INTRODUCTION
Although ankle injuries are among the most common injuries that occur in athletes, the severity and degree of these injuries vary greatly owing to the complexity of the ankle and surrounding structures. Compared with lateral ankle sprains, syndesmotic or high ankle sprains occur less often in the general and sport populations and usually experience a longer recovery period further compounding the difficulty of evaluating and treating this type of injury. Syndesmotic injuries that have radiographic widening as evidence of disruption are relatively straightforward in terms of making the diagnosis, and therefore directing treatment. However, as seen much more commonly in sports, those sprains with normal radiographic joint and bony relationships are much more difficult to assess in terms of severity. The reason for the difficulty is that diagnosis is dependent on subjective clinical findings. As a result, these present a significant diagnostic and treatment dilemma for the sports medicine physician. It would be advantageous to be able to delineate the severity of injury in syndesmotic sprains without obvious widening or mechanical abnormalities. The purpose of this paper is to review the literature as a means of elucidating any diagnostic radiographic findings, including MR imaging, with the anticipation this review may lead to further research directions on this topic.
BACKGROUND
Reports of syndesmotic sprain incidence vary from 1% to 11% of all ankle injuries.1,2 Jones et al. conducted an in-depth analysis of several studies and found that time lost from sport due to syndesmosis sprains ranged from 0 to 137 days, with averages ranging from 10 to 14 days up to 52 days.3 The ranges stated illustrate the variability in degree and severity of syndesmotic ankle injury. Furthermore, research conducted on the evaluation and treatment of syndesmotic ankle sprains has been relatively nominal, although interest has grown in recent years.3-9 In a study done by Wright et al. on National Hockey League players, out of 14 syndesmosis ankles sprains examined, only one player showed mortise diastasis on stress x-rays although 74% of ankle injuries studied were syndesmosis injuries.10 Nussbaum et al. also found a low number of radiographs with mortise widening; only 1 out of 17 athletes tested demonstrated widening on his radiograph.11 Therefore, there lies a great importance in augmenting our evaluation and imaging techniques as well as our understanding of the mechanisms and anatomy of tibiofibular syndesmotic injuries in order to improve assessment and management of high ankle sprains with a normal mortise relationship.
ANATOMY
