Abstract
The present study examined changes in the perceived health of older Korean Americans (n = 141) over a 2-year period: 2003 (T1) and 2005 (T2). A hierarchical regression model of changes in perceived health was estimated with the following array of predictors: (1) background variables (age, gender, marital status, education, and length of stay in the United States), (2) initial perceived health (T1), (3) physical and mental health conditions at T1 (chronic conditions, functional disability, and depressive symptoms), and (4) changes in physical and mental health conditions (T2 – T1). When the effects of background variables and baseline perceived health were controlled, baseline chronic conditions and changes in both chronic conditions and depressive symptoms were found to predict changes in perceived health. Older individuals who initially had more chronic conditions and those who had experienced an increasing number of chronic conditions and depressive symptoms over 2 years viewed their health more negatively at follow-up. Findings highlight the importance of interventions for disease management and mental health promotion to enhance subjective health among older Korean immigrants.
Keywords: Health, Depression, Korean American Elders
Introduction
Over the past few decades, research findings have accumulated on the importance of self-perceived health as an indicator of general health and well-being [1–3]. Even when physical health conditions are controlled, perceived health has been found to predict a variety of outcomes, including quality of life, service utilization, morbidity, and mortality [1, 3–7]. Due to the greater likelihood of health deterioration, the significance of perceived health among older populations is pronounced [5, 8]. However, existing studies tend to be limited by the use of cross-sectional designs and lack of attention to racial/ethnic minorities.
In considering the predictors of perceived health, health-related factors are an obvious starting point. Indicators of physical health conditions such as chronic illness and functional disability form an underlying basis for evaluating one’s own health [4]. The relation of physical health conditions to perceived health however does not explain all the variance. Studies have found that persons with equivalent levels of physical conditions have different ratings of perceived health [9, 10]. The discordance between objective and subjective health measures implies that the process of health appraisals is complex and goes beyond a simple summing of medical conditions or level of disability [1, 4, 6]. Moreover, the literature suggests that perceived health has a role to play in the health equation that is independent of its roots in actual physical health [9, 10].
Recent studies on potential predictors of perceived health have focused their attention on the individuals’ mood or emotional state, particularly depressive symptoms [7, 11–13]. Individuals with greater levels of depressive symptoms are likely to rate their health as poorer, and this association is sustained even after controlling for the effects of objective health indicators [7, 8]. The independent relationship of depressive symptoms with perceived health suggests that subjective health outcomes might be optimized by interventions that target emotional states. In an initial foray into this line of investigation, indeed, Miller and colleagues [14] showed that treatment of depression led to the improved perceptions of health among depressed individuals even when there was no change in objective health conditions.
Longitudinal studies have expanded the horizon of research by exploring the trajectories of changes in perceived health over time. Earlier studies suggested an apparent stability of subjective health among community-dwelling older populations [15]; however, further studies suggested that the stability was an artifact of the multidirectionality of change [16, 17]. In the latter studies, analyses at the individual level revealed that, contrary to the stability suggested by minimal change at the overall group mean level, multiple patterns of changes in subjective health exist, including substantial improvement as well as decline [16, 17]. Factors that determine changes in perceived health have not been fully explored, including the role of race and ethnicity.
In order to confirm and extend the previous literature, the present study of perceived health and depressive symptoms drew upon a longitudinal sample of older Korean Americans. The study assessed both physical and mental health conditions and their changes as predictors to changes in perceived health. The ability to include changes in physical and emotional states in the predictive model is a virtue of longitudinal assessment and provided an opportunity to further explore mechanisms underlying physical and mental health. The significant effect of declining physical health on changes in perceived health is intuitive and has been reported in previous longitudinal studies [17]. However, few researchers have attended to the influence of changes in depressive symptoms [18]. Independent of physical health status and its changes, individuals who have recently experienced elevated depressive symptoms are hypothesized to show negative changes in perceived health.
