Abstract
Vitamin D deficiency associates with increased risk for cardiovascular events and mortality, but the mechanism driving this association is unknown. Here, we tested whether circulating 25-hydroxyvitamin D concentration associates with coronary artery calcification (CAC), a measure of coronary atherosclerosis, in the Multi-Ethnic Study of Atherosclerosis. We included 1370 participants: 394 with and 976 without chronic kidney disease (estimated GFR <60 ml/min per 1.73 m2). At baseline, CAC was prevalent among 723 (53%) participants. Among participants free of CAC at baseline, 135 (21%) developed incident CAC during 3 yr of follow-up. Lower 25-hydroxyvitamin D concentration did not associate with prevalent CAC but did associate with increased risk for developing incident CAC, adjusting for age, gender, race/ethnicity, site, season, physical activity, smoking, body mass index, and kidney function. Further adjustment for BP, diabetes, C-reactive protein, and lipids did not alter this finding. The association of 25-hydroxyvitamin D with incident CAC seemed to be stronger among participants with lower estimated GFR. Circulating 1,25-dihydroxyvitamin D concentrations among participants with chronic kidney disease did not significantly associate with prevalent or incident CAC in adjusted models. In conclusion, lower 25-hydroxyvitamin D concentrations associate with increased risk for incident CAC. Accelerated development of atherosclerosis may underlie, in part, the increased cardiovascular risk associated with vitamin D deficiency.
Vitamin D deficiency is associated with increased risks for cardiovascular disease (CVD) and death.1 Specifically, low circulating concentrations of 25-hydroxyvitamin D [25(OH)D] are associated with increased risks for mortality among incident hemodialysis patients and patients with stages 2 through 5 chronic kidney disease (CKD),2,3 cardiovascular events in the Framingham Offspring Study,4 myocardial infarction in the Health Professionals Follow-up Study,5 cardiovascular- and all-cause mortality among patients with acute coronary syndrome,6 and all-cause mortality in follow-up from the Third National Health and Nutrition Examination Survey (NHANES III).7 Observational studies among patients with CKD suggested that treatment with 1,25-dihydroxyvitamin D (calcitriol) reduces mortality.8–12 A meta-analysis of clinical trials, conducted predominantly among postmenopausal women, demonstrated a statistically significant 7% reduction in total mortality with cholecalciferol or ergocalciferol supplementation.13
Accelerated atherosclerosis may explain in part the associations of vitamin D deficiency with CVD and death. Low circulating 25(OH)D concentration is associated with a number of established risk factors for atherosclerosis, including obesity, diabetes, hypertension, and dyslipidemia.14–18 Moreover, vitamin D seems to regulate additional biologic pathways implicated in the development of atherosclerosis. Calcitriol downregulates the renin-angiotensin-aldosterone system in animal models and modulates immune cell function, enriching the antiatherogenic Th2 lymphocyte population and reducing proinflammatory cytokine secretion.19,20 The presence in vascular smooth muscle cells of 1-α hydroxylase, which converts 25(OH)D to calcitriol, suggests that vitamin D may also have direct effects on the vascular wall, potentially including prevention of vascular calcification.21,22
We tested whether low circulating levels of 25(OH)D are associated with prevalent and incident coronary artery calcium (CAC) in the Multi-Ethnic Study of Atherosclerosis (MESA), a community-based cardiovascular cohort study. 25(OH)D concentration reflects total intake of vitamin D from cutaneous synthesis and dietary intake.23 CAC is a sensitive measure of subclinical coronary atherosclerosis and a strong risk factor for cardiovascular events.24 Serum concentrations of calcitriol (1,25-dihydroxyvitamin D), the most biologically potent metabolite of vitamin D, were additionally measured among participants with CKD.
Results
Baseline Characteristics
Mean (SD) 25(OH)D concentration was 21.4 (11.3) ng/ml. Lower 25(OH)D concentration was associated with younger age, male gender, nonwhite race/ethnicity, measurement during winter months, higher body mass index (BMI), current smoking, diabetes, hypertension, lower HDL cholesterol concentration, and higher triglyceride concentration (Table 1). Mean (SD) estimated GFR (eGFR) was 51.4 (8.2) ml/min per 1.73m2 for participants with CKD (eGFR <60 ml/min per 1.73 m2) and 81.4 (14.4) ml/min per 1.73m2 for participants without CKD. Compared with participants in the full MESA population, those included in this study were slightly older (64.0 versus 61.7 yr), more likely to have hypertension (54.7 versus 47.4%), and less likely to smoke (10.0 versus 13.8%); other characteristics were similar.
Table 1.
