Abstract
Background
Sympathetic blockade is used in the management of complex regional pain syndromes in children but there are no data on the efficacy or mechanism(s) by which it produces pain relief. The purpose of this study is to compare the efficacy of lidocaine administered by lumbar sympathetic to intravenous route.
Methods
Under general anesthesia, children with unilateral lower limb complex regional pain syndromes received catheters along the lumbar sympathetic chain. In a double blind placebo-controlled crossover design, patients received intravenous lidocaine and lumbar sympathetic saline, or lumbar sympathetic lidocaine and intravenous saline. Spontaneous and evoked pain ratings and sensory thresholds were assessed before and after these two lidocaine/saline doses and between routes of lumbar sympathetic blockade and intravenous.
Results
Twenty-three patients, ages 10–18 years, were enrolled. There was evidence for reduction of mean pain intensity of allodynia to brush (mean −1.4, 95% CI −2.5, −0.3) and to pinprick temporal summation (mean −1.3, 95% CI −2.5, −0.2) with lidocaine treatment via the lumbar sympathetic blockade compared to intravenous route. Lumbar sympathetic blockade also produced significant reduction in pain intensity compared to pretreatment values of allodynia to brush, pinprick and pinprick temporal summation and verbal pain scores. Intravenous lidocaine did not produce significant changes in spontaneous and evoked pain intensity measurements compared to pretreatment values. There were no carry-over effects as assessed by route-by-period interaction.
Conclusions
Under the conditions of this study, the results provide some direct evidence that a component of pain may be mediated by abnormal sympathetic efferent activity.
Introduction
Complex regional pain syndromes (CRPS) type 1 and 2 are increasingly recognized in children. Although children generally respond more favorably to conservative therapy than adults with CRPS, the treatment of childhood CRPS remains unsatisfactory in some cases, with persistent pain and impairment despite intensive rehabilitative treatment.1
In adults with CRPS, it is a common practice to perform serial sympathetic nerve blockade to mitigate the presumed sympathetic over-activity, and thereby temporarily alleviate pain and facilitate physical therapy.2,3 In children, sympathetic nerve blockade is performed infrequently and there are no data to support its efficacy. For safety reasons, it is more common to place indwelling epidural catheters to avoid serial injections under general anesthesia, as is required for children to tolerate needle placement.4
We found only two randomized double blind crossover studies examining the efficacy of sympathetic blockade in adults with CRPS.5,6 To our knowledge no such controlled trials have been performed in children with CRPS.6
There are several methodological problems in interpreting the results of treatment responses to sympathetic blockade in adults with CRPS. Among these problems are spread of local anesthetics to epidural and subarachnoid sites, rapid systemic absorption and suppression of ectopic impulse generators in the injured peripheral nerve, and placebo responses.7–11 In view of these interpretive limitations, lack of data on efficacy of lidocaine for intravenous or lumbar sympathetic blockade and the high placebo responses to treatment of pain in pediatric parallel design trials,12 we chose to compare the efficacy of a single injection of lidocaine by lumbar sympathetic blockade (LSB) to intravenous (IV) route in children in a randomized placebo-controlled double-blind crossover design. Our null hypotheses were that the differences in the mean change of evoked pain measures including allodynia to brush, pinprick, and pinprick temporal summation between LSB and IV administered lidocaine is zero (H0: μLSB - μIV = 0). Our alternative hypotheses were that mean differences of 2 points or more in reductions for each of the following three pain measures: a) brush allodynia, b) pinprick allodynia, and c) allodynia to pinprick temporal summation as assessed by 0-to-10 point Color Analog Scale (CAS) could be observed between LSB and IV lidocaine administration (HA: μLSB - μIV > 2 points).
Materials and Methods
The study protocol was approved by the institutional Clinical Investigation Committee (Children’s Hospital, Boston, Massachusetts) and was conducted between June 2002 and August of 2004. Written informed parental consent and patient assent were obtained. Diagnosis of CRPS was based on the international association for the study of pain taxonomy.13 We did not categorize patients into subgroups of CRPS 1 and 2 because the diagnosis of CRPS 2 was not confirmed by electrodiagnostic tests, either because they were not clinically indicated or patients and parents objected to tests that involved repeat needle insertions into the painful limb without sedation.
Enrollment was restricted to children with CRPS in one lower limb who failed to respond to a 6-week trial of aggressive physical, bio-behavioral, and pharmacological therapies, as described previously.1 Exclusion criteria included: (1) ongoing chronic medical illness other than CRPS, (2) features indicative of a current or past underlying neurologic, rheumatologic or dermatologic disorder, (3) pregnancy or lactation, (4) history of attention deficit hyperactivity disorder or use of stimulants and/or central nervous system depressant drugs within a week of testing because, they can alter alertness and/or pain perception, (5) previous LSB with local anesthetic and/or surgical or chemical sympathectomy of the affected limb, (6) presence of mechanical allodynia or hyperalgesia at the identical opposite side to the painful area, and (7) presence of major psychiatric comorbidity. If a patient was receiving non-steroidal anti-inflammatory drugs, these agents were withheld for two days prior to the testing. At our multidisciplinary clinic a psychologist formally evaluates all patients on the initial visits. No financial compensation was offered to subjects for participating in this study.
On the day of admission, LSB and lumbar epidural catheters were placed under general anesthesia with sevoflurane and nitrous oxide via mask and spontaneous breathing. A single anesthesiologist (NFS) performed all catheter placements. Patients were placed in lateral decubitus with the affected side in nondependent position. A standard percutaneous lateral paravertebral approach was used for lumbar sympathetic blockade.4 A 20-gauge multipore epidural catheter was placed through an 18-gauge Tuohy needle at the anteromedial border of L2 or 3 vertebral bodies. The correct needle and catheter placement was guided by fluoroscopy in antero-posterior and lateral views and confirmed with noting prevertebral linear spread of 2 mL of Iohexol 180 injected at approximate rate of 1mL/10 seconds. Both LSB and epidural catheters were not injected with test doses or other doses of local anesthetics. Patients were prescribed acetaminophen and intravenous ketorolac for management of pain related to catheter placement. In one patient, initial contrast injection into the psoas muscle was identified and the needle tip was redirected and repositioned in the correct site. There were no procedure-related complications. An indwelling epidural catheter was also placed at L2-L3 for each patient for management of pain after completion of the study to facilitate in-house daily physical therapy as part of routine clinical care.4
The reliability of LSB in this study was assessed by semi-objective clinical criteria of increased ipsilateral skin temperature and reduction of evoked pain. Both these criteria are surrogate measures of sympathetic nerve blockade but they do not necessarily predict complete inhibition of sympathetic nerve function. The optimal predictors of a response to sympathetic nerve blockade are positive quantitative sudomotor axon reflex test, and rise in skin temperature.14 We did not perform quantitative sudomotor axon reflex test because it is time consuming and requires trained personnel and dedicated laboratory.
