Abstract
To examine the fracture pattern in older women whose bone mineral density (BMD) T-score criteria for osteoporosis at hip and spine disagree, hip and spine BMD were measured in Study of Osteoporotic Fractures participants using dual energy x-ray absorptiometry (DXA). Hip osteoporosis was defined as T-score ≤-2.5 at femoral neck or total hip, and spine osteoporosis as T-score ≤-2.5 at lumbar spine. Incident clinical fractures were self-reported and centrally adjudicated. Incident radiographic spine fractures were defined morphometrically. Compared to women with osteoporosis at neither hip nor spine, those osteoporotic only at hip had a 3.0-fold age and weight-adjusted increased risk for hip fracture (95%CI 2.4-3.6), and smaller increases in risk of nonhip nonspine (HR=1.6), clinical spine (OR=2.2), and radiographic spine fractures (OR=1.5). Women osteoporotic only at spine had a 2.8-fold increased odds of radiographic spine fracture (95%CI 2.1-3.8), and smaller increases in risk of clinical spine (OR=1.4), nonhip nonspine (HR=1.6), and hip fractures (HR=1.2). Discordant BMD results predict different fracture patterns. DXA fracture risk estimation in these patients should be site-specific. Women osteoporotic only at spine would not have been identified from hip BMD measurement alone, and may have a sufficiently high fracture risk to warrant preventive treatment.
Keywords: Osteoporosis, bone density, fractures, prospective studies, DXA
Introduction
Bone mineral density (BMD) is well established as a predictor of future fracture risk. Decreased BMD at the proximal femur, lumbar spine, radius, and calcaneus all predict increased risk of incident hip, spine, and nonhip nonspine fractures.(1,2) In 1994, the World Health Organization (WHO) published BMD-based criteria for classifying Caucasian postmenopausal women as osteoporotic, osteopenic (low bone mass) or normal. For epidemiologic purposes, osteoporosis was defined as BMD at least 2.5 standard deviations (SD) below the young adult mean (T-score ≤-2.5).(3) Low bone mass has been defined as BMD more than 1.0 but fewer than 2.5 SD below the young adult mean (T-score >-2.5 and <-1.0).(4)
Although these WHO criteria were not designed for individual clinical diagnosis of osteoporosis or for use in making treatment decisions, they have been widely utilized for these purposes. As T-score values from different skeletal sites often disagree, individual patients may be classified as having osteoporosis, low bone mass, or normal BMD depending on which skeletal site or sites are measured.(5,6,7,8)
Clinicians may resolve this labeling dilemma by following International Society for Clinical Densitometry (ISCD) and American Society for Bone and Mineral Research (ASBMR) recommendations to classify patients on the basis of the skeletal site (total hip, femoral neck, or lumbar spine) with the lowest T-score.(9,10,11) Alternatively, the International Osteoporosis Foundation (IOF) has stated that because spine BMD does not enhance fracture prediction (any osteoporotic, hip, or spine) once hip BMD is known, only hip BMD should be measured.(12) Implementation of the IOF position would eliminate the need to interpret discordant hip-spine BMD results. However, if patients with a T-score ≤-2.5 at spine alone are at high fracture risk, then the IOF approach could lead to under-treatment of these individuals. With this issue as yet unresolved, the clinician still faces the question of whether hip-spine BMD discordance is of clinical importance, in particular with respect to risk of future fractures.
Therefore, it is the aim of the present analyses to describe, in patients with BMD measures at both hip and spine, the patterns for incident hip, spine, and nonhip nonspine fractures in women with a T-score ≤-2.5 at the hip but not the spine, and in those with a T-score ≤-2.5 at the spine but not the hip.
Materials and Methods
Participants
The Study of Osteoporotic Fractures (SOF) is a prospective cohort study that enrolled 9704 community-dwelling women aged 65 years or older at baseline (1986-1988).(13) Participants were recruited primarily from population-based listings at four U.S. clinical sites: Baltimore, Maryland; Minneapolis, Minnesota; Portland, Oregon; and the Monongahela Valley, Pennsylvania. SOF exclusion criteria included an inability to walk without assistance from another person and a history of bilateral hip replacement. Written informed consent was obtained from all participants and the institutional review boards at all participating centers approved the study protocol.
Clinical Fracture Cohort
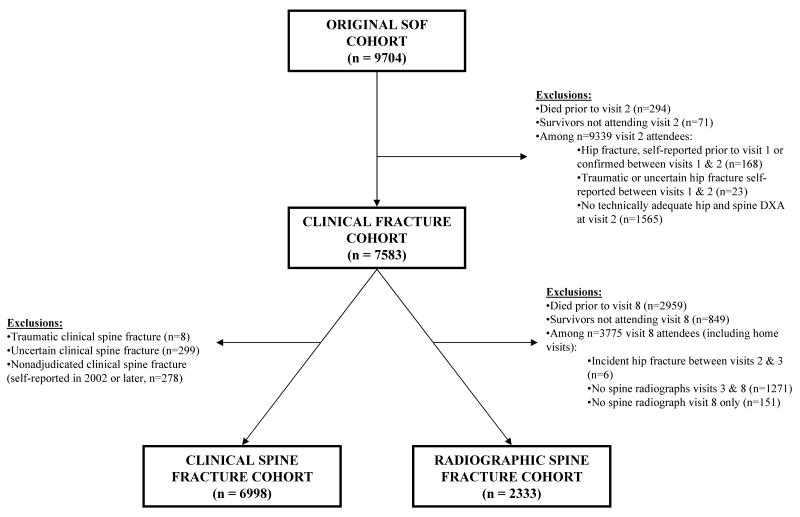
Between 1989 and 1990, 9339 women (99% of SOF survivors) attended a 2nd SOF study exam. Of these women, 7583 had no prior hip fracture and completed technically adequate hip and spine BMD measurements at this visit. These women were the subject of all subsequent analyses related to incident hip, and nonhip nonspine fractures (Clinical Fracture Cohort) (Figure 1).