Characteristics of 1370 MESA participants at baseline, by circulating 25(OH)D concentration
| Characteristic | 25(OH)D |
|
|---|---|---|
| ≥15 ng/ml(n = 1004) | <15 ng/ml(n = 366) | |
| Age (yr; mean ± SD) | 64.6 ± 9.9 | 62.1 ± 10.3 |
| Male gender (n [%]) | 454 (45.2) | 178 (48.6) |
| Race/ethnicity | ||
| white | 484 (48.2) | 77 (21.0) |
| Chinese | 144 (14.3) | 37 (10.1) |
| black | 192 (19.1) | 172 (47.0) |
| Hispanic | 184 (18.3) | 80 (21.9) |
| Site (n [%]) | ||
| Wake Forest University, Winston-Salem, NC | 146 (14.5) | 58 (15.8) |
| Columbia University, New York, NY | 139 (13.8) | 69 (18.9) |
| Johns Hopkins University, Baltimore, MD | 129 (12.8) | 66 (18.0) |
| University of Minnesota, Twin Cities, MN | 176 (17.5) | 49 (13.4) |
| Northwestern University, Chicago, IL | 200 (19.9) | 76 (20.8) |
| University of California, Los Angeles, Los Angeles, CA | 214 (21.3) | 48 (13.1) |
| Season of measurement (n [%]) | ||
| January through March | 246 (24.5) | 137 (37.4) |
| April through June | 316 (31.5) | 110 (30.1) |
| July through September | 200 (19.9) | 40 (10.9) |
| October through December | 242 (24.1) | 79 (21.6) |
| Diabetes (n [%]) | 121 (12.1) | 63 (17.3) |
| BP (n [%]) | ||
| normal | 284 (28.3) | 93 (25.4) |
| prehypertension | 187 (18.6) | 57 (15.6) |
| hypertension | 533 (53.1) | 216 (59.0) |
| Smoking (n [%]) | ||
| never | 526 (52.5) | 181 (49.7) |
| former | 392 (39.1) | 130 (35.7) |
| current | 84 (8.4) | 53 (14.6) |
| CKD | 305 (30.4) | 89 (24.4) |
| eGFR (ml/min per 1.73 m2; mean ± SD) | 72.0 ± 17.7 | 75.3 ± 20.9 |
| BMI (kg/m2; mean ± SD) | 27.6 ± 4.9 | 30.4 ± 6.0 |
| Physical activity (MET min/wk; mean ± SD) | 1710 ± 2430 | 1160 ± 1680 |
| CRP (mg/L; geometric mean ± geometric SD) | 1.84 ± 3.11 | 2.17 ± 3.09 |
| Total cholesterol (mg/dl; mean ± SD) | 195 ± 35 | 191 ± 36 |
| HDL cholesterol (mg/dl; mean ± SD) | 52.1 ± 15.1 | 49.1 ± 14.5 |
| Triglycerides (mg/dl; mean ± SD) | 131 ± 97 | 136 ± 83 |
| LDL cholesterol (mg/dl; mean ± SD) | 117 ± 30 | 115 ± 33 |
25(OH)D Concentration and Prevalent CAC
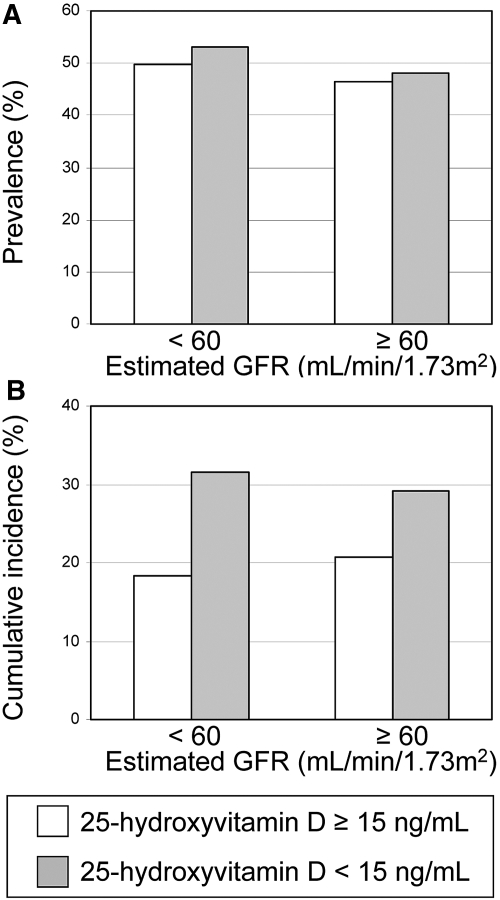
CAC was prevalent at baseline among 723 (53%) participants (65% of participants with CKD and 48% of participants with normal kidney function). 25(OH)D concentration was not associated with prevalent CAC (Table 2 and Figure 1A).
Table 2.