The study sample is timely and relevant because older Korean Americans are undergoing an exponential population growth [19] but remain understudied and underserved [20]. The general physical and mental health profile of older Korean Americans positions them as a high risk group [21]. A previous cross-sectional assessment of elders living in Korea found that health indicators such as chronic conditions, functional disability, vision, and the number of sick days were associated with perceived health [22]; however, the issues surrounding changes in both potential predictors as well as in perceived health over time have not been addressed. Indeed, longitudinal data on Korean or Korean American elders are scarce [23]. The present assessment will therefore not only further understanding of mechanisms underlying physical and mental health, but also add to information about how the perceived health of Korean American elders changes over time.
Methods
Participants and Data Collection
The sample was drawn from two studies of Korean American elders. The initial study was conducted in 2003 with 230 older Korean Americans residing in two cities in Florida (Tampa and Orlando). In a subsequent study conducted in 2005, 472 older Korean Americans were surveyed in the same geographical areas. Although the two projects were not initially designed as a follow-up study, they had considerable overlaps in survey items and participants. One hundred and forty one individuals were common participants in both datasets, and their information was used in the present analysis. Hereafter, information from the 2003 survey and the 2005 survey will be referred as Time 1 (T1) and Time 2 (T2) data.
Sampling procedures for the two studies were similar. Participants were required to be Korean Americans aged 60 or older and have sufficient cognitive ability to understand and complete the survey. Given that minority elders are often difficult to recruit from any one source or using any one strategy [24], participants were recruited from multiple sources including local Korean churches, senior centers, elder associations and telephone directories for Korean residents. Data were collected through both face-to-face interviews and mail surveys. The structured questionnaires used in data collection were in Korean and developed using a back translation method. Respondents were paid $10 for their participation. Detailed information about the two projects is available elsewhere [25, 26].
Measures
Perceived Health
Three items from the Older Americans Resources and Services [27] questionnaire were used to assess perceived health. Items include “How would you rate your overall health at the present time?” “How is your present health compared to 5 years ago?” and “How much do your health troubles stand in the way of your doing the things you want to do?” Total scores ranged from 3 (positive health perceptions) to 10 (negative health perceptions). Internal consistencies for the measure were satisfactory for both time points (αT1 = 0.70, αT2 = 0.77).
Chronic Conditions
Individuals were asked to report existing medical conditions using a 9-item list of chronic diseases and conditions commonly found among older populations (e.g., arthritis, stroke, heart problems, diabetes, cancer), using a yes/no response format. A summated score was used for the analysis.
Functional Disability
Functional status was assessed with a composite measure based on four scales: the Physical Activities of Daily Living [27], the Instrumental Activities of Daily Living [27], the Physical Performance Scale [28], and the Functional Health Scale [29]. The twenty items cover a wide range of activities including eating, dressing, traveling, managing money, carrying a bag of groceries, and reaching out above head with arms. Participants were asked whether they could perform each activity. The responses were coded as 0 (without help), 1 (with some help) or 2 (unable to do). Responses for individual items were summed for total scores. The possible range for functional status was 0 (no disability) to 40 (severe disability). Internal consistencies for the measure were shown to be high at both time points (αT1 = 0.87, αT2 = 0.93).
Depressive Symptoms
A 10-item short form of the Center for Epidemiologic Studies-Depression Scale [30, 31] was utilized to index depressive symptoms. Rated on a 4-point scale, the items included how often symptoms such as loneliness, feelings of fearfulness, and restless sleep were experienced during the past week. The CES-D has been translated into the Korean language, and its psychometric properties have been validated in previous studies [25, 32]. A satisfactory level of internal consistency was obtained at both time points (αT1 = 0.76, αT2 = 0.74).
Other Variables
Background information included age (in years), gender (1 = male, 2 = female), marital status (1 = not married, 2 = married), education (1 = <high school education, 2 = ≥high school education), and length of stay in the United Sates (in years).