In an attempt to address some expectation and desire for relief in placebo responders, we instructed all patients that the study drug may be effective and that it was just as important for the study personnel to know if it was ineffective in relieving patient’s pain. It was also explained that their response to study medication would have no impact on treatment of the limb pain with epidural analgesia after the completion of the study.
The morning following placement of LSB and epidural catheters, we randomized the patients using a pseudo-random number generator to receive either: (1) injection of lidocaine 1% (0.1 mL/kg over 1 minute) by LSB catheter and preservative-free physiological saline 0.9% (0.1 mL/kg) intravenously or (2) saline by LSB catheter and lidocaine intravenously. These two-paired injections were administered in two session 12 hours apart, in order to allow adequate systemic washout of lidocaine. The volume of lidocaine 1% was 0.1mL/kg and did not exceed a total of 6 mL which is minimally adequate to achieve satisfactory sympathetic ganglia blockade.15 The dose of lidocaine was deliberately selected to be fairly low, in an effort to minimize the chances for spillover to somatic nerves. In this choice, we recognized the potential for incomplete sympathetic blockade in some cases. A single blinded researcher (PM) performed all bedside examinations and computerized quantitative sensory testing (QST) according to standard study protocols described below on page 11.16,17 Neither the investigator (PM) who performed and collected the pain assessment data in all patients nor the patients were aware of the nature of the solutions injected.
In each session the spontaneous and evoked mechanical pain intensity and thermal QST thresholds were measured before and after drug administration. Patients were asked to describe the quality of pain. If the patient had difficulty, verbal descriptors of the pain from McGill Pain Questionnaires were read to assist, but no formal effort was made to define these words. The pain intensity was assessed using a global 4-point verbal pain scale (none, slight, moderate, severe) and CAS for spontaneous pain, brush allodynia, and allodynia to pinprick, and pinprick temporal summation.18,19
Stimulus-evoked pain was assessed by a standardized testing protocol. Brush allodynia (mechanical dynamic allodynia) was assessed by stroking the skin in painful area with a hand-held soft brush and swept at a rate of approximately 3–5 cm/second. The intensity of pain evoked was graded on the CAS.
Pinprick allodynia (mechanical static allodynia) was tested with a single application of a pinprick (nonpenetrating needle prick). A 20-gauge Quincke tip needle was suspended through a 5cc-syringe barrel to serve as a handle and was brought in to a gentle contact at 90° with the skin. The needle load was adjusted at a constant weight of 1.2 g (∼11.8 mN), which is within one standard deviation value of pinprick detection threshold for healthy adult skin.20–22 Perception of pinprick sharp pressure or mild unpleasantness was first established on the unaffected homologous site. If patients reported that the perception of unpleasantness/pain on the affected side was different than the unaffected side, she/he was asked to rate the pain on the affected side using the CAS, and this rating was taken as a measure of pinprick allodynia. The intensity of sharpness-pressure sensation was not graded on the unaffected site.
Allodynia to pinprick temporal summation (allodynia to punctuate temporal summation) was evaluated by presenting repetitive tapping of the skin with 5 identical pinprick stimuli delivered at a 3-second interval using a hand-held device and needle weighing 1.2 g (∼11.8 mN) described above on page 9. The needle moved freely for an approximately one-centimeter vertical distance when applied at right angle to the skin and the contact time with the skin was one second. The five stimuli were presented only once and patients rated the evoked pain intensity of the second and the fifth stimuli on the CAS. Temporal summation was established if the intensity of the last stimulus in the train of five was at least 33% greater than the intensity of the second stimulus in the train.
Quantitative thermal thresholds were determined using the Medoc TSA-2001 device (Medoc Ltd. Advanced Medical Systems, Ramat Yishai, Israel) and by the method of limits, as described in our previous studies of establishing normative values in healthy children and adolescents and in those with CRPS.16,17 The thermal sensory analyzer operates by a microcomputer-driven 3 cm × 3 cm (9 cm2) Peltier contact thermode. The entire thermode-stimulating surface was placed in contact with the skin-testing site and secured by a velcro band without stretch. The thermode baseline temperature was kept at 32°C and stimulation temperature had a potential range of 0–50°C. If patients were unable to feel heat or cold pain at the cut off temperature values of 0° or 50°C respectively, the temperature ramp was terminated and the low or high temperature limit value was assigned to avoid potential tissue injury. The rate of temperature change was kept constant at 1°C/second for assessment of cold and warm sensations and at 1.5°C/second for assessment of cold and heat pain. The thermal stimulus intensity was increased linearly from the baseline thermode temperature of 32°C and subjects were asked to press a button when a specified sensation was first perceived (detection threshold). Halting the stimulus reset the thermode temperature to baseline. The return rate of the stimulus was 1°C/second for cold and warm sensation and 10°C/second for cold and heat pain. Stimuli were presented as a train of four with an interstimulus interval of 6 seconds for measurement of cold and warm detection thresholds, and as a train of three stimuli at 10-second intervals for cold and heat pain detection thresholds. Mean values of a set of responses to a train of stimuli were calculated as the detection threshold.16
Skin temperatures of both affected and unaffected foot dorsum were recorded using a contact thermistor (Mallinckrodt Mon-a-Therm Model 4070, St. Louis, MO).
Vital signs (blood pressure, heart rate, electrocardiogram, pulse oximetry) were monitored at 5-min intervals for an hour after study drug injection and patients were observed for mental status change and signs and symptoms of lidocaine toxicity.
On the day of the testing, a single researcher (PM) documented the symptoms and signs using a CRPS checklist based on the international association for the study of pain criteria.13 All sensory tests were performed before and approximately 30 min after injections of the lidocaine/saline in a quiet room, temperature 20–23°C, with the patient comfortably seated and skin sites were exposed to ambient temperature for 10–15 min prior to testing. Each patient marked out the site of maximum pain, and the periphery of the painful zone. Boundaries of the allodynia zone, evoked by a soft brush, were defined before testing by stimulating from nonpainful sites converging onto the affected area of greatest pain in four directions or more. Sensory testing was conducted on the skin area of greatest reported pain intensity. Testing was completed within 80–90 minutes. The pain terms used in the study follows the definitions recommended by the international association for the study of pain.