Associations of circulating 25(OH)D concentration with prevalent and incident CAC in the MESAa
| Parameter | 25(OH)D |
P for linear trend | ||
|---|---|---|---|---|
| ≥15 ng/ml | <15 ng/ml | Per 10-ng/ml Lower Concentration | ||
| Prevalent CAC | ||||
| No. At risk (No. of events) | 1,004 (545) | 366 (178) | 1370 (723) | |
| model 1 (RR [95% CI])b | 1.00 (reference) | 1.02 (0.91 to 1.15) | 1.00 (0.97 to 1.04) | 0.92 |
| model 2 (RR [95% CI])c | 1.00 (reference) | 0.98 (0.87 to 1.11) | 0.98 (0.95 to 1.02) | 0.33 |
| model 3 (RR [95% CI])d | 1.00 (reference) | 0.99 (0.88 to 1.11) | 0.98 (0.95 to 1.01) | 0.28 |
| Incident CAC | ||||
| No. At risk (No. of events) | 459 (86) | 188 (49) | 647 (135) | |
| model 1 (RR [95% CI])b | 1.00 (reference) | 1.58 (1.14 to 2.21) | 1.35 (1.11 to 1.64) | 0.002 |
| model 2 (RR [95% CI])c | 1.00 (reference) | 1.40 (0.99 to 1.99) | 1.23 (1.00 to 1.52) | 0.046 |
| model 3 (RR [95% CI])d | 1.00 (reference) | 1.38 (0.95 to 1.99) | 1.23 (1.00 to 1.52) | 0.049 |
aRR, relative risk.
bAdjusted for age, gender, race/ethnicity, site, season, and measurement batch.
cAdditionally adjusted for physical activity, BMI, and smoking.
dAdditionally adjusted for diabetes, BP, CRP, total cholesterol, HDL cholesterol, and triglycerides.
Figure 1.
(A and B) Prevalence (A) and 3-yr cumulative incidence (B) of CAC, by eGFR and 25(OH)D concentration, adjusted for age, gender, and race/ethnicity.
25(OH)D Concentration and Incident CAC
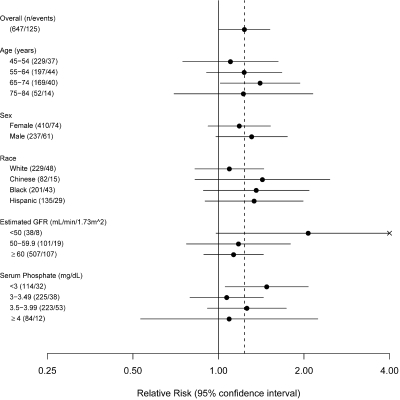
Of 647 participants without CAC at baseline, 135 (21%) developed incident CAC during a median follow-up duration of 3 yr. Lower 25(OH)D concentration was associated with increased risk for incident CAC (Table 2 and Figure 1B). Specifically, each 10-ng/ml lower 25(OH)D concentration was associated with a 23% increased risk for developing CAC, after full adjustment (P = 0.049). This association did not vary by age, gender, race/ethnicity, or serum phosphate concentration but seemed to be stronger among participants with lower eGFR (Figures 1 and 2). The formal statistical test for interaction by eGFR was NS (P = 0.31). Attenuation comparing model 2 with model 1 was largely attributable to adjustment for BMI.
Figure 2.
Subgroup associations of circulating 25(OH)D concentration with incident CAC. Circles represent point estimates; horizontal bars represent 95% CIs. Risk is assessed per 10-ng/ml lower 25(OH)D concentration, adjusted for age, gender, race/ethnicity, site, season, measurement batch, physical activity, BMI, smoking, diabetes, BP, CRP, total cholesterol, HDL cholesterol, and triglycerides. Shown in parentheses are numbers of participants at risk/numbers of participants with incident CAC.
Among the 723 participants with prevalent CAC, 25(OH)D concentration was not associated with severity of CAC: Each 10-ng/ml lower 25(OH)D concentration was associated with a 3.0-U lower Agatston score (untransformed analysis, 95% confidence interval [CI] 48.6 to 42.7; P = 0.90) or a 4% lower geometric mean Agatston score (log-transformed analysis, 95% CI 13 to 7%; P = 0.50), adjusted for precision variables and potential confounders. Similarly, 25(OH)D concentration was not associated with progression of CAC: Each 10-ng/ml lower 25(OH)D concentration was associated with only a 0.2% greater decrease in geometric mean Agatston score during follow-up (95% CI −4 to 4%; P = 0.93).
