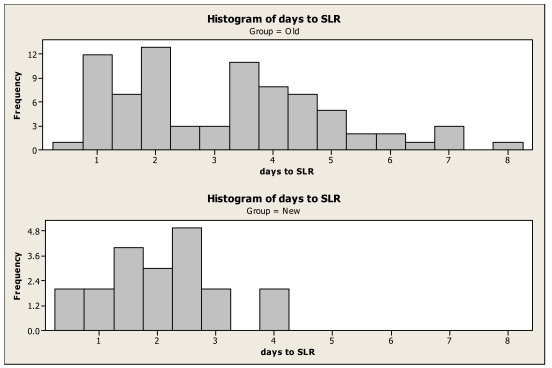
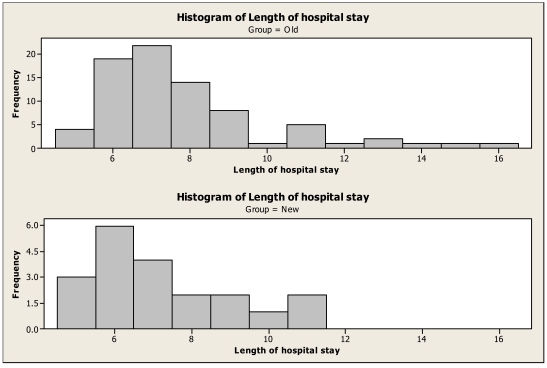
The distribution of the post-operative length of stay (LOS) data was skewed to the right and therefore all analysis of variance tests and t-tests were performed on log (LOS). The time to straight leg raise (SLR) data was reasonably symmetric and no transformation was required (Table 1 and Figure 2).
TABLE 1.
| Variable | Method | n | Mean | StDev | Minimum | Median | Maximum |
|---|---|---|---|---|---|---|---|
| Length of hospital stay | MV | 20 | 7.3 | 1.9 | 5 | 7 | 11 |
| MPP | 80 | 7.8 | 2.3 | 5 | 7 | 16 | |
| Days to SLR | MV | 20 | 2.1 | 1.0 | 0.5 | 2 | 4 |
| MPP | 80 | 3.2 | 1.8 | 0.5 | 3.5 | 8 | |
Figure 2.
Days to straight leg raise. Old = medial para-patellar approach. New = mid-vastus, quadriceps spacing approach.
For the LOS there was no significant difference in means (p = 0.24 using two independent samples t-test on log (LOS)) and no significant difference in variances (p = 0.82 using Levene's test on LOS) (Figure 3). It can also be seen that the median LOS was identical for both approaches (Table 1).
Figure 3.
Old = medial para-patellar approach. New = mid-vastus, quadriceps sparing approach.
For the time to SLR there was a significant difference in means (p = 0.001 using two independent samples t-test with unequal variances) and a significant difference in variances (p = 0.006 using an F-test). The estimated difference in means is 1.1 days (MPP-MV) with a 95% confidence interval of 0.5 to 1.7 days. There is 1.8 times more variation in time to SLR using the MPP approach than there is using the MV approach based on a comparison of standard deviations.
CONCLUSION
The purpose of this study was to see if employing the mid vastus approach for TKR significantly reduced time to discharge when compared to the medial para-patellar approach.
It has already been shown that the length of time a patient stays in hospital after undergoing a TKR is dependant on multiple factors. Crowe and Henderson5 showed that a single pre-operative physiotherapy education session reduced length of hospital stay from 10.5 to 6.5 days. The type of anaesthesia used can also affect length of stay. Wang et al.6 showed that although local nerve blocks generally wear off rapidly (within the first 18 hours) they do provide excellent analgesia allowing early mobilisation and an earlier discharge.
This study confirms the finding of White et-al that the mid-vastus approach significantly reduces the time taken to achieve a straight leg raise after TKR.
It also demonstrates the multi-factorial nature of rehabilitation and shows that by altering the approach alone, in our study at least, the length of hospital stay is not significantly reduced. If a significant reduction in post-operative length of stay is to be achieved then the whole episode needs to be addressed; from pre-operative patient information through surgical and anaesthetic technique to a robust discharge package involving physiotherapists, occupational therapists and general practitioners.
Footnotes
No grants were received towards the project.
REFERENCES
- 1.Shakespeare D., Kinzel V. Rehabilitation after total knee replacement. Time to go home? The Knee. 2005;12:185–189. doi: 10.1016/j.knee.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Insall J.N. A midline approach to the knee. JBJS. 1971;53A:1584–1586. [PubMed] [Google Scholar]
- 3.Engh G.A., Holt B.J., et al. A midvastus muscle splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12:322–331. doi: 10.1016/s0883-5403(97)90030-9. [DOI] [PubMed] [Google Scholar]
- 4.White R.E., Allman J.K., et al. Clinical comparison of the midvastus and medial parapatellar surgical approaches. Clin Orthop and related research. 1999;367:117–122. [PubMed] [Google Scholar]
- 5.Crowe J., Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther. 2003 Apr;70(2):88–96. doi: 10.1177/000841740307000204. [DOI] [PubMed] [Google Scholar]
- 6.Wang H., Boctor B., Verner J. The effect of single-injection femoral nerve block on rehabilitation and length of hospital stay after total knee replacement. Anesth Pain Med. 2002 Mar–Apr;27(2):139–44. doi: 10.1053/rapm.2002.29253. [DOI] [PubMed] [Google Scholar]