FIGURE 1. Study Flow Diagram.
Clinical Spine Fracture Cohort
Among the 7583 women in the Clinical Fracture Cohort, clinical spine fracture analyses were performed in 6998, after exclusion of 585 women who had either traumatic, uncertain, or unadjudicated clinical spine fractures (Clinical Spine Fracture Cohort). (Figure 1) Uncertain fractures (n=299) were those for which no supporting medical records were available or for which, after review of medical records, adjudicators were uncertain that a vertebral fracture had occurred. SOF adjudication of self-reported clinical spine fractures was discontinued after 2001, after which all these self-reports were categorized as unadjudicated (n=278).
Radiographic Spine Fracture Cohort
Among the 7583 women in the Clinical Fracture Cohort, 3775 (84% of Clinical Fracture Cohort survivors) attended an 8th SOF study exam between 2002 and 2004. Of these women, 2333 had no history of hip fracture prior to the 3rd SOF exam and completed technically adequate spine radiographs at both the 3rd and 8th SOF exams. These women were the subject of all subsequent analyses related to incident radiographic spine fractures (Radiographic Spine Fracture Cohort) (Figure 1).
Measurement and Categorization of BMD
At the 2nd SOF exam, BMD (g/cm2) of the lumbar spine, total hip and hip subregions was measured in the anteroposterior (AP) projection using dual energy x-ray absorptiometry (DXA) (QDR 1000, Hologic, Inc., Waltham, MA) in all SOF participants. Based on measurements of research staff who visited all four clinical centers, the mean coefficients of variation between centers were 1.2% for the proximal femur and 1.5% for the lumbar spine.(14) At the time of the lumbar spine DXA readings, abnormal vertebrae and other vertebral artifacts were neither documented nor excluded from estimates of lumbar spine BMD.
Total hip and femoral neck BMD results were transformed to T-scores using a population-based white female reference database from the NHANES III study.(15) Lumbar spine BMD results were transformed to T-scores using a Hologic white female reference database. Based on their total hip and femoral neck T-scores, women were categorized as osteoporotic at the hip if either T-score was ≤-2.5, as osteopenic (low bone mass) at the hip if both were >-2.5 but at least one was <-1.0, and as normal at the hip if both were ≥-1.0. Based on their lumbar spine T-score, women were categorized as osteoporotic at the spine if the spine T-score was ≤-2.5, low bone mass at the spine if the T-score was >-2.5 but <-1.0, and normal at the spine if it was ≥-1.0.
Participants then were categorized with respect to osteoporosis as: (1) osteoporotic only at hip, (2) osteoporotic only at spine, (3) osteoporotic at both sites, or (4) osteoporotic at neither site. Secondarily, participants who were osteoporotic at the hip were subcategorized based on their spine BMD category into those who also were osteoporotic at spine (i.e. concordant with spine), those with low bone mass at the spine (i.e. minor discordance with spine), and those with normal BMD at the spine (i.e. major discordance with spine). Similarly, participants who were osteoporotic at the spine were subcategorized based on their hip BMD category into those who also were osteoporotic at the hip (i.e. concordant with hip), those with low bone mass at the hip (i.e. minor discordance with hip), and those with normal BMD at the hip (i.e. major discordance with hip).
Identification of Clinical Fractures
Incident hip, nonhip nonspine, and clinical spine fractures were identified by self-report and confirmed by review of radiological reports. SOF participants were contacted by mail or telephone and asked about incident fractures every four months; follow-up was >95% complete. Study adjudication of clinical spine fractures was discontinued after 2001. A detailed description of the implementation and accuracy of SOF fracture data was previously reported.(16)
Identification of Radiographic Spine Fractures
Incident radiographic spine fractures were defined morphometrically by comparison of spine radiographs completed at the 3rd and 8th SOF exams (mean interval between exams 11.3 years, range 10.0-13.2). Incident fractures were defined by a decrease in vertebral height at any vertebral level of ≥20% and at least 4 mm. Prevalent vertebral deformities were defined using modified Melton/Eastell vertebral height ratio criteria.(17,18) Three heights were calculated for each vertebral body: anterior (Ha), middle (Hm), and posterior (Hp), and a vertebral body was considered deformed if any of the following height ratios exceeded 3 SD below the mean value for that vertebral level: Ha/Hp, Hm/Hp, Ha/Ha+1, Hp/Hp+1, Ha/Ha-1 or Hp/Hp-1.(19)
Statistical Analyses
Analyses of differences between participants in the four osteoporosis categories (i.e. osteoporotic only at hip, osteoporotic only at spine, osteoporotic at both sites, osteoporotic at neither site) were assessed using Chi-square tests for dichotomous variables and ANOVA and Kruskal-Wallis tests for continuous variables.
To characterize the pattern of site-specific fractures in participants in the four osteoporosis categories, age-adjusted rates and 95% confidence intervals were estimated for incident hip fractures and incident nonhip nonspine fractures within these categories of participants in the Clinical Fracture Cohort, but not for incident spine fractures in either cohort as the dates of spine fractures were unknown.
To estimate the risk of incident fractures among participants in the four osteoporosis categories, age- and weight-adjusted Cox proportional hazards regression analyses were employed to examine the hazard ratios (HR) and 95% confidence intervals for incident hip fractures and incident nonhip nonspine fractures within the Clinical Fracture Cohort. Risks for fractures were estimated in women who were osteoporotic only at hip, osteoporotic only at spine, or osteoporotic at both sites, using women with osteoporosis at neither site as the referent group. Because time to incident spine fractures could not be determined, age- and weight-adjusted logistic regression analyses were employed to examine the odds ratio (OR) and 95% confidence intervals for incident clinical spine fractures within the Clinical Fracture Cohort and for incident radiographic spine fractures within the Radiographic Spine Fracture Cohort. As in the proportional hazards models, women with osteoporosis at neither site were used as the reference group.