Calcitriol Concentration and CAC
Calcitriol measurements were additionally available for 350 participants with eGFR <60 ml/min per 1.73 m2. Of these, 226 (65%) had prevalent CAC at baseline, and 26 (21%) of 124 without prevalent CAC developed incident CAC during follow-up. Lower calcitriol concentrations were associated with trends toward increased risks for prevalent and incident CAC (Table 3). Among the 226 participants with baseline CAC, calcitriol concentration was not correlated with CAC severity or progression. 25(OH)D and calcitriol concentrations were weakly correlated (Spearman ρ = 0.21). When both measurements were included in a model together, relative risks for incident CAC in this subgroup were 1.29 (95% CI 0.85 to 1.95) per 10-ng/ml lower 25(OH)D and 1.17 (95% CI 0.86 to 1.58) per 10-pg/ml lower calcitriol, adjusting for age, gender, race/ethnicity, site, season, measurement batch, physical activity, BMI, and smoking.
Table 3.
Associations of circulating calcitriol (1,25-dihydroxyvitamin D) concentration with prevalent and incident CAC in the MESAa
| Parameter | RR (95% CI) | P |
|---|---|---|
| Prevalent CAC | ||
| model 1b | 1.09 (1.02 to 1.16) | 0.01 |
| model 2c | 1.08 (1.01 to 1.15) | 0.018 |
| model 3d | 1.06 (1.00 to 1.13) | 0.065 |
| model 4e | 1.06 (1.00 to 1.13) | 0.064 |
| Incident CAC | ||
| model 1b | 1.18 (0.84 to 1.67) | 0.35 |
| model 2c | 1.19 (0.88 to 1.60) | 0.26 |
| model 3d | 1.22 (0.91 to 1.65) | 0.10 |
| model 4e | 1.32 (0.95 to 1.85) | 0.11 |
aRR is assessed per 10-pg/ml lower calcitriol concentration.
bAdjusted for age, gender, race/ethnicity, site, season, and measurement batch.
cAdditionally adjusted for physical activity, BMI, and smoking.
dAdditionally adjusted for diabetes, BP, CRP, total cholesterol, HDL cholesterol, and triglycerides.
eAdditionally adjusted for eGFR and serum phosphorous concentration.
Discussion
Lower 25(OH)D concentrations were associated with increased risk for developing new-onset CAC during 3 yr of follow-up in a large, community-based, multiethnic population without preexisting clinical CVD. These results suggest that accelerated development of coronary atherosclerosis may underlie, in part, the increased cardiovascular risk associated with vitamin D deficiency.
This is the first report to our knowledge to assess the relationship of 25(OH)D concentration with CAC or with change in any measure of subclinical CVD over time. 25(OH)D levels have been correlated with other measures of subclinical atherosclerosis in cross-sectional studies. In NHANES 2001 through 2004, lower 25(OH)D concentrations were associated with increased prevalence of peripheral artery disease, defined as an ankle-brachial index <0.9, in a dose-dependent manner.25 Among 390 patients with type 2 diabetes, 25(OH)D concentrations were inversely correlated with carotid intima-media thickness.26 In animal models, calcitriol at dosages sufficient to correct secondary hyperparathyroidism prevented vascular calcification, whereas very high dosages of calcitriol caused vascular calcification.27 Given results of animal models and widespread clinical use of vitamin D supplements, it is important to note that we did not observe any association of higher 25(OH)D concentrations with CAC.
The association of lower 25(OH)D concentrations with incident CAC was independent of established risk factors for atherosclerosis, including smoking, diabetes, BP, dyslipidemia, BMI, and C-reactive protein (CRP). This suggests that vitamin D deficiency may be related to CVD through unique biologic pathways. Direct effects on the renin-angiotensin-aldosterone system, immune cell function, and vascular smooth muscle cells are possible candidates.19–22 It is also possible that this relationship is mediated by bone. Both osteoporosis and low-turnover bone disease have been associated with vascular calcification, and vitamin D may affect deposition of vascular calcium by altering the flux of calcium and phosphorus into and out of bone or by modifying levels of hormones and other signaling molecules released by bone.28,29
In our study, the association of incident CAC with lower 25(OH)D concentrations seemed to be greater in magnitude among participants with impaired kidney function. This interaction was not statistically significant and must be viewed as hypothesis generating; however, it is biologically plausible, because patients with CKD may not be able to compensate for insufficient 25(OH)D by increasing the rate of its conversion to calcitriol in the kidney. Calcitriol concentrations across the range of GFR may help in the evaluation of this possibility but were not available for analysis. It is also possible that CAC includes medial calcification among patients with CKD,30 with low vitamin D concentrations associated more strongly with medial calcification than with intimal calcification. That risk associated with lower 25(OH)D concentrations does not increase until GFR is <50 ml/min per 1.73 m2 may reflect misclassification of eGFR in the 50- to 60-ml/min per 1.73 m2 range or may reflect a threshold effect of declining calcitriol production. If replicated in future studies, then the potential GFR–25(OH)D interaction would suggest that people with impaired kidney function may be more susceptible to detrimental effects of insufficient 25(OH)D and that renally produced calcitriol may be important in prevention of CAC.