Statistical Analysis
The goal of using the crossover design in this study was to enhance efficiency since each patient serves as his or her own control, which increases statistical power and precision for estimating treatment differences. In our two-session crossover design, we used a pseudo random number generator to assign patients to the sequence of treatments (AB or BA) with the goal of analyzing differences between the individual treatments (LSB vs. IV). The uniform (0,1) distribution was used for randomization; by default, SPSS software package (version 16.0, SPSS Inc., Chicago, IL) uses a random seed for initialization.
The nonparametric Wilcoxon signed-ranks test was used to evaluate changes in CAS, verbal pain scores and thermal QST for each route of lidocaine administration (LSB, IV). Since variables demonstrated some skewness as assessed by the Kolmogorov-Smirnov test, data are presented both in terms of the median and range as well as in terms of the mean difference (post-pre) between the two routes with 95% confidence intervals.23 The potential for carry-over effects was assessed for each variable using the F-test in within-subjects analysis of variance (ANOVA) with repeated-measures based on the route-by-period interaction.24 Patients in this AB/BA crossover trial were randomly assigned to the order of the period in order to ensure unbiased comparisons between the LSB and IV routes in assessing treatment efficacy. Statistical analysis was performed using the SPSS software package. Power analysis indicated that the sample size of 23 subjects provided 80% power (a = 0.05, b = 0.20) to detect a mean difference of 2 points or more in each of the CAS pain measures between the LSB and IV methods of lidocaine administration assuming a variability of 3 points (standardized effect size = 0.67) using repeated-measures analysis (version 7.0, nQuery Advisor, Statistical Solutions, Saugus, MA).25 Two-tailed values of P<0.05 were considered statistically significant.
Results
Twenty-five consecutive patients were enrolled and two were excluded because of severe intolerance to/avoidance of light brush as required for this protocol. Twenty-three patients (20 females, 3 males, ages 14.4 ± 2.4 years, range 10–18 years), were included in the final analyses.
The onset of pain followed a specific noxious event in all patients except one. Eight experienced sports-related injuries, six developed pain after surgery, eight reported accidental trauma, and one patient was unable to recall a specific inciting event. The median duration of the symptoms of CRPS was 9 months (interquartile range 4.5–23, range 2–72 months). All patients in this study reported spontaneous persistent pain at rest and most of them used sensory pain descriptors rather than affective and other pain dimensions on modified McGill pain scale; sensory (n=19), affective (n=5), evaluative (n=2), and miscellaneous (n=6). The spontaneous pain increased with movement of the affected limb and was associated with difficulty weight bearing. Fourteen patients were partially weight bearing: 3 used wheelchairs, 10 walked with crutches and 1 walked with a cane. Nine patients walked with a limp.
The following autonomic features were present; purple/red color change (n=21), excessive sweating (n=3), dry skin (n=5), swelling (n=16), hair growth increase/decrease (n=8), and excessive nail growth and/or brittle nails (n=5). Skin temperature in the affected foot was more than 1ºC colder than the unaffected foot in 15 subjects, more than 1ºC warmer in 5 subjects and within 1ºC in 3 subjects. Mild-to-moderate atrophy (calf muscles circumference differences of 2 cm or greater) of the calf muscles was present in 11 patients and swelling of the calf muscles was present in 5 patients.
Patients presented with allodynia to light brush (n=20), pinprick (n=21) and to pinprick temporal summation (n=22) and all these three mechanically evoked allodynia were concurrently present in 20 out of the 23 patients.
Compared with intravenous lidocaine route, LSB lidocaine route produced clinically significant reduction in mean allodynia to brush (mean −1.4, CI −2.5, −0.3) and pinprick temporal summation (mean −1.3, CI −2.5, −0.2) (table 1). There was no evidence of a difference between the two routes in allodynia to pinprick. The improvement in verbal pain scores after treatment with lidocaine by LSB was clinically significant compared to IV route (table 2).
Table 1.
Difference Between Lumbar Sympathetic Blockade and Intravenous Lidocaine Routes for Color Analog Scale Pain Scores
| CAS Pain Score | Mean Difference (LSB – IV) | 95% Confidence Interval of the Difference | ||
|---|---|---|---|---|
| Spontaneous Pain | −0.5 | −1.4, 0.5 | ||
| Brush Allodynia | −1.4 | −2.5, −0.3* | ||
| Pinprick Allodynia | −0.5 | −1.3, 0.2 | ||
| Pinprick Temporal | ||||
| Summation Allodynia | −1.3 | −2.5, −0.2* | ||
Mean difference was determined by computing the post – pre change in pain score for each route and then comparing the results between the routes.
A negative mean difference indicates that the reduction in pain was on average greater for LSB than IV and the significance of this difference is evaluated by the 95% CIs. (* mean difference between the two routes is significantly different from 0).
CAS = Color Analog Scale
IV = Intravenous
LSB = Lumbar Sympathetic Blockade
Table 2.
Changes in Verbal Pain Scores Between Lumbar Sympathetic Blockade and Intravenous Lidocaine Routes
| LSB Lidocaine (N = 23) | IV Lidocaine (N = 23) | |||
|---|---|---|---|---|
| Verbal Pain Score | Pre | Post | Pre | Post |
| Slight Pain | 3 | 7 | 3 | 5 |
| Moderate Pain | 6 | 7 | 10 | 5 |
| Severe Pain | 14 | 9 | 10 | 13 |
| Improvement after* | ||||
| LSB > IV route | 11 | |||
| IV >LSB route No difference between routes |
3 9 |
|||
Changes in ordinal pain scores (post – pre) were compared between the different routes of administration.
Comparison of the results between routes indicated greater improvement following LSB (P = 0.05, Wilcoxon signed-ranks test).
