INTRODUCTION
Giant cell tumor of bone, sometimes referred to as conventional giant cell tumor, is a benign locally aggressive neoplasm which accounts for five percent of primary osseous neoplasms. Giant cell tumors most commonly occur in the distal femur, proximal tibia and distal radius. This neoplasm usually affects young adults; about two thirds of patients are between ages 20 and 40. Giant cell tumor is very unusual in patients older than age 55.1 This study reports ten patients with giant cell tumor who range in age from age 62 to 78. We discuss whether giant cell tumors in elderly patients behave differently than those that occur in the usual age group. In addition, we outline how problems of differential diagnosis in this age group differ from those in conventional patients.
MATERIALS AND METHODS
These ten patients were collected from the personal consultation files of one of us (EFM). The images, histologic material, and clinical information with follow-up were available on all ten patients (see Table 1).
TABLE 1.
| Case # | Patient Age/Gender | Location | Years of disease free follow up | Treatment | Comments |
|---|---|---|---|---|---|
| 1 | 78/F | Distal femur | 10 | Curettage w/ bone graft | Patient also had osteoarthritis |
| 2 | 70/F | Distal radius | 14 | Curettage w/ bone graft | Patient died of unrelated causes |
| 3 | 73/M | Distal radius | 2 | Resection w/ allograft | |
| 4 | 72/F | Proximal humerus | 6 | Curettage w/ MMA | Extensive fibrohistiocytic reaction |
| 5 | 72/F | Distal femur | 3 | Curettage w/ MMA | |
| 6 | 68/F | Proximal tibia | 3 | Curettage w/ MMA | Patient died of unrelated causes |
| 7 | 64/F | Spine T-ll | 4 | Resection | |
| 8 | 63/F | Proximal tibia | 5 | Curettage w/ MMA | Extensive necrosis |
| 9 | 63/F | Distal humerus | 2 | Curettage | |
| 10 | 62/F | Spine C-4 | 3 | Resection | |
RESULTS
The ten patients ranged from age 62 to age 78. There were three males and seven females. Seven lesions were in long bones, and two were in the vertebrae. Vertebral lesions were T-11 and C-4. In the long bones there were two lesions each in the distal radius, proximal tibia and distal femur. Two patients had involvement of the humerus. All patients presented with pain. One patient (patient 3) presented with a pathologic fracture.
RADIOGRAPHIC FEATURES
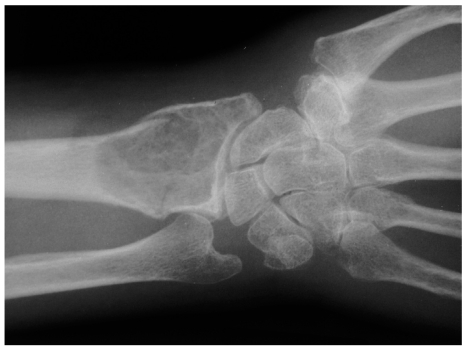
Lesions in the long bone were well defined lytic lesions which involved both the epiphyseal and metaphyseal portions of the bone (Figure 1). Patient 3 presented with a pathologic fracture (Figure 2). Lesions in the spine (patient 7 and patient 10) involved the vertebral body.
Figure 1.
Plain radiograph of the giant cell tumor in the proximal tibia of patient 6. The lesion is a well defined zone of radiolysis involving the epiphyseal and metaphyseal end of the bone. This is a characteristic pattern for giant cell tumor.
Figure 2.
Radiograph of the giant cell tumor of the distal radius from patient 3. There is a pathologic facture through an otherwise typical giant cell tumor.
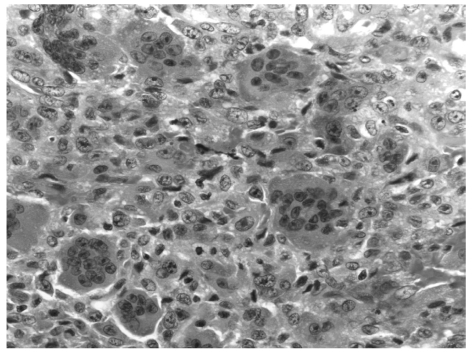
HISTOLOGIC FEATURES
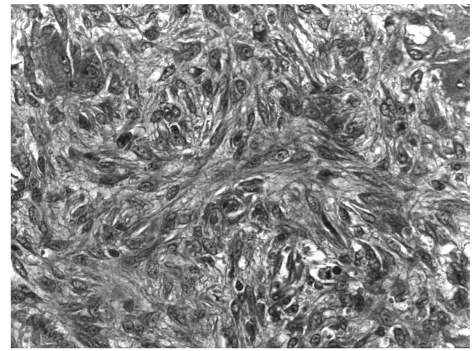
All lesions showed characteristic features of conventional giant cell tumor of bone (Figure 3). Two patients had extensive secondary histologic features. Patient 4 had a pronounced fibrohistiocytic reaction (Figure 4) and patient 8 showed extensive necrosis throughout the lesion.
