Summary
Objective
To discuss interdisciplinary research and education in the context of informatics and medicine by commenting on the paper of Kuhn et al. “Informatics and Medicine: From Molecules to Populations”.
Method
Inviting an international group of experts in biomedical and health informatics and related disciplines to comment on this paper.
Results and Conclusions
The commentaries include a wide range of reasoned arguments and original position statements which, while strongly endorsing the educational needs identified by Kuhn et al., also point out fundamental challenges that are very specific to the unusual combination of scientific, technological, personal and social problems characterizing biomedical informatics. They point to the ultimate objectives of managing difficult human health problems, which are unlikely to yield to technological solutions alone. The psychological, societal, and environmental components of health and disease are emphasized by several of the commentators, setting the stage for further debate and constructive suggestions.
Keywords: Medical informatics, biomedical informatics, health informatics, interdisciplinarity
With these comments on the paper “Informatics and Medicine: From Molecules to Populations”, written by Prof. Klaus Kuhn and others [1], Methods of Information in Medicine wants to stimulate an urgently needed broad discussion for further interdisciplinary research and education of informatics and medicine, and beyond. An international group of experts in biomedical and health informatics and related disciplines have been invited by the editor of Methods to comment on this paper. Each of the invited commentaries forms one section of this paper.
1. Informatics for the “Networked” Generation (by Russ B. Altman)
The paper by Kuhn et al. [1] offers an exciting and comprehensive vision of how informatics can be a unifying force for integrative research in biology and medicine. They make a convincing case that the physical spectrum from atoms and molecules to populations and global health has a parallel “informatics spectrum” from bioinformatics to public health informatics. What can be added to their comprehensive and convincing analysis? I would like to stress one important emerging phenomenon: the empowered, independent, and thoroughly “networked” consumer.
Modern youth have access to technology that arguably makes their intellectual, social and economic development radically different from not only their parents, but from any generation of humans that have yet lived. Young adults have grown up in a world with routine access to information around the globe via the internet (news sites, blogs, wikis, chat rooms, social networking sites, and more). They have and expect rapid access to volumes of information that could hardly be imagined 25 years ago. They manage this information with novel strategies that emerge by necessity: some use fairly static trusted sources (in the form of blog sites, wikipedia or even traditional news agencies) to aggregate information and distill it to something more consumable. Others have increased their communication bandwidth through apparently constant, uninterrupted use of e-mail, instant messaging, and text messaging to create multiplexed conversations that allow them to “sense” their environment and make decisions about how to respond. Of course, most use combinations of these strategies. The revolutionary nature of these changes is clear to anyone who speaks to a young person: “Why do we even have libraries? What are newspapers for? Why would I use e-mail when I can `text'? Why should I pay for music?”
What does this have to do with biology and medicine?I think we are already seeing changes in the fabrics of both disciplines that we can attribute to these trends. In science, there is great interest among young scientists in open access publications, open source software, and open data sharing. The traditional silos that provided protection and controlled access to information are not acceptable anymore. This creates not only major social and economic challenges (which I will not address here), but creates fascinating informatics research problems. Indeed, the availability of all these data sources creates a market for innovative informatics tools that can connect people to the information they want, when they want it, and in the (integrated) form they want it in. Research about how these tools should work will transcend any division between bioinformatics, engineering informatics, eHealth and public health informatics, because the best tools are likely to be general purpose.
In medicine, the effects of this transition are likely to have an even larger impact. Health care consumers are increasingly rejecting a model of parentalistic healthcare, where the physician is a parent-figure who makes independent decisions based on access to specialized information and as a proxy decision-maker for the patient. Consumers now have access to massive amounts of information on the web, and access to other consumers with similar health issues, and a willingness to share their experiences, treatments, and opinions. Even access to tests of potential medical relevance, such as large-scale genotyping of an individual's genome, is now available “direct to consumer” along with web resources to assist in the interpretation. The implications of all these activities for the informatics research agenda are tremendous: How can we support decision-making by healthcare consumers in partnership with their physician, as well as in partnership with their social network? How can we help them best use the network of health information and health providers to manage their health? How can we create methods for helping consumers gauge the credibility of an information source, and integrate information sources dynamically for a given health-related query? Finally, how can we ensure that the overall outcome of this new health-information economy is improved health?
One approach to these challenges may be to radically reconsider the structure of how we train scientists and medical students, and how we model the interaction between physicians and patients. In both cases, I think that the principles of informatics can be the actual basis of the “curriculum”. We should acknowledge to young researchers and physicians-in-training that there is too much knowledge for them to master in their brains, and so we will present a framework for knowledge and information use that stresses how to gather, organize and use information in their professional life, with much less stress on large amounts of content. Through problem-based learning, and research projects, they will get experience collecting and using detailed information to solve problems, but the curriculum will be entirely about collecting and managing information for the purposes of research and providing healthcare.
For patients, we should acknowledge that health-related information is overwhelming, and their physician is a collaborator who will help them navigate through this information, formulate questions and potential actions, and help them make decisions about how to proceed. The primary physician will be a “general contractor” for health information, who will work with the patient to find “subcontractors” that can provide specialized services and information that the patient needs.
In summary, current trends indicate that an information-processing metaphor for scientists, healthcare providers and patients is a more realistic model as we move forward. If this is true, the research opportunities for bringing it to reality are extremely exciting.
2. Let's Merge Coffeerooms (by Rudi Balling)
My first reaction to the article by Klaus A. Kuhn and his colleagues was asking myself, whether the first author was related to Thomas S. Kuhn, the author of the famous book “The Structure of Scientific Revolutions”, published in 1962. In this book T. Kuhn describes the development of new paradigms in the course of the history of science stating: “Conversions will occur a few at a time until, after the last holdouts have died, the whole profession will again be practicing under a single, but now a different, paradigm” (p 151).
I think there is no doubt that we are currently in the midst of a scientific revolution. The question is which one: The revolution triggered by the progress in information and communication technology, where we have developments such as the Turing-machine, the invention of the transistor, integrated circuits and the computer? Or the revolution in genetics and genomics providing completely new insights into the complexity, emergence and regulation of biological systems?
The article by K. A. Kuhn et al. “Informatics and Medicine” reminds us that we are already at the next phase, which is characterized by the merger of these two fields and how they influence each other. The authors provide an impressive description of the “application space” of these new technologies and one wonders if their outline of the convergence of informatics and medicine is already an indicator of a 6th “Kondratieff-cycle”.
Being excited and enthusiastic about the scientific and economic potential, or skeptic and reflective about the social and ethical risks involved is one side of the story. Equally interesting is the question of how we, as a scientific community, cope with the challenges of interdisciplinary research. Kuhn et al. argue for a strengthening of interdisciplinary collaboration and education.
It is much easier to talk about interdisciplinarity than to practice it. There is no doubt that, quoting Leland H. Hartwell [3]: “The next generation of students should learn how to look for amplifiers and logic circuits, as well as to describe and look for molecules and genes.” But how do we teach the ability to work in an interdisciplinary environment? How should future curricula for biology and informatics look like? “Depth or breadths?”
Kuhn et al. describe the cultural gap between classical natural sciences (e.g. chemistry, biology, physics) and engineering and informatics. I spent some time during the last years in talking to engineers, physicists, mathematicians and computer science/informatics professionals trying to entice them for joint research programs tackling the complexity of biological systems. I had to learn that many of these colleagues were as scared of biology as biologists are often scared of mathematics. Nevertheless, the interest and the excitement to bridge the gap of disciplines and go beyond one's own “domestic culture”was enourmous.
It is not so long ago, that mathematicians, computer scientists and physicists were looked down upon by their colleagues if they devoted their research to biological problems. Apparently they didn't make it in their own hard and stringent discipline. This has changed. The grand challenges of the future have been recognized to lie, not exclusively but increasingly, in understanding the complexities of biological systems. And this is recognized by the best and the brightest in these “hard and stringent” disciplines.
My suggestion is to put the emphasis on our ability to talk with each other across the various disciplines. Talking to each other requires either the same language or at least some basic knowledge in the foreign language. Mathematics is THE language if we want to tackle the issue of predicting how biological systems will behave in case they are perturbed. Information science and technology could not exist witout mathematics at the heart of it.
I am not sure whether I agree with the suggestion made by Kuhn et al. that “... the most effective way of changing the patterns of scientific education is to address the level where teaching and research meet:MSc and PhD programs”. I fully support their proposal to set up coordinated and combined courses and research training for advanced students in medicine, science and engineering/informatics. I am also a great fan defining joint research projects and workshops, to foster links at the institutional and personal level and to encourage team-work at a high scientific level.
I am worried that all of this will come will come too late. We need to start much earlier. There are a lot of complaints from our colleagues teaching first year biology about a declining level of the students profiency (and interest) in mathematics. At least in German highschools one can observe a dramatic degradation in the importance given to mathematics, physics and biology. Parents are more worried about getting their children through highschool at all, opening the doors to soft(er) disciplines and a lack of appreciation for a solid education in natural sciences.