25(OH)D concentration was not associated with the prevalence of CAC at baseline or with severity or progression of prevalent CAC. There are at least three possible explanations for differing results comparing incident and prevalent CAC. First, baseline 25(OH)D concentration may reflect current vitamin D status and risk for imminent CAC formation more accurately than vitamin D status and risk for CAC formation years earlier, when CAC present at baseline was forming.31 Second, inclusion only of participants who underwent repeat measurements (“survivors”) may have biased analyses of prevalent CAC. Third, results for incident CAC could be due to residual confounding or chance. Differing results for incident CAC versus CAC severity and progression suggest several possible explanations: Vitamin D may be related to the initiation of CAC but not to its progression, difficulties quantifying extent of CAC and its change over time may have biased results toward the null, or results for incident CAC may be due to chance. Further studies are warranted to distinguish these possibilities.
Among participants with impaired kidney function, lower calcitriol concentrations were associated with increased risks for prevalent and incident CAC, but these associations did not meet the α = 0.05 level of statistical significance. Compared with 25(OH)D concentration, circulating calcitriol concentration is a less robust biomarker. Calcitriol concentration is tightly regulated by renal 1-α hydroxylase activity, so associations with circulating calcitriol concentration may be confounded by factors that affecting the activity of this enzyme, including kidney function, diabetes, serum phosphate, fibroblast growth factor 23, parathyroid hormone, and acid-base status.22 We account for some but not all of these factors. In addition, calcitriol has a relatively short half-life, so a single measurement may poorly reflect long-term exposure. Watson et al.32 reported an inverse correlation of calcitriol concentration with severity of CAC among 173 patients with elevated cardiovascular risk. Associations with CAC severity, in contrast with CAC prevalence and incidence as observed in our study, may reflect differences in study population and/or method of CAC measurement.
Strengths of this study include its diverse, community-based population with four racial/ethnic groups; longitudinal measurements of CAC; a reduced likelihood of confounding by chronic disease given the absence of clinical CVD at baseline and well-measured covariates; and the relatively large size. This study also has limitations. 25(OH)D has a relatively long circulating half-life (approximately 3 wk) and is considered a good biomarker, but a single measurement cannot fully capture cumulative vitamin D exposure.23,31 A temporal relationship between low 25(OH)D concentration and the development of CAC was observed, but this does not necessarily demonstrate causality. Calcitriol concentrations were available for only a subset of the population, and associations with calcitriol may be particularly subject to residual confounding. Power was insufficient to examine whether threshold concentrations of vitamin D were associated with risk for disease or to evaluate covariate interactions with statistical confidence. It cannot be determined whether lower vitamin D concentrations are associated with the development of atherosclerotic plaque per se or with its calcification.
In conclusion, lower 25(OH)D concentrations were associated with increased risk for developing new-onset CAC during 3 yr of follow-up in a diverse, community-based population. Subclinical coronary atherosclerosis may contribute to the increased risks for cardiovascular events and mortality associated with low vitamin D concentrations. Further studies are needed to confirm these results and to determine whether vitamin D interventions prevent the development of CVD.
Concise Methods
Study Population
The MESA is a prospective cohort study designed to investigate the prevalence, correlates, and progression of subclinical CVD. As described in detail elsewhere, 6814 community-dwelling residents aged 45 to 84 were recruited between 2000 and 2002 at six centers across the United States.33 Individuals with previous clinical CVD, defined as physician-diagnosed heart attack, angina, stroke, transient ischemic attack, heart failure, or atrial fibrillation; use of nitroglycerin; or previous angioplasty, coronary artery bypass graft, valve replacement, pacemaker or defibrillator implantation, or any surgery on the heart or arteries, were excluded. Detailed data describing demographics, comorbidities, and medications were collected at enrollment, and each participant gave baseline blood samples. Study protocols were approved by the institutional review board at each participating institution, and all MESA participants granted informed consent.
This study includes all MESA participants with 25(OH)D concentration measured at baseline and CAC measured at baseline and follow-up (n = 1370). Baseline 25(OH)D concentration was measured in two subsets of MESA participants, which were combined for this study. The first subset includes 455 MESA participants with baseline CKD, defined by an eGFR < 60 ml/min per 1.73 m234; 388 of these underwent repeat CAC measurement and were included in analyses. For the purpose of the study described herein, we measured 25(OH)D concentration for an additional 1000 MESA participants with normal baseline kidney function. These were randomly sampled from the pool of participants who underwent repeat CAC measurement after 3 yr of follow-up.