Analytic Strategies
Change scores were calculated for chronic conditions, functional disability, depressive symptoms, and perceived health by subtracting T1 scores from T2 scores. Higher change scores indicate increases in chronic conditions, functional disability, and depressive symptoms and worsening of health perceptions. Changes in perceived health served as an outcome criterion, and its predictive model was estimated by entering blocks of variables in the following order: (1) background variables (age, gender, marital status, education, and length of stay in the United States), (2) initial perceived health (T1), (3) physical and mental health conditions at T1 (chronic conditions, functional disability, and depressive symptoms), and (4) changes in physical and mental health conditions (T2 – T1). Prior to the regression analysis, intercorrelations among study variables and variance inflation factors (VIF) were assessed to check collinearity.
Results
Characteristics of the Sample
Among the 230 participants at T1, 141 were also included in the T2 survey: an inclusion rate of 61%. Descriptive analysis (t test and chi square) was conducted (results are not shown in tabular form) to examine whether there are any differences in baseline characteristics between the two groups who participated in both surveys (n = 141) and who were not included in the later survey (n = 89). Those who participated in both time points and included in the present analysis were found to be younger (t = 3.61, P <0.001), more likely to be married (χ2 = 4.98, P < 0.05), better educated (χ2 = 5.09, P < 0.05) and to have lived longer in the United States (t = −2.17, P < 0.05) than those who were not included in T2 survey. No gender difference was shown between the groups (χ2 = 3.12, P > 0.05). Given the selection biases, findings should be interpreted with caution.
Descriptive characteristics of the longitudinal sample (n = 141) are presented in Table 1. At T1, the sample ranged in age from 60 to 94 with an average age of 68.5 years (SD = 6.40). More than half (54.6%) was female, and three quarters (78%) were married. About 65% of the sample had received more than a high school education. The number of years lived in the US at T1 ranged from 2 months to 51 years with a mean year of 24.2 (SD = 10.4).
Table 1.
Sample characteristics at Time 1 and Time 2
| Time 1 |
Time 2 |
t | |||
|---|---|---|---|---|---|
| M/SD | % | M/SD | % | ||
| Age | 68.5/6.40 | ||||
| Female | 54.6 | ||||
| Married | 78.0 | ||||
| ≥High school | 64.7 | ||||
| Length of stay in US | 24.2/10.4 | ||||
| Chronic conditions | 1.30/1.09 | 1.41/1.15 | 1.50 | ||
| Functional disability | 1.16/2.77 | 2.05/4.71 | 2.56* | ||
| Depressive symptoms | 7.59/4.68 | 7.46/4.23 | −0.95 | ||
| Perceived health | 6.32/1.60 | 6.55/1.76 | 1.85 | ||
P < 0.05
Table 1 also presents descriptive information on major study variables at the two time points. A majority of the sample had at least one chronic condition (73.6% at T1 and 75.7% at T2), and about 33% at T1 and 41% at T2 reported that they had at least some difficulty in performing one or more of the activities on the list. At both time points, the most prevalent chronic condition was high blood pressure followed by arthritis. When applying the cut-off score for the short form of the CES-D [30], more than 30% of the sample (36% at T1 and 32% at T2) falls under the category of probable depression (scores equal to or higher than 10). As shown in Table 1, no differences in mean scores of chronic conditions, depressive symptoms, and perceived health were found between the two time points, but the score for functional disability was significantly higher at T2 compared to T1 (t = 2.56, P < 0.05).