An appreciation of the anatomy related to the syndesmotic relationship is essential in understanding the injury and related pathoanatomy and radiographic findings. In the inferior tibiofibular syndesmosis, the distal fibula (with a convex surface) unites with the distal tibia (with a concave surface).6,12,13 The three ligaments that help stabilize this articulation are the anterior tibiofibular ligament (AITFL), the superficial and deep components of the posterior tibiofibular ligament (PITFL), and the interosseous ligament or membrane. The AITFL originates from the anterolateral tubercle of the tibia and its fibers run in an oblique direction, distally and laterally inserting on the longitudinal tubercle on the anterior border of the lateral malleolus.9,14,15 This ligament may consist of two to three bands or be multi fascicular.16 The AITFL is wider at the tibial insertion than at the fibular insertion, and has been described as having a triangular13 or trapezoidal shape.9,14,15 The PITFL consists of superficial and deep components,6,12,14 although some categorize the deep component as a separate ligament.13,15 The superficial component fulfills the same purpose as the AITFL holding the fibula and tibia together. Originating from the posterolateral distal fibula, the PITFL runs more horizontally and inserts on the posteromedial distal tibia. The deep component, also known as the inferior transverse ligament, is a strong collection of fibers located below the posterior tibial margin and runs from the posterior ridge of the tibia to the lateral malleolar fossa even more horizontally than the superficial component.6,14
The interosseous membrane (IOM) facilitates the prevention of posterolateral bowing of the fibula during activities that place stress on the fibula.17 The IOM connects the tibia and fibula along nearly the entire length of the medial aspect of the two bones and separates the anterior and posterior muscles in the leg.12 Located just above the talocrural joint, the interosseous ligament is a collection of fibers at the distal end of the IOM that mostly run from the tibia to the fibula.14-16 Its function has been described as spring-like, allowing the medial and lateral malleolus to slightly separate during dorsiflexion at the ankle joint.6,16
PATHOANATOMY
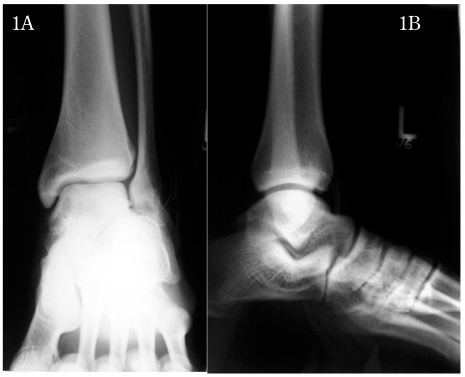
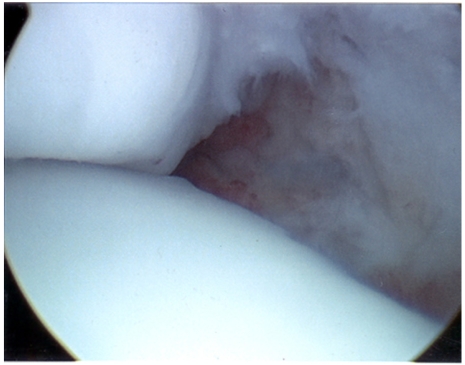
Considering the anatomy, the usual injury pattern of syndesmosis sprains will be easier to understand. In an incomplete syndesmotic sprain, the anterior portion of the AITFL (need to be consistent with abbreviation— choose ATFL or AITFL) may be partially or completely torn as a result of the fibula separating from the tibia in an external rotation mechanism, for example. Although this ligament may be completely torn, normal x-rays taken will still appear to be normal (no mortise widening) as the PITFL (need to be consistent with abbreviation) and interosseous membrane provide enough stability to hold the ankle joint in place (see Figures 1A-B, 2A-D, 3A-B, 4A-B). However, a comprehensive physical examination of the ankle joint should indicate a significant ankle injury, usually because the patient has difficulty pushing off and weight bearing, arousing suspicion of a syndesmosis sprain.
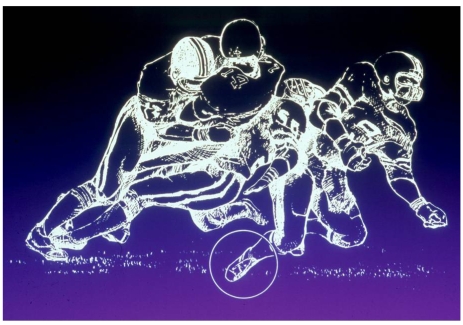
Figure 1A, B.
AP and Lat x-ray of 18 year old football player with high ankle sprain. AP shows lack of tibio fibular overlap.
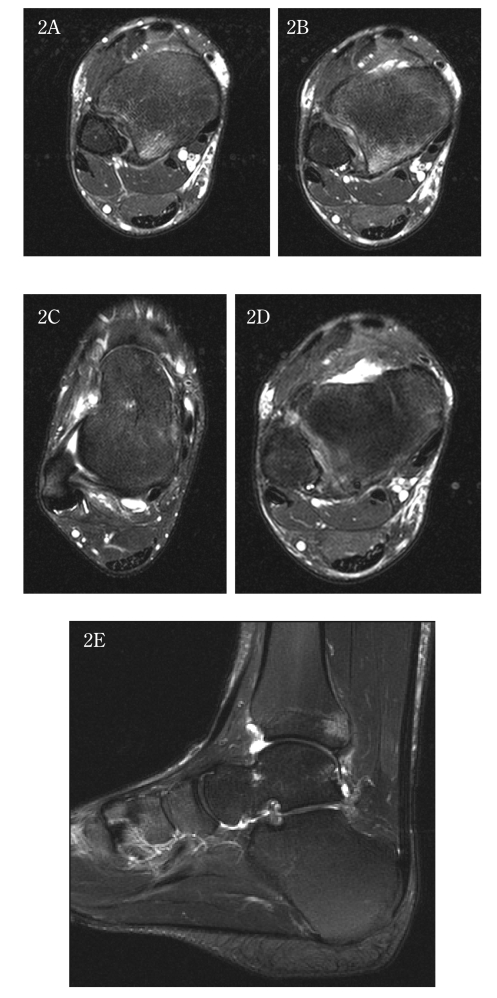
Figure 2.