Unfortunately this trend is amplified by many of our leading politicians. We are heading for a disaster, and our political leadership still braggs about how little they understand about mathematics and genetics. The waters might be muddy and the logic might be fuzzy, but the message is clear: Informatics and medicine will converge. Kuhn et al. give us a valuable orientation on how to structure the bewildering heterogeneity and opportunities of cooperation of these fields. As a first step I suggest to merge the coffeerooms for our students and faculties. Then all the rest will follow.
3. Towards Biomedical Informatics as a Scientific Field (by James F. Brinkley)
This paper by Kuhn et al. [1] is the result of a set of meetings among leaders of two universities in Munich, the goal being to implement an interdisciplinary graduate school in biomedical informatics. Members of the group, who are the authors of this paper, are generally the leaders of biomedical, technical and management departments at the two universities. Specific fields represented include medical informatics, bioinformatics and systems biology, robotics, computer architecture, software engineering, databases, algorithms, augmented reality, nuclear medicine, molecular biology, cardiovascular surgery, genetics, radiology, internal medicine, dermatology, orthopedics, biometry, and epidemiology. The particular list of fields is relevant because much of the paper can be seen as an attempt to discover and classify the common biomedical informatics activities already ongoing in these separate disciplines. In fact the recognition of this commonality, along with the increasing relevance of informatics to biomedicine, is undoubtedly the major impetus for the creation of the interdisciplinary graduate school. Such an endeavor is truly visionary, going far beyond most academic biomedical informatics programs, many of which are struggling to achieve departmental status, let alone the status of an entire graduate school. Yet the shear breadth of activities described in the paper makes it clear that there are enough biomedical research problems to justify the creation of an entire graduate school, so it is likely that this effort will not be the last of its kind.
In order to create a graduate school the many activities need to be organized into separate but overlapping units. In the US such units would be called departments. Thus, the four classifications in the paper suggest separate departments of bioinformatics and systems biology, bioengineering informatics, health informatics and eHealth, and public health informatics. This classification is similar to one that we use in our University of Washington (UW) Biomedical and Health Informatics graduate program (BHI): biology informatics, clinical informatics, and public health informatics. We never considered including bioengineering informatics in our program because the UW already has a very strong bioengineering department, many members of which are involved in some aspect of computing. On the other hand we do collaborate with faculty in bioengineering, bringing expertise in information and knowledge management, which the bioengineering faculty are generally not experts in. Thus, a case could certainly be made for including bioengineering informatics, especially if there is not already a separate bioengineering department.
One difference in terminology appears to come from the use of the term “bioinformatics”. In the paper it is stated that“the goal of bioinformatics is to understand the molecular mechanisms, their genetic frame-work for diseases and their responsiveness to therapy...”, yet many of the research problems described in section 3.1 involve correlating genotype with phenotype, which often means dealing with information at all structural levels ranging from genes to the whole organism. Although it is true that the common understanding of bioinformatics is that it deals with the molecular level, the need to correlate genotype with phenotype has led many researchers to move beyond the molecular level. With the completion of the various genome projects this migration will only become more prominent, and in fact several groups have attempted to extend the definition of bioinformatics to include all of basic biology, thereby automatically including such fields as physiological simulation and systems biology (which many would argue are the same thing). One reason we chose not to use the term“bioinformatics”in our program is to avoid this ambiguity.
A second difference in terminology is in the use of the word “informatics”. In the introduction it is stated that the European use of this word corresponds more or less to the term “computer science” in English speaking countries. Yet the many research problems described in the paper go beyond what is generally taught in most US computer science departments, including activities like imaging, signal processing and computational modeling, which are generally taught in electrical engineering or bioengineering departments. Thus, the impression is that the use of the term “informatics” in the title of the paper implies all these activities applied to biomedicine. Such a broad definition is appealing because it helps to unify many activities under one umbrella -although such a unification would not occur in the US given our more narrow definition of computer science.
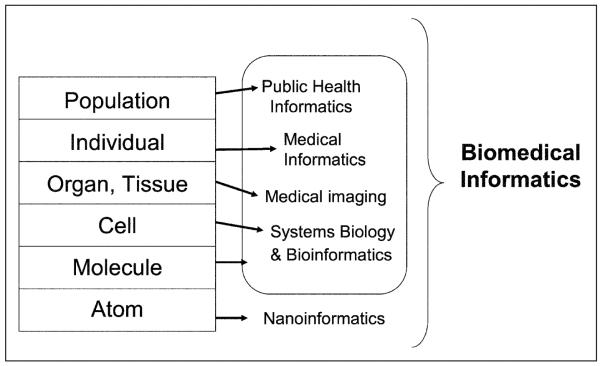
Given the broad definition of informatics as defined in the paper, it might be useful to list the informatics research issues that are described under the four categories. These issues include but are not limited to: signal and image processing, simulation and modeling, data and knowledge representation, data management and integration, visualization, information retrieval, and sociotechnical issues. As noted several times in the paper these informatics issues occur in many if not all of the four fields described in the paper, which is where the commonality of these fields is seen to lie. Thus, in some ways figure 2 is misleading: in fact arrows should be drawn between each box on the left side and every box on the right side, not just those on the same level.
Fig. 2.
Information and medicine: from atom to population
This commonality leads to the notion that there is a core set of informatics methodologies that underlies all four of the areas. Thus, in the BMI program we would call the areas in the paper application domains (which in our case are basic biology, clinical medicine and public health), and we define core informatics domains as those areas that underlie biomedical informatics research in all the application domains. These areas are generally drawn from and include pre-requisites from underlying disciplines such as computer science or electrical engineering, but the courses that teach them are tailored to the biomedical domain. Thus, as the new graduate school is developed it might be worth while considering the addition of a unit that could teach these core informatics areas. Such a unit would formalize the commonality that is already evident in the descriptions seen in the paper, and would help transform the field of biomedical informatics from a collection of loosely connected application areas to a scientific or engineering field in its own right, with its own core principles and methodology distinct from any other field.
4. Systems Informatics and the Socio-technology of Bioscience (by Enrico Coiera)
The agenda of informatics researchers almost inevitably returns to technology, and for good reason. Information and communication systems are transforming our world in a powerful way. We would not be able to anticipate climate change without highly sophisticated computational models to alert us to its risks. We would not be able to more robustly deal with international financial shocks than we did in past centuries without the web of economic data shared by central banks globally. And we would not be able to anticipate the now palpable revolutions in systems biology and genome science that foreshadow truly personalised medicine, without IT. The human genome project after all, in the end hinged on computers to pull together shot-gunned genetic fragments into a plausible pastiche of a whole genome.
The technological challenge in bringing together systems biology and clinical medicine, what we now seem to be calling translational bioinformatics [4], is huge. This union “from cell to system” has been long anticipated, and Blois back in the 1980s already then wrote of the nature of `vertical reasoning' that takes place in clinical decisions, from low-level biology through to clinical and organisational levels [5]. Kuhn and his colleagues paint us a broad and exciting picture of many of the information technology challenges that we face in that journey [1]. Not least of these is the huge representational and inferential challenges of build knowledge structures at different scales and expecting them all to effectively interact and generate meaningful information [6]. They also note in passing that humans themselves are part of the big picture, and that there are cultural barriers to be breached if we are to bring bioscientists and clinicians together.
I have said in the past that health informatics is “the study of how clinical knowledge is created, shaped, shared and applied. Ultimately, it is the study of how we organise ourselves to create and run healthcare organisation” [7]. In other words, we cannot separate the cognitive and the social from the technical, and this lesson is as true of the challenges for e-health at the clinical level as it will be for translational bioinformatics. Indeed, if we are to imagine an informatics which is all about integrating different biomedical, clinical and organisational systems - let us call it a systems informatics - then I want to argue again that we must put ourselves into the middle of that system as primary actors whose behaviour needs to be modelled, along with molecules and medicines.
At present the cross-systems informatics research agenda is driven largely by the technical challenges of information integration, and an analysis based upon an assumption about the way scientists “do things around here”. In many ways the bioscience informatics agenda is where clinical informatics was in the eighties, where we used idealised models of what work should be, and were blind to how things actually were. The last 20 years have seen a growing sociotechnical critique, for example from influential commentators like Berg [8], who began to highlight how often seemingly well-designed IT failed when it was finally put into the clinical workplace, because it's designers fundamentally misunderstood how clinical work was done. The mantra of `re-engineering' clinical work for efficiency, and of clinicians and not technologists needing to change their attitudes was the initial informatics response to this clinical push-back.
But we now know a little better. Clinicians usually resist change for very good reasons - we still build systems that help administrators more than clinicians. We still build electronic record systems that on the face of it take longer to use than pen and paper, even if there is a big downstream payoff in safety, quality and efficiency. And we build systems that still ignore the fundamentally complex nature of healthcare. Clinical work is not like work in a factory, is not like a pilot's cockpit nor like a bank, and many of the models of workflow automation that work so well in other settings ill-fit clinical practice, which is fluid, multi-tasking, interrupt-driven [9], complex, and where treatment is often necessarily bespoke because of patient differences.