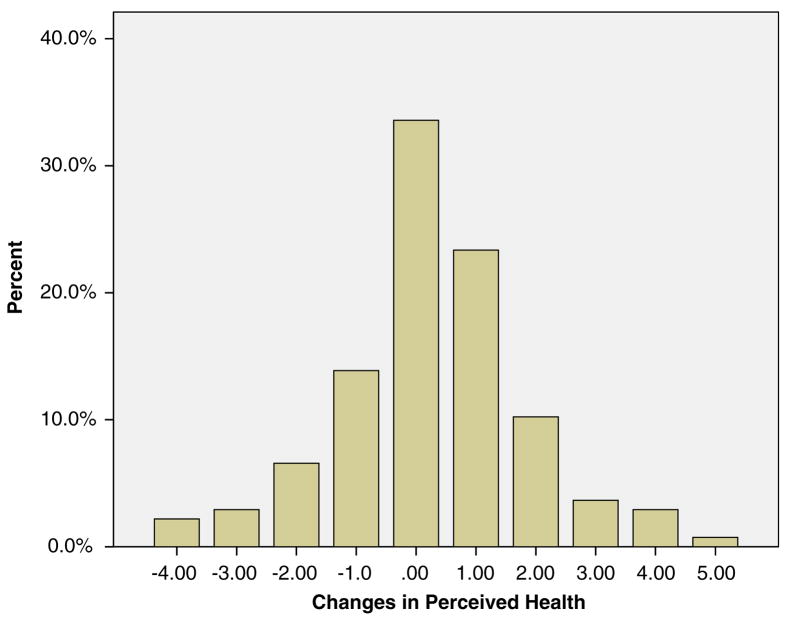
The outcome criterion, changes in perceived health, ranged from −4 to 5 with a mean of 0.25 (SD = 1.60). Figure 1 shows score distributions of changes in perceived health. About 41% of the sample showed positive scores (indicating a worsening of health perceptions), more than quarter (25.5%) showed negative scores (indicating an improvement in health perceptions), and approximately one third showed no change. The distribution is close to normal curve with a skewness of −0.006 (SD = 0.20).
Fig. 1.
Changes in perceived health from 2003 to 2005 (T2 − T1). Note: Change scores in perceived health were calculated by subtracting perceived health at T1 from perceived health at T2. Positive scores indicate worsening of perceived health, negative scores indicate improvement in perceived health, and zero implies no change
Determinants of Changes in Perceived Health
In preparing the regression models, one concern was whether or not collinearity might affect results. All zero-order correlations (results are not shown in tabular form), however, were below 0.54. Changes in perceived health was highly correlated with changes in chronic conditions (r = 0.30, P < 0.001), changes in functional disability (r = 0.23, P < 0.01), and changes in depressive symptoms (r = 0.38, P < 0.001). The absence of collinearity was also confirmed in the regression by the absence of VIF >2.10.
Table 2 summarizes the results of the estimated hierarchical regression model of changes in perceived health. The sequence of models was primarily based on chronology, with antecedent sets entered earlier and change scores later. In the initial model, background variables (age, gender, marital status, education, and length of stay in the United States) explained 6% of the variance, and none of the individual variables contributed significantly. At the second step, perceived health at T1 was added: it explained an additional 14% of the variance. The baseline perceived health was adjusted for all subsequent models. Inclusion of physical and mental health status at T1 increased the explanatory power of the model by 10%. Those who had more chronic conditions at T1 were likely to view their health more negatively by T2. In the final step, changes in physical and mental health accounted for an additional 22% of the variance, resulting in a total of 52% of the variance explained by the estimated model (F (12, 105) = 8.42, P < 0.001). Increases in chronic conditions and depressive symptoms were identified as significant risks to the subsequent decline in perceived health.
Table 2.