IV = Intravenous
LSB = Lumbar Sympathetic Blockade
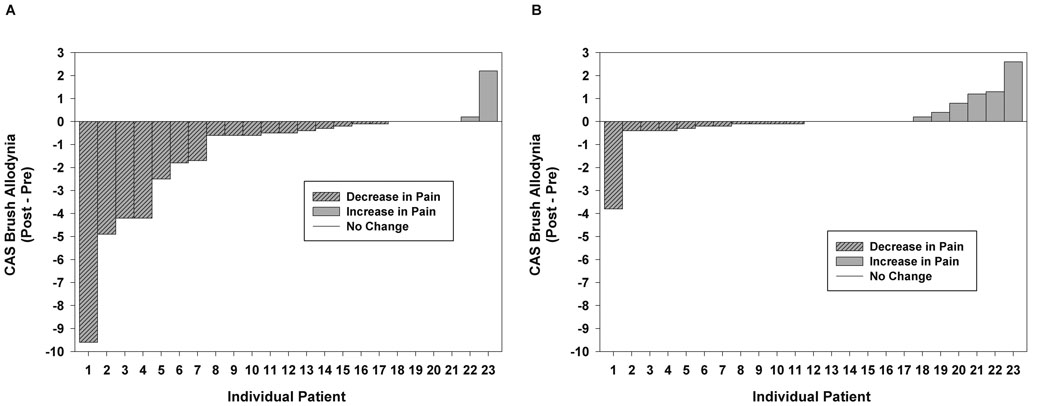
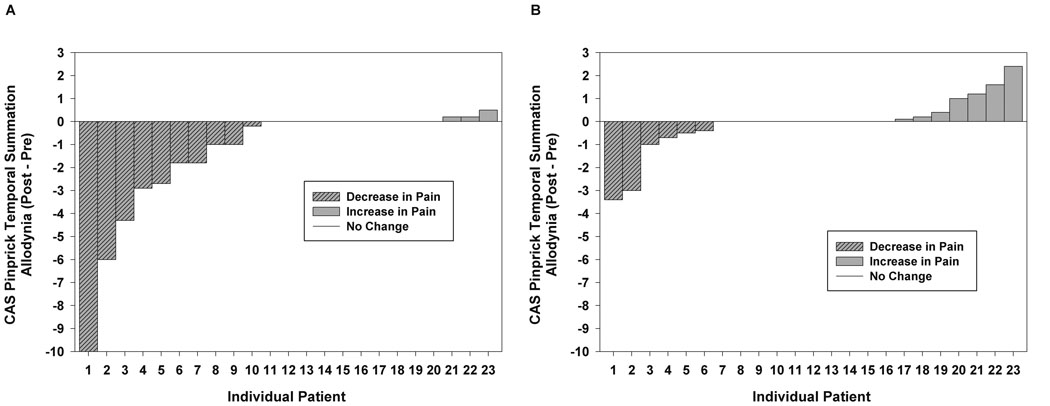
Lumbar sympathetic blockade with lidocaine produced significant statistical and clinical reduction in allodynia to brush and temporal summation compared to pretreatment values (table 3). Clinically significant reduction in CAS pain intensity of 2 points or greater occurred after LSB for allodynia to brush in 5 patients (fig. 1), allodynia to pinprick in 3 patients (not shown in the figure) and allodynia to pinprick temporal summation in 5 patients (fig. 2). Intravenous lidocaine did not produce significant changes relative to pretreatment values of allodynia to brush, pinprick and pinprick temporal summation (table 3).
Table 3.
Comparison of Color Analog Scale Pain Scores Before and After Administration of Lidocaine via the Lumbar Sympathetic Blockade and Intravenous Routes
| LSB Lidocaine (N = 23) | IV Lidocaine (N = 23) | |||||
|---|---|---|---|---|---|---|
| CAS Scores | Pre | Post | P-value | Pre | Post | P-value |
| Spontaneous | 5.4 | 4.8 | 6.0 | 5.8 | ||
| Pain | 1.5 – 10 | 1.4 – 10 | 0.19 | 1.8 – 9.8 | 1.6 – 10 | 0.88 |
| Brush | 5.9 | 2.8 | 6.2 | 5.8 | ||
| Allodynia | 0 – 10 | 0 – 10 | <0.01* | 0 – 10 | 0 – 10 | 0.92 |
| Pinprick | 6.8 | 5.2 | 7.0 | 6.6 | ||
| Allodynia | 0 – 10 | 0 – 10 | <0.05* | 0 – 10 | 0 – 10 | 0.72 |
| Pinprick | 9.8 | 8.2 | 9.0 | 10 | ||
| Temporal | 0 – 10 | 0 – 10 | <0.01* | 0 – 10 | 0 – 10 | 0.91 |
| Summation | ||||||
| Allodynia | ||||||
Data are median and range. P-values were determined by the Wilcoxon signed-ranks test (two-tailed).
Statistically significant.
CAS = Color Analog Scale
IV = Intravenous
LSB = Lumbar Sympathetic Blockade
Figure 1.
A. Lumbar Sympathetic Blockade with lidocaine. Color analog scale (CAS) scores of brush allodynia intensity differences pre- and post-lumbar sympathetic blockade.
B. Intravenous lidocaine administration. Color analog scale (CAS) scores of brush allodynia intensity differences pre- and post-intravenous lidocaine treatment.
Figure 2.
A. Lumbar Sympathetic Blockade with lidocaine. Color analog scale (CAS) scores of pinprick temporal summation allodynia intensity differences pre- and post-lumbar sympathetic blockade.
B. Intravenous lidocaine administration. Color analog scale (CAS) scores of pinprick temporal summation allodynia intensity differences pre- and post-intravenous lidocaine treatment.
LSB produced clinically relevant improvement of verbal pain scores compared to pretreatment values in 9 patients and no change in pain scores in 14 patients. Intravenous lidocaine produced reduction of pain in 3 patients and worsening of pain in 5 patients (table 2).
The injection of either lidocaine or saline via the LSB catheter or the intravenous route did not produce changes in QST detection thresholds (table 4).
Table 4.