To explore whether incident fracture risk in women osteoporotic only at spine was explained by concomitantly low hip BMD, women with osteoporosis only at spine were stratified into their total hip T-score tertiles, and incident fracture risk within each tertile was compared to that in women with osteoporosis at neither site. A similar approach was taken to explore whether differences in incident fracture risk in women osteoporotic at both hip and spine compared to those osteoporotic at neither site or those osteoporotic only at hip were explained by between-group differences in hip BMD. First, women osteoporotic at both hip and spine were stratified into their total hip T-score tertiles. Then, incident fracture risk within each tertile was compared to that in women with osteoporosis at neither site and separately to that in women with osteoporosis only at hip.
To explore whether the magnitude of BMD discordance between hip and spine sites impacted subsequent risk of fracture, women with hip osteoporosis were stratified into those with normal spine BMD, low bone mass at the spine, or osteoporosis at the spine. Risk of incident fracture within each of these groups was compared to that in women with osteoporosis at neither site. Similarly, women with spine osteoporosis were stratified into those with normal hip BMD, low bone mass at the hip, or osteoporosis at the hip. Risk of incident fracture within each of these groups was compared to that in women with osteoporosis at neither site.
To explore the impact of prevalent baseline vertebral deformity status on the association between discordance status and subsequent risk of radiographic spine fractures, incident fracture risks were estimated in subgroups of the Radiographic Spine Fracture Cohort defined according to presence or absence of prevalent vertebral deformity at the 3rd SOF exam.
Finally, to explore whether associations of BMD discordance with risk of clinical spine fracture might be impacted by imprecision in the clinical spine fracture adjudication process, we performed a sensitivity analysis assuming that all self-reported clinical spine fractures adjudicated as “uncertain” represented true spine fractures.
All analyses were performed with SAS, version 9.1 (SAS Institute, Inc., Cary, NC).
Results
Site-Specific Osteoporosis Status
Within the 7583 participants in the Clinical Fracture Cohort (Table 1), 10% were osteoporotic only at hip, 16% were osteoporotic only at spine, 17% were osteoporotic at both hip and spine, and 58% were osteoporotic at neither site. Among the 2041 (27%) participants with osteoporosis at the hip, 1314 (64%) were also osteoporotic at the spine (i.e. concordant with spine), 602 (29%) had low bone mass at the spine (i.e. minor discordance with spine), and only 125 (6%) had normal spine BMD (i.e. major discordance with spine). Among the 2493 (33%) participants with osteoporosis at the spine, 1314 (53%) were osteoporotic at the hip (i.e. concordant with hip), 1139 (46%) had low bone mass at the hip (i.e. minor discordance with hip), and only 40 (2%) had normal hip BMD (i.e. major discordance with hip). The distribution of participants among these categories was similar within the Radiographic Spine Fracture Cohort (data not shown).
Table 1. Participant Visit 2 Characteristics by Cohort and Osteoporosis Status*.
| Characteristic | Osteoporosis Status | ||||
|---|---|---|---|---|---|
| Clinical Fracture Cohort (n=7583) | Hip only | LS only | Hip + LS | Neither | P-value |
| N (%) | 727(9.6) | 1179 (15.6) | 1314 (17.3) | 4363 (57.5) | |
| Mean age, y (SD) | 75.8 (5.7) | 72.6 (4.3) | 75.0 (5.6) | 72.7 (4.6) | <.001 |
| Mean weight, kg (SD) | 62.1 (10.4) | 64.3 (10.5) | 57.9 (9.2) | 70.5 (12.4) | <.001 |
| BMD, g/cm2 (SD) | |||||
| Femoral neck | .54 (.04) | .65 (.06) | .53 (.05) | .71 (.09) | <.001 |
| Total hip | .65 (.07) | .74 (.06) | .60 (.07) | .83 (.11) | <.001 |
| Lumbar spine | .87 (.09) | .70 (.05) | .66 (.07) | .96 (.14) | <.001 |
| BMD, T-score (SD) | |||||
| Femoral neck | -2.80 (.39) | -1.83 (.53) | -2.91 (.45) | -1.26 (.85) | <.001 |
| Total hip | -2.40 (.56) | -1.66 (.52) | -2.77 (.56) | -0.90 (.87) | <.001 |
| Lumbar spine | -1.62 (.81) | -3.12 (.48) | -3.50 (.63) | -0.82 (1.23) | <.001 |
| Radiographic Spine Fracture Cohort (n=2333) | Hip only | LS only | Hip + LS | Neither | P-value |
| N (%) | 153 (6.6) | 402 (17.2) | 306 (13.1) | 1472 (63.1) | |
| Mean age, y (SD) | 72.2 (3.8) | 70.9 (3.0) | 71.8 (3.5) | 70.8 (3.2) | <.001 |
| Mean weight, kg (SD) | 63.6 (9.3) | 64.4 (10.6) | 58.9 (9.0) | 70.6 (12.1) | <.001 |
| Prevalent vertebral deformity, n (%)† | 22.2 | 22.6 | 32.7 | 13.9 | <.001 |
| BMD, g/cm2 (SD) | |||||
| Femoral neck | .54 (.04) | .65 (.06) | .53 (.04) | .72 (.09) | <.001 |
| Total hip | .66 (.07) | .75 (.06) | .62 (.06) | .84 (.10) | <.001 |
| Lumbar spine | .86 (.08) | .70 (.05) | .67 (.07) | .95 (.13) | <.001 |
| BMD, T-score (SD) | |||||
| Femoral neck | -2.75 (.36) | -1.77 (.56) | -2.84 (.40) | -1.19 (.83) | <.001 |
| Total hip | -2.29 (.58) | -1.60 (.53) | -2.66 (.50) | -0.82 (.86) | <.001 |
| Lumbar spine | -1.70 (.71) | -3.11 (.47) | -3.45 (.60) | -0.90 (1.18) | <.001 |
Osteoporosis status categorized as osteoporotic only at hip (Hip only), only at lumbar spine (LS only), both sites (Hip + LS), or at neither site.