Regression model of changes in perceived health
| Step | Predictor | β | t | R2 | ΔR2 |
|---|---|---|---|---|---|
| 1 | Age | 0.08 | 0.77 | 0.06 | 0.06 |
| Female | −0.17 | − 1.57 | |||
| Married | 0.02 | 0.19 | |||
| ≥High school | 0.04 | 0.39 | |||
| Length of stay in US | −0.15 | − 1.43 | |||
| 2 | Perceived health (T1) | −0.40 | − 4.12*** | 0.20*** | 0.14*** |
| 3 | Chronic conditions (T1) | 0.23 | 2.29* | 0.30*** | 0.10** |
| Functional disability (T1) | 0.18 | 1.76 | |||
| Depressive symptoms (T1) | 0.16 | 1.50 | |||
| 4 | Changes in chronic conditions (T2 − T1) | 0.30 | 3.60** | 0.52*** | 0.22*** |
| Changes in functional disability (T2 − T1) | 0.12 | 1.26 | |||
| Changes in depressive symptoms (T2 − T1) | 0.33 | 3.40** |
P < 0.05,
P < 0.01,
P < 0.001
Discussion
The present study examined a predictive model of changes in perceived health using a longitudinal sample of older Korean Americans (n = 141) over a 2-year period (2003–2005). The estimated hierarchical regression model explained a substantial amount of variance and identified significant determinants of changes in perceived health.
Contrary to earlier research on stability of subjective health among older populations [15], our analysis found that only 34% of the sample showed stability in their perceived health. It is notable that more than a quarter of this sample of older Korean Americans showed improvement in their health perceptions. Our findings are consistent with those of recent studies suggesting multidirectionality of changes in perceived health [16, 17]. The findings suggest that simply focusing on changes in overall group means may overlook the individual levels of variations.
After adjusting for background variables and baseline perceived health, the number of chronic conditions at T1 was found to be a significant predictor of changes in perceived health. As might be expected, those who initially had more chronic conditions were more likely to report worsening of health perceptions. In cross-sectional studies, the critical role of chronic conditions in subjective health has been well-documented [11–13]. Our findings add to the literature by showing that the existence of chronic diseases not only predicts concurrent health perception but also its subsequent deterioration.
Another set of variables identified as significant determinants of changes in perceived health dealt with changes in chronic conditions and depressive symptoms. Older individuals who reported an increase in the number of chronic conditions were more likely to perceive their health as worse. The experience of being diagnosed with a new disease is a stressful life event that negatively influences perceptions of health. This finding, along with the nature of chronic conditions as a persistent life strain, calls attention to the management of chronic diseases. Unlike acute diseases which are most likely curable, the chronic conditions of later life often persist for the remainder of life. The facts that chronic diseases generally cannot be cured and affect one’s overall sense of health suggest the need for interventions designed to enhance a positive adaptation in the course of disease. In this regard, a line of research has postulated that optimistic views and attitudes toward one’s health play beneficial roles in health-related quality of life [33, 34].
One of the important findings from the present study is the significant role of changes in depressive symptoms. Independent of physical health status and its changes, elevated depressive symptoms played a substantial role in predicting subsequent decline in perceived health. These findings suggest the importance of positive mental health in efforts to promote subjective health. Our findings should be considered in the context of previous studies suggesting a particular connection between physical and mental health among Asians American groups such as Korean Americans [35]. In contrast to the Western mind-body dichotomy, Asians tend to view mind and body as integrated; with the result that somatization is a more frequent method of experiencing and expressing emotional distress [35]. Given these unique cultural characteristics, the linkage between depressive symptomatology and perception of physical health may be greater than that found in non-Asian populations. Accordingly, the benefits of prevention, early detection, and proper treatment of depression may not be limited to mental well-being but also include favorable health outcomes.
Some limitations to the present should be noted. Due to the non-random nature of sample recruitment over the two points of data collection, caution should be exercised in interpreting research findings. Also, the 2-year interval may not be sufficient to address dynamic changes in physical and mental health. Findings from the present study are therefore only suggestive and invite further investigation.
Despite the above mentioned limitations, the present study provided implications for research and practice. Our findings demonstrate that perceived health is a complex construct that encompasses physical and emotional components, and that even in later years individuals may improve in their self-perceived health. These findings suggest avenues to enhance positive perceptions of health such as teaching management skills for chronic conditions and promoting mental health. Intervention efforts to maintain or enhance positive perceptions will help older individuals make a healthy adjustment to various challenges in later years regardless of objective life circumstances.
