Abstract
Purpose
In an effort to reduce the cost of surgical care, Medicare has introduced a new facility fee schedule for ambulatory surgical centers (ASCs). This prospective payment system increases reimbursement for many urologic procedures while decreasing reimbursement for others. All stakeholders: physicians, the Medicare program, and hospitals, will be affected by these changes.
Materials and Methods
Using the Agency for Healthcare Research and Quality’s State Ambulatory Surgery Databases, we identified Medicare patients in Florida undergoing urologic procedures in ASCs from 1998 to 2005. Three facility groupings were created: urology-dominant, multi-specialty, and other-specialty dominant. First, the impact of reimbursement changes at the procedure and facility levels was assessed using data from 2005. Projections of ASC utilization and reimbursement in 2008 were then generated using all available data.
Results
In 2008, we project total payments by Medicare to increase by $4,233,080 (26% Range 22% to 32%) under the new reimbursement system compared to the old system. At the facility level, reimbursement to multi-specialty facilities increases substantially (49% increase), while urology-specialty facilities receive less benefit (10% increase). Compared to multi-specialty facilities, urology-specialty facilities perform a higher proportion of cases where the reimbursement is set to decrease
Conclusions
Under the new payment scheme for ASCs, winners and losers emerge. Facilities with diversified procedure mixes will find increased revenue, while those with less diversification will find slower growth to their revenue streams. Counter to the desire of the Medicare program to decrease surgical costs, the new program may increase the payments made for urologic surgery.
Keywords: Medicare, Reimbursement Incentive, Urology, Ambulatory Surgical Procedures, Ownership
Introduction
The inexorable growth of health care expenditures1 has motivated payers to explore mechanisms of curtailing costs. Central to these efforts have been initiatives at the Centers for Medicare and Medicaid Services (CMS). These cost control efforts have altered the landscape of surgical care delivery. Initially, movement from fee-for-service to diagnosis-related group reimbursement for hospital care fostered the growth of ambulatory surgery.2–4 Additional policy changes facilitated the development of the freestanding ambulatory surgery center (ASC). These facilities are generally physician-owned2, 3 and have engendered significant competition between the hospital and the physician.4, 5
Though a central aspect of cost control efforts by payers,6 shifting surgical care from the hospital to the ambulatory setting has not been an effective means to lower overall costs. Rather than replacing hospital-based surgery, the growth of ambulatory surgery has added capacity, and overall utilization of surgical services has increased.7 To further encourage ambulatory surgery in the lower cost ASC environment, CMS has instituted a new prospective payment system for ASCs, in which facility reimbursement is two thirds of the hospital reimbursement.8 Under this new system, all surgical procedures will be eligible for reimbursement in the ASC.9
These changes in reimbursement have implications for all stakeholders. Since the reimbursement for some procedures increases and for others it decreases, financial success for an ASC will hinge on the procedure mix done in the facility. However, cost control will occur only if procedures migrate from the hospital to the ASC (i.e., stable rates of ambulatory surgery). For these reasons, we undertook a study to understand the financial impact of the new fee changes for ambulatory surgery to CMS and the ASC.
Methods
Patients
All visits for ambulatory surgery in the Agency for Healthcare Research and Quality’s State Ambulatory Surgery Databases (SASD) within the State of Florida between 1998 and 2005 were identified. The SASD is a compendium of data from 24 states that is compiled by the Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilization Project. These data provide patient-level discharge data for 100% of the ambulatory surgeries at facilities in the participating states.10 We chose data from Florida as our substrate because it includes discharges from both freestanding ASCs and hospital outpatient departments.
