Abstract
Distal tibia fractures remain difficult injuries to treat when fracture displacement precludes non-operative treatment. Different methods of treatment including limited internal fixation with external fixation, as well as open reduction and internal fixation have been recommended. Open reduction and internal fixation is often favored for the improved ability to anatomically reduce displaced fractures, particularly articular fractures. However, wound complications due to the associated trauma to the fragile soft tissue envelope in this region continue to be a significant concern.
The authors present a surgical approach for open reduction and fixation of distal tibia and fibula fractures through a single lateral incision, which respects the angiosomes of the distal leg and ankle. This can, in some cases, resolve the need to delay ORIF of the tibia since the incision is essentially the same as that used for the immediate ORIF of fibula fractures, which is commonly used in the staged treatment of distal tibial and plafond fractures. This approach can be extended proximally and distally to allow treatment of other injuries about the ankle and hindfoot. Illustrative cases are provided.
INTRODUCTION
Current treatment of displaced pilon fractures is frequently performed with immediate ORIF of the distal fibular fracture and delayed ORIF of the tibial plafond by various approaches,1-4 which require temporary spanning external fixation of the medial side of the ankle. Delay of ORIF of the tibia is based on the concern of the risk of significant wound healing problems with early incisions over the tibia whether anteromedial or anterolateral.3,4 The anteromedial approach provides good exposure of the articular surface centrally and medially and allows for placement of a medial buttress plate to support the comminuted metaphyseal portion of the fracture. It is however less advantageous for exposure of the lateral column of the distal tibia and the syndesmosis. This is especially important in cases where the lateral tibial plafond is dissociated from the fibula and indirect reduction of this lateral fragment cannot be obtained by reducing the fibula fracture. The anteromedial approach has been associated with concerning wound complications. When wound complications do occur with the anteromedial approach they can leave the distal tibia and hardware exposed. Even when healing is uneventful, the subcutaneous location of an anteromedial plate can lead to patient discomfort.3,6-8 The minimally invasive percutaneous plating through a medial approach has been recommended by some9,10 but often the skin over the medial malleolus, which is the location of the incision for inserting the plate, is particularly thin and commonly traumatized with displaced fractures. For these reasons, delayed treatment has been recommended to minimize the risk of wound complications.5
An anterolateral approach to distal tibial pilon fractures has been described.11,12 This approach uses a skin incision placed between the distal tibia and fibula, overlying the anterior border of the fibula. This approach avoids the fragile medial soft tissues and allows for a single incision for plating of both the tibia and fibula fractures. This approach also has the advantages of utilizing a single incision for open reduction and internal fixation of both the distal tibia and fibula, and provides excellent exposure of the articular surface and lateral plafond, and lateral column of the distal tibia.11 However, the superficial peroneal sensory nerve is at risk as it traverses this incision and must be directly identified and retracted. Also, the anterior perforating peroneal artery originates from the deep posterior compartment and passes anteriorly through the hiatus that lies between the proximal aspect of the syndesmosis and the interosseous membrane. While this is often traumatized by the injury, and is frequently not of significant size, it can be the sole dorsal artery of the foot in 3% of cases. A wound dehiscence however will occur directly over the hardware for both the tibia and fibula.
The direct lateral approach to the distal tibia and fibula is performed through a skin incision that is made along the posterior border of the fibula, which is the same incision used for immediate fixation of distal fibula fractures. This incision is generally considered safe for performing immediate open reduction and internal fixation of the distal fibula in cases of displaced and intra-articular distal tibia fractures. The deep portion of the dissection used to approach the tibia from the lateral side does not involve any devitalization of the bone or of the soft tissue flap overlying the distal tibia. The incision preserves the angiosomes of the anterior skin over the distal tibia and ankle by keeping the anterior soft tissues envelope completely intact and thus preserving the blood supply from the anterior tibial artery13 (Figure 1). This approach provides excellent exposure of all aspects of both the tibia and fibula fractures, and when closure is performed the intact anterior compartment soft tissues lie over the bone and hardware, which are well away from the skin incision (Figure 2). The superficial peroneal nerve is also maintained within the anterior soft tissue flap without the need for subcutaneous dissection (Figure 3). The anterior perforating peroneal artery can be identified and if intact can be preserved when warranted, although it rarely supplies the anterior skin to any significant extent, since the anterior tibial artery usually provides most of the anterior angiosome (Figure 4). Extension of the incision distally utilizes the standard lateral hindfoot approach, and the proximal extent of the incision can reach the proximal third junction of the tibia, and would only limited by the proximal branching of the common peroneal nerve and anterior tibial artery through the interosseous membrane.