Figure 3.
(right) Photomicrograph (H&E x 40) of the giant cell tumor from patient 5. The histologic features are characteristic of giant cell tumor.
Figure 4.
Photomicrograph (H&E x 40) of the lesion from patient 4 showing extensive fibrohistiocytic reparative reaction.
With the exception of the two spinal lesions and the fractured distal radius lesion which were treated with resection, all other lesions were treated with curettage followed by bone graft or methyl methacrylate cement. Two patients died from causes unrelated to the giant cell tumor. Patient 1 died after a 14 year disease free follow up and patient 6 died after 4 years with no evidence of recurrence. All other patients are disease free from two years to ten years.
DISCUSSION
Rare isolated reports of giant cell tumors in patients over age 60 illustrate either chromosomal imbalances or treatment options.2,3 Numerous large series of giant cell tumors include a few elderly patients. However, these series do not focus on any distinctive features in these older patients.4,5,6,7 The ten cases in the present series illustrate that the behavior of giant cell tumor in elderly patients is no different from lesions occurring in more commonly involved younger patients. First, the location distribution is identical. In this series, the most common locations were the distal femur, proximal tibia and distal radius. These are the most common locations for giant cell tumor in all age groups. Second, the radiographic features of these lesions are identical to the giant cell tumors in younger patients. Lesions are well defined and involve both the epiphyseal and metaphyseal portions of the long bone. Third, the behavior of these lesions is identical to giant cell tumors in general. In fact, lesions in this age group may be less aggressive than those in younger patients because there were no recurrences. In general the recurrence rate after curettage for giant cell tumor is between 25 and 35 percent. Although recurrence may be delayed as long as fourteen years,4 almost all recurrences occur before two years.8 In our study, two years was the minimum follow up. Two patients showed histologic features of senescence (necrosis and fibrohistiocytic repair). These features may be signs of indolent lesions present for many years.
Giant cell tumor of bone in elderly patients presents diagnostic problems that are not seen in the more commonly involved younger patients. First, in this age group, the most common bone neoplasm is metastatic carcinoma. Although metastatic carcinoma favors the axial skeleton, some carcinomas will metastasize to the ends of long bones. Moreover, some carcinomas, including carcinomas of the breast, kidney, lung and pancreas, contain heavy populations of osteoclast-like giant cells.9 This histologic pattern may be mistaken for giant cell tumor of bone. Therefore, metastatic carcinoma must be ruled out in giant cell tumor patients in this age group. Lesions in these elderly patients should be stained with cytokeratin despite the number of giant cells present.
A second differential diagnostic problem in this age group is pigmented villonodular synovitis. From 15 to 50 percent of cases of pigmented villonodular synovitis involve bone.10 Because the process arises in joints, the bone involvement is almost always epiphyseal and metaphyseal, identical to the bone destruction pattern seen in giant cell tumor.11 Also, pigmented villonodular synovitis has a large population of giant cells which can be mistaken for giant cell tumor. Indeed, pigmented villonodular synovitis in bone can be mistaken for a primary bone neoplasm (Figure 5). A pre-operative MRI will help eliminate this diagnostic confusion because pigmented villonodular synovitis will show extensive synovial membrane involvement and secondary bone invasion.
Figure 5.
Radiograph of a 54 year old man with pigmented villonodular synovitis of the knee. There is extensive bone erosion in the proximal tibia which is causing radiolysis of the epiphysis and metaphysis. This is producing an identical radiographic picture as a conventional giant cell tumor.
A third differential diagnostic problem in this age group is the possibility that patients may have, instead of a giant cell tumor, a large osteoarthritic cyst. Large osteoarthritic cysts, sometimes known as geodes, involve the subchondral bone and may spread into the metaphysis causing identical radiographic features of giant cell tumor.12,13 Sometimes the evidence of osteoarthritis is minimal. Any older patient with an epiphyseal metaphyseal lesion should be carefully evaluated for the presence of osteoarthritis (Figure 6). The presence of an osteoarthritic cyst can be confirmed with an MRI that shows a bright signal on a T-2 weighted image. This will help eliminate the possibility of a giant cell tumor.