Presence of prevalent vertebral deformity determined by spinal radiograph at 3rd SOF exam.
Participant Characteristics
In both the Clinical Fracture Cohort and the Radiographic Spine Fracture Cohort, there were significant differences in age, weight and site-specific BMD between the four categories of participants defined by osteoporosis status. For both cohorts, those with osteoporosis at neither site generally appeared younger and weighed more, those osteoporotic at both hip and spine were older and lighter, those osteoporotic only at hip were older but of intermediate weight, and those osteoporotic only at spine were younger and of intermediate weight (Table 1). Compared to participants with osteoporosis at neither site, those osteoporotic only at spine appeared to have modestly lower BMD at both femoral neck and total hip, while those osteoporotic only at hip appeared to have modestly lower spine BMD. When compared to all participants in the Clinical Fracture Cohort, the subset comprising the Radiographic Spine Fracture Cohort appeared younger, but was similar with respect to weight and BMD.
Incident Fractures
Overall
Among the 7583 participants in the Clinical Fracture Cohort, during a mean follow-up period of 11.8 years (range 13 days to 16.9 years), 908 women (12%) experienced an incident hip fracture and 2222 (29%) experienced an incident nonhip nonspine fracture. Incident clinical spine fractures were confirmed in 181 women (3%). Within the 2333 participants in the Radiographic Spine Fracture Cohort, during a mean interval between initial and follow-up spine x-rays of 11.3 years (range 10.0 to 13.2 years), 356 women (15%) experienced an incident radiographic spine fracture.
Women with Osteoporosis at Hip Only
Compared to women with osteoporosis at neither hip nor spine, after adjustment for age and weight, those osteoporotic only at hip had a 3.0-fold increased risk of incident hip fractures (95%CI 2.4-3.6), 1.6-fold increased risk of incident nonhip nonspine fractures (95%CI 1.4-1.8), 2.2-fold increased odds of clinical spine fractures (95%CI 1.3-3.8), and 1.5-fold increased odds of incident radiographic spine fractures (95%CI 0.9-2.4) (Table 2).
Table 2. Risk of Incident Fractures by Osteoporosis Status.
| Osteoporosis Status* | ||||
|---|---|---|---|---|
| Hip only | LS only | Hip + LS | Neither | |
| Incident Hip Fractures | ||||
| n/N (%) | 172/727 (23.7) | 116/1179 (9.8) | 284/1314 (21.6) | 336/4363 (7.7) |
| Rate, n/1000 p-yr (95% CI)† | 20.6 (17.2-24.0) | 8.6 (6.9-10.2) | 18.4 (16.1-20.6) | 6.6 (5.9-7.3) |
| Risk, HR (95% CI)‡ | 3.0 (2.4-3.6) | 1.2 (1.0-1.5) | 2.7 (2.2-3.2) | 1.0 (referent) |
| Incident Nonhip Nonspine Fractures | ||||
| n/N (%) | 247/727 (34.0) | 396/1179 (33.6) | 491/1314 (37.4) | 1088/4363 (24.9) |
| Rate, n/1000 p-yr (95% CI)† | 39.2 (33.7-44.8) | 40.9 (36.6-45.2) | 51.2 (46.1-56.2) | 26.1 (24.5-27.6) |
| Risk, HR (95% CI)‡ | 1.6 (1.4-1.8) | 1.6 (1.4-1.8) | 2.0 (1.8-2.2) | 1.0 (referent) |
| Incident Clinical Spine Fractures§** | ||||
| n/N (%) | 19/673 (2.8) | 19/1040 (1.8) | 84/1115 (7.5) | 59/4170 (1.4) |
| Risk, OR (95% CI)‡ | 2.2 (1.3-3.8) | 1.4 (0.8-2.4) | 6.5 (4.4-9.6) | 1.0 (referent) |
| Incident Radiographic Spine Fractures§ | ||||
| n/N (%) | 23/153 (15.0) | 94/402 (23.4) | 94 / 306 (30.7) | 145 / 1472 (9.9) |
| Risk, OR (95% CI)†† | 1.5 (0.9-2.4) | 2.8 (2.1-3.8) | 4.0 (2.9-5.5) | 1.0 (referent) |
Osteoporosis status categorized as osteoporotic only at hip (Hip only), only at lumbar spine (LS only), both sites (Hip + LS), or at neither site.
P-yr = person-years; results adjusted for age at 2nd SOF exam.
Results adjusted for age and weight at 2nd SOF exam.
Spine fracture rates not available because dates of spine fractures were unknown.
Results adjusted for age and weight at 3rd SOF exam.
To explore whether these results were explained by between-group differences in spine BMD, women with osteoporosis only at hip were stratified according to their spine BMD osteoporosis category. Relative to nonosteoporotic women, the increased risk of incident hip, nonhip nonspine, and radiographic spine fractures in those osteoporotic only at the hip appeared similar in magnitude whether they had normal spine BMD or low bone mass at the spine (data not shown). Similar analyses were limited for incident clinical spine fractures by the relatively low number of these fractures within each spine BMD stratum of subjects osteoporotic only at hip.