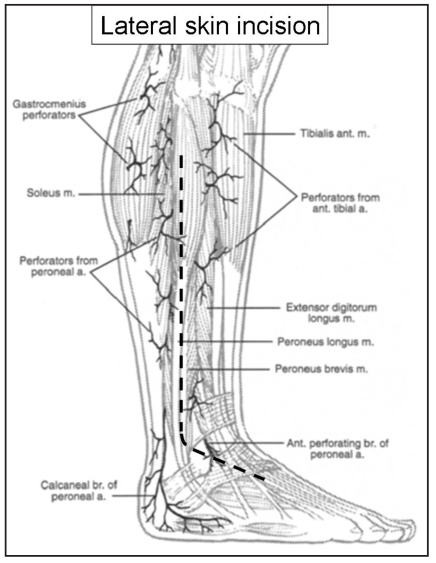
Figure 1.
The lateral skin incision was made between the course of the terminal calcaneal branch and anterior perforating branch of the peroneal artery. Reprinted with permission from Attinger, C. Vascular anatomy of the foot and ankle.
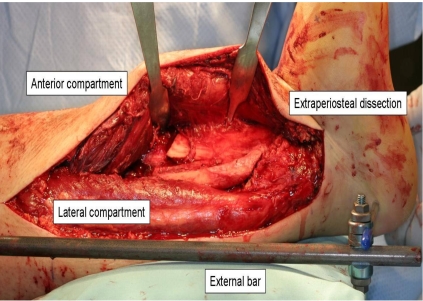
Figure 2.
Exposure to the distal tibia from the single extensile lateral approach in an extraperiosteal plane. The anterior compartment has been mobilized with only release of the superior extensor retinaculum and anterior compartment fascia from the intermuscular septum.
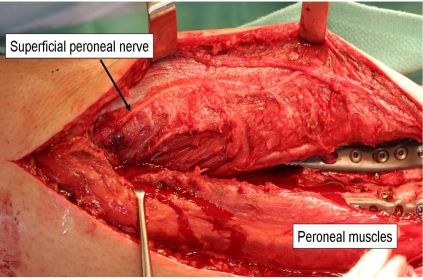
Figure 3.
The superficial peroneal nerve crosses anteriorly. In this case the nerve was mobilized with the anterior compartment after the intermuscular septum was released. No dissection at the fascial exit or in the subcutaneous plane was needed.
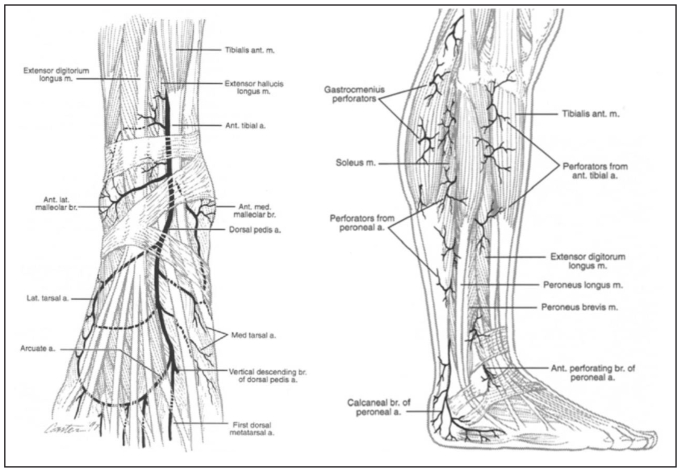
Figure 4.
The typical anastomosis of the anterior perforating branch of the peroneal artery and the lateral malleolar artery supplies the skin over anterolateral part. Reprinted with permission from Attinger, C. Vascular anatomy of the foot and ankle. Operative Techniques in Plastic and Reconstructive Surgery1997;4:183 - 198.