MRI visualization of syndesmosis sprain through injury to the AITFL and PITFL A, B, C: Edema in the area of the PITFL attachment on the tibia, but the ligament is intact; D: AITFL intact therefore likely ER mechanism, not inversion; E: AITFL is disrupted.
Figure 3.
Arthroscopic view with missing anterior inferior tibio fibular ligament (evidence for disruption).
Figure 4 A, B.
AP and Lat post arthroscopic debridement and fixation with syndesmosis screw.
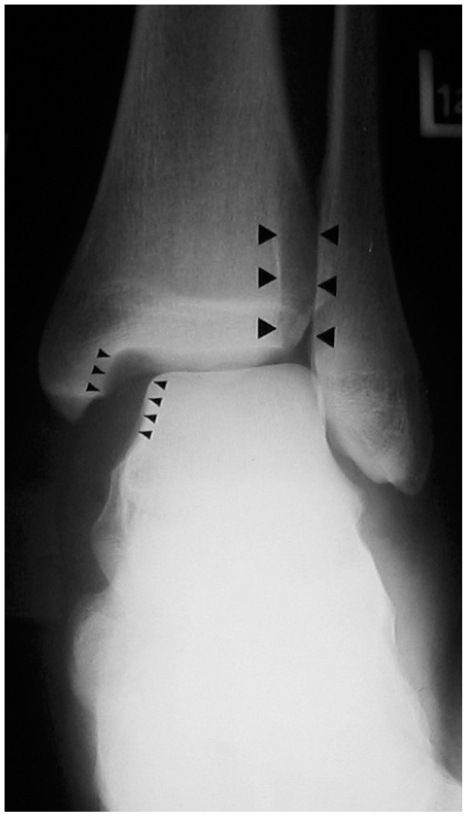
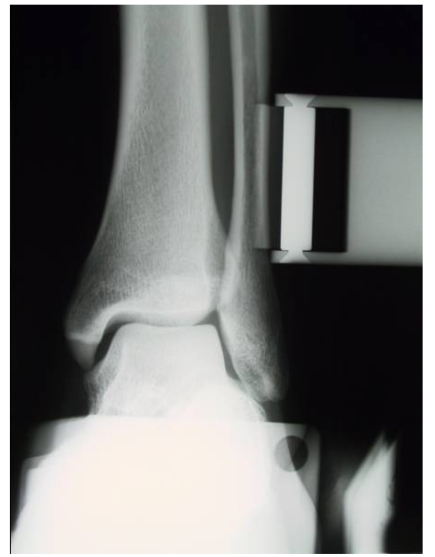
On the other hand, in cases where complete disruption has occurred and mortise widening is present, the diagnosis is generally very clear (see Figure 5). In addition to trauma to the anterior tibiofibular ligament, the deltoid ligament, the posterior tibiofibular ligament and interosseous membrane may be affected as well. As a result, the ankle becomes much less stable and the mortise relationship is not able to be maintained, thus easily seen on radiographs. As mentioned above, mortise widening only occurs in a small percentage of syndesmotic injuries10,11 and usually the radiographic diagnosis is difficult with those partial injuries.
Figure 5.
Radiographic AP view of mortise wid
MECHANISM
Although less frequent in the general population, Boytim et al. noted that there was a greater incidence in the professional football population included in a study on syndesmosis injuries.18 High ankle sprains are more common in collision sports including football, ice hockey, and soccer18 (see Figures 6A, 6B). This suggests that athletes participating in such sports are more susceptible to syndesmosis injuries. Fritschy et al. also did a study on Olympic skiers that experienced external rotation and syndesmotic injury due to the twisting nature of the sport and the rigidness of ski boots.19 External rotation has been described as the most common mechanism for this type of injury, 1,11,18-20 but there have also been reports of hyperdorsiflexion associated with external rotation,1,6,18 axial loading of the ankle,11 and inversion.1 Although these are the major mechanisms which have been discussed, any mechanism which results in a force on the separation of the tibia and fibula or a rotation of the talus within the mortise is significant.