We should therefore already intuitively understand that bioscientists do more than analyse complex data sets. Before the experiment, before the analysis, there is a complex social process, in some way similar to the processes that clinicians undertake before a treatment plan is agreed upon. And once an analysis is done, its meaning is debated and shaped socially, because of the inherent ambiguity and incompleteness of our knowledge, and the various perspectives scientists bring to such discussions. For example, co-expression of cellular proteins does not strictly imply co-regulation or a causal relationship in biochemical processes. Scientists employ additional background knowledge to make assessments about the weight of evidence behind known relationships, or the likely causal relations that might be implied through associational studies. Whose background knowledge triumphs in a research team's debate is still no doubt often a tribal affair.
Latour has written vividly about such social aspects of science [10] and our new challenge is to embrace a richer sociotechnical agenda so that we can craft systems that truly link bench to bedside [11]. The `secret' work that gives rise to bioscience data and its interpretation is something we really need to understand, because what bioscientists do today, clinicians will do tomorrow. The clinicians of the near future will be awash with genetic and biomarker data from their patients, and they will often have little concrete information to guide them to what they all really mean. As ever, we have much more data than we have knowledge about what those data might mean.
Socio-technical systems science has arisen in response to the challenges of understanding complex technical systems that are embedded in a human world [12]. It has arisen most strongly because the unexpected interactions between humans and artefacts often produce unanticipated errors, system failures, cost overruns and breakdowns. The socio-technical view attempts to understand the contribution of phenomena at the human social level to the performance of technical systems, and vice versa. It is thus the missing system in any bold re-conceptualisation of our field as a systems informatics. What is therefore needed is a way of describing events at the socio-technical level, connecting them to system behaviours and thence to artefact design. We need to get `technical' about what we mean when we describe socio-technical events, `technical' about what we want from system design, and we need to work both alongside technologists to shape technology, as well as with the processes, organizations and cultures within which they will be embedded [13].
Socio-technical systems thinking is an essential prerequisite to the process of developing new, safer and more effective ICT systems that span different social systems like bioscience, clinical medicine and the citizen. Each is its own universe, and technology will not `normalise' these universes into one. Instead it must help bridge these universes, which are ever evolving, ever different, ever new.
5. Enhancing the “Human Factor” into the Framework (by Fabrizio Consorti)
Multidisciplinary integration at research and educational level is surely the right way to proceed and face the relevant challenges that the inner complexity of healthcare domain put forward, especially when the management of information is concerned. The paper of Klaus Kuhn and co-workers [1] represents a powerful effort toward a comprehensive framework for an inter-professional curriculum in health informatics. Nevertheless, to the taste of a physician - like I am - an essential ingredient is still scarce in the recipe, in its dual flavor of “caregiver” and “patient”: the human factor.
In the paper, social sciences are quoted in conjunction with economics, ethics or with passive concepts like “acceptance” or “impact”, along with functional expressions as “time-saving” or “cost-saving”. Moreover, topics like the Internet or the web, intended as social environments, are never explicitly mentioned. Maybe these remarks come just from a wrong feeling, based on a misunderstanding of the sense of some sentences, but all the same it's a worth discussing the dimensions of the “human factor” in deeper details.
Multi-professionalism is not just a matter of exchange of competencies but mainly an encounter of professional paradigms, aimed at the definition of a common meta-paradigm, bridging cultural gaps. Mutual awareness of the different points of view is as important as the acknowledgment of the different, specific technical competencies. Then my contribution to the discussion will bring an up-to-date clinical point of view, by briefly summarizing the role of the web-based social cooperative environments in the evolution of current “master narratives” related to the healthcare domain. Concepts like wellness and illness, process of care, patient-caregiver relationship are changing in their social representation and ICT is a factor of the process. This trend will be framed in the context of the two conflicting paradigms of evidence-based medicine (EBM) and narrative-based medicine (NBM).
Narrative has always been the main way to communicate knowledge about facts in the world. Even scientific knowledge needs the support of narrative to be communicated: a scientific paper is the “story” of an experiment, even if it is expressed in a rather formalized structure. More specifically, narrative knowledge is focused about understanding the situation of a singular person through cognitive, symbolic and affective means. A master narrative (or meta-narrative) “is a global or totalizing cultural narrative schema which orders and explains knowledge and experience” [14]. It acts as an organizing principle which provides sense to every-day experience and synthesizes shared ideas in an archetypical way. Examples of master narratives are myths and popular tales, the narration of national historical events, masterpieces of literature. Personal identities too are narratively constituted [15], as complex networks made by self-narration and by the stories told by others about ourselves. In this context, identity is then a social construct and every mean affecting in some way socially shared narratives has a relevant consequence for everyone [16]. Technological innovations such as the Internet have increased the interconnectedness of groups. The web has contributed to the erosion of traditional community life by decreasing the importance of proximal, local sites of social influence with respect to the global community [17]. Basic concepts like health, illness and risk conditions are evolving in their meaning [18] and the evolution is strongly influenced not only by the great availability of healthcare-related information on the web but also by social environments like virtual communities [19, 20]. As a matter of fact, the largest part of knowledge present on the web - in forums and blogs - has a narrative format.
The term “narrative based medicine” was born by the end of nineties, in a series of papers on the British Medical Journal [21], based on an original book by Katrin Hunter [22]. NBM is a novel approach to medical practice, as a reaction to a technology-driven practice lacking empathy. It has been often opposed to the other raising professional paradigm of the evidence-based medicine (EBM), even if the competition has in fact no foundation, because NBM and EBM simply define two different, paired dimensions of medical knowledge.
However, since its more known definition by Sackett in 1996 [23] as “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients, integrating individual clinical expertise with the best available external clinical evidence” EBM produced an uninterrupted flow of discussion, which reveals how sensitive is the topic of representing medical knowledge among physicians.
EBM as intended nowadays would be virtually impossible without the availability of digital libraries. This last point, together with the diffusion of systems for at-distance learning based on a constructivist approach, highlights the importance of considering the ongoing shift from a static representation of knowledge as a “content” (accurate and universal representation of some prior reality) to a concept of knowledge as an enactment of “knowing” in a given context [24]. Focusing on the contextualized act of knowledge rather than on the content in fact strongly reduces the difference between “knowing” and “learning” and it blurs the boundaries between knowledge management systems and e-learning systems [25, 26].
Which consequences for research and education can we drive from all of these considerations?
There should be an explicit involvement of anthropology, sociology, social psychology and education sciences in the blend of multi-professionalism, for an effective curriculum and a creative research environment.
Attention should be devoted not only to technologic development (technology in itself is not inherently empowering) and to quantitative research aimed to maximize/minimize a parameter but also to qualitative research, aimed to “knowing”, also in terms of personal commitment of the intended users of ICT systems.
From an educational point of view, a systemic approach should be adopted, always keeping in mind the whole while discussing the detail and highlighting the links and the relationships among dimensions and contexts.
A particular attention should be devoted to emerging topics for research and education like the management of narrative knowledge, also in considering that in a few years the generation of “digital natives” will be adult and will have an active role in society. For them, booking an appointment or accessing personal health data by the Internet will be just a routinary task, while probably they will be demanding for much more sophisticated possibilities of interaction.
6. Informatics and Medicine from a Developing World Perspective (by AliDhansay)
When I was invited to write a commentary on the paper by Kuhn et al. [1], I was uncertain since I saw myself as being `informatics naïve'. On the other hand, I thought I could bring to the discussion a multidisciplinary medical background (pediatrics and child health with research experience in the same fields), as well as nutrition research and research management experience at a senior level in a developing country setting - South Africa. Some might argue, justifiably to my mind, that SA is a `hybrid' of a developing (major part) and developed country, which lends itself to novel research opportunities and challenges. I consider the invitation as a learning (for myself in the area of informatics) and a sharing opportunity (from a South African, research and medical perspective).
6.1 Introduction
“Knowledge of what is, does not directly open the door to what should be.”- Albert Einstein
The above quote, in effect, exhorts one to move towards action, i.e. translating knowledge into outcomes beneficial for the health and well-being of populations [27, 28]. It captures the essence of what Kuhn and colleagues from two Munich universities and the Munich Heimholz Center have achieved, with the establishment of a `research-oriented interdisciplinary Graduate School'. Their paper neatly captures the `knowledge of what is', as well as the `what should be' parts of the above quote. They have moved from theory to practice in a sense and should be commended for this. The bottom line, of course, will be the evaluation of whether the graduate school reached its intended goals - a keenly awaited result in light of the dearth of documentation of such experiences [29].
6.2 Interdisciplinary Research (IDR)
A definition of IDR is appropriate at this time: “Interdisciplinary research is a mode of research by teams or individuals that integrates information, data, techniques, tools, perspectives, concepts, and/or theories from two or more disciplines or bodies of specialized knowledge to advance fundamental understanding or to solve problems whose solutions are beyond the scope of a single discipline or area of research practice” [30].