OPERATIVE TECHNIQUE
A lateral skin incision is made along the posterolateral border of the fibula. At the tip of the fibula this is then directed toward the base of the fourth metatarsal. The skin incision is extended to the level of the anterior calcaneal process, although deep dissection distally is not necessary unless there is an associated talus, calcaneal or cuboid fracture. The dissection is deepened to the fibula and extraperiosteal dissection is carried anteriorly to the anterior syndesmotic fibers and the attachment of the superior extensor retinaculum (SER) onto the fibula. The SER is released sharply off of the anterior border of the fibula with care not to inadvertently cut the underlying anterior perforating branch of the peroneal artery. If the vessel is intact it is usually easiest to directly cauterize it, as it can retract posteriorly if cut at the interosseous membrane exit (Figure 5). The only other soft tissue attachment that must be released is the anterior ankle joint capsule. A blunt elevator such as a freer is passed in the extraperiosteal plane deep to the anterior compartment just above the ankle joint. This plane is advantageous because there are no soft tissue attachments to the distal tibia anteriorly, as the anterior compartment structures must glide over the bone in this area to allow for necessary soft tissue excursion with ankle and hindfoot motion. The anterolateral capsule of the ankle joint is thin and can be found between the inferior aspect of the anterior syndesmotic fibers and the superior border of the anterior talofibular ligament (ATFL). A freer elevator is used to retract the anterior soft tissues, while another freer elevator is placed across the anterior ankle joint to retract the anterior joint capsule anteriorly as well. This places the anterior ankle joint capsule attachment onto the tibia under tension. It can then be sharply elevated off of the anterior edge of the tibial plafond. In some cases the ATFL can be sharply incised to allow for greater visualization of the tibial articular surface. This can later be directly repaired. Proximally the plane between the anterior and lateral compartments is followed until the superficial pe-roneal nerve (SPN) is identified. It can run along either side of the intermuscular septum, but most commonly within the lateral compartment. The nerve is mobilized without the need for superficial dissection in most cases (Figure 3). In some cases a fibula fracture may occur at the fascial exit of the SPN, in which case a local release of the nerve at the fascial exit may be prudent. At this point the anterior flap can be retracted medially, and broad exposure of the tibia can be appreciated (Figure 2). If the anterior perforating peroneal artery is still intact after the fracture and preserving it is preferred, such as in the case of a large vessel that represents the main blood supply to the dorsal foot, then it is best to use angled retractors rather than a straight retractor to avoid stretching the vessel. The distal 6-7cm of the tibia can be easily approached without sacrificing the vessel, but a plate can be slid beneath it and accessed above and below. Fortunately this anatomic variant is rare occurring only 3% of the time. Posteriorly, the fibula can be exposed by release of the lateral compartment from the posterolateral border of the fibula with preservation of the superior peroneal retinaculum (SPR). The authors prefer to reduce and fix the tibia first to gain anatomic length and alignment and allow the fibular fracture to provide easier access to the tibial fracture. The syndesmotic incisura is reconstructed and the fibula is reduced and fixed. Medial malleolar fractures can be visualized and reduced from the lateral side and percutaneous fixation can be placed through an incision placed distal to the medial malleolus or at a later time if the medial skin is too fragile even for this (Figure 6).
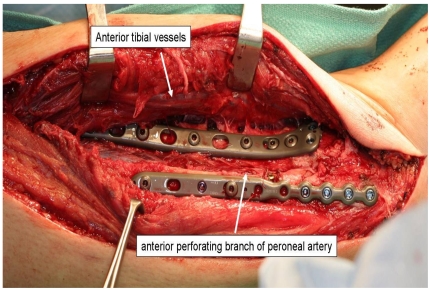
Figure 5.
The anterior perforating branch of peroneal artery which was sacrificed in this case does not lend any meaningful blood supply to the anterior ankle skin flap.
Figure 6.
Anatomic reduction and fixation of a Pilon fracture, syn-desmotic disruption and fibula fracture. A medial malleolar fracture reduction can be visualized through the lateral incision and fixation applied percutaneously through an incision placed distally.
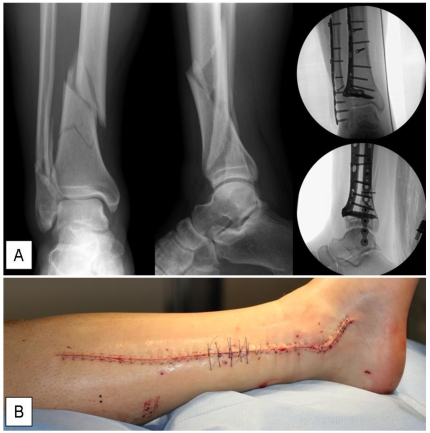
Figure 7.