Figure 6A.
External rotation mechanism as often observed in football but can occur in other sports. Drawing courtesy of the late Dr. J. C. Kennedy.
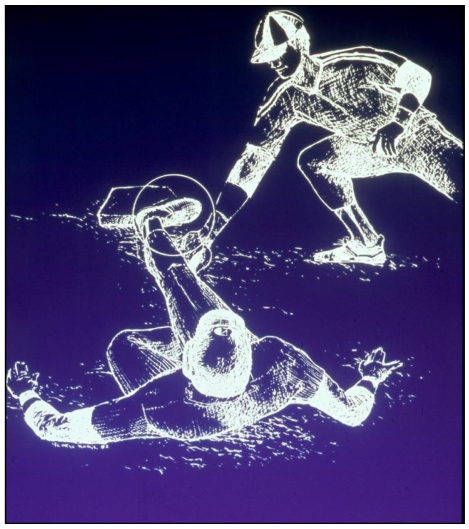
Figure 6B.
Axial loading and hyperdorsiflexion mechanism observed in baseball players sliding into a base; can occur in other sports. Drawing courtesy of the late Dr. J. C. Kennedy.
DIAGNOSIS
In regards to evaluation of syndesmosis sprains, there remains a controversy over the most effective approach.7,8,21,22 In the physical examination, evaluation of the syndesmosis is commonly conducted using localization of pain, anatomic palpation, and a variety of stress tests including the squeeze test, the external rotation test, the fibula-translation (drawer) test, the Cotton test, and the crossed-leg test.3,5,9,18,20,23
EXAMINATION OF THE SYNDESMOSIS SPRAIN (NORMAL MORTISE RELATIONSHIP)
In a syndesmosis without any mortise widening, physical examination may become an important part of diagnosing the patient. Upon reviewing the mechanism involved in a patient's injury, suspicion of a syndesmosis sprain may be raised. If palpating the areas usually affected in a high ankle sprain (AITFL, PITFL, medial malleolus) causes pain, the examiner may surmise further that the syndesmosis is involved in the injury.5,9,18,20 The stability of the ankle joint may be examined by asking the patient to perform a number of maneuvers including performing a toe raise, walking, and jumping. In a gait analysis performed by Spaulding,24 findings showed that syndesmosis injury decreased the ability to push off of the toes while walking, and therefore the above-mentioned actions should be painful or hindered if there is a syndesmosis injury. Described by Williams et al., Amendola has incorporated the “stabilization test,” which is performed by tightly taping patient's leg just above the ankle joint in an attempt to stabilize the syndesmosis9 (see Figure 7A). If toe raises, walking, and/or jumping are less painful upon taping, this would indicate a positive test result9 (see Figure 7B). The Cotton test, performed by translating the talus medial to lateral within the mortise, may also indicate deltoid ligament injury associated with the syndesmosis sprain if increased translation or pain is noted.9,20,23 Finally, as external rotation is one of the more common mechanisms, the external rotation test proves to be useful in confirming suspicions of syndesmosis involvement in the injury (see Figure 8).5,9,11,20,23
Figure 7A.
A stabilization taping technique to assess the injury.
Figure 7B.
Functional activity improves with the taping technique, confirming syndesmotic instability.
Figure 8.
External rotation stress test reproduces pain in the syndesmotic area.
IMAGING
Although helpful in identifying problematic areas, these physical tests are mostly used in conjunction with radiographic findings. With imaging, the ankle may be examined in the anteroposterior (AP), lateral, and mortise views. The mortise view is another form of the AP view internally rotating the tibia by 15° to 20° which allows a better visualization of any diastasis in the syndesmosis.5 Again, with sprains these views will be normal.