“It took an ex-physicist - Francis Crick - and a former ornithology student - James Watson - to crack the secret of life. They shared certain wanderlust, an indifference to boundaries.”- Robert Wright
It is refreshing to see that informatics researchers are looking at concrete ways of contributing, nay, being part of the current movement towards translating knowledge to practice. The paper reflects, on one hand, the universal call for employing interdisciplinary research to tackle the complex nature of disease and ill health in today's globalized society, and on the other, seeks to specifically establish the role of informatics and its disciplines as part of this important challenge. There is no doubting the role of ID health research [30-35]. ID health research is based upon the recognition of diversity/differences, yet agreeing upon the ultimate objective of a unitary outcome, viz. improvement of health and well-being for individuals and populations. Interdisciplinary thinking is rapidly be coming an integral feature of research as a result of four powerful “drivers” [30]:
the inherent complexity of nature and society;
the desire to explore problems and questions that are not confined to a single discipline;
the need to solve societal problems;
the power of new technologies.
It is encouraging to note that Kuhn and colleagues have moved beyond the bedside, to the community and population level. The keywords that stand out in the paper are collaborative research and structured interdisciplinary education. While somewhat `lost' within figure 1 and not repeated again in the text, the critical phrase `Informatics in Support of Translational Research' captures the essence of their paper.
Fig. 1.
Researchers per million inhabitants - year 2000 (source: National Research Foundation, South Africa)
Kuhn et al. have also traversed the intersection of bioinformatics and medical informatics (biomedical informatics) [36-39] and cogently address the issues of public health informatics and public health, with prevention as an ultimate target. They present a practical framework of how informatics can act as driver/enabler/interlocker in the continuum from molecules to population via the fields of biosciences, medicine and public health. The authors call for collaborative research and structured interdisciplinary education in four priority areas: bioinformatics and systems biology; informatics for biomedical engineering; health informatics and e-Health; and public health informatics and public health.
6.3 The Challenges of IDR
When setting up their graduate school, one accepts that the authors would have taken into account the comments of the National Academy of Sciences [30] and others [40-43] regarding IDR, viz. (not in order of importance)
need for structures to support interdisciplinary research;
job opportunities for IDR;
evaluation of IDR and scientists and out-puts will need modification of the peer-review process to include researchers with interdisciplinary expertise in addition to researchers with expertise in the relevant disciplines;
funders' views on IDR and its support;
role of professional and academic societies;
shortage of health workers and scientists/researchers in developing countries;
the success of IDR groups depends on institutional commitment and leadership;
promotion, tenure, and resource allocation;
institutions are impeded by traditions and policies that govern hiring practices;
the success of IDR groups depends on institutional commitment and research leadership;
new modes of organization and a modified reward structure to facilitate interdisciplinary interactions;
professional societies have the opportunity to facilitate IDR by producing state-of-the-art reports on recent research developments and on curriculum, assessment, and accreditation methods; enhancing personal interactions; building partnerships among societies; publishing interdisciplinary journals [44] and special editions of disciplinary journals and promoting mutual understanding of disciplinary methods, languages, and cultures;
learning from collaborative interdisciplinary research partnerships among universities, industry, and government.
The above points immediately present a bigger challenge to researchers in developing countries, faced with problems of rudimentary health systems, poor infrastructure and human resources for health, and low spending on research and development. Table 1 and Figure 1 below illustrate the situation well.
Table 1.
Researchers and GERD in developing and developed countries
| World population | World researchers | World GDP | World GERD | |
|---|---|---|---|---|
| Developing countries | 79% | 28% | 42% | 20% |
| Developed countries | 21% | 72% | 58% | 80% |
GERD = gross expenditure on research and development
6.4 IDR Leading to Translational Research
While the lack of funding, health infrastructure and resources can be seen as added impediments to IDR in developing countries, this makes it even more important to `work smartly' in multidisciplinary and interdisciplinary collaborations than ever. Similarly, the need to fast track knowledge translation in these countries is just as urgent - interventions which are cost-effective need to be implemented. In this regard, the framework for the integration of informatics with health as presented by Kuhn et al. needs to be tested and implemented in developing country settings as a matter of urgency.
6.5 Context Is Important
While there are many similarities in health challenges facing developing countries compared to developed countries (e.g. health and nutrition transition to `diseases of lifestyle'), there are also major differences, e.g. the massive burden of HIV and AIDS, tuberculosis and malaria in Africa. Health information systems are not efficient, impacting on resource allocation and evaluations of the health system. Developing countries including South Africa are experiencing severe shortages of health care personnel in the public sector to Europe and North America, as well as to the WHO! Poverty and inequity (in general and in health) are inexorably linked, and this is reflected in the not unexpected differentials in morbidity and mortality found in South Africa (skewed unfavorably towards blacks). Inequality and inequity at all levels and sectors present many challenges to the goal of improving the health of nations [45].
In South Africa, 93% of the majority black African population (80% of SA population) has no medical aid (insurance) and is dependent on the public health sector, while 58% of the minority white population (9% of SA population) has no private medical cover. These differences in health care financing are important in the context of funding of `high tech' innovations. A recent survey of the role of genomics medicine in developing country contexts, which included South Africa, argues that there is a role for investing in genomic sciences in developing countries. They posit that investing in the field, identifying niche areas within it and within areas of local interest, and building life sciences-based capacity around such knowledge could contribute to improving local health, as well as potentially stimulating economic development. The role of private partnerships in this regard is also highlighted [46]
The area of personalized medicine was also mentioned by Kuhn et al. in the context of public health and genomics. Again, in the South African context, issues such as race and ethnicity and the medicalization of race are issues that numerically and ethically assume much greater importance than the BiDil debate in the USA [47]. These are fertile areas of potential research for interdisciplinary teams, including informaticians.
6.6 What Are the Implications of the Paper for Developing Countries?
There is a need to embrace the call for interdisciplinary research and education, and to highlight the role of informatics as an enabler in the whole process from bench to bedside to the community.
Collaboration with developing countries on an equal footing should be encouraged.
Realization that there are context-specific issues that have to be considered, e.g. local technological, funding, population dynamics. Recognition of diversity and differences.
Foster debate around ethics (of genomic medicine and personalized medicine), information access, education and social issues in developing country settings.
Personalized medicine also raises the question of identification of patients who are most likely to benefit.
Ensure partnerships with, for example private sector are conducted ethically and openly for the benefit of public health.
6.7 Conclusion
One trusts that new synergies will be forged between the various disciplines, e.g. medical informatics and bioinformatics, based on the promise outlined in the paper by Kuhn et al. To quote the present director of the National Institutes of Health, Dr. E. A. Zerhouni: “It is the responsibility of all of us who are involved in health research to translate the remarkable scientific achievements/innovations we are witnessing into health gains for the nation” [28]. Of course, this should be extended to the global community, and especially the developing nations with their greater burden of disease.
The authors have taken a bold step in establishing the Graduate School in Munich - in effect demonstrating the move from theory to practice. To my mind, there is a dearth of information on such initiatives; little has been documented about how researchers experience interdisciplinary health research in practice. Furthermore, factors such as career path opportunities, reward and recognition, evaluation criteria, long-term future etc. are all important. It is therefore imperative that they document and share their experiences, which will be keenly awaited by the scientific, academic, medical, and informatics fraternity.
Both the medical and informatics communities need to extend the discourse initiated by Kuhn et al. to the challenges posed by developing country settings. It is only proper that those areas of the world most beset by ill health should be part of the move towards working smartly and in an interdisciplinary fashion. South Africa has the unenviable reputation of being the world leader in many disease areas such as HIV and AIDS, tuberculosis and fetal alcohol syndrome. With its diversity of populations (exemplified by its rainbow nation tag) and in burden of disease patterns, the country lends itself to opportunities for collaborative research on informatics and health between north and south [48, 49].
7. On Global Trends and Challenges (by Antoine Geissbuhler)
Enabling information and knowledge to flow and grow from molecular scale to patients and populations is one of our ambitious goals and grand challenges. This “info-bio convergence” has an enormous potential to improve our fundamental knowledge in life sciences, the ability to translate it into better and individualized patient care, and will open new ways of studying and steering our pressured health and healthcare systems. Further down the road, many foresee the additional convergence with nanotechnologies and cognitive sciences, thus realizing an unprecedented synergy of skills and knowledge [50].
Although the way seems clear and the future bright, there are many obstacles that need to be overcome, many of which lie partly within the scope of biomedical informatics, and most of which will require new forms of collaboration, of research, and probably of education.
We must be able to connect information from these various knowledge domains. Connectivity of the infrastructure from multiple, heterogeneous, and distributed resources is likely to evolve from the current data and computational grids. Connecting the physical and the information world will require new abilities to identify, track, and link objects from both worlds. But the main connection challenge will be the semantic integration of these mostly distinct domains, as exemplified by the IUPS Physiome Project [51].