(A) An anatomical reduction and internal fixation with lateral plating of distal tibia and fibula, which was not amenable to intramedullary rodding due to traumatic abrasion over the knee. Operative treatment was performed within 24 hours of injury.(B) The closed surgical skin incision of the direct lateral approach.
Finally, the syndesmosis can be reduced and fixed and any remaining soft tissue reconstruction such as the ATFL or SPR can be repaired.
Proximal Extension
The incision can be extended proximally by furthering the mobilization of the anterior compartment off the interosseous membrane and releasing the anterior compartment fascia from the intermuscular septum. There is at least one perforating vessel from the deep posterior compartment that will require cauterization. The proximal extension is limited only by the branching of the common peroneal nerve and the tibial artery exiting through the proximal interosseous membrane.
Distal Extension
Distal extension of the incision can allow access to the lateral talus, calcaneus via the sinus tarsi and the calcaneocuboid joint. The inferior extensor retinaculum can be mobilized from the lateral talar neck for exposure of a talar neck fracture. The inferior extensor retinacular attachment to the calcaneus can be released and the extensor digitorum brevis muscle reflected distally and dorsally to expose the calcaneocuboid joint. The sinus tarsi and posterior facet of the calcaneus are directly observed at this level, inferior to the Anterior talofibular ligament.
DISCUSSION
The classic principles of the treatment of pilon fractures were described by Ruedi and Allgower in 1979. They included restoration of fibular length, anatomical reconstruction of the articular surface of the tibia, bone-grafting to the metaphyseal defect and use of a medial buttress plate.14 Operative treatment of distal tibial fractures requires flexibility in choosing a treatment based on the fracture pattern and soft tissue injuries. One limitation of the classic approach of Ruedi and Allgower is that the lateral column of the tibia does not always reduce with reduction of the fibula. Lateral approaches are thus more favorable for approaching this fragment and the syndesmosis injury. Newer plates allow for buttressing of the metaphyseal fracture from the lateral side as opposed to the medial side, thus large medial plates can be avoided in some cases.6,15 Some fracture patterns may not be amenable to a lateral-only approach, and smaller medial incisions for placement of augmentation may be required.5 The combined medial and lateral incisions may be at risk of skin slough, particularly if the injury involves more extensive soft tissue damage or as has been reported, the two incisions are not separated by 7 centimeters or more.16 Knowledge of the angiosomes and vascular anatomy of skin over the ankle would make the length of parallel incisions and the skin bridge between the edges of the bipedicle flap created by parallel incisions more important than the absolute distance between two incisions.
The posterolateral approach which makes incision through the abundant soft-tissue coverage of the posterior distal tibia does not eliminate the complications common to others approaches.17 The postero-medioanterior approach has been described for pilon fracture which prevents further soft tissue injury but there are limited in their ability of visualization for entire articular surface exposure.18 Minimally invasive percutaneous techniques have been reported and have the advantage of preserving soft tissues, but limited exposure may limit the extent of reduction.10,19 Articular reduction under fluoroscopic imaging without direct visualization may limit full appreciation of incongruity when it exists.20
CONCLUSION
The direct lateral approach to the distal tibia and fibula is a useful surgical approach that utilizes a single skin incision commonly used for immediate open reduction and internal fixation of distal fibula fractures. This approach respects the angiosomes of the skin overlying the anterior ankle region, and preserves the entire soft tissue envelope overlying the distal tibia, which allows for complete coverage of the internal fixation upon wound closure. The skin incision is advantageously remote from the hardware. The lateral column of the tibia and syndesmosis can be directly visualized and reduced. The superficial peroneal nerve can be minimally dissected and preserved within the subcutaneous plane. The incision can be extensile both proximally and distally, and may provide for earlier open treatment of some pilon fractures.