25(OH)D and Calcitriol
Serum was collected at the baseline MESA examination and frozen at −70°C. 25(OH)D was measured in thawed samples using a RIA (DiaSorin, Stillwater, MN; coefficient of variation over multiple runs 8.2 to 11.0%). Measurements were completed using the same assay in three batches by eGFR. Compared with the single batch completed for participants with normal kidney function, mean 25(OH)D concentrations in the two batches completed for participants with CKD were 2 ng/ml higher and 0.1 ng/ml lower, adjusting for age, gender, race/ethnicity, site, and season of measurement. Calcitriol was measured among participants with CKD only using a RIA (DiaSorin; coefficient of variation over multiple runs 12.3 to 15.3%).
Coronary Artery Calcium
CAC was quantified using an electron-beam computed tomography (CT) scanner or a multidetector CT system, as described previously in detail.35 At each CAC measurement, each MESA participant underwent two scans. A radiologist or a cardiologist blinded to clinical data read all CT scans at a single center, using an interactive scoring system to calculate Agatston score.36 The mean Agatston score for each pair of concurrent scans was used for all analyses, with any Agatston score >0 defining the presence of CAC. κ values for intraobserver and interobserver agreement were 0.93 and 0.90, respectively.24
Covariates
Race/ethnicity was self-classified by participants as Caucasian, Chinese, African-American, or Hispanic. Diabetes was defined as a fasting blood glucose ≥126 mg/dl or use of diabetes medications (insulin, sulfonylureas, biguanides, thiazolidinediones, or α-glucosidase inhibitors).37 BP was categorized as hypertension (systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, or use of antihypertensive agents), prehypertension (systolic BP ≥120 mmHg or diastolic BP ≥80 mmHg in the absence of hypertension), or normal, according to current guidelines.38 CKD was defined by an eGFR < 60 ml/min per 1.73 m2, calculated using the Modification of Diet in Renal Disease (MDRD) formula after indirectly calibrating serum creatinine to Cleveland Clinic values.39 Lipid concentrations were measured using standard enzymatic methods, with LDL cholesterol calculated using the Friedewald formula.40 Total intentional physical activity was quantified from questions assessing sporting, conditioning, and walking activities.41,42 Time spent on each activity was multiplied by its standard metabolic equivalent of the task (MET) before summing, with physical activity reported in MET minutes per week.43
Statistical Analysis
25(OH)D concentration varies strongly by season, so single measurements may yield substantial misclassification of year-long vitamin D exposure. Thus, primary analyses evaluated 25(OH)D concentration as a continuous variable, adjusted by season and scaled to 10 ng/ml, a difference readily attained using a moderate dosage of cholecalciferol supplement.44 25(OH)D concentration was also categorized using a threshold of 15 ng/ml, because 25(OH)D concentrations below this level are associated with increased risk for incident cardiovascular events.4,5 Calcitriol concentration was evaluated as a continuous variable only, because accepted categories have not been established.
Prevalent CAC was defined as any Agatston score >0 at baseline. Poisson regression models quantified relative risk for prevalent CAC,45 with and without adjustment for precision variables [site, season, and 25(OH)D measurement batch], potential confounders (age, gender, race/ethnicity, BMI, physical activity, and smoking), and potential mediators (diabetes, BP, inflammation as assessed by CRP, and serum lipid concentrations). Age, BMI, physical activity, CRP (log-transformed), and lipids were modeled as continuous variables. For physical activity, results were not changed by addition of a quadratic term, using minutes instead of MET minutes, or substituting total moderate and vigorous physical activity for total intentional physical activity. Because measurement batch was determined by eGFR, adjustment for batch also adjusts for CKD. Adjusting 25(OH)D analyses for eGFR as a continuous variable did not substantially change results. Analyses assessing calcitriol were further adjusted for eGFR and serum phosphorous (continuous variables), because these factors affect renal production of calcitriol.
Incident CAC was defined as any follow-up Agatston score >0 among participants with an Agatston score of 0 at baseline. Poisson models were used to estimate risk associated with 25(OH)D concentration, as already described, with further adjustment for time between CAC measurements (median and mode 3 yr; range 1 to 6 yr).
Interaction was assessed for covariates that may affect conversion of 25(OH)D to calcitriol (age, gender, race/ethnicity, CKD, and serum phosphate) by including interaction terms for covariates (categorical variables) with 25(OH)D (continuous variable). The presence of interaction was formally assessed using the Wald test.
Severity and progression of CAC were examined among participants with Agatston scores >0 at baseline. Severity was examined using linear regression. Agatston scores were assessed as dependent variables, both untransformed and log-transformed, with models adjusted as already described. Progression of CAC was assessed by comparing the ratio of follow-up CAC with baseline CAC on the geometric mean (log) scale.