With the advent of our knowledge society, we need to rethink the way we design research. Digging in the massive amount of data that is made available on the Web, will need new research paradigms, potentially moving away from hypothesis-driven research (whether in vivo, in vitro or in silico) into data-driven research [52]. At the same time, citizens of our knowledge society will have the opportunity to reshape the way their information can be used for research, potentially displacing the centers of knowledge production away from the academic environments [53]. Furthermore, the new interactions between humans and machines that are currently appearing will require new research disciplines, such as the Web science, coined by the Web inventor, Tim Berners-Lee [54].
In this interconnected, highly complex landscape, multidisciplinary collaboration will indeed be the rule for progress. A challenge will be to foster the right mix of hard sciences, life sciences and social sciences necessary to apprehend the problems at hand. The collaborative tools of the social Web will help to some extent, as will the knowledge engineering tools brought by informatics research. It is however likely that the current educational models will not be able to cope with the increased needs for cross-disciplinary skills and will have to be revisited.
Finally, we must realize that the knowledge society is becoming global, bringing new challenges and new opportunities. In order to limit the progress of the digital divide between those who have access to these new tools and those who don't, we will have to learn how to better share knowledge, and make it relevant to multiple contexts, in order to solve real and urgent problems, and in particular those of the health systems. For example, it is likely that biomedical informatics, e-health and telemedicine will enable new solutions for the current healthcare workforce crisis, helping to train, inform and support healthcare professionals and patients in the poorest and most remote parts of the world, where they are most needed [55].
Enthused by these new promises, we should always keep in mind that the overarching goal of our efforts, from fundamental research to the bedside activities, from molecules to populations, is to improve the health and quality of life of the people of the world.
8. From Molecules to Populations Is Only One Dimension of Health and Biomedical Informatics (by William Hersh)
The paper by Kuhn et al. [1] describing the spectrum of health and biomedical informatics provides an excellent elucidation of the subject domains that describe our field. But the subject domain is only one dimension of informatics, and other important dimensions must be described and explored. In my commentary, I will set forth my own view of informatics, health and biomedical informatics, and the dimensions that the field covers.
First, what exactly is informatics? The paper discusses this only briefly, noting but expressing some dissent the European view that informatics is fundamentally computer science. I am glad to see this view changing in Europe and beyond. My view of informatics is that it is fundamentally about information, in particular what humans do with it and how they apply technology to improve its use for improving the human condition. Informatics is an integrative discipline, drawing upon areas such as information and computational sciences, business and management, and other fields, but also deeply rooted in a subject domain. In the field of health and biomedical informatics, the subject domains range from biology to medicine to personal and public health.
All branches of health and biomedical informatics are heterogeneous yet have a common intellectual core. The bioinformatician who analyzes gene expression microarray data may seem to have little in common with the clinical informatician who is trying to reconcile with highly interrupted workflow of clinical care with collecting high-quality information that can be used not only for better patient care, but also to drive decision support systems and quality assessment. Likewise, a consumer health informatician might be focused on helping an individual maintain optimal health, while the public health informatician is likely to be focused on monitoring risk factors for disease in a community.
Yet all of these areas of health and biomedical informatics have common underlying themes. All are focused on the optimal collection and use of information. All would benefit from technology systems that have optimal usability, facilitate collection and use of high-quality data, and aim for interoperability based on the best standards. All require attention to the larger contexts and human organizations in which they are used, whether biomedical research organizations, health care delivery systems, or public health agencies.
The paper by Kuhn et al. acknowledges that all subject domains of biomedical informatics have related areas, whether the statistical methods of bioinformatics, the people and organizational issues of medical informatics, or the social and economic aspects of public health. I would argue that these related areas are not necessarily limited to any particular subject domain. Examples include the application of qualitative methods to bioinformatics [56] and the need to be cognizant of genomics (e.g., single-nucleotide polymorphisms or SNPs) and clinical data quality issues in genomewide association studies [57].
It is thus imperative for us to move beyond arguing what adjective should precede informatics (e.g., bio-, medical, consumer health, etc.) and instead focus on the core attributes that unite all aspects of informatics and how we apply them in health and biomedical informatics. Our discipline is indeed interdisciplinary, and some of its key attributes reflect that. Informatics is integrative, drawing on computational and information sciences as well as business and management sciences, yet firmly rooted in a deep understanding of the discipline in which it is applied, be it biology, medicine, or health.
Our academic departments must recognize this fundamental undercurrent of all informatics. Our educational programs should teach from this perspective. Not every health and biomedical informatics department or degree program must cover the entire domain perspective, but they should perform their research, teaching, and service from the viewpoint of informatics. Likewise, their educational programs should recognize there is no single career pathway within the field. What an informatician does as a job is a function both of what he or she did before entering training and what knowledge and skills he or she gained from that training.
The 21st century provides exciting opportunities in health and biomedical informatics. Improvements in information technology provide us a growing ability to use information to improve human health at the personal, health care, and public health levels. This will require research and educational programs that acknowledge the core similarities across the subject domains of health and biomedical informatics and train new practitioners and academicians in this point of view.
9. The Value Chain “from Bench to Bedside” (by Yunkap Kwankam)
The paper of Dr. Klaus Kuhn et al. [1] is well documented (researched) and clearly written. It captures the essence of the broad spectrum of issues spanning the continuum from molecular genetics to public health policy. The fact that it elaborates on the quite intuitive value of interdisciplinary research in health informatics, is itself indicative of the imperviousness of the silos into which research has fallen. The reaffirmation is thus very welcome.
And although the consultation on creating the graduate program was local - limited to Germany - the challenges discussed cover a variety of socio-political and economic contexts, and thus the paper is of much broader relevance than to single a typology of health system context.
9.1 Assessment of Health Informatics
The paper mentions the importance of assessment and the dearth of robust methodologies for such assessments. This is the crux of the matter. Methodological improvements in the assessment of informatics are needed to convincingly chart influence pathways from health informatics interventions to health intermediate and final outcomes. This is the key to unlocking funding for the very promising research described and support for the marketing, deployment and use of the fruits of such research. Until the return on investment, or return on value, is demonstrated, the funding levels needed to sustain interdisciplinary efforts will continue to be a challenge and thus an inhibitor to the change in culture within disciplines that the paper calls for.
Funding for public health informatics is in competition with other priorities, and this competition is especially fierce in resource-challenged health systems. Health, as a production function, shows a number of variables, water and sanitation, for example, accounting for nearly 10% of the global burden of disease. A 2008 WHO report estimates the economic benefits of investing in drinking-water and sanitation in several forms: “health-care savings of US$ 7 billion a year for health agencies and US$ 340 million for individuals; 320 million productive days gained each year in the 15- to 59-year age group, an extra 272 million school attendance days a year, and an added 1.5 billion healthy days for children under five years of age, together representing productivity gains of US$ 9.9 billion a year; time savings resulting from more convenient drinking-water and sanitation services, totaling 20 billion working days a year, giving a productivity payback of some US$ 63 billion a year.” [58]. The above figures are taken from a study which shows a total payback of US$ 84 billion a year from the US$ 11.3 billion per year investment needed to meet the drinking-water and sanitation target of the Millennium Development Goals [59].
Health informatics would need to show similar, or better benefits, in order to get a fare share of limited budgets.
9.2 Translating Knowledge into Policy and Action
The paper lays heavy emphasis on greater levels of sophistication in research for scientific discovery. However, one could argue that the weakest link in the research continuum from discovery to dissemination and deployment, is perhaps in the latter phases of this chain. Therefore, there needs to be a balance between efforts aimed at discovery and those targeted at the so called “know-do gap” - the gulf between what is known and what is done in policy and practice. Again, interdisciplinary training, which the paper advocates, would strengthen research into “technology enhanced knowledge translation” [60]. The field examines the role that ICT can play in the actions of individuals, as well as systemic factors that militate in favor of successful transformation of available information and knowledge into action. It also looks at what informatics tools need to be devised for capturing and sharing experiential (or tacit) knowledge, which unfortunately is compartmentalized in individuals. Can health informatics networks in support of communities of practice serve as a model for breaking down these silos, so as to promote sharing of available tacit knowledge? Can such networks improve the use of experiential knowledge on a systematic basis within health systems?
ICT can remove distance and time barriers to the flow of information and knowledge for health and help ensure that our collective knowledge is brought to bear effectively on health problems in individual countries, as well as globally. It would require a system where all decision-making in health is supported by an ICT-mediated knowledge-coupling system which builds on Weed's vision [61] as adapted by Kwankam et al. [62] and ensures that: a) all relevant options known to the health sciences are readily available for consideration; b) specific features of the situation at hand that bear on the discrimination among these options are taken into account; c) appropriate associations are made between the specific features of the situation and the many options; and d) the right technology is deployed and local capacity developed to permit access to the information.
9.3 Building on the Collective Wisdom
Several recent meetings have raised the issue of an international registry for informatics research/trials - to provide a repository of research information/experience and the potential to build on successes while learning from the errors of one and all.
The paper's broad scope also covers the role that informatics can play in empowering citizens to contribute to their health. The authors thus encourage one to hope that such thinking also offers an opportunity to focus less on health as the absence of disease, and the attendant emphasis on disease mechanisms, and more on the WHO vision of an ecological balance between the physical, mental and social dimensions of life.