Comparison of Quantitative Sensory Testing Parameters Before and After Administration of Lidocaine via the Lumbar Sympathetic Blockade and Intravenous Routes
| LSB Lidocaine (N = 23) | IV Lidocaine (N = 23) | |||||
|---|---|---|---|---|---|---|
| QST (°C) | Pre | Post | P-value | Pre | Post | P-value |
| Cold Sensation | 29.6 | 30.2 | 30.1 | 29.8 | ||
| 17.0 – 31.6 | 25.6 – 31.5 | 0.16 | 25.1 – 31.5 | 22.6 – 31.2 | 0.06 | |
| Warm Sensation | 35.2 | 35.4 | 35.3 | 35.4 | ||
| 33.5 – 39.4 | 33.3 – 41.1 | 0.52 | 33.3 – 40.3 | 33.9 – 40.5 | 0.78 | |
| Cold Pain | 27.4 | 25.5 | 27.4 | 25.9 | ||
| 0.9 – 31.1 | 17.2 – 31.2 | 0.23 | 0.6 – 31.1 | 10.9 – 31.0 | 0.20 | |
| Heat Pain | 39.9 | 40.2 | 40.3 | 39.8 | ||
| 33.9 – 48.3 | 33.4 – 44.1 | 0.62 | 33.2 – 47.4 | 33.3 – 45.0 | 0.54 | |
Data are median and range. P-values were determined by the Wilcoxon signed-ranks test (two-tailed). No significant differences were detected between pre and post results for LSB or IV lidocaine administration.
IV = Intravenous
LSB = Lumbar Sympathetic Blockade
QST = Quantitative Sensory Testing
No carry-over effects were found for any variable of spontaneous and evoked pain assessment and QST parameters based on route-by-session interaction test (table 5).
Table 5.
Assessment of Carry-Over Effects*
| F-test | P-value | |
|---|---|---|
| Verbal Pain Scores | 0.25 | 0.86 |
| Color Analog Scale Pain Scores | 0.20 | 0.89 |
| Brush Allodynia | 0.27 | 0.85 |
| Pinprick Allodynia | 0.16 | 0.92 |
| Pinprick Temporal Summation Allodynia | 0.02 | 0.99 |
| Cold sensation (°C) | 0.03 | 0.99 |
| Warm sensation (°C) | 0.24 | 0.87 |
| Cold pain (°C) | 0.08 | 0.97 |
| Heat pain (°C) | 1.08 | 0.37 |
evaluated using interaction F-test (route by period).
The mean ambient room temperatures were similar between the first and second sessions (22 + 0.7 ºC vs. 22.8 + 1ºC). There was no difference observed at baseline skin temperature between IV and LSB groups.
Two-way repeated-measures ANOVA was performed to evaluate changes in the skin temperature after administration of lidocaine by IV and LSB routes. The analyses revealed a significant difference in temperature for the route of administration with trends for temperature increase by LSB and decrease by IV routes (P = 0.008, interaction test). At the completion of lidocaine administration, the skin temperature was significantly lower by IV compared to that after LSB route (29.4 ± 2.0ºC vs. 31.4 ± 2.6ºC respectively, P = 0.009).
There were no clinical or statistical significant differences in vital signs measurement compared to pre-blockade baseline values after administration of lidocaine by intravenous route (systolic blood pressure 114.7 + 9 vs. 114.0 + 10; diastolic blood pressure 61.5 + 6 vs. 64.2 + 9; heart rate 91 + 15 vs. 90 + 14, oxyhemoglobin saturation 99.5 + 0.7 vs. 99.6 + 0.6) and by LSB route (systolic blood pressure 114.1 + 11 vs. 116.3 + 10; diastolic blood pressure 62.5 + 8 vs. 64.9 + 5; heart rate 95.7 + 17 vs. 92.8 +15, oxyhemoglobin saturation 99.4 +0.7 vs. 99.5 + 0.7).
Patients were queried for side effects every five minutes after infusion of the study drugs. Patients in the intravenous lidocaine group reported higher frequency of adverse effects of headache (n=4), lightheadedness (n=7), nausea (n=1), blurred vision (n=1), muffled sounds (n=1) and oral numbness (n=1). Patients in the LSB lidocaine group reported lightheadedness only (n=6). None of these side effects in either group lasted more than 5–10 min.
Discussion
We found evidence for reduction in pain intensity of allodynia to brush and pinprick temporal summation and of verbal pain scores with administration of lidocaine via LSB compared to IV route. The administration of lidocaine via the LSB route (with concomitant IV saline) produced clinical and statistical improvement compared to pretreatment values of verbal pain scores and evoked pain by two points or more on CAS for allodynia to brush, pinprick and to pinprick temporal summation. Intravenous lidocaine (and concomitant saline via LSB) administration did not produce clinical or statistical significant changes in spontaneous and mechanically evoked pain. There were no apparent carry-over effects of lidocaine between sessions at 12-hour intervals.
Local anesthetics are frequently used for sympathetic nerve blockade as a part of multidisciplinary management to alleviate pain and promote functional restoration in patients with CRPS, but the results of several studies have been inconclusive.26,27 Pain relief assessments after therapeutic procedures can be confounded by technical difficulties and placebo responses. A recent systematic review found only two randomized, blinded, and crossover trials in a small number of reflex sympathetic dystrophy/CRPS adults who received stellate and lumbar sympathetic blockade. The first study remains in an abstract format, and showed that at two hours after stellate ganglion blockade, there was at least 50% pain relief following injection of bupivacaine 0.125% in 12/16 patients and of saline in 8/16; at 48-hours, the pain relief persisted in 5/16 bupivacaine group and in 8/16 saline group. 6 In the second study, stellate ganglion blockade was performed in 4 and LSB in 3 patients with either bupivacaine 0.125% or lidocaine 1%. The peak reduction in pain intensity measured at 30 minutes after blockade was observed in 6 out of 7 patients, and was similar for local anesthetics (74%) and saline (69%). The mean duration of pain relief was longer with local anesthetics (3 days and 18h) than with saline (20 h).5
The high incidence of brief reduction in self-reported pain and mechanical allodynia after sympathetic blockade with saline could have resulted from direct physical effect on the sympathetic chain/trunk or from placebo responses.5,6,28 The total volume of saline injected varied from 10 mL28, 25 mL5, to unspecified volumes.6 The benefit of pain relief with local anesthetic lasted longer than saline in one study and the pain relief occurred with saline in a larger number of patients in a second study could possibly be due to placebo responses.5,6
In the current study, the injection of saline through intravenous or LSB catheters did not produce changes in pain intensity or thermal thresholds. The discrepancy in the findings between this and the adult studies could have resulted from different testing paradigms evoking different degrees of placebo responsiveness, or could be related to a specific physiochemical effect of saline in different volumes and/or temperatures. Conceivably, in adult studies, the administration of larger volumes of saline at room temperature could have spread to sensory roots and suppressed somatic nerve conduction by transient local cooling and/or mass effect that may compress the sympathetic ganglia.28
A previous effort to determine the efficacy of sympathetic blockade with local anesthetics from review of 29 studies was hampered by poor design, non-randomization, small sample size, and unstandardized outcome measures.2 The pain relief was complete in 29% of patients, partial or adequate in 41% and minimal in 32% of patients.2 The absence of controls raises questions about the efficacy of sympathetic blockade and possibility of overestimation of treatment response.