Acknowledgments
The project was partially supported by the National Institute on Aging Research Grant Program (1R03 AG 26332-01).
References
- 1.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 2.Liang J. Self-reported physical health among aged adults. J Gerontol. 1986;41:248–60. doi: 10.1093/geronj/41.2.248. [DOI] [PubMed] [Google Scholar]
- 3.Wolinsky FD, Johnson RJ. Perceived health status and mortality among older men and women. J Gerontol: Social Sci. 1992;47:S304–12. doi: 10.1093/geronj/47.6.s304. [DOI] [PubMed] [Google Scholar]
- 4.Borawski EA, Kinney JM, Kahana E. The meaning of older adults’ health appraisals: congruence with health status, determinant of mortality. J Gerontol: Social Sci. 1996;51B:S157–70. doi: 10.1093/geronb/51b.3.s157. [DOI] [PubMed] [Google Scholar]
- 5.Hays J, Schoenfeld D, Blazer D. Determinants of poor self-rated health in later life. Am J Geriatr Psychiatry. 1996;4:188–96. doi: 10.1097/00019442-199622430-00002. [DOI] [PubMed] [Google Scholar]
- 6.Maier H, Smith J. Psychological predictors of mortality in old age. J Gerontol: Psychol Sci. 1999;54B:P44–54. doi: 10.1093/geronb/54b.1.p44. [DOI] [PubMed] [Google Scholar]
- 7.Ormel J, Kempen G, Deeg D, Brilman E, van Sonderen E, Relyveld J. Functioning, well-being, and health perception in late middle-aged and older people: comparing the effects of depressive symptoms and chronic medical conditions. J Am Geriatr Soc. 1998;46:39–48. doi: 10.1111/j.1532-5415.1998.tb01011.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodin J, McAvay G. Determinants of change in perceived health in a longitudinal study of older adults. J Gerontol: Psychol Sci. 1992;47:P373–84. doi: 10.1093/geronj/47.6.p373. [DOI] [PubMed] [Google Scholar]
- 9.Kahana E, Resmond C, Hill GJ, Kercher K, Kahana B, Johnson JR, Young R. The effects of stress, vulnerability, and appraisal on the psychological well-being of the elderly. Res Aging. 1995;17:459–89. [Google Scholar]
- 10.Schulz R, Williamson GM. Psychosocial and behavioral dimensions of physical frailty. J Gerontol. 1993;48:39–43. doi: 10.1093/geronj/48.special_issue.39. [DOI] [PubMed] [Google Scholar]
- 11.Bryant L, Beck A, Fairclough D. Factors that contribute to positive perceived health in an older populations. J Aging Health. 2000;12:169–92. doi: 10.1177/089826430001200202. [DOI] [PubMed] [Google Scholar]
- 12.Cott C, Gignac M, Badley E. Determinants of self-rated health for Canadians with chronic disease and disability. J Epidemiol Community Health. 1999;53:731–6. doi: 10.1136/jech.53.11.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinquart M. Correlates of subjective health in older adults: a meta-analysis. Psychol Aging. 2001;16:414–26. doi: 10.1037//0882-7974.16.3.414. [DOI] [PubMed] [Google Scholar]
- 14.Miller M, Schulz R, Paradis C, Houck P, Mazumdar S, Frank E, et al. Changes in perceived health status of depressed elderly patients treated until remission. Am J Psychiatry. 1996;153:1350–2. doi: 10.1176/ajp.153.10.1350. [DOI] [PubMed] [Google Scholar]
- 15.Maddox G, Douglass E. Self-assessment of health: a longitudinal study of elderly subjects. J Health Soc Behav. 1973;14:87–93. [PubMed] [Google Scholar]