SYNDESMOSIS INJURIES WITH MORTISE WIDENING
Among the AP and mortise views, there are a number of measurements taken in an attempt to quantify the severity of the injury. On the AP view, the tibiofibular clear space (TFCS) is measured horizontally between the lateral border of the posterior tibial malleolus at its widest point and the medial border of the fibula.25,26 Also measured horizontally on the AP view, tibiofibular overlap (TFO) is the distance between the medial border of the fibula and the lateral border of the anterior tibial tubercle.25,26 Finally, the medial clear space (MCS) measured on the mortise radiograph is described as the distance between the lateral aspect of the medial malleolus and medial border of the talus.25,26 There remains a controversy over the reliability of these three parameters,5,7,25,26 although a study conducted by Nielson et al. indicates a correlation between MCS widening and deltoid ligament tears.26 Beumer et al. also proposes that syndesmotic injury may be indicated by a unilateral absence of TFO.25
Even though the combination of physical examination and radiology is the more common diagnostic tool in the field of orthopaedics, a number of studies have found that radiographic measurements fail to be entirely reliable due to the difficulty in accurately positioning the ankle even in ideal laboratory conditions.25-27 Therefore, other forms of radiology, including CT (Computed Tomography) and MRI (Magnetic Resonance Imaging) have been utilized in order to improve accurate diagnosis.7,8,21,22,26 It has been noted that CT is more effective at picking out 2-mm and 3-mm diastases than plain radiography.27 Although CT is more sensitive than radiography in visualizing the syndesmosis, more subtle 1-mm diastases remain difficult to pick out in a CT scan.8 Taser et al. introduced a novel solution to this problem. Taser used CT in order to render a three-dimensional reconstruction of the tibiofibular joint space thereby allowing calculations of the volume.8 In this manner, using CT to render three-dimensional images may enable the physician to more effectively grade the severity of a syndesmotic ankle sprain when compared to the normal joint volume.
SYNDESMOSIS SPRAINS: NORMAL MORTISE RELATIONSHIP
Initial investigation should include routine x-rays. Occasionally there may be some suggestion of injury, but not commonly. On a delayed basis, calcification may occur at the posterior tibia and the interosseous membrane following the initial injury (see Figure 9).
Figure 9.
AP view calcification in the interosseous space 2 mos after a high ankle sprain.
Under normal mortise relationship, it remains difficult diagnosing a syndesmosis sprain with plain radiography. If there is suspicion of a syndesmotic injury but no evidence on a plain x-ray, one may choose to perform stress views. These may be performed manually or with a Telos stress device. Beumer et al. utilized the Telos device (Austin and Associates) on cadaver specimens and concluded that external rotation stress radiostereometric analysis (RSA) is useful in detection of some forms of syndesmotic instability.28 However, we have found that due to the stability of the mortise these stress views will usually be stable unless it is a complete disruption. (see Figure 10)
Figure 10A.
External rotation stress test using the Telos device to apply force to the syndesmosis.
Figure 10B.
Radiographic view of the ankle while utilizing the Telos external rotation stress test.
Owing to this uncertainty, close follow-up should be conducted on the patient. Moreover, follow-up is also important in regards to delayed heterotropic ossification occurring on the posterior aspect of the tibia and the distal portion of the interosseous membrane.9,11,18,23 If trauma occurred in the PITFL or the IOM, bleeding may have occurred and subsequently healed as an abnormal formation of bone on these surfaces. It has been noted in the literature that this may not be visible until 6 months after the injury. This reinforces the importance of following up on syndesmosis sprains even after symptoms have subsided.