In this study, administration of small doses of lidocaine (5.3 + 1 ml) for LSB produced reduction in verbal and evoked pain (table 2 and table 3). While the direct application of lidocaine to sympathetic ganglia produces noticeable sympatholytic blockade, its systemic absorption may attenuate the peripheral sensory activity of the injured neuron at doses that do not produce nerve conduction blockade.29,30 Animal studies have shown that high lidocaine doses, equivalent to anti-arrhythmic blood level in man, are necessary to effectively suppress the ectopic and evoked neurophysiological activity from injured axons.31
The data from this study indicate that intravenous lidocaine did not produce measurable effect on the spontaneous and evoked pain, possibly because the dose was too small to suppress ectopic impulse generators of the peripheral axon. The dose is also much lower than the dose that produces significant diminution of spontaneous pain and brush allodynia in adult patients with peripheral neuropathy and CRPS.11,32
Both IV and LSB lidocaine produced minor side effects. The most prominent was lightheadedness that resolved promptly within 5–10 min. Although we did not measure plasma concentrations after injection of IV lidocaine we expect that the mean peak plasma level in our patients would be comparable to that observed after IV lidocaine 1 mg/kg administered in anesthetized children.33 Such a plasma level when sustained for 10–20 min by lidocaine infusion in awake adults with neuropathic pain is shown to produce side effects similar to those seen in our patients.11,32
Unlike adult studies, neither IV nor LSB lidocaine produced significant reductions in spontaneous pain on CAS. The intravenous lidocaine plasma concentrations required to produce considerable reduction in spontaneous pain in adults with neuropathic pain including reflex sympathetic dystrophy is in the therapeutic range of anti-arrhythmic effect and is much higher than that produced by the single dose of lidocaine used in this study.34 Spontaneous pain, does not always result from direct nerve injury but could result from the inflammation of the adjacent uninjured nerves that may not respond to selective sympathetic blockade.34
Variable spontaneous pain relief is observed after sympathetic ganglion blockade in adults with neuropathic pain ranging from nil to complete relief.27 In our study, only LSB lidocaine produced significant reduction in verbal pain scores but not with visual analog scores (table 2 and table 3). The lack of concordance between these two scales in our study could be explained by the lack of interchangeability observed in a recent adult study involving diverse pain mechanisms.35 Additionally, the baseline median pain on visual analog scale in this study was moderate and various studies have shown inconsistent reliability of assessing moderate pain with visual analog scale compared to verbal rating scale.35,36
Patients in the LSB group, 39% experienced considerable reduction in verbal pain scores from severe to moderate/slight and moderate to slight pain. Twenty-two percent of patients experienced clinically significant reduction in brush allodynia or allodynia to pinprick temporal summation. This response rate is relatively low compared to open-label adult reflex sympathetic dystrophy trials using comparatively larger doses of local anesthetics that range from 48% improvement with fluoroscopic guided stellate blockade and 83% with computerized tomography guided LSB blockade as measured by cutaneous temperature and sympathetic skin responses.7,37 The reduction of both spontaneous and evoked pain after lidocaine LSB in this study could have resulted from suppression of sympathetic system overactivity that may have been amplified and dynamically maintained by ongoing abnormal peripheral input in some patients.5
The baseline median thermal sensory thresholds of the affected limbs in both LSB and IV groups were within normal reference interval of 2.5th−97.5th percentile values for age and were not significantly different after administration of the study drugs (table 4).16 None of these patients reported numbness or motor weakness suggestive of inadvertent somatic nerve blockade. This suggests that the small dose of lidocaine used in this study produced a relatively specific sympathetic blockade without somatic blockade. Administration of intravenous lidocaine has no known effect on normal C-fiber and A-delta fiber nerve conduction therefore would not be expected to alter thermal sensory thresholds.7,38
An interesting finding in this study is that IV lidocaine and concomitant LSB saline produced worsening of brush allodynia and allodynia to temporal summation in some patients (fig. 1B and fig. 2B). It is possible that the higher rate of central nervous system side effects might have induced anxiety/distress that lowered the threshold of the ongoing evoked pain.5 The improvement of brush allodynia occurred in one and of pinprick summation allodynia in 2 patients following IV lidocaine could be attributable to direct effect of lidocaine at the sensitive sodium channels of the injured nociceptors.34
The rise in skin temperature (1.3 + 0.4ºC) after LSB lidocaine in this study was lower than the magnitude reported in an adult study (mean 4ºC) after LSB with a large volume of bupivacaine 15 mL.39 However, the magnitude of skin temperature rise following sympathetic blockade does not always correlate predictably with the success of sympathetic blockade or the magnitude of pain relief; the lower the baseline skin temperature, the higher the rise in temperature after sympathetic blockade.5,27
This study has limitations and there are several reasons that may explain the low success rate of LSB in this study compared to adult trials. As noted above on page 9, we deliberately chose quite small doses of lidocaine for LSB and IV administration, to increase the specificity of the block and to avoid other confounding effects. Such small doses of intravenous lidocaine are also not expected to produce effective suppression of ectopic impulses in the injured peripheral nerves responsible for generation of spontaneous pain. We did not confirm the completeness of LSB with the use of an objective test for sympathetic function inhibition such as the quantitative sudomotor axon reflex test for reasons outlined above on page 9. Because the LSB indwelling catheters were injected over 24-hour period, it is possible that in some patients incomplete response was due to catheter displacement away from the sympathetic trunk. The low response rate may also reflect a lower incidence of truly sympathetically-maintained pain in children. The true incidence of sympathetically mediated pain in children and adults is unknown but reportedly rare in adults with post-traumatic neuropathic pain.40 An alternative explanation is that the pain complex could be only partly sympathetically dependent, as inferred from studies involving intravenous phentolamine trials.26 The use of fluoroscopic rather than computerized tomography guidance in this study and in view of variability in anatomical location of the sympathetic chain might have also contributed to the lower reliability in our patients.37 Lastly, inclusion of children with unilateral warm affected skin may account for failed response to LSB because it indicates abnormal hypoactive sympathetic function and further inhibition with LSB is not expected to sizably increase the skin temperature and relief pain.41
Conclusion
Under the study conditions, LSB with small doses of lidocaine produces variable degrees of pain relief with overall significantly greater reductions in specific pain measures in children with CRPS compared to the same doses of lidocaine administered IV. Our data provide evidence that a component of pain can be mediated by abnormal sympathetic efferent activity.5,13,41
Acknowledgments
Financial Support:
Navil F. Sethna, MB, ChB. Reflex Sympathetic Dystrophy Research Fund by Elizabeth. A. Schissler fund. 1 Seabury Avenue. Ledyard, Connecticut
Petra M. Meier, MD. Bernische Krebsliga (Bernese Cancer Society), Bern, Switzerland. Swiss Society of Anesthesiology, Bern, Switzerland. Department Klinische Forschung Medizinische Fakultaet der Universitaet Bern (Research Department of the Medical School Bern), Bern, Switzerland.