Since the anticipated regulations will apply to Medicare patients, we limited our analysis to surgeries in which CMS was the primary payer and to those patients 65 years of age and older. To limit potential bias induced by cross specialty competition, we further limited our population to admissions where the primary procedure was one typically performed by a urologist (Current Procedure Terminology (CPT) codes 50000 to 56000). Finally we restricted our analysis to 30 most common procedures performed in ASCs in each year of the study. The final study consisted of 35 CPT codes, accounting for 95% of all urologic ambulatory surgeries performed during the study interval. Our final cohort for the years 1998 through 2005 consisted of 206,676 procedures performed in 144 facilities. For the last year of available data (2005) we identified 24,780 procedures in 79 facilities.
Procedure-mix within ASCs
Because changes in reimbursement will vary by procedure, winners and losers will emerge depending on the procedure-mix of the ASC. As the regulations will impact the bottom line for ASCs based on procedure mix, we constructed our exposure to reflect the breadth of procedures done within a facility: urology-dominant ASC, multi-specialty ASC, and other specialty-dominant-ASC. First, we classified all procedures done within the ASCs according to AMA surgery classification codes.11 Next, we estimated the proportion of cases done by each specialty. For example, an ASC was considered to be urology-dominant if the majority of procedures in the ASC consisted of classification codes for the “Urinary System” or “Male Genital System” (CPT codes 50000–56000). Using this approach with the 2005 data, we identified 9 (11%) ASCs that were urology-dominant and 27 ASCs (34%) that were other-specialty dominant. In 43 ASCs (54%), no single organ system accounted for the majority and these were classified as multi-specialty.
Procedure Reimbursement
For each procedure, we used the difference in the reimbursement for the year 2005 and the reimbursement in 2008 based on the final 2008 fee schedule for ASC from the Federal Register8 to classify procedures into one of two groups: 1) those with decreasing ASC reimbursement, and 2) those with increasing ASC reimbursement (Table 1). No procedure had the same payment in the old and new reimbursement systems. When multiple procedures were performed in a single admission in the 2005 data, we calculated the total reimbursement for the visit based on the full payment for the CPT code with the highest payment, and 50% payment for the other codes.12 All costs were calculated using the full new fee schedule without a phase in period, and are expressed in 2005 dollars using a 3% annual discount rate.
Table 1.
Utilization Code Groupings
| Reimbursement | CPT |
|---|---|
| Decreasing | 51726 – Complex cystometrogram |
| 51772 – Urethral pressure profile studies (UPP) | |
| 51785 – Needle electromyography studies (EMG) | |
| 52000 – Cystourethroscopy | |
| 52310 – Cystourethroscopy, with removal of foreign body, calculus, or ureteral stent from urethra or bladder (separate procedure); simple | |
| 55700 – Biopsy, prostate; needle or punch, single or multiple; any approach | |
| Increasing | 50590 - Lithotripsy, extracorporeal shock wave |
| 51715 - Endoscopic injection of implant material into the submucosal tissues of the urethra and/or bladder | |
| 51725 – Simple cystometrogram (CMG) | |
| 51741 – Complex uroflowmetry | |
| 51784 – Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique | |
| 51795 – Voiding pressure studies (VP); bladder voiding pressure, any technique | |
| 51797 - intra-abdominal voiding pressure (AP) (rectal, gastric, intraperitoneal) | |
| 52005 – Cystourethroscopy, with ureteral catheterization, with or without irrigation, installation, or ureteropyelography, exclusive of radiologic service | |
| 52204 – Cystourethroscopy, with biopsy | |
| 52214 – Cystourethroscopy, with fulguration (including cryosurgery or laser surgery) of trigone, bladder neck, prostatic fossa, urethra, or periurethral glands | |
| 52224 – Cystourethroscopy with fulguration (including cryosurgery or laser surgery) or treatment of MINOR (less than 0.5cm) lesion(s) with or without biopsy | |
| 52234 - Cystourethroscopy with fulguration (including cryosurgery or laser surgery) and/or resection of; SMALL bladder tumor(s) (0.5 up to 2.0 cm) | |