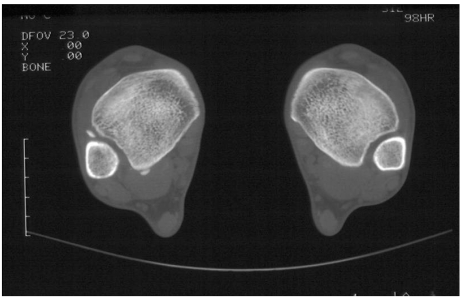
In a CT scan of an ankle with normal mortise relationship, visualization of any diastasis will not be applicable. Therefore, CT has another useful application in order to detect an additional injury associated with some syndesmosis sprains: avulsion fractures. Avulsion fractures occur when a fragment of bone tears away from the main mass of bone where a ligament attaches. In syndesmosis sprains, avulsion fractures may occur on either the anterior or posterior aspect of the tibia and have been noted to occur in up to 50% of syndesmosis injuries.29 In this case, CT becomes an important radiographic tool owing to the fact that avulsion fractures can occur without diastasis (see Figure 11). Therefore, if CT is not utilized this type of fracture may be missed.
Figure 11.
CT view of anterior and posterior avulsion fractures of the tibia as a result of syndesmosis sprain.
MRI provides yet another important method of diagnosing syndesmosis injuries with a normal mortise relationship. Looking at MRI films, it becomes much easier to visualize ligament tears, ankle joint fluid leaking into the tibiofibular space, and edema.4,30 Therefore, syndesmosis sprains may again be identified despite an ankle appearing normal on plain x-ray. Oae et al. found that obtaining transverse sections offered the view most useful for evaluation of the tibiofibular syndesmosis. Furthermore, in their MR imaging study, the two criteria that they employed in assessing ligament disruption were ligament discontinuity and either a wavy or curved ligament contour or nonvisualization of the ligament.7
Utilizing MR imaging, soft tissue injuries are visualized more extensively than plain radiography, allowing the observer to improve assessment of syndesmotic diastasis and ligament damage.4,7,30 Numerous studies have indicated a much higher accuracy, sensitivity, and specificity associated with MR imaging when confirmed by ankle arthroscopy.7,8,21,22 Furthermore, a study done by Brown et al. noted that syndesmotic disruption may be associated with a number of secondary findings in MR imaging including anterior talofibular ligament injury, osteochondral lesions, bone bruise, and tibiofibular joint incongruity4 (see Figures 2A-E).
DISCUSSION
Even after a thorough review of the literature, it is difficult to identify an adequate method of evaluating-syndesmosis sprains with a normal mortise relationship. The literature on these types of injuries is lacking, and the severity of the injuries has been poorly appreciated. As a result, predictions on time lost from sport continue to be elusive to the physician. A complete diagnosis is best made through appropriate imaging modalities in conjunction with and correlated with the history and physical examination. Using all of these tools along with repeat examinations and complete follow-up, it may be easier to determine the extent of the injury.
Currently, more prospective research is needed to accurately assess the extent and severity of these injuries. This information is essential in order to improve predictability of down time associated with syndesmosis sprains as well as conservative versus operative treatment options. Currently, non-operative treatment seems to be the conventional approach, with Nussbaum et al. and Williams et al. both preferring a 3-phase approach.9,11 The first phase (acute phase) aims to protect the injured joint and reduce pain and swelling through complete immobilization (splint, cast, or boot) and pain control. The second phase (subacute phase) includes an increase in exercise intensity with goals of restoring strength and function in basic motions such as ambulation. The third phase (advanced training phase) continues with the goal of discharging the patient back to sports participation. The patient engages in continued strengthening, neuromuscular training, and sport-specific exercises in order to evaluate stability of the syndesmosis. Determining when the patient may return to sports is a difficult decision and is based upon a combination of physical examination and ability to perform sport-specific skills and movements.9,11
If diastasis on plain or stress radiography or arthroscopic evidence of instability in the syndesmosis exists, surgical treatment is recommended. Indications for operative treatment in the case of sprains without any evidence of diastasis still remain controversial. Surgical treatment consists of reduction and fixation of the syndesmosis across the distal fibula and tibia using either 1 or 2 screws or a recently described suture technique known as the TightRope Syndesmosis Repair (Arthrex) which is gaining increased recognition as an alternative to trans- syndesmotic fixation.31 This suture and button technique eliminates complications associated with screws such as hardware pain and screw breakage.