Charles B. Berde, M.D., Ph.D., National Institute of Child Health and Human Development Grant 1RO1HD35737. Rehabilitative Care of Children with Neuropathic Pain. National Institutes of Health, Rockville, MD 20847
Footnotes
Abstract presentation: Portions of this study were presented at the Annual Meeting, of American Society of Anesthesiologists, October 13–17, 2007, San Francisco, California
Summary Statement: In a randomized controlled trial of children with Complex Regional Pain Syndrome, lumbar sympathetic blockade produced significant reduction of verbal pain scores and allodynia to brush and temporal summation compared to treatment with intravenous lidocaine.
References
- 1.Lee BH, Scharff L, Sethna NF, McCarthy CF, Scott-Sutherland J, Shea AM, Sullivan P, Meier P, Zurakowski D, Masek BJ, Berde CB. Physical therapy and cognitive-behavioral treatment for complex regional pain syndromes. J Pediatr. 2002;141:135–140. doi: 10.1067/mpd.2002.124380. [DOI] [PubMed] [Google Scholar]
- 2.Cepeda MS, Lau J, Carr DB. Defining the therapeutic role of local anesthetic sympathetic blockade in complex regional pain syndrome: A narrative and systematic review. Clin J Pain. 2002;18:216–233. doi: 10.1097/00002508-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Nelson DV, Stacey BR. Interventional therapies in the management of complex regional pain syndrome. Clin J Pain. 2006;22:438–442. doi: 10.1097/01.ajp.0000192515.50955.9f. [DOI] [PubMed] [Google Scholar]
- 4.Sethna NF, Wilder RT. Regional anesthetic techniques for chronic pain. Pain in infants, children, and adolescents. In: Schechter NL, Berde CB, Yaster M, editors. Baltimore: Williams & Wilkins; 1993. pp. 281–293. [Google Scholar]
- 5.Price DD, Long S, Wilsey B, Rafii A. Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome patients. Clin J Pain. 1998;14:216–226. doi: 10.1097/00002508-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Cepeda MS, Carr DB, Lau J. Local anesthetic sympathetic blockade for complex regional pain syndrome. Cochrane Database Syst Rev. 2005 doi: 10.1002/14651858.CD004598.pub2. CD004598. [DOI] [PubMed] [Google Scholar]
- 7.Dellemijn PL, Fields HL, Allen RR, McKay WR, Rowbotham MC. The interpretation of pain relief and sensory changes following sympathetic blockade. Brain. 1994;117:1475–1487. doi: 10.1093/brain/117.6.1475. [DOI] [PubMed] [Google Scholar]
- 8.Dick AM, Gabbott DA, Hardy PA. Plasma concentrations of bupivacaine following single needle lumbar sympathectomy using two volumes of 0.25% bupivacaine plain solution. Anaesthesia. 1996;51:750–751. doi: 10.1111/j.1365-2044.1996.tb07889.x. [DOI] [PubMed] [Google Scholar]
- 9.Erickson SJ, Hogan QH. CT-guided injection of the stellate ganglion: Description of technique and efficacy of sympathetic blockade. Radiology. 1993;188:707–709. doi: 10.1148/radiology.188.3.8351337. [DOI] [PubMed] [Google Scholar]
- 10.Hogan QH, Erickson SJ, Abram SE. Computerized tomography-guided stellate ganglion blockade. Anesthesiology. 1992;77:596–599. doi: 10.1097/00000542-199209000-00030. [DOI] [PubMed] [Google Scholar]
- 11.Wallace MS, Ridgeway BM, Leung AY, Gerayli A, Yaksh TL. Concentration-effect relationship of intravenous lidocaine on the allodynia of complex regional pain syndrome types I and II. Anesthesiology. 2000;92:75–83. doi: 10.1097/00000542-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Lewis DW, Winner P, Wasiewski W. The placebo responder rate in children and adolescents. Headache. 2005;45:232–239. doi: 10.1111/j.1526-4610.2005.05050.x. [DOI] [PubMed] [Google Scholar]
- 13.Stanton-Hicks M, Janig W, Hassenbusch S, Haddox JD, Boas R, Wilson P. Reflex sympathetic dystrophy Changing concepts and taxonomy. Pain. 1995;63:127–133. doi: 10.1016/0304-3959(95)00110-E. [DOI] [PubMed] [Google Scholar]
- 14.Chelimsky TC, Low PA, Naessens JM, Wilson PR, Amadio PC, O'Brien PC. Value of autonomic testing in reflex sympathetic dystrophy. Mayo Clin Proc. 1995;70:1029–1040. doi: 10.4065/70.11.1029. [DOI] [PubMed] [Google Scholar]
- 15.Walsh JA, Glynn CJ, Cousins MJ, Basedow RW. Blood flow, sympathetic activity and pain relief following lumbar sympathetic blockade or surgical sympathectomy. Anaesth Intens Care. 1984;13:18–24. doi: 10.1177/0310057X8501300103. [DOI] [PubMed] [Google Scholar]
- 16.Meier PM, Berde CB, DiCanzio J, Zurakowski D, Sethna NF. Quantitative assessment of cutaneous thermal and vibration sensation and thermal pain detection thresholds in healthy children and adolescents. Muscle Nerve. 2001;24:1339–1345. doi: 10.1002/mus.1153. [DOI] [PubMed] [Google Scholar]
- 17.Sethna NF, Meier PM, Zurakowski D, Berde CB. Cutaneous sensory abnormalities in children and adolescents with complex regional pain syndromes. Pain. 2007;131:153–161. doi: 10.1016/j.pain.2006.12.028. [DOI] [PubMed] [Google Scholar]
- 18.McGrath PA, Seifert CE, Speechley KN, Booth JC, Stitt L, Gibson MC. A new analogue scale for assessing children's pain: An initial validation study. Pain. 1996;64:435–443. doi: 10.1016/0304-3959(95)00171-9. [DOI] [PubMed] [Google Scholar]