Women with Osteoporosis at Spine Only
Compared to women with osteoporosis at neither hip nor spine, after adjustment for age and weight, those osteoporotic only at spine had a 1.2-fold increase in risk of incident hip fracture (95%CI 1.0-1.5), a 1.6-fold increase in risk of incident nonhip nonspine fracture (95%CI 1.4-1.8), a 1.4-fold increase in odds of clinical spine fracture (95%CI 0.8-2.4), and a 2.8-fold increased odds of incident radiographic spine fracture (95%CI 2.1-3.8) (Table 2).
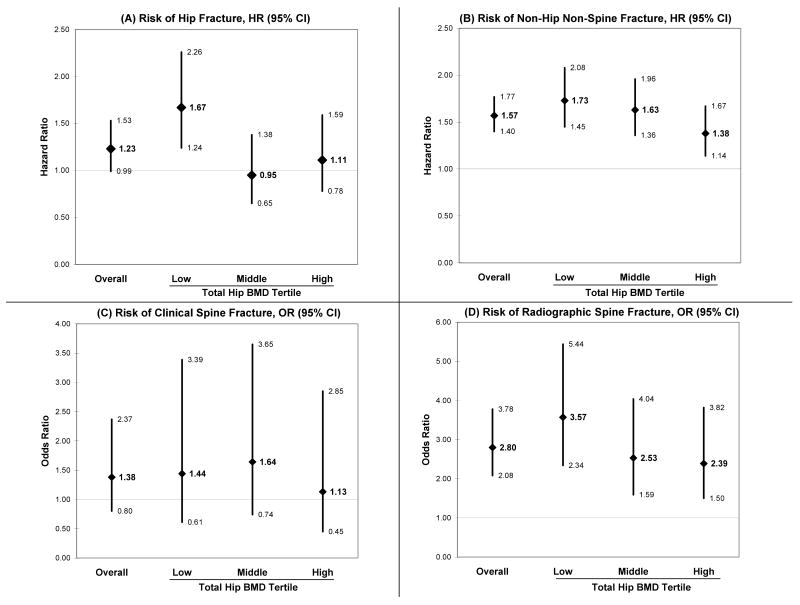
To explore whether these results were explained by between-group differences in hip BMD, women with osteoporosis only at spine were stratified according to their total hip T-scores or their hip BMD osteoporosis category. Relative to women with osteoporosis at neither hip nor spine, age and weight-adjusted hip fracture risk in women with osteoporosis only at spine was increased only in those in the lowest total hip BMD tertile (HR=1.7, 95%CI 1.2-2.3) (Figure 2). Similarly, women osteoporotic only at the spine had an increased risk of incident hip fracture if they had low hip bone mass (HR=1.3, 95%CI 1.0-1.6), but not if they had normal hip BMD. By contrast, compared to women without osteoporosis, those with osteoporosis only at spine had a significantly increased risk of nonhip nonspine fracture in all hip BMD categories. The magnitude of increased risk appeared similar across total hip BMD tertiles (Figure 2) as well as between women categorized with normal hip BMD and those with low hip bone mass (data not shown). In further comparison to women with osteoporosis at neither hip nor spine, all total hip BMD tertiles of women with osteoporosis only at spine had a significantly increased odds of incident radiographic spine fracture and a modestly though not statistically significantly increased odds of clinical spine fracture (Figure 2).
FIGURE 2. Risk of Incident Fractures in Women Osteoporotic Only at Spine, Overall and by Total Hip BMD Tertiles*†.
*All results adjusted for age and weight at Visit 2
†Within women osteoporotic only at spine, total hip BMD tertiles were as follows: low <0.706 g/cm2 (T-score < -1.934); middle 0.706 to 0.757 g/cm2 (T-score -1.508 to -1.934); high >0.757 g/cm2 (T-score > -1.508)
Among women with osteoporosis at spine only, those with a baseline vertebral deformity more frequently had incident radiographic spine fractures than those without a baseline vertebral deformity (41% vs. 18%). However, the increase in odds of incident radiographic spine fracture conferred by being osteoporotic at spine only vs. osteoporotic at neither hip nor spine appeared attenuated in women with baseline vertebral deformities (OR=2.1, 95%CI 1.2-3.7) versus those with no baseline vertebral deformity (OR=2.8, 95%CI 1.9-4.0).
Women with Osteoporosis at Both Hip and Spine
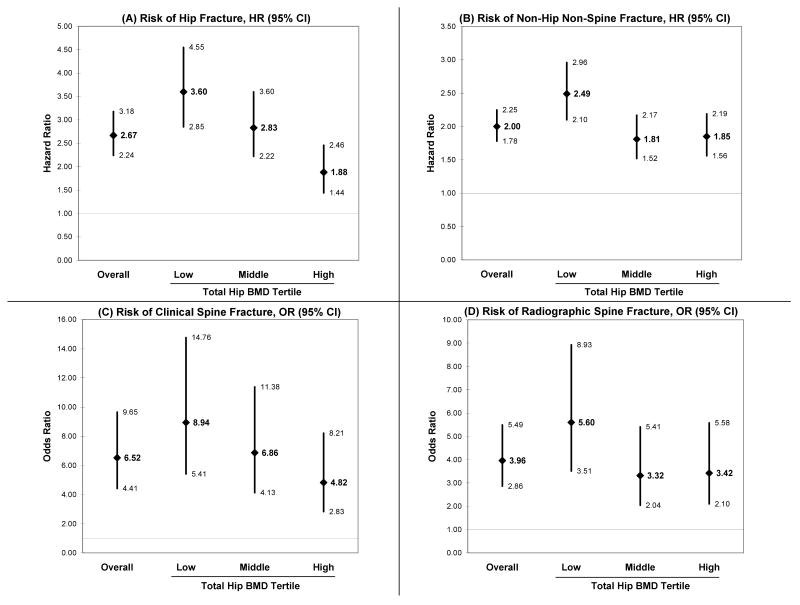
Compared to women with osteoporosis at neither hip nor spine, after adjustment for age and weight, those osteoporotic at both hip and spine had a 2.7-fold increased risk of incident hip fracture (95%CI 2.2-3.2) (Table 2), a 2.0-fold increased risk of incident nonhip nonspine fracture (95%CI 1.8-2.3), a 6.5-fold increased odds of clinical spine fracture (95%CI 4.4-9.6), and a 4.0-fold increased odds of incident radiographic spine fracture (95%CI 2.9-5.5).