The paper concludes that “it is only through having experts in one scientific discipline who have a profound understanding of the other disciplines' terminology and scientific culture, that true inter-disciplinarity can develop …”. Such interdisciplinary understanding would greatly facilitate visualizing and understand the big picture. Then the boundary conditions that are necessary for information and knowledge exchange between disciplines, and between sub-disciplines within disciplines, in the value chain that leads from bench to improved health, may be better understood and managed.
10. Envisioning the Future - Informatics and Collaboration (by Nancy Lorenzi)
In Lewis Carroll's classic book, Alice in Wonderland [63], Alice comes to a fork in the road with two paths leading in different directions. Confronted by a Cheshire cat she asks: “Which path should I take.” The response from the Cheshire cat is: “Well, that depends on where you want to end up?” Alice said she did not know. The Cheshire cat responds: “If you don't know where you want to go, it doesn't matter which path you take.”
Without vision we are both unclear about our direction and at times have conflicting directions. This makes it difficult to formulate plans, objectives, goals, actions, and no way to measure results. Unless we know where we need to go, we cannot create the path to the future
The Informatics and Medicine: From Molecules to Population article presents an outstanding overview of the current progress in medicine, bioinformatics and biology informatics, biomedical engineering health informatics and eHealth, and public health, life sciences, public health, life sciences and public health informatics. This article will become an instant cornerstone classic article not only for its overview, but for its challenges and directions. Congratulations to the multiple authors for creating this article that is a world-wide guide.
I titled my commentary “Envisioning the Future - Informatics and Collaboration”. The phrase “envisioning the future” characterizes the challenge that we face in achieving the overall picture painted in the vision the Informatics and Medicine: From Molecules to Population article creates. The sub-title “Informatics and Collaboration” not only supports that informatics will be “the most important driver and mediator for innovation” as stated in the article, but stresses that we need collaboration to be successful.
One organization that is prepared to support collaboration is the International Medical Informatics Association (IMIA). Three of IMIA's goals include:
promote informatics in health care and research in health, bio and medical informatics;
advance and nurture international cooperation;
further the dissemination and exchange of knowledge, information and technology.
IMIA created a strategic plan (Towards IMIA 2015 [64-67]). Knowledge is the central core of IMIA's strategies, interactions and efforts. The plan next focuses on science, portraying IMIA members' connection and integration with the science and discovery of informatics. The next connection is the application of scientific discoveries, including the multiple questions and issues that are created and disseminated in informatics. This is followed by IMIA's impact, referring to the potential impact that IMIA and its members can have on governments, nations, outcomes, health professionals, and all other stakeholders. The last major focus represents IMIA's interactions with individuals, citizen organizations, personal health involvement, dissemination and acceptance, enabling personal responsibility, and public/personal health.
The second dimension of IMIA's Strategic Plan represents six key sectors that IMIA as an international association is prepared to facilitate or work with others to effectively address. The six sectors are:
health improvement;
research/science (including how we understand and create evidence to support health);
the behavioral responsibility (ethics) that refers to our ethical and social responsibility;
education (including best practices in educating ourselves and others);
the multiple types of relationships (communications and connections to build relationships among stakeholders); and
the equity of IMIA, our obligation to share, distribute and disseminate.
We stand at the crossroads of tomorrow, compelled to address the challenges outlined in the article and impact of our multiple efforts and the visions they enable.
Inherent in IMIA's role is to bring together, from a global perspective, scientists, researchers, users, vendors, developers, consultants and suppliers in an environment of cooperation and sharing to research and develop the concepts needed to support the organizations of the world seeking technology as transformational. Through its many publications (Methods of Information in Medicine, International Journal of Medical Information and Yearbook of Medical Informatics) and electronic communication mechanisms IMIA can be a major disseminator of the knowledge created. As an organization committed to promoting best practice in the use of information and communication technologies within biomedical informatics and in health and healthcare, IMIA will ensure that it uses and promotes best practice in its own use of technology as a transformational strategic asset.
We stand looking at the future portrayed by the Informatics and Medicine article. We have a vision. If we work independently toward various isolated goals we will lose the opportunity to work together to create the synergy needed for reaching the desired state. This is an excellent time for international cooperation.
11. Nanomedicine and Regenerative Medicine Pose New Challenges for Biomedical Informatics (by Fernando Martin-Sanchez)
The reading and study of the paper of Kuhn et al. [1] has represented a particularly motivating and scientifically enriching task. After several years of working on aspects related with the analysis and implementation of the synergy between medical informatics and bioinformatics, this document represents the most complete updated review of the research challenges in each of the four areas that are accepted as constituent of biomedical informatics (BMI). Furthermore, these four disciplines are not described independently, instead a thorough analysis of their mutual relations is provided. The analysis of the connections between BMI and biomedical engineering results especially interesting because this is a topic that has given rise to some controversial opinions in the past. The authors provide here a framework that can be very useful to facilitate a reciprocal collaboration between experts in both fields and to define some common ground (such as image processing or modeling and simulation of biological entities and processes).
It is also very valuable the effort made by the authors to provide a model for interdisciplinary education that it is clearly oriented towards facilitating translational research. I fully agree with their claim that the new generation of scientists should have to be exposed to (at least) two of the core disciplines at early stages of education. Furthermore, I believe that the integrative approach that has inspired the authors to design the new Graduate School will become a reference and will be followed by other academic centers.
Indeed, there is no a major criticism to the paper from my side, however, taking into account that several outstanding bioengineers have participated in the work leading to this paper, I believe that it would have been important to raise the issue of nanotechnology and regenerative medicine since they pose new challenges for BMI. It is not my intent to consider these issues in depth in this brief commentary. Rather, I will point out some considerations and let the reader become more informed and interested about these topics, particularly with reference to their complementarity with the paper authors' design of educational programs.
11.1 Nanomedicine and Regenerative Medicine Represent New Trends beyond Genomic Medicine
Although the paper only mentions nanotechnology on one occasion in section 2, nanomedicine and regenerative medicine are recognized to be among the most promising trends in medicine for the future. Nanomedicine is defined as the use of nanoscale tools and components for the diagnosis, prevention and treatment of diseases and for understanding their pathophysiology (European Science Foundation, Nov. 2005). Regenerative medicine seeks to develop functional cell, tissue, and organ substitutes to repair, replace or enhance biological function that has been lost due to congenital abnormalities, injury, disease, or aging (NIH Definition, NIBIB, June 2004).
Interestingly, while genomic medicine is based on the use of molecular information to design new approaches to promote health, and prevent, diagnose, cure and treat disease, nanomedicine and regenerative medicine go beyond that point, in the sense that they can entail an intervention on the biological structure of the human being. It is my belief that these two fields pose new challenges for informatics beyond those addressed under the realm of genomic medicine.
11.2 Impacts of these New Trends that Can Be Envisioned in Every Facet of Healthcare
Nowadays the number of clinical applications of nanotechnology is increasing with research at the nanoscale providing important information prior to clinical application. Just as mentioned above, we are likely to see nanomedicine impacting on areas such as biomedical research, prevention, diagnosis and therapy [68].
Prevention and diagnosis - All the new advances in nanotechnology are encouraging the scientific community, especially in biomedicine, to use the `nanoscope' that will allow them to see a new scale of genomic, phenotypic and environmental data to integrate with the information already available. As an example, the next generation of DNA sequencers makes use of beads and other nanotechnologies. Nanosensors and nanodevices will permit to assess the different positive and negative environmental factors that affect an individual's risk to suffer from a disease. New in vitro diagnostic tests and miniaturized imaging systems will provide more sensitive detection methods.
Therapy - New nanostructures will be used as drugs. Novel methods of drug delivery systems consisting of anti-cancer products bound to nanoparticles such as buckyballs, nanocapsules and dendrimers are already a reality. Imaging techniques will be used to monitor drug release or for patient's follow-up. Stem cells may provide tissue for transplants in the context of degenerative diseases. Finally regenerative medicine will allow the manufacture of new artificial tissues or organs, or the use of nanotubes and nanofibers to build scaffolds where cells from different organs can grow.
Nevertheless, some of the recently developed nanoparticles may have negative side effects. For instance, an article in Nature Nanotechnology has recently reported that some forms of carbon nanotubes could be as harmful if inhaled in sufficient quantities [69]. This fact justifies the need of careful data handling in clinical trials in this area.
11.3 Nanoinformatics Could Represent a New Subdiscipline within Biomedical Informatics
Nanotechnology requires the contribution of informatics to process all the knowledge that is being generated at the nano level and to integrate it with the biomedical (phenotypic, genotypic and environmental) data. Nanomedicine gathers and deals with large volumes of complex data, linked with external sources and usually distributed in heterogeneous locations.
Nanoinformatics involves the research and development of effective tools/technologies for collecting, standardizing, sharing, analyzing and visualizing the vast amounts of data and information relevant to the nanoscale science in several areas such as literature, physico-chemical properties, biological and toxicological interactions and clinical effects [70].