Statistical analyses were performed using R (R Foundation, Vienna, Austria) and Stata (Stata Corp., College Station, TX). All regression models used robust SEs. Statistical significance was taken to be P < 0.05, and no adjustments were made for multiple comparisons.
Disclosures
None.
Acknowledgments
This research was supported by contracts N01-HC-95159 through N01-HC-95165 and N01-HC-95169 from the National Heart, Lung, and Blood Institute; by grant 1KL2RR025015-01 from the National Center for Research Resources; and by grant K23 DK63274-01 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Data contained in this article were presented, in part, at the annual meeting of the American Society of Nephrology; 2008; Philadelphia, PA; November 4 through 9, 2008.
We thank the other investigators, the staff, and the participants of the MESA study for valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Low Calcidiol Levels and Coronary Artery Calcification: True, True, and Related?” on pages 1663–1665.
References
- 1.Michos ED, Melamed ML: Vitamin D and cardiovascular disease risk. Curr Opin Clin Nutr Metab Care 11: 7–12, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, Steele D, Chang Y, Camargo CA, Jr, Tonelli M, Thadhani R: Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int 72: 1004–1013, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Ravani P, Malberti F, Tripepi G, Pecchini P, Cutrupi S, Pizzini P, Mallamaci F, Zoccali C: Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int 75: 88–95, 2009 [DOI] [PubMed] [Google Scholar]
- 4.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D'Agostino RB, Wolf M, Vasan RS: Vitamin D deficiency and risk of cardiovascular disease. Circulation 117: 503–511, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giovannucci E, Liu Y, Hollis BW, Rimm EB: 25-Hydroxyvitamin D and risk of myocardial infarction in men: A prospective study. Arch Intern Med 168: 1174–1180, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, Kinkeldei J, Boehm BO, Weihrauch G, Maerz W: Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med 168: 1340–1349, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Melamed ML, Michos ED, Post W, Astor B: 25-Hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med 168: 1629–1637, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teng M, Wolf M, Ofsthun MN, Lazarus JM, Hernan MA, Camargo CA, Jr, Thadhani R: Activated injectable vitamin D and hemodialysis survival: A historical cohort study. J Am Soc Nephrol 16: 1115–1125, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Tentori F, Hunt WC, Stidley CA, Rohrscheib MR, Bedrick EJ, Meyer KB, Johnson HK, Zager PG: Mortality risk among hemodialysis patients receiving different vitamin D analogs. Kidney Int 70: 1858–1865, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Melamed ML, Eustace JA, Plantinga L, Jaar BG, Fink NE, Coresh J, Klag MJ, Powe NR: Changes in serum calcium, phosphate, and PTH and the risk of death in incident dialysis patients: A longitudinal study. Kidney Int 70: 351–357, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Lee GH, Benner D, Regidor DL, Kalantar-Zadeh K: Impact of kidney bone disease and its management on survival of patients on dialysis. J Ren Nutr 17: 38–44, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Shoben AB, Rudser KD, de Boer IH, Young B, Kestenbaum B: Association of oral calcitriol with improved survival in nondialyzed CKD. J Am Soc Nephrol 19: 1613–1619, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Autier P, Gandini S: Vitamin D supplementation and total mortality: A meta-analysis of randomized controlled trials. Arch Intern Med 167: 1730–1737, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF: Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72: 690–693, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Scragg R, Sowers M, Bell C: Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 27: 2813–2818, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Ford ES, Ajani UA, McGuire LC, Liu S: Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 28: 1228–1230, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Forman JP, Giovannucci E, Holmes MD, Bischoff-Ferrari HA, Tworoger SS, Willett WC, Curhan GC: Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension 49: 1063–1069, 2007 [DOI] [PubMed] [Google Scholar]
- 18.Martins D, Wolf M, Pan D, Zadshir A, Tareen N, Thadhani R, Felsenfeld A, Levine B, Mehrotra R, Norris K: Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: Data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 167: 1159–1165, 2007 [DOI] [PubMed] [Google Scholar]
- 19.Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP: 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110: 229–238, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dusso AS, Brown AJ, Slatopolsky E: Vitamin D. Am J Physiol Renal Physiol 289: F8–F28, 2005 [DOI] [PubMed] [Google Scholar]