To explore whether these results were explained by between-group differences in hip BMD, women with osteoporosis at both hip and spine were stratified according to their total hip T-scores. Compared to women with osteoporosis at neither hip nor spine, the risk for hip fracture within those osteoporotic at both hip and spine increased according to the severity of decreased hip BMD (Figure 2). Compared to women without osteoporosis, risk of nonhip nonspine fracture in women osteoporotic at both hip and spine was significantly more elevated among women in the lowest total hip BMD tertile than in those in the upper tertiles (p<0.01 for both comparisons) (Figure 2). Similar analyses suggested that within women osteoporotic at both hip and spine, odds of incident radiographic and clinical spine fractures were substantially increased by severity of decreased hip BMD, though these between-tertile differences were only borderline statistically significant (Figure 2).
When compared to women osteoporotic only at hip, those osteoporotic at both hip and spine were not at greater risk of hip fracture, and were at greater risk of nonhip nonspine fracture only in the lowest total hip BMD tertile. However, they had a significantly greater odds of clinical and radiographic spine fractures regardless of how severely osteoporotic they were at the hip (p<0.05 for all comparisons).
Additional Analyses
In sensitivity analyses in which self-reported clinical spine fractures adjudicated as “uncertain” were considered true clinical spine fractures, the association of osteoporosis only at spine with clinical spine fractures appeared to be strengthened (OR=2.0, 95%CI 1.5-2.7 vs. OR=1.4, 0.8-2.4 in analyses excluding “uncertain” clinical spine fractures). However, the estimated risk of clinical spine fractures conferred by osteoporosis at hip only or by osteoporosis at both hip and spine appeared modestly attenuated (OR=1.8, 95%CI 1.3-2.6 vs. OR=2.2, 1.3-3.8 for osteoporosis only at hip; and OR=5.2, 4.1-6.7 vs. OR=6.5, 4.4-9.6 for osteoporosis at hip and spine).
Discussion
In this large prospective study of postmenopausal women, discordant hip-spine BMD results were common and predicted differences in the pattern of skeletal site-specific fracture risk. Among study participants who met T-score criteria for osteoporosis at either hip or spine, nearly 25% were osteoporotic only at hip and more than 40% were osteoporotic only at spine. Of those women with discordant hip-spine BMD results, most had low bone mass and fewer than 10% had normal BMD at the nonosteoporotic site. Women with osteoporosis at the spine but not the hip had a substantially increased risk of spine fracture, but only modest increases in risk of hip and nonhip nonspine fracture. In contrast, women with osteoporosis at the hip but not the spine had a substantially increased risk of hip fracture, but more modest increases in risk of spine and nonhip nonspine fracture.
In women with osteoporosis only at the spine, increased risk of incident hip fracture appeared attributable to lower hip BMD even while hip BMD did not meet osteoporotic criteria. However, the increased risk for nonhip nonspine and radiographic spine fractures observed in these women was less clearly associated with worse hip BMD within the nonosteoporotic range. In women with osteoporosis only at the hip, risk of all fracture types did not appear to differ significantly based on whether these women had normal spine BMD or low bone mass at the spine, suggesting that severity of nonosteoporotic levels of spine BMD do not add predictive value in these patients.
In women with osteoporosis at both hip and spine, the risk of each fracture type compared to women without osteoporosis was substantially increased by severity of decreased hip BMD. When women with osteoporosis at both hip and spine were compared to women with osteoporosis only at hip, the combined osteoporotic group had no excess risk of hip or nonhip nonspine fractures, but risk of spine fractures was increased in all hip BMD severity categories examined. These results suggest that results from spine BMD may enhance prediction of spine fractures even in women known to be osteoporotic at the hip, no matter the severity of hip osteoporosis.
Our results are consistent with those reported in previous studies in showing limited within-subject agreement of hip vs. spine BMD for osteoporosis classification and in demonstrating an increase in sensitivity for diagnosis of osteoporosis when BMD is measured at multiple sites.(20,20,21) Also in accord with earlier studies, our results show that an increase in the number of osteoporotic sites predicts a higher risk of incident fractures.(21,22,20) For example, in one large clinical referral population, the age-adjusted risk of any osteoporotic fracture ascertained from administrative records increased as the number of osteoporotic sites (total hip, femoral neck, trochanter, or lumbar spine) increased.(20) This association was eliminated by adjustment for total hip BMD as a continuous risk factor. An increased number of osteoporotic sites also separately increased age-adjusted risks for hip, spine, or miscellaneous fractures (i.e. not involving hip, spine, forearm or proximal humerus), with only the increase in risk for spine fractures not eliminated by adjustment for total hip BMD. However, this earlier study did not report incident fracture risks according to which specific sites were osteoporotic, particularly for patients osteoporotic at spine but not hip and at hip but not spine, which was the focus of the current study.