- 16.Han B. Depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. J Am Geriatr Soc. 2002;50:1549–56. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- 17.Kim H, Wolde-Tsadik G, Reuben D. Predictors of perceived health in hospitalized older persons: a cross-sectional and longitudinal study. J Am Geriatr Soc. 1997;45:420–6. doi: 10.1111/j.1532-5415.1997.tb05165.x. [DOI] [PubMed] [Google Scholar]
- 18.Datto C, Thompson R, Knott K, Katz I. Older adult report of change in depressive symptoms as a treatment decision tool. J Am Geriatr Soc. 2006;54:627–31. doi: 10.1111/j.1532-5415.2006.00660.x. [DOI] [PubMed] [Google Scholar]
- 19.U. S. Bureau of the Census. Population Census. Washington D.C: United States Department of Commerce; 2000. [Google Scholar]
- 20.Andersen R, Harada N, Chiu V, Makinodan T. Application of the behavioral model to health studies of Asian and Pacific Islander Americans. Asian Am Pac Isl J Health. 1995;3:128–41. [PubMed] [Google Scholar]
- 21.Hurh W, Kim K. Correlates of Korean immigrant’s mental health. J Nerv Ment Dis. 1990;178:703–11. doi: 10.1097/00005053-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Jang Y, Poon LW, Kim S, Shin B. Self-perception of aging and health among older adults in Korea. J Aging Stud. 2004;18:485–96. [Google Scholar]
- 23.Min J, Moon A, Lubben J. Determinants of psychological distress over time among older Korean immigrants and non-Hispanic White elders: evidence from a two-wave panel study. Aging Ment Health. 2005;9:210–22. doi: 10.1080/13607860500090011. [DOI] [PubMed] [Google Scholar]
- 24.Curry L, Jackson J. The science of inclusion: recruiting, retaining racial and ethnic elders in health research. Washington D.C: The Gerontological Society of American; 2003. [Google Scholar]
- 25.Jang Y, Kim G, Chiriboga D. Acculturation and manifestation of depressive symptoms among Korean American older adults. Aging Ment Health. 2005;9:500–7. doi: 10.1080/13607860500193021. [DOI] [PubMed] [Google Scholar]
- 26.Jang Y, Kim G, Hansen L, Chiriboga D. Attitudes of older Korean Americans toward mental health services. J Am Geriatr Soc. 2007;55:616–20. doi: 10.1111/j.1532-5415.2007.01125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fillenbaum G. Multidimensional functional assessment: The Duke older Americans resources, services procedure. Hillsdale NJ: Erlbaum; 1988. [Google Scholar]
- 28.Nagi S. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q. 1976;54:439–67. [PubMed] [Google Scholar]
- 29.Rosow I, Breslau N. A Guttman Health Scale for the aged. J Gerontol. 1966;21:556–9. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 30.Andresen E, Malmgren J, Carter W, Patrick D. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 31.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 32.Cho M, Nam J, Suh G. Prevalence of symptoms of depression in a nationwide sample of Korean adults. Psychiatry Res. 1998;81:341–52. doi: 10.1016/s0165-1781(98)00122-x. [DOI] [PubMed] [Google Scholar]
- 33.Fredman L, Hawkes W, Black S, Bertrand R, Magaziner J. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc. 2006;54:1074–81. doi: 10.1111/j.1532-5415.2006.00786.x. [DOI] [PubMed] [Google Scholar]
- 34.Salovey P, Rothman A, Detweiler J, Steward W. Emotional states and physical health. Am Psychol. 2000;55:110–21. doi: 10.1037//0003-066x.55.1.110. [DOI] [PubMed] [Google Scholar]
- 35.Lin KM, Cheung F. Mental health issues for Asian Americans. Psychiatr Serv. 1999;50:774–80. doi: 10.1176/ps.50.6.774. [DOI] [PubMed] [Google Scholar]