| 52235 - Cystourethroscopy with fulguration (including cryosurgery or laser surgery) and/or resection of; MEDIUM bladder tumor(s) (2.0 up to 5.0 cm) | |
| 52240 - Cystourethroscopy with fulguration (including cryosurgery or laser surgery) and/or resection of; LARGE bladder tumor(s) | |
| 52260 – Cystourethroscopy, with dilation of bladder for interstitial cystitis; general or conduction (spinal) anesthesia | |
| 52276 – Cystourethroscopy with direct vision internal urethrotomy | |
| 52281 – Cystourethroscopy, with calibration and/or dilation of urethral stricture or stenosis, with or without meatotomy, with or without injection procedure for cystography, male or female | |
| 52315 - Cystourethroscopy, with removal of foreign body, calculus, or ureteral stent from urethra or bladder (separate procedure); complicated | |
| 52332 - Cystourethroscopy, with insertion of indwelling ureteral stent (eg Gibbons or double-J type) | |
| 52351 - Cystourethroscopy, with ureteroscopy and/or pyeloscopy; diagnostic | |
| 52352 - Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with removal or manipulation of calculus (ureteral catheterization is included) | |
| 52353 - Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with lithotripsy (ureteral catheterization is included) | |
| 52500 – Transuretrhal resection of bladder neck (separate procedure) | |
| 52601 – Transuretrhal electrosurgical resection of the prostate, including control of postoperative bleeding, complete | |
| 52648 - Laser vaporization of the prostate, including control of postoperative bleeding, complete | |
| 54161 - Circumcision | |
| 54520 – Orchiectomy, simple (including subcapsular), with or without testicular prosthesis, scrotal or inguinal approach | |
| 55040 – Excision of hydrocele; unilateral | |
| 55859 - Transperineal placement of needles or catheters into prostate for interstitial radioelement application, with or without cystoscopy | |
Statistical Analysis
Our primary outcome of interest was the Medicare costs of ambulatory urologic surgery in the State of Florida following the institution of scheduled reimbursement changes outlined in the Federal Register.8 We examined the anticipated financial impact to Medicare in two ways. First, we applied the anticipated reimbursement changes to the 2005 utilization among Medicare recipients, the last year of observable data. This approach, of course, assumes stable rates of surgery. Using the reimbursement for each CPT code under old and new systems, we calculated the total reimbursement according to the type of ASC (urology-dominant, multi-specialty, other specialty-dominant). We then assessed the procedure-mix within each facility to determine the relative proportions of procedures performed with increasing and decreasing reimbursements.
Because rates of utilization will likely change between 2005, the last year of observable data, and 2008, the year in which the new reimbursement policies take effect, we forecasted rates of procedure use for 2006–2008 based upon prior utilization (1998–2005). These forecasts were performed with autoregressive forecasting models in SAS (v9.1.2, Cary, NC). For each admission, the CPT code with the highest reimbursement was determined based on the old and new reimbursement systems. For these projections, we forecast the proportion of cases where the CPT code represented the highest payment and applied full reimbursement to that percentage of the cases, and 50% reimbursement to the remainder of the cases.12 These forecasted rates enabled us to generate anticipated Medicare costs of ambulatory urologic surgery for the years 2006–2008.
All statistical analyses were two-sided. The probability of Type 1 error was set at 0.05. This study, dealing with publicly available data, was exempt from Institutional Review Board approval in accordance with the Code of Federal Regulations, Title 45, Section 46.101.
Results
Overall utilization of ambulatory surgical procedures increased from 689 to 1027 cases per 100,000 population over the study interval—a 49% increase. Between 1998 and 2005, the use of procedures where reimbursement is targeted to increase grew at a slightly faster pace (296 to 434 cases per 100,000 population) compared to those with anticipated declining reimbursement (392 to 593 cases per 100,000 population), with relative increases of 46% and 51%, respectively.