Figure 6.
Radiograph of a 70 year old man with a large osteoarthritic cyst of the proximal tibia. The radiolysis involves both the epiphysis and the metaphysis in the pattern of a giant cell tumor. However, there is marked medial compartment osteoarthritis which is the clue that this is an osteoarthritic cyst.
Finally, giant cell tumor is a well-documented but rare complication of Paget's disease, a disease of older patients.14,15 Therefore, any elderly patient with a giant cell tumor should be studied for the possibility of Paget's disease.
In summary, giant cell tumor of bone in elderly patients has a similar biologic behavior to lesions in the more commonly involved younger patients. In fact, lesions in this age group may be less aggressive. Problems in differential diagnosis can be eliminated if biopsies are studied with cytokeratin immunostains and pre-operative MRIs are done to rule out pigmented villonodular synovitis or osteoarthritic cysts.
REFERENCES
- 1.Dorfman HD, Czerniak B. Bone Tumors. Mosby; 1998. Giant-Cell Lesions; pp. 559–606. [Google Scholar]
- 2.Meyer A, Bastian L, Bruns F. Benign giant cell tumor of the spine: an unusual indication for radiotherapy. Arch Orthop Trauma Surg. 2006;126:517–21. doi: 10.1007/s00402-006-0174-x. [DOI] [PubMed] [Google Scholar]
- 3.Garcia JL, Robeldo C, Lumbreras E, Flores T, Ramos L, Hernandez JM. Analysis of chromosomal imbalances in an elderly woman with a giant cell tumour. Virchows Arch (Pathol Anat) 2006;448:95–9. doi: 10.1007/s00428-005-0079-z. [DOI] [PubMed] [Google Scholar]
- 4.Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, Koehler G, et al. Giant cell tumor of bone: treatment and outcome of 214 cases. J Cancer Res Clin Oncol. 2008;134:969–78. doi: 10.1007/s00432-008-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg. 1987;69-A(1):106–13. [PubMed] [Google Scholar]
- 6.Goldenberg RR, Campbell CJ, Bonfiglio M. Gaint-Cell Tumor of Bone. J Bone Joint Surg. 1970;52-A(4):619–64. [PubMed] [Google Scholar]
- 7.McDonald DJ, Sim FH, McLeod RA, Dahlin DC. Giant-cell tumor of bone. J Bone Joint Surg. 1986;68-A(2):235–42. [PubMed] [Google Scholar]
- 8.Turcotte RE. Giant cell Tumor of Bone. Orthop Clin North Am. 2008;37(l):35–51. doi: 10.1016/j.ocl.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Cantalejo FB, Marco VS, Hernandez SA, Pena RJ, Martorell Cebollada MA. Syncytial giant cell component. Review of 55 renal cell carcinomas. Histol Histopathology. 2004;19:113–8. doi: 10.14670/HH-19.113. [DOI] [PubMed] [Google Scholar]
- 10.Zwass A, Abdelwahab IF, Klein MJ. Case Report 463. Pigmented villonodular synovitis (PVNS) of knee. Skeletal Radiol. 1988;17(l):81–4. doi: 10.1007/BF00361462. [DOI] [PubMed] [Google Scholar]
- 11.Jergesen HE, Mankin HJ, Schiller AL. Diffuse pigmented villonodular synovitis of the knee mimicking primary bone neoplasm. A report of 2 cases. J Bone Joint Surg. 1978;60-A(6):825–9. [PubMed] [Google Scholar]
- 12.Landells JW. The bone cysts of osteoarthritis. J Bone Joint Surg. 1953;35-B(4):643–9. doi: 10.1302/0301-620X.35B4.643. [DOI] [PubMed] [Google Scholar]
- 13.Ondrouch AS. Cyst formation in osteoarthritis. J Bone Joint Surg. 1963;45-B(4):755–60. [PubMed] [Google Scholar]
- 14.Mirra J, Bauer FCH, Grant TT. Giant Cell Tumor with Viral-like Intranuclear inclusions Associated with Paget's Disease. Clin Orthop Relat Res. 1981;158:243–51. [PubMed] [Google Scholar]
- 15.Hoch B, Hermann G, Klein MJ, Abdelwahab IF, Springfield D. Giant cell tumor complicating Paget disease of long bone. Skeletal Radio. 2007;36:973–8. doi: 10.1007/s00256-007-0310-x. [DOI] [PubMed] [Google Scholar]