Future investigation and research will likely prove to be very useful in improving knowledge and treatment of syndesmosis injuries. Controversy surrounds almost every aspect of syndesmosis injuries from diagnosis to treatment and more research will help in defining all these aspects of this injury. One important topic of research can include assessing the value of current physical examination techniques and investigating the correlation of new diagnostic techniques. Further investigation on imaging modalities and their value in aiding the evaluation of severity should be helpful. Research on treatment should include investigating conservative versus surgical treatment in patients with very similar severity of syndesmosis sprains, in particular those injuries without syndesmotic widening. Overall syndesmotic sprains still remain a controversial subject, diagnostic imaging remains cloudy at best, and therefore this subject will benefit greatly from further study.
REFERENCES
- 1.Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10:325–30. doi: 10.1177/107110079001000607. [DOI] [PubMed] [Google Scholar]
- 2.Katznelson A, Lin E, Militiano J. Ruptures of the ligaments about the tibio-fibular syndesmosis. Injury. 1983;15:170–2. doi: 10.1016/0020-1383(83)90007-4. [DOI] [PubMed] [Google Scholar]
- 3.Jones MH, Amendola A. Syndesmosis sprains of the ankle: a systematic review. Clin Orthop Relat Res. 2007;455:173–5. doi: 10.1097/BLO.0b013e31802eb471. [DOI] [PubMed] [Google Scholar]
- 4.Brown KW, Morrison WB, Schweitzer ME, Parellada JA, Nothnagel H. MRI findings associated with distal tibiofibular syndesmosis injury. AJR Am J Roentgenol. 2004;182:131–6. doi: 10.2214/ajr.182.1.1820131. [DOI] [PubMed] [Google Scholar]
- 5.Lynch SA. Assessment of the Injured Ankle in the Athlete. J Athl Train. 2002;37:406–12. [PMC free article] [PubMed] [Google Scholar]
- 6.Norkus SA, Floyd RT. The anatomy and mechanisms of syndesmotic ankle sprains. J Athl Train. 2001;36:68–73. [PMC free article] [PubMed] [Google Scholar]
- 7.Oae K, Takao M, Naito K, Uchio Y, Kono T, Ishida J, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology. 2003;227:155–61. doi: 10.1148/radiol.2271011865. [DOI] [PubMed] [Google Scholar]
- 8.Taser F, Shafiq Q, Ebraheim NA. Three-dimensional volume rendering of tibiofibular joint space and quantitative analysis of change in volume due to tibiofibular syndesmosis diastases. Skeletal Radiol. 2006;35:935–41. doi: 10.1007/s00256-006-0101-9. [DOI] [PubMed] [Google Scholar]
- 9.Williams GN, Jones MH, Amendola A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35:1197–207. doi: 10.1177/0363546507302545. [DOI] [PubMed] [Google Scholar]
- 10.Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in national hockey league players. Am J Sports Med. 2004;32:1941–5. doi: 10.1177/0363546504264581. [DOI] [PubMed] [Google Scholar]
- 11.Nussbaum ED, Hosea TM, Sieler SD, Incremona BR, Kessler DE. Prospective evaluation of syndesmotic ankle sprains without diastasis. Am J Sports Med. 2001;29:3l–5. doi: 10.1177/03635465010290011001. [DOI] [PubMed] [Google Scholar]
- 12.Gray H. Gray's anatomy: the anatomical basis of medicine and surgery. 38th. New York: Churchill Livingstone; 1995. [Google Scholar]
- 13.Gray H. Philadelphia: Courage Books; 1999. Anatomy, Descriptive and Surgical. [Google Scholar]
- 14.Bartonicek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25:379–86. doi: 10.1007/s00276-003-0156-4. [DOI] [PubMed] [Google Scholar]
- 15.Ebraheim NA, Taser F, Shafiq Q, Yeasting RA. Anatomical evaluation and clinical importance of the tibiofibular syndesmosis ligaments. Surg Radiol Anat. 2006;28:142–9. doi: 10.1007/s00276-006-0077-0. [DOI] [PubMed] [Google Scholar]