To understand the financial impact of the regulatory changes, we first applied the reimbursements anticipated in 2008 to the last year of observable data (2005). From Medicare’s perspective, the new payment scheme would increase the total reimbursement to ASCs for urologic procedures. Under the previous payment rules, these procedures would cost Medicare $11,459,209 compared to $14,435,429 based on the new rules, an absolute increase of $2,976,220 (+26%). Among procedures with decreasing reimbursement, the total cost to Medicare would decline from $5,308,868 to $3,992,328 (−25%). However, these savings were outweighed by the cost of procedures with increasing reimbursement, expenditures for which rose from $6,150,341 to $10,443,102 (+70%). This translated into an overall Medicare payment increase of 26% for urologic ambulatory surgery procedures within the State of Florida.
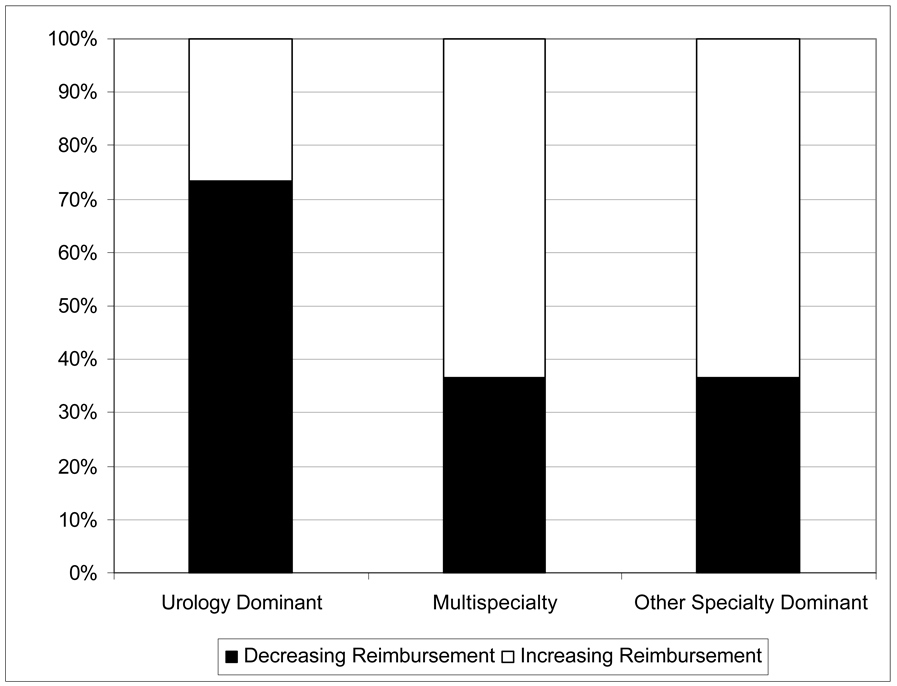
With respect to procedure mix, there were no absolute losers based on the anticipated changes (Table 2). However, the net and relative increases in reimbursement at multi-specialty and other specialty-dominant ASCs would outpace those at urology-dominant ASCs. This is a consequence of the reliance of urology-dominant ASCs on procedures targeted for decreasing reimbursement (Figure 1). Based on the 2005 data, 73% of procedures performed at urology-dominant facilities (11473 of 15628) have declining reimbursement compared to 37% for multi-specialty (2511 of 6845) facilities (p < 0.01 for the comparison of urology-dominant to multi-specialty) and 36% for other specialty-dominant (841 of 2307) facilities (p < 0.01 for the comparison of urology-dominant to other specialty-dominant).
Table 2.
Anticipated ASC reimbursements using 2005 utilization rates
| Number of ASCs | Old Payment Regulations* | New Payment Regulations* | Absolute Difference | Relative Difference | |
|---|---|---|---|---|---|
| Urology-dominant ASC | 9 | $6,678,649 | $7,328,513 | +$649,864 | +10% |
| Multi-specialty ASC | 43 | $3,563,686 | $5,324,720 | +$1,761,034 | +49% |
| Other Specialty-dominant ASC | 27 | $1,216,874 | $1,782,196 | +$565,322 | +46% |
| Total | 79 | $11,459,209 | $14,435,429 | +$2,976,220 | +26% |
costs expressed in year 2005 dollars
Figure 1.