Several requirements for BMI come from the need of improved tools for designing, modeling, and visualizing the new nanomaterials and scaffolds for tissue engineering. Also, new databases will have to be designed to store physical, chemical and biological properties of nanotechnology developments. Semantic interoperability will have to be granted not only between nano resources, but also between them and the existing medical terminology and coding systems. Biomedical informatics can support regenerative medicine through the application of tools and information systems to characterize the molecules involved in differentiation mechanisms, including growth factors, hormones, cytokines or integrins.
ACTION-Grid is a new research project funded by the European Commission (2008-2009) on healthcare information systems based on grid capabilities and nano/bio/medical informatics. This project, coordinated by Prof. Maojo from the Universidad Politécnica de Madrid and our own group has as its main objectives to analyze synergies between biomedical informatics and nanoinformatics and to combine these results with data from an inventory of grid/nano/bio/medical methods and services developed by the consortium [71].
11.4 In Conclusion
Nanomedicine and regenerative medicine open new avenues for research in biomedical informatics methods and tools. Just as the advances in “-omics” research brought about the connection of medical informatics with the molecular domain, is BMI ready now for addressing the nano world and expanding its scope down to the atomic level as shown in Figure 2?
None of my views expressed in this commentary should be interpreted as a critic to the paper by Kuhn et al. On the contrary, an educational program such as the one described in the paper by our colleagues from Munich, that is based on interdisciplinarity and with a clear translational vocation, is placed in the best position to face the new challenges related to information processing in medicine, whether they come from the side of nanotechnology or from any other new development that may arise in the future.
In this regard, a new generation of scientists knowledgeable about nanotechnology will be essential to manage this new information and efficiently integrate it with biomedical data from the atomic to the populational level to translate all these findings into better healthcare.
12. The Need to Create the Frame for Interdisciplinary Collaboration (by George Mihalas)
Biomedical informatics is today a field with one of the highest rates of development. New techniques or devices, new approach or methods, new applications or solutions are reported every day [1]. Such an avalanche of news needs a systematic work for classifying and stratifying all accumulated data and knowledge. The most natural approach in classification would start from the structural level of the studied system [72]. And this approach has been adopted also by Kuhn and his collaborators [1] who emphasized this view even in the title: “From Molecules to Population”. Their excellent paper is fully comprehensive by counting all topics of research, brings some refinement in description and updates the actual trends. It is worth to make here some short comments concerning the research challenges on each level.
12.1 Bio-silico Interfacing
I would start my comments by noting the original approach in the second chapter “The Overall Picture: Where Do We Stand and Where Do We Go”, with a detailed list of technical trends in computer science and adjacent domains which will bring a significant impact biomedical informatics. We can add here the interdisciplinary research (biophysics and computer science) on the direct information transfer between biological system and computers [73]. The potential applications are tremendous and still seem close to“science-fiction”.
12.2 Neuroinformatics
During the nineties most prospective views about medical informatics research used to consider bioinformatics and neuroinformatics as most promising [74]. The previsions on bioinformatics turned out to be true. However, the chapters on neuroinformatics are now rarely present. The reason might be that the impact of neuroinformatics research would rather be on cognitive sciences than on medical sciences. And the same might be true about “affective computing” [75]. However, applications in neurosciences and psychology, with their “medical” shadows - neurology and psychiatry - , show that the connections to biomedical informatics are strong enough and the integrative view, which has been repeatedly mentioned by the authors, would become even more consistent by including these items too.
12.3 Simulations in System Biology and Virtual Physiological Human
Another welcomed feature in the article is the specific reference and the detailed presentation of “Informatics for Biomedical Engineering”, a topic often left on a second place or treated superficially. The research challenges cover, indeed, several directions, requiring various tools. And when we talk about new informatics tools in cell biology we must mention the work of Masaru Tomita and his co-workers [76] on the “virtual cell” - a package for computer simulation of cellular processes, dedicated software developed for this purpose [77]. We can expect that specialized software or even new theoretical models will be developed for each level. On the next structural level we have to mention the Physiome Project, initiated by Peter Hunter [78], followed by the Europhysiome Project, and continued by the Virtual Physiological Human Project of the European Commission [79].
12.4 Integration and the Role of Professional Organizations
Various aspects of integration have been discussed in the paper and there are also several other studies dedicated to integration (refs. 9, 10, 12, 17, 37, 39 of [1]). The emphasis on integration is understandable: the properties of a level are different from a simple sum of the properties of lower component levels! Some recent events organized by the European Federation for Medical Informatics EFMI had topics dedicated to integration of biomedical information [80, 81].
Actually the integrative view supposes a quite complex approach and here it is the origin of the need to create the frame for interdisciplinary collaboration and provide an education which crosses the boundaries - as so well is presented in the paper in chapter 4. I fully share the view of the authors and do consider that biomedical and health informatics professional organizations, like EFMI or IMIA (International Medical Informatics Association) should get involved in creating the appropriate collaborative frame and contribute to educational programs, following the good example of the 10×10 program of the American Medical Informatics Association AMIA (ref. 18 of [1]).
13. The Need for a Human Clinome Project (by Yuval Shahar)
The “Molecules to Populations” paper by Kuhn et al. is a highly commendable effort at a through, in-depth analysis of the need for multidisciplinary collaboration in the 21st century between informatics, as an area of scientific endeavor, and several specific subareas of medicine and biology, as other such areas. I would like to comment on some of its key strengths as well as on several important key challenges to be faced that should be added to its research challenges list.
First, regarding the key strengths and main significance of the paper: I had found both the descriptive insights provided from this analysis, and the specific educational structural recommendations implied by these insights, to be quite invigorating, and potentially highly beneficial. In particular, the authors emphasize that only through experts in one discipline who profoundly understand the conceptual world of another discipline can true multidisciplinary research develop. This emphasis is very important, and is certainly evident to multidisciplinary researchers, but unfortunately is not as obvious to decision makers in education as one would like it to be. One often encounters the view that, for example, having a well trained computer scientist or informatician work with biologists or clinicians is sufficient for bringing about new breakthroughs in bioinformatics or medical informatics; similar views are often held in the case of other disciplines. But, as the authors point out, the various sub-cultures of the disciplines studied by Kuhn et al. have been highly resilient to change or to integration. Only by what the authors term “boundary breaking agents”, i.e., personal examples of multidisciplinary researchers that the students meet during their training, can true interdisciplinary understanding and research exist.
A particularly good example out of the several potential interdisciplinary collaborations suggested by the authors, is, in my opinion, the need to strengthen the links among bioengineering and medical informatics. A specific example, not explicitly discussed by the authors but probably on their mind, is the possibility of developing a “smart medical home”, which monitors its residents, alerts them or specific care centers when unusual patterns are detected (e.g., an elderly person falls, or seems to have a heart attack). Developing such a smart home requires understanding of both the multiple sophisticated (and possibly quite new) sensors involved, as well as development of intelligent computational methods for analyzing the huge volumes of data emerging from these sensors, and for continuously integrating these data with up-to-date clinical and epidemiological knowledge.
Second, regarding several of the areas I would like to see more strongly emphasized as part of the key research challenges, at least as a part of any interdisciplinary research program that includes as one of its components the area of medical informatics: I would like list three such challenges, although they are somewhat linked.
1) The first grand challenge for a multidisciplinary collaboration is the creation of a universal, formal, computationally accessible medical knowledge base. Much of the collaboration among areas such as clinical medicine, clinical research, public health, and medical informatics, can and should be distilled into a set of formal representations of declarative and procedural knowledge that would be stored in a universally accessible (to humans and machines) knowledge base. That is, insights regarding meaningful [declarative] patterns of both individual (clinical) or population (epidemiological) data, and, most importantly, the best state-of-the-art [procedural] methods, protocols, guidelines, and care plans, to deal with such patterns, can and should be organized, specified, stored, and maintained within a universally accessible digital library, using a machine-comprehensible format (including the use of a set of ontological and terminological standards) that supports maintenance, use, reuse, and sharing of the knowledge.
I call such a continuously changing library of declarative and procedural clinical knowledge “the Human Clinome Project”, in homage to the Human Genome project - or perhaps it should be termed the Human Cli-Knowme project, since it would encompass all currently known declarative and procedural human knowledge that can be represented within and accessed by computational means.
A particular section of the Human Clinome project that I have in mind as a good specific starting point is a worldwide machine-comprehensible digital library of procedural knowledge, namely, clinical guidelines and their somewhat more rigorous version, clinical protocols. These guidelines have been shown to be highly beneficial with respect to both improving the quality of care [82] and reducing its cost; it is also clear that to be effective, the guidelines must be integrated within the clinician's workflow [83]. Free-text and even somewhat structured guideline libraries exist and are accessible through the World-Wide Web. However, to be truly effective, guidelines must be continuously updated and universally accessible in a machine-comprehensible way, so that they can be automatically applied to the relevant patient (or patient population). One such attempt at a digital guideline architecture is the DeGeL project [84], which includes a comprehensive methodology for specification, maintenance, search, retrieval, and application of clinical guidelines, using a hybrid methodology that support several intermediate formats on the way from a free-text-based representation to a completely formal, executable format. The collaborative methodology for guideline specification was recently evaluated in a multinational collaboration and found to be feasible [85]. Of course, many sub-parts of such an architecture require further research and enhancement; multiple researchers throughout the medical informatics community are working on various aspects of this challenging problem, such as how to expressively represent the guidelines, or how to automatically verify and validate the knowledge expressed within them.