- 21.Somjen D, Weisman Y, Kohen F, Gayer B, Limor R, Sharon O, Jaccard N, Knoll E, Stern N: 25-Hydroxyvitamin D3–1alpha-hydroxylase is expressed in human vascular smooth muscle cells and is upregulated by parathyroid hormone and estrogenic compounds. Circulation 111: 1666–1671, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Andress DL: Vitamin D in chronic kidney disease: A systemic role for selective vitamin D receptor activation. Kidney Int 69: 33–43, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Standing Committee on the Scientific Evaluation of Dietary Reference Intakes: Dietary reference intakes: Calcium, Phosphorous, Magnesium, Vitamin D, and Fluoride, Washington, DC, National Academy Press, 1997 [Google Scholar]
- 24.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA: Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 358: 1336–1345, 2008 [DOI] [PubMed] [Google Scholar]
- 25.Melamed ML, Muntner P, Michos ED, Uribarri J, Weber C, Sharma J, Raggi P: Serum 25-hydroxyvitamin D levels and the prevalence of peripheral arterial disease: Results from NHANES 2001 to 2004. Arterioscler Thromb Vasc Biol 28: 1179–1185, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Targher G, Bertolini L, Padovani R, Zenari L, Scala L, Cigolini M, Arcaro G: Serum 25-hydroxyvitamin D3 concentrations and carotid artery intima-media thickness among type 2 diabetic patients. Clin Endocrinol (Oxf) 65: 593–597, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Mathew S, Lund RJ, Chaudhary LR, Geurs T, Hruska KA: Vitamin D receptor activators can protect against vascular calcification. J Am Soc Nephrol 19: 1509–1519, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schulz E, Arfai K, Liu X, Sayre J, Gilsanz V: Aortic calcification and the risk of osteoporosis and fractures. J Clin Endocrinol Metab 89: 4246–4253, 2004 [DOI] [PubMed] [Google Scholar]
- 29.London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC: Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15: 1943–1951, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Gross ML, Meyer HP, Ziebart H, Rieger P, Wenzel U, Amann K, Berger I, Adamczak M, Schirmacher P, Ritz E: Calcification of coronary intima and media: Immunohistochemistry, backscatter imaging, and x-ray analysis in renal and nonrenal patients. Clin J Am Soc Nephrol 2: 121–134, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Rejnmark L, Lauridsen AL, Brot C, Vestergaard P, Heickendorff L, Nexo E, Mosekilde L: Vitamin D and its binding protein Gc: Long-term variability in peri- and postmenopausal women with and without hormone replacement therapy. Scand J Clin Lab Invest 66: 227–238, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Watson KE, Abrolat ML, Malone LL, Hoeg JM, Doherty T, Detrano R, Demer LL: Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation 96: 1755–1760, 1997 [DOI] [PubMed] [Google Scholar]
- 33.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O'Leary D, Saad MF, Shea S, Szklo M, Tracy RP: Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 156: 871–881, 2002 [DOI] [PubMed] [Google Scholar]
- 34.Adeney KL, Siscovick DS, Ix JH, Seliger SL, Shlipak MG, Jenny NS, Kestenbaum B: Association of serum phosphate concentration with vascular and valvular calcification in moderate chronic kidney disease: The multi-ethnic study of atherosclerosis. J Am Soc Nephrol 20: 381–387, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC: Calcified coronary artery plaque measurement with cardiac CT in population-based studies: Standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology 234: 35–43, 2005 [DOI] [PubMed] [Google Scholar]
- 36.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R: Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15: 827–832, 1990 [DOI] [PubMed] [Google Scholar]
- 37.Standards of medical care in diabetes: 2006. Diabetes Care 29 [Suppl 1]: S4–S42, 2006 [PubMed] [Google Scholar]
- 38.The Seventh Report of the Joint National Committee in Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, Bethesda, US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, 2004 [PubMed] [Google Scholar]
- 39.Levey AS, Greene T, Kusek JW, Beck GJ: A simplified equation to predict glomerular filtration rate from serum creatinine [Abstract]. J Am Soc Nephrol 11: A0828, 2000 [Google Scholar]
- 40.Friedewald WT, Levy RI, Fredrickson DS: Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18: 499–502, 1972 [PubMed] [Google Scholar]
- 41.Ainsworth BE: Assessment of Moderate Physical Activity of Minority Women in South Carolina. Available at: http://www.cdc.gov/prc/program-material/community-prevention-research-womens-health.htm Accessed February 24, 2009
- 42.Ainsworth BE, Irwin ML, Addy CL, Whitt MC, Stolarczyk LM: Moderate physical activity patterns of minority women: The Cross-Cultural Activity Participation Study. J Womens Health Gend Based Med 8: 805–813, 1999 [DOI] [PubMed] [Google Scholar]
- 43.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS: Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sports Exerc 32: S498–S504, 2000 [DOI] [PubMed] [Google Scholar]
- 44.Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ: Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77: 204–210, 2003 [DOI] [PubMed] [Google Scholar]
- 45.McNutt LA, Wu C, Xue X, Hafner JP: Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 157: 940–943, 2003 [DOI] [PubMed] [Google Scholar]