Procedure mix by Type of ASC. Urology-dominant facilities performed a significantly higher percentage of cases where the facility fee declines in the new payment scheme (73%) compared to multi-specialty (37%) and other-specialty dominant (36%) ASC (chi-square p < 0.01 for between group comparisons to urologydominant ASCs).
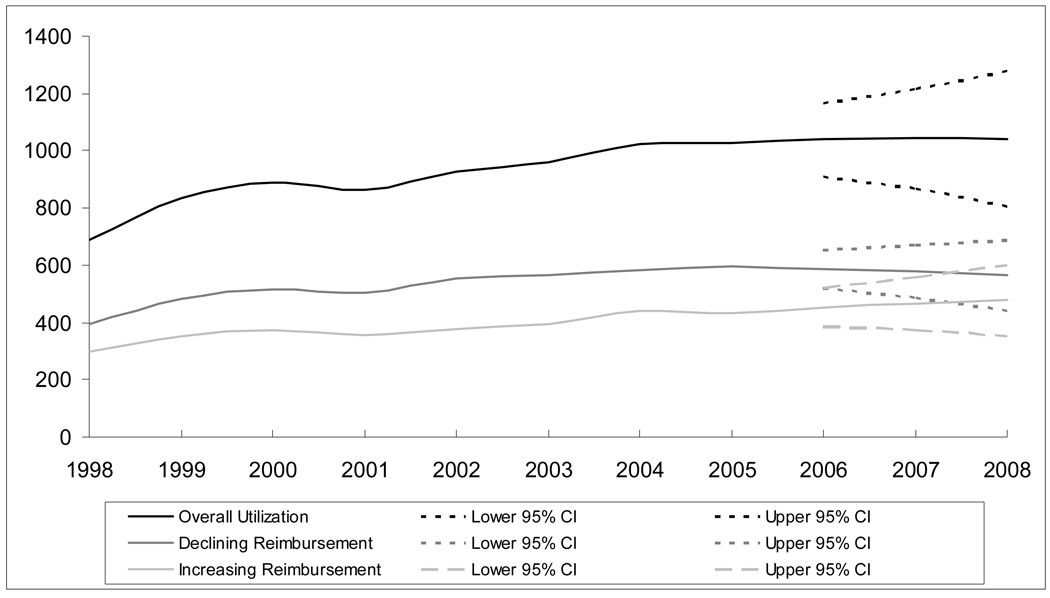
Recognizing that rates of surgery are unlikely to remain stable between 2005 and 2008, we used eight years of data to forecast anticipated utilization in 2006 through 2008. Our forecast did reveal a continued increase in the utilization of ASCs for these procedures (Figure 2). We forecast a slight increase in the use of those procedures that will have higher reimbursement (from 434 to 476 cases per 100,000 population between years 2005 and 2008), and a small decline in use of procedures with lower reimbursement (from 593 to 565 cases per 100,000 population between years 2005 and 2008). Table 3 illustrates the impact of reimbursement changes. The total in projected payments to ASC for urologic procedures in 2008 (in 2005 dollars) would be $19,219,544 [95% confidence interval (CI), $11,935,670- $27,465,487] under the new reimbursement regulations compared to $15,460,380 (95% CI, $9,962,419- $21,088,249) using the old reimbursement system for a net increase of $3,759,164.
Figure 2.
ASC Utilization for the Urologic Procedures in Florida from 1998 to 2005, with Projection to 2008. The vertical line at year 2006 represents the start of the forecast, and the dashed lines represent the upper and lower confidence intervals for each forecasted rate.