REFERENCES
- 1.Patterson M.J., J.D. Cole, Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13(2):85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Sirkin M., et al. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 1999;13(2):78–84. doi: 10.1097/00005131-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Blauth M., et al. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15(3):153–60. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Borrelli J., Jr, Catalano L. Open reduction and internal fixation of pilon fractures. J Orthop Trauma. 1999;13(8):573–82. doi: 10.1097/00005131-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Assal M., Ray A., Stern R. The extensile approach for the operative treatment of high-energy pilon fractures: surgical technique and soft-tissue healing. J Orthop Trauma. 2007;21(3):198–206. doi: 10.1097/BOT.0b013e3180316780. [DOI] [PubMed] [Google Scholar]
- 6.Mast J.W., Spiegel P.G., Pappas J.N. Fractures of the tibial pilon. Clin Orthop Relat Res. 1988;230:68–82. [PubMed] [Google Scholar]
- 7.McFerran M.A., et al. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992;6(2):195–200. doi: 10.1097/00005131-199206000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Shantharam S.S., Naeni F., Wilson E.P. Single-incision technique for internal fixation of distal tibia and fibula fractures. Orthopedics. 2000;23(5):429–31. doi: 10.3928/0147-7447-20000501-10. [DOI] [PubMed] [Google Scholar]
- 9.Collinge C, et al. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007;21(6):355–61. doi: 10.1097/BOT.0b013e3180ca83c7. [DOI] [PubMed] [Google Scholar]
- 10.Krackhardt T., et al. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125(2):87–94. doi: 10.1007/s00402-004-0778-y. [DOI] [PubMed] [Google Scholar]
- 11.Grose A., et al. Open reduction and internal fixation of tibial pilon fractures using a lateral approach. J Orthop Trauma. 2007;21(8):530–7. doi: 10.1097/BOT.0b013e318145a227. [DOI] [PubMed] [Google Scholar]
- 12.Manninen M.J., et al. Lateral approach for fixation of the fractures of the distal tibia. Outcome of 20 patients. Technical note. Arch Orthop Trauma Surg. 2007;127(5):349–53. doi: 10.1007/s00402-006-0278-3. [DOI] [PubMed] [Google Scholar]
- 13.Salmon M., Taylor G.I., M.N. Tempest, Arteries of the skin. 1st English ed. xxxii. London; New York: Churchill Livingstone; p. 174. [1] leaf of plates. [Google Scholar]
- 14.Ruedi T.P., Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res. 1979;138:105–10. [PubMed] [Google Scholar]
- 15.Wyrsch B, et al. Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am. 1996;78(11):1646–57. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Müller M.E. Manual of internal fixation: techniques recommended by the AO Group. 2d ed. xii. Berlin; New York: Springer-Verlag; 1979. p. 409. [Google Scholar]
- 17.Bhattacharyya T, et al. Complications associated with the posterolateral approach for pilon fractures. J Orthop Trauma. 2006;20(2):104–7. doi: 10.1097/01.bot.0000201084.48037.5d. [DOI] [PubMed] [Google Scholar]
- 18.Kao K.F., et al. Postero-medio-anterior approach of the ankle for the pilon fracture. Injury. 2000;31(2):71–4. doi: 10.1016/s0020-1383(99)00202-8. [DOI] [PubMed] [Google Scholar]
- 19.Wolinsky P., Lee M. The distal approach for anterolateral plate fixation of the tibia: an anatomic study. J Orthop Trauma. 2008;22(6):404–7. doi: 10.1097/BOT.0b013e31817614b2. [DOI] [PubMed] [Google Scholar]
- 20.Ebraheim N., Sabry F.F., Mehalik J.N. Intraoperative imaging of the tibial plafond fracture: a potential pitfall. Foot Ankle Int. 2000;21(1):67–72. doi: 10.1177/107110070002100112. [DOI] [PubMed] [Google Scholar]
- 21.Hazarika S., Chakravarthy J., Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia-results in 20 patients. Injury. 2006;37(9):877–87. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Attinger C., et al. The safest surgical incisions and amputations applying the angiosome principles and using the Doppler to assess the arterial-arterial connections of the foot and ankle. Foot Ankle Clin. 2001;6(4):745–99. doi: 10.1016/s1083-7515(02)00012-8. [DOI] [PubMed] [Google Scholar]
- 23.Deangelis J.P., Deangelis N.A., Anderson R. Anatomy of the superficial peroneal nerve in relation to fixation of tibia fractures with the less invasive stabilization system. J Orthop Trauma. 2004;18(8):536–9. doi: 10.1097/00005131-200409000-00009. [DOI] [PubMed] [Google Scholar]