Our findings have important clinical implications. Our study suggests that measurement of spine BMD adds clinical value to hip BMD measurement. For example, women meeting osteoporosis criteria only at the spine would not be identified as osteoporotic based on hip BMD measurement alone and may have a sufficiently high risk of fractures, particularly of spine fracture, to warrant preventive treatment. Further, our finding that patients' patterns of osteoporotic sites predict their site-specific risk of future fractures may allow clinicians reading DXA results to provide patients more individualized prognoses.
The current study has several important strengths. Among these is the long follow-up time and complete ascertainment of incident fractures, including far more total fractures and hip fractures than either the recent meta-analysis of cohort studies(22) or the clinical administrative database study that also examined BMD measurement at multiple sites for prediction of fractures.(20)
These analyses also have several limitations. Abnormal vertebrae and the effects of aortic calcification could not be excluded from measurements of baseline spine BMD. This is likely to have modestly overestimated spine BMD and very slightly underestimated the association between lower spine BMD and increased fracture risk.(23) Second, because the relationship between BMD and fracture risk is continuous,(2) use of categorical T-score criteria to define between-site BMD discordance is arbitrary. These analyses employed T-score criteria in current clinical use to examine the future fracture implications in patients with known discordant hip-spine BMD results. They did not attempt to identify the optimum BMD cutpoints at hip and spine to maximize sensitivity and specificity for prediction of incident fractures, and did not directly compare whether, at a population level, fractures are best predicted by measurement of hip BMD alone, spine BMD alone, or measurement of BMD at both sites, such as with the use of the minimum T-score. Third, because most of the women osteoporotic only at spine had low bone mass at the hip, detection of many could have been accomplished by using a less stringent hip T-score diagnostic criterion. Fourth, because incident radiographic spine fractures could only be identified in participants who attended the eighth SOF study visit, these may not have been representative of all incident radiographic spine fractures and this may have impacted their observed association with hip-spine BMD discordance. Fifth, although hip-spine BMD discordance may be highly prevalent in younger postmenopausal women, because SOF participants were aged 65 years or older, the impact of BMD site discordance on risk of future fractures in younger women cannot be determined from these data. Sixth, some true clinical spine fractures may have been adjudicated as uncertain. Sensitivity analyses considering all self-reported clinical spine fractures adjudicated as uncertain to be true clinical spine fractures suggested that women osteoporotic only at spine may have a greater risk for clinical spine fractures than originally estimated. Finally, because study participants were community-dwelling, largely healthy Caucasian women, study findings also may not be generalizable to institutionalized individuals, to men, or to nonwhite women.
In conclusion, we found that older women commonly had discordant hip-spine BMD results and that these predicted different patterns of fracture risk. Women meeting osteoporosis criteria only at hip were at greatest risk for incident hip fracture, with smaller elevations in risk for other fracture types. Women with osteoporosis only at spine were at increased risk for radiographic spine and nonhip nonspine fractures. Women meeting osteoporosis criteria only at spine would not have been identified solely from hip BMD measurement, and may benefit from preventive treatment.
FIGURE 3. Risk of Incident Fractures in Women Osteoporotic at Both Hip and Spine, Overall and By Total Hip BMD Tertiles*†.
*All results adjusted for age and weight at Visit 2
†Within women osteoporotic at both hip and spine, total hip BMD tertiles were as follows: low <0.582 g/cm2 (T-score < -2.958); middle 0.582 to 0.633 g/cm2 (T-score -2.524 to -2.958); high >0.633 g/cm2 (T-score > -2.524)
Acknowledgments
A portion of the data in this manuscript was presented at the 2005 meeting of the American Society of Bone and Mineral Research. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Research Grant Support: H.A. Fink (None); S.L. Harrison (None); B.C. Taylor (None); K.E. Ensrud (Bionovo, Inc.); J.T. Schousboe, (Hologic, Inc); M.A. Kuskowski (None); K.L. Stone (None); S.R. Cummings (Amgen, Eli Lilly & Co., Novartis).
Footnotes
Funding Sources: National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), and the National Cancer Institute (NCI), under the following grant numbers: AG05394, AG05407, AR35582, AR35583, AR35584.
Potential Financial Conflicts of Interest: Honoraria: H.A. Fink (None); S.L. Harrison (None); B.C. Taylor (None); K.E. Ensrud (None); J. T. Schousboe (None); M.A. Kuskowski (None); K.L. Stone (None); S.R. Cummings (Novartis, Amgen, Pfizer Pharmaceuticals, Eli Lilly & Co., Merck).
Speaker's Bureau: H.A. Fink (None); S.L. Harrison (None); B.C. Taylor (None); K.E. Ensrud (None); J. T. Schousboe (None); M.A. Kuskowski (None); K.L. Stone (None); S.R. Cummings (None).
Author Contributions
Conception and design: H.A. Fink; S.R. Cummings; K.E. Ensrud.
Acquisition of participants and/or data: K.E. Ensrud; S.R. Cummings
Analysis and interpretation of the data: H.A. Fink; S.L. Harrison; B.C. Taylor; K.E. Ensrud; J.T. Schousboe; M.A. Kuskowski; K.L. Stone; S.R. Cummings.
Drafting of the article: H.A. Fink.
Critical revision of the article for important intellectual content: H.A. Fink; S.L. Harrison; B.C. Taylor; K.E. Ensrud; J.T. Schousboe; M.A. Kuskowski; K.L. Stone; S.R. Cummings.
Final approval of the article: H.A. Fink; S.L. Harrison; B.C. Taylor; K.E. Ensrud; J.T. Schousboe; M.A. Kuskowski; K.L. Stone; S.R. Cummings.
Sponsor's Role: The funding agencies played no role in the design, analysis and preparation of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Howard A. Fink, Email: howard.fink@va.gov.
Stephanie L. Harrison, Email: slitwack@psg.ucsf.edu.