Overall utilization of ambulatory surgical procedures increased over the eight years of the study from 689 cases per 100,000 to 1027 cases per 100,000 (a 49% increase), with forecasted growth to 1041 procedures per 100,000 by 2008. We forecast a slight increase in the use of those procedures that will have higher reimbursement (from 434 to 476 cases per 100,000 population between years 2005 and 2008), and a small decline in use of procedures with lower reimbursement (from 593 to 565 cases per 100,000 population between years 2005 and 2008).
Table 3.
Projected Utilization and Reimbursement for 2007 and 2008 (in 2005 dollars)
| Year | Rate per 100,000 (95% CI) | Old Payment Regulations* (95% CI) | New Payment Regulations* (95% CI) | Absolute Difference | Relative Difference |
|---|---|---|---|---|---|
| 2005 | 1027 (observed) | 11,459,209 | - | - | - |
| 2006 | 1051 (820 – 1324) | $13,020,768 ($10,358,165 – $15,994,116) | - | - | - |
| 2007 | 1079 (764 – 1439) | $14,194,048 ($10,086,162 – $18,315,099) | - | - | - |
| 2008 | 1106 (691 – 1583) | $15,460,380 ($9,962,419 – $21,088,249) | $19,219,544 ($11,935,670 – $27,465,487) | + $3,759,164 ($1,973,251 – $6,377,238) | + 24% (20% - 30%) |
costs expressed in year 2005 dollars using a 3% annual discount rate
Discussion
In this study, we have demonstrated that the changes to regulations pertaining to ASC reimbursement by Medicare will not adversely impact the revenue at ASCs based on contemporary and forecasted utilization rates of ambulatory urologic surgery in the State of Florida. At the facility level, multi-specialty and other-specialty dominant ASCs appear to benefit the most from the new reimbursement system while urology-dominant ASCs can expect more limited gains. This difference is largely a reflection of the breadth of procedure-mix done within an ASC. For example, the most common procedures done in urology-dominant ASCs are targeted for lower future reimbursement. However, this future loss of revenue appears to be offset by revenue generated by procedures targeted for greater reimbursement.
These findings have implications for all stakeholders, including providers, CMS, and hospitals. Among providers, it is evident that, on average, ASCs will be insulated from the effect of reimbursement changes. However, at the level of the facility, physicians should be cognizant of procedure-mix performed in the ASC. The observed gains in revenue reflect cross-subsidization of common procedures, for which reimbursement will decline, by uncommon procedures, where reimbursement will increase. Clearly, it is possible for ASC revenue to decline under these new regulations if the procedure-mix is not favorably oriented.
The impact on the bottom line, from the perspective of CMS, is unclear. Ultimately, the goal of reducing overall health care costs can only be realized if rates of utilization remain relatively stable and there is a migration of procedures from the hospital outpatient department to the ASC.8 While the overall effect of these regulatory changes is not explicitly measured in the current study, hospital-based rates of ambulatory urologic surgery have remained stable throughout the study interval (unpublished data). Further, prior disincentives (e.g., exemption from ASC reimbursement)9 to performing select ambulatory procedures in ASCs will be removed under the new regulations, which may foster the migration of some procedures from the office to the ASC.9 While office-based treatment is clearly more efficient from a payer perspective,9 and may be revenue neutral from the physician perspective, alternative incentives, (including physician convenience and the necessity to demonstrate “need” requirements) may facilitate this movement.
The migration of ambulatory surgery from the hospital to the ASC has the potential to be detrimental to the hospital. As evidenced in other contexts, community-based hospitals typically provide a substantial component of non-reimbursed care whose costs are generally cross-subsidized by more lucrative care.13 If ambulatory surgery, including the more lucrative procedures, were to further migrate to the ASC as payers would hope, the ability to cross-subsidize “charity” care may evaporate. Although many freestanding ASCs are currently owned by physicians, additional migration may prompt greater hospital corporate investment in these facilities thereby fueling the competition between the hospital and physician for these patients.