- 19.Wallenstein SL, Heidrich G, 3rd, Kaiko R, Houde RW. Clinical evaluation of mild analgesics: The measurement of clinical pain. Br J Clin Pharmacol. 1980;10:319–327. doi: 10.1111/j.1365-2125.1980.tb01816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan AW, MacFarlane IA, Bowsher D, Campbell JA. Weighted needle pinprick sensory thresholds: A simple test of sensory function in diabetic peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1992;55:56–59. doi: 10.1136/jnnp.55.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sethna NF, Liu M, Gracely R, Bennett GJ, Max MB. Analgesic and cognitive effects of intravenous ketamine-alfentanil combinations versus either drug alone after intradermal capsaicin in normal subjects. Anesth Analg. 1998;86:1250–1256. doi: 10.1097/00000539-199806000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Ziegler EA, Magerl W, Meyer RA, Treede RD. Secondary hyperalgesia to punctate mechanical stimuli. Central sensitization to A-fibre nociceptor input. Brain. 1999;122:2245–2257. doi: 10.1093/brain/122.12.2245. [DOI] [PubMed] [Google Scholar]
- 23.Rosner B. 6th Edition. Belmont CA: Duxbury Press; 2006. Fundamentals of Biostatistics; pp. 359–384. [Google Scholar]
- 24.Senn S. 2nd Edition. Chichester, England: John Wiley and Sons; 2007. Cross-over trials Statistical Issues in Drug Development; pp. 273–285. [Google Scholar]
- 25.Muller K, LaVange LM, Landesman Ramey S, Ramey CT. Power calculations for general linear multivariate models including repeated measures application. J Am Stat Assoc. 1992;87:1209–1226. doi: 10.1080/01621459.1992.10476281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raja SN, Treede RD, Davis KD, Campbell JN. Systemic alpha-adrenergic blockade with phentolamine: A diagnostic test for sympathetically maintained pain. Anesthesiology. 1991;74:691–698. doi: 10.1097/00000542-199104000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Treede RD, Davis KD, Campbell JN, Raja SN. The plasticity of cutaneous hyperalgesia during sympathetic ganglion blockade in patients with neuropathic pain. Brain. 1992;115:607–621. doi: 10.1093/brain/115.2.607. [DOI] [PubMed] [Google Scholar]
- 28.Benzon HT, Linde HW, Hawes DD, Brunner EA. Stellate ganglion block using physiologic saline solution. Anesthesiology. 1980;52:511–512. doi: 10.1097/00000542-198006000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Boas RA, Covino BG, Shahnarian A. Analgesic responses to i.v. lignocaine. Br J Anaesth. 1982;54:501–505. doi: 10.1093/bja/54.5.501. [DOI] [PubMed] [Google Scholar]
- 30.Devor M, Wall PD, Catalan N. Systemic lidocaine silences ectopic neuroma and DRG discharge without blocking nerve conduction. Pain. 1992;48:261–268. doi: 10.1016/0304-3959(92)90067-L. [DOI] [PubMed] [Google Scholar]
- 31.Tanelian DL, MacIver MB. Analgesic concentrations of lidocaine suppress tonic A-delta and C fiber discharges produced by acute injury. Anesthesiology. 1991;74:934–936. doi: 10.1097/00000542-199105000-00020. [DOI] [PubMed] [Google Scholar]
- 32.Wallace MS, Dyck JB, Rossi SS, Yaksh TL. Computer-controlled lidocaine infusion for the evaluation of neuropathic pain after peripheral nerve injury. Pain. 1996;66:69–77. doi: 10.1016/0304-3959(96)02980-6. [DOI] [PubMed] [Google Scholar]
- 33.Finholt DA, Stirt JA, DiFazio CA, Moscicki JC. Lidocaine pharmacokinetics in children during general anesthesia. Anesth Analg. 1986;65:279–282. [PubMed] [Google Scholar]
- 34.Galer BS, Miller KV, Rowbotham MC. Response to intravenous lidocaine infusion differs based on clinical diagnosis and site of nervous system injury. Neurology. 1993;43:1233–1235. doi: 10.1212/wnl.43.6.1233. [DOI] [PubMed] [Google Scholar]
- 35.Lund I, Lundeberg T, Sandberg L, Budh CN, Kowalski J, Svensson E. Lack of interchangeability between visual analogue and verbal rating pain scales: A cross sectional description of pain etiology groups. BMC Med Res Methodol. 2005;5:31. doi: 10.1186/1471-2288-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimeters? Pain. 1997;72:95–97. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 37.Schmid MR, Kissling RO, Curt A, Jaschko G, Hodler J. Sympathetic skin response: Monitoring of CT-guided lumbar sympathetic blocks. Radiology. 2006;241:595–602. doi: 10.1148/radiol.2412051229. [DOI] [PubMed] [Google Scholar]
- 38.Wallace MS, Laitin S, Licht D, Yaksh TL. Concentration-effect relations for intravenous lidocaine infusions in human volunteers: Effects on acute sensory thresholds and capsaicin-evoked hyperpathia. Anesthesiology. 1997;86:1262–1272. doi: 10.1097/00000542-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Tran KM, Frank SM, Raja SN, El-Rahmany HK, Kim LJ, Vu B. Lumbar sympathetic block for sympathetically maintained pain: Changes in cutaneous temperatures and pain perception. Anesth Analg. 2000;90:1396–1401. doi: 10.1097/00000539-200006000-00025. [DOI] [PubMed] [Google Scholar]
- 40.Blumberg H, Hoffmann U, Mohadjer M, Scheremet R. Sympathetic nervous system and pain: A clinical reappraisal. Behav Brain Sci. 1997;20:426–434. doi: 10.1017/s0140525x97271487. [DOI] [PubMed] [Google Scholar]
- 41.Gradl G, Schurmann M. Sympathetic dysfunction as a temporary phenomenon in acute posttraumatic CRPS I. Clin Auton Res. 2005;15:29–34. doi: 10.1007/s10286-005-0237-z. [DOI] [PubMed] [Google Scholar]