- 16.Saraffian S. Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. 2nd ed. Philadelphia: J.B. Lippincott Company; 1993. [Google Scholar]
- 17.Thomas KA, Harris MB, Willis MC, Lu Y, MacEwen GD. The effects of the interosseous membrane and partial fibulectomy on loading of the tibia: a biomechanical study. Orthopedics. 1995;18:373–83. doi: 10.3928/0147-7447-19950401-11. [DOI] [PubMed] [Google Scholar]
- 18.Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19:294–8. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- 19.Fritschy D. An unusual ankle injury in top skiers. Am J Sports Med. 1989;17:282–5. 5–6. doi: 10.1177/036354658901700223. discussion. [DOI] [PubMed] [Google Scholar]
- 20.Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br. 2008;90:405–10. doi: 10.1302/0301-620X.90B4.19750. [DOI] [PubMed] [Google Scholar]
- 21.Kim S, Huh YM, Song HT, Lee SA, Lee JW, Lee JE, et al. Chronic tibiofibular syndesmosis injury of ankle: evaluation with contrast-enhanced fat-suppressed 3D fast spoiled gradient-recalled acquisition in the steady state MR imaging. Radiology. 2007;242:225–35. doi: 10.1148/radiol.2421051369. [DOI] [PubMed] [Google Scholar]
- 22.Muratli HH, Bicimoglu A, Celebi L, Boyacigil S, Damgaci L, Tabak AY. Magnetic resonance arthrographic evaluation of syndesmotic diastasis in ankle fractures. Arch Orthop Trauma Surg. 2005;125:222–7. doi: 10.1007/s00402-004-0721-2. [DOI] [PubMed] [Google Scholar]
- 23.Amendola A, Williams G, Foster D. Evidence-based approach to treatment of acute traumatic syndesmosis (high ankle) sprains. Sports Med Arthrosc. 2006;14:232–6. doi: 10.1097/01.jsa.0000212329.32969.b8. [DOI] [PubMed] [Google Scholar]
- 24.Spaulding S. Monitoring recovery following syndesmosis spraa case report. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 1995 Oct;:655–60. doi: 10.1177/107110079501601014. [DOI] [PubMed] [Google Scholar]
- 25.Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin Orthop Relat Res. 2004:227–34. doi: 10.1097/01.blo.0000129152.81015.ad. [DOI] [PubMed] [Google Scholar]
- 26.Nielson JH, Gardner MJ, Peterson MG, Sallis JG, Potter HG, Helfet DL, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res. 2005:216–21. doi: 10.1097/01.blo.0000161090.86162.19. [DOI] [PubMed] [Google Scholar]
- 27.Ebraheim NA, Lu J, Yang H, Mekhail AO, Yeasting RA. Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 1997;18:693–8. doi: 10.1177/107110079701801103. [DOI] [PubMed] [Google Scholar]
- 28.Beumer A, Valstar ER, Garling EH, van Leeuwen WJ, Sikma W, Niesing R, et al. External rotation stress imaging in syndesmotic injuries of the ankle: comparison of lateral radiography and radiostereometry in a cadaveric model. Acta orthopaedica Scandinavica. 2003;74:201–5. doi: 10.1080/00016470310013969. [DOI] [PubMed] [Google Scholar]
- 29.Sclafani SJ. Ligamentous injury of the lower tibiofibular syndesmosis: radiographic evidence. Radiology. 1985;156:21–7. doi: 10.1148/radiology.156.1.4001407. [DOI] [PubMed] [Google Scholar]
- 30.Vogl TJ, Hochmuth K, Diebold T, Lubrich J, Hofmann R, Stockle U, et al. Magnetic resonance imaging in the diagnosis of acute injured distal tibiofibular syndesmosis. Invest Radiol. 1997;32:401–9. doi: 10.1097/00004424-199707000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Cottom JM, Hyer CF, Philbin TM, Berlet GC. Treatment of syndesmotic disruptions with the Arthrex Tightrope: a report of 25 cases. Foot & ankle international / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society. 2008;29:773–80. doi: 10.3113/FAI.2008.0773. [DOI] [PubMed] [Google Scholar]