Our findings should be interpreted with certain limitations in mind. First, the data source represented 100% of all ambulatory surgeries among Medicare recipients performed within the State of Florida, and therefore may have limited generalizability to the remainder of the US. However, CMS regulations apply universally to all states and regional reimbursement differences are relative; thus, our findings likely reflect national changes to the extent that the procedure mix in Florida is consistent with that elsewhere in the country. Second, our projected rates, while clearly imprecise, do reveal growth trends that have been consistent through the eight years of available data. However, the rates do not reflect future changes in utilization patterns by owners that better align their procedure mix more favorably based on new reimbursements. Finally, other procedural classifications, such as eye surgery and GI endoscopy, commonly performed in the ASC are targeted for substantially decreased reimbursement rates under the new payment system. In the context of overall CMS costs, these changes may outweigh the increases seen in urology.
Conclusions
Overall payment to ASC for urologic procedures will likely increase under the new Medicare reimbursement system, but will vary at the facility level based on procedure mix. The impact on the Medicare program and hospitals is less clear. Medicare depends on cases shifting from hospitals to ASC to achieve cost saving. If such shifts occur, the financial position of hospitals could be compromised. In this event, further competition between hospitals and physician-owned ASC is likely to occur.
References
- 1.Bodenheimer T. High and rising health care costs. Part 1: seeking an explanation. Ann Intern Med. 2005;142:847. doi: 10.7326/0003-4819-142-10-200505170-00010. [DOI] [PubMed] [Google Scholar]
- 2.Becker S, Biala M. Ambulatory surgery centers--current business and legal issues. Journal of Health Care Finance. 2000;27:1. [PubMed] [Google Scholar]
- 3.If You're Niched, It Might be You're Fault: Physician-Driven Specialty Hospitals and Ambulatory Surgery Centers. New York: Cain Brothers; 2003. pp. 1–13. [Google Scholar]
- 4.Medicare program; ambulatory surgical services--Health Care Financing Administration. Final rule. Fed Regist. 1982;47:34082. [PubMed] [Google Scholar]
- 5.Lynk WJ, Longley CS. The effect of physician-owned surgicenters on hospital outpatient surgery. Health Aff. 2002;21:215. doi: 10.1377/hlthaff.21.4.215. [DOI] [PubMed] [Google Scholar]
- 6.Schramm C, Gabel J. New England Journal of Medicine. Vol. 318. 1988. Prospective payment Some retrospective observations; p. 1681. [DOI] [PubMed] [Google Scholar]
- 7.Kozak L, McCarthy E, Pokras R. Changing patterns of surgical care in the United States, 1980–1995. Health Care Financ Rev. 1999;21:31. [PMC free article] [PubMed] [Google Scholar]
- 8.Medicare program; revised payment system policies for services furnished in ambulatory surgical centers (ASCs) beginning in CY 2008. Final rule. Fed Regist. 2007;72:42469. [PubMed] [Google Scholar]
- 9.OIG. Payment for procedures in outpatient departments and ambulatory surgical centers. 2003. OIG Report OEI-05-00-00340: i. [Google Scholar]
- 10.AHRQ. Introduction to the HCUP State Ambulatory Surgery Database (SASD) 2007 [Google Scholar]
- 11.Beebe M, Dalton JA, Espronceda M, Evans DD, Glenn RL, Green G, Hayden D. CPT 2007. Chicago: American Medical Association; 2006. [Google Scholar]
- 12.Code of Federal Regulations. Edited by D. o. H. a. H. S. Centers for Medicare and Medicaid Services. National Archives and Records Administration. 2004;vol. 2:730. [Google Scholar]
- 13.Choudhry S, Choudhry NK, Brennan TA. Specialty versus community hospitals: what role for the law? Health Aff (Millwood) 2005 doi: 10.1377/hlthaff.w5.361. Suppl Web Exclusives:W5. [DOI] [PubMed] [Google Scholar]