Brent C. Taylor, Email: taylorbc@umn.edu.
Steven R. Cummings, Email: scummings@sfcc-cpmc.net.
John T. Schousboe, Email: schouj@parknicollet.com.
Michael A. Kuskowski, Email: mike@james.psych.umn.edu.
Katie L. Stone, Email: kstone@sfcc-cpmc.net.
Kristine E. Ensrud, Email: ensru001@umn.edu.
References
- 1.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: scientific review. JAMA. 2002;288:1889–1897. doi: 10.1001/jama.288.15.1889. [DOI] [PubMed] [Google Scholar]
- 3.Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. 1994;4:368–381. doi: 10.1007/BF01622200. [DOI] [PubMed] [Google Scholar]
- 4.Leslie WD, Adler RA, El Hajj FG, et al. Application of the 1994 WHO classification to populations other than postmenopausal Caucasian women: the 2005 ISCD Official Positions. J Clin Densitom. 2006;9:22–30. doi: 10.1016/j.jocd.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Varney LF, Parker RA, Vincelette A, Greenspan SL. Classification of osteoporosis and osteopenia in postmenopausal women is dependent on site-specific analysis. J Clin Densitom. 1999;2:275–283. doi: 10.1385/jcd:2:3:275. [DOI] [PubMed] [Google Scholar]
- 6.Woodson G. Dual X-ray absorptiometry T-score concordance and discordance between the hip and spine measurement sites. J Clin Densitom. 2000;3:319–324. doi: 10.1385/jcd:3:4:319. [DOI] [PubMed] [Google Scholar]
- 7.Arlot ME, Sornay-Rendu E, Garnero P, Vey-Marty B, Delmas PD. Apparent pre- and postmenopausal bone loss evaluated by DXA at different skeletal sites in women: the OFELY cohort. J Bone Miner Res. 1997;12:683–690. doi: 10.1359/jbmr.1997.12.4.683. [DOI] [PubMed] [Google Scholar]
- 8.Faulkner KG, von Stetten E, Miller P. Discordance in patient classification using T-scores. J Clin Densitom. 1999;2:343–350. doi: 10.1385/jcd:2:3:343. [DOI] [PubMed] [Google Scholar]
- 9.Hans D, Downs RW, Jr, Duboeuf F, et al. Skeletal sites for osteoporosis diagnosis: the 2005 ISCD Official Positions. J Clin Densitom. 2006;9:15–21. doi: 10.1016/j.jocd.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Management of osteoporosis in postmenopausal women: 2006 position statement of The North American Menopause Society. Menopause. 2006;13:340–367. doi: 10.1097/01.gme.0000222475.93345.b3. [DOI] [PubMed] [Google Scholar]
- 11.Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ. 2002;167:S1–34. [PMC free article] [PubMed] [Google Scholar]
- 12.Kanis JA, Seeman E, Johnell O, Rizzoli R, Delmas P. The perspective of the International Osteoporosis Foundation on the official positions of the International Society for Clinical Densitometry. Osteoporos Int. 2005;16:456–9. doi: 10.1007/s00198-005-1861-0. discussion. [DOI] [PubMed] [Google Scholar]
- 13.Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 14.Black DM, Cummings SR, Genant HK, Nevitt MC, Palermo L, Browner W. Axial and appendicular bone density predict fractures in older women. J Bone Miner Res. 1992;7:633–638. doi: 10.1002/jbmr.5650070607. [DOI] [PubMed] [Google Scholar]
- 15.Looker AC, Wahner HW, Dunn WL, et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int. 1998;8:468–489. doi: 10.1007/s001980050093. [DOI] [PubMed] [Google Scholar]
- 16.Nevitt MC, Cummings SR, Browner WS, et al. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992;135:490–499. doi: 10.1093/oxfordjournals.aje.a116315. [DOI] [PubMed] [Google Scholar]
- 17.Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ., III Classification of vertebral fractures. J Bone Miner Res. 1991;6:207–215. doi: 10.1002/jbmr.5650060302. [DOI] [PubMed] [Google Scholar]
- 18.Black DM, Palermo L, Nevitt MC, et al. Comparison of methods for defining prevalent vertebral deformities: the Study of Osteoporotic Fractures. J Bone Miner Res. 1995;10:890–902. doi: 10.1002/jbmr.5650100610. [DOI] [PubMed] [Google Scholar]
- 19.Black DM, Cummings SR, Stone K, Hudes E, Palermo L, Steiger P. A new approach to defining normal vertebral dimensions. J Bone Miner Res. 1991;6:883–892. doi: 10.1002/jbmr.5650060814. [DOI] [PubMed] [Google Scholar]
- 20.Leslie WD, Tsang JF, Caetano PA, Lix LM. Number of osteoporotic sites and fracture risk assessment: a cohort study from the manitoba bone density program. J Bone Miner Res. 2007;22:476–483. doi: 10.1359/jbmr.061112. [DOI] [PubMed] [Google Scholar]
- 21.Lu Y, Genant HK, Shepherd J, et al. Classification of osteoporosis based on bone mineral densities. J Bone Miner Res. 2001;16:901–910. doi: 10.1359/jbmr.2001.16.5.901. [DOI] [PubMed] [Google Scholar]
- 22.Kanis JA, Johnell O, Oden A, et al. The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int. 2006;17:527–534. doi: 10.1007/s00198-005-0014-9. [DOI] [PubMed] [Google Scholar]
- 23.Tsang JF, Leslie WD. Exclusion of focal vertebral artifacts from spine bone densitometry and fracture prediction: a comparison of expert physicians, three computer algorithms, and the minimum vertebra. J Bone Miner Res. 2007;22:789–798. doi: 10.1359/jbmr.070319. [DOI] [PubMed] [Google Scholar]