Such a grand challenge would bring together many of the disciplines mentioned by the authors of Kuhn et al.'s paper, and enforce true collaboration to be successful.
2) Much of the declarative biomedical knowledge necessary for better management of patients, in particular, chronic patients (the care of which is responsible for about 80% of the health care costs in developed countries), such as might be part of the Human Clinome project, should be acquired from analysis of massive amounts of data of patients monitored longitudinally for significant amounts of time (i.e., often, many years), to mine meaningful patterns from the data, using pre-existing clinical knowledge. In other words, we need to continuously perform massive, distributed, intelligent temporal data mining. Indeed, it has been recently suggested, although without much emphasis on the temporal aspect, that “clinarrays” (influenced by microarrays) might be constructed from analyzing large amounts of population-based laboratory data, possibly correlating it with biological data, so as to suggest new ways for disease subtyping [86]. However, adding the temporal dimension as well as the effect of using existing medical ontologies and knowledge bases to better interpret the data would shift the emphasis towards a massive, large scale, continuous clinical trial that uses and reuses the world's increasingly voluminous electronic medical record data base. Needless to say, ontological and terminological standards are an absolute prerequisite in the case of accessing clinical data as they are in the case of accessing medical knowledge.
Such an analysis would better identify meaningful [temporal] patterns and associations within and among features of diseases such as diabetes, hypertension, cerebral stroke, AIDS, etc. The goal would be to discover the “natural” course of such diseases, to identify meaningful temporal clusters and patient types, to detect patterns predictive of certain intermediate and final outcomes, to improve best practice guidelines (i.e., affect also the procedural aspect of the Human Clinome library), and to enhance our epidemiological knowledge and preventive care understanding.
Such a challenge requires and fosters close collaboration among clinicians, epidemiologists, informaticians, mathematicians, computer scientists, biomedical engineers (consider the effect of a “smart medical home” technology on the source of data available for such a project), biologists, and other disciplines.
3) One aspect I would like to see better represented in the context of both individual and public health care (and it could be eventually part of the universal procedural knowledge base) is an emphasis on medical decision support that considers individual, customizable, patient preferences as an inherent part of each decision that might include an option for deliberative thinking.
Examples include genetic consultation (e.g., the value of early knowledge of potential serious disabilities of the baby, versus the risk of spontaneous abortion of a healthy baby), therapy of hypercholesterolemia, hypertension, and depression, oncological care (e.g., weighing the benefits and costs of surgery, chemotherapy, and irradiation), and many other situations that are not life-threatening in an immediate fashion, enable a certain amount of deliberation on the side of the patient and care provider, and might be potentially affected by patient preferences. Such an endeavor is not only useful; it is ethically imperative, even if some of the patients might elect to not use it, delegating the responsibility of deciding on the best course of action to their care provider [87].
Again, effective solution of such a challenging problem requires and fosters the collaboration and deep mutual understanding of care providers, decision analysts, game theorists, behavioral scientists, economists, computational scientists, and other medical, engineering, and computational disciplines. Typical challenging research tasks include finding and developing increasingly effective ways to elicit patient preferences [88], and efficiently integrating such preferences within the overall clinical and public health care workflow [89].
In summary, I welcome the discussion started by Kuhn et al. and its stimulating educational implications, while suggesting a particular set of challenges that we might focus on, especially in the area of enhancing our understanding of individual and population-based patient care.
14. Collaboration of Specialists Is more Practical than to Find a Genius (by Katsuhiko Takabayashi)
Current medical and health care domains can be divided into several fields from molecular medicine to public health and in each field informatics plays a significant role. Kuhn et al. described precisely each relationship and explained the importance of interdisciplinary collaboration and education in their review. Kuhn realized the substantial change from hospital information systems to electric health records (EHRs) in the early days with distinguished ability [90]. Here he classified informatics into four areas for corresponding medicine and health care; bioinformatics and systems biology, informatics for biomedical engineering, health informatics and eHealth, and public health informatics in order from the point of micro to the mass world. In fact it is incredible to do without informatics in all fields nowadays and he also provided their perspectives respectively.
As for bioinformatics and systems biology, there are large amounts of data in omic (genomics, transcriptomics, proteomics and phenomics) world [91, 92]. Because genomic and proteomic data will explode to astronomical numbers of information in the very near future, researchers cannot work without informatics to handle these data and to know their relations. Since even SNPs which just express point mutations exist in one million per person, or there are 22,000 genes and more than 100,000 proteomes, it is quite easy to imagine numerous combinations existing between them to be explored. Thus sophisticated and useful information technology and powerful software will contribute to a great progress in molecular medicine. Especially data mining techniques [93] will be very useful tools for translational research to connect omic data and clinical phenomenon or contribution to diagnosis and selection of treatment with omics data. Therefore we must provide suitable environments to use them [94]. As it will bring reasonable profits in this field, many industries will emerge to deal with them as venture companies as in Silicon valley.
Healthcare information is also a field for blue chip industries, because eHealth provides a large portion of healthcare expenditure [95] in this decade as Kuhn mentioned. Electronic medical records (EMRs) will certainly advance in the near future, and EHRs hold many dreams as integration of not only EMR but also with many other health areas or even other information not related to health. Some governments consider an electronic post office box or an ATM card system for the integration of pensions, EMR of several hospitals, health checkup data, health insurance and so on. This personal health records (PHR) concept [96] is also open to industries as well, and all data of one individual about not only PHR but also various information would be stored. Of course data of PHR must be strictly limited to personal use because it includes confidential information. However, when some common parts can be utilized as EHR in broad terms, it will be reutilized in many other ways apart from personal use. To achieve it, preparing the rules and guidelines such as access control [97] and protection systems of privacy as well as many sophisticated systems in compliance with regulatory requirements are crucial. Additionally even after de-identification, proprietary of the data to use is not clearly defined in law, though it is very important in the near future for transverse study. If someone would not accept one's data to be used for such a study, it will make some bias in results. Therefore all data should be enrolled for special studies, which is controversial in regard to individual rights.
As Kuhn emphasized, digital data have become a core element of research, knowledge generation and knowledge management. EMRs and EHRs are ultimate targets for automated research like text mining [98]. We would find drug interactions or potential effects and side effects quite easily from medical records with them. Sometimes we need the tools to transform original data into other expressions in order to use them more easily. For example, time-oriented clinical data such as laboratory findings or prescriptions will be perhaps transformed into other expressions for easy manipulation and accurate enhancement of clinical assessment such as temporal abstraction [99]. There are only few practical tools at the moment but we will obtain universal tools after trial and error in the future. Moreover, for these trials, we also need long data storage beyond facilities. With them we can complete one's whole life data for PHR and also to compare with or integrate with omic (genome or proteome) data, which will be a very strong method for translational studies. In these days retrospective studies are not well estimated in medical journals. However when we expect the effects or outcome of some treatment over the long term such as ten years or more, we have to wait for the results many years, and expected results would not be obtained because of changes of treatment or other circumstances in that period. From this point of view, the retrospective study is very important and efficient when informatics can provide enough huge data to be analyzed.
Public health informatics seems to have more weight than any informatics in other fields of medicine or health care, because the results of analysis of information in this field directly affects critical politics such as global warming, biofuels, or global food shortage, which relates to the fate of humanity. Since public health informatics should include all information comprehensively with absolute accuracy, it is expensive to create and maintain vital information. Even though, we cannot completely entrust industries with these works, because the results might be crucial in deciding our destiny.
Finally, in all informatics fields, data value increases when integrated under the guarantee of their credibility in quality and they are now showing their whole appearance as the name of truth in front of us by integrating. However they might be so huge like an ocean or a big forest. Unless we have strong tools to discover their relations and offer them before us, we cannot say that we can really see them, though it might be a vicious cycle between the data and data mining tools.
Kuhn mentioned how vital it is for generations of scientists who can combine knowledge and skills from both medicine and informatics and emphasized the importance of the interdisciplinary education in early phases as well as interdisciplinary collaboration. He started to strengthen the collaboration and structured interdisciplinary education in encompassing medicine, informatics, bioinformatics, biology and system biology, engineering, health informatics and public health in Munich. In eastern Asian countries like Japan, different environments from those of the European countries, most researches in clinical medicine have been proceeding in the departments of medical informatics at national university hospitals. They consist of medical doctors and specialists of informatics or computer sciences and there were few departments for bioinformatics in other faculties. This might mean that they are still in the course of western countries in the old days where bioinformatics was not independent of medical school, or it might be as a result of different historical perspectives. At any rate they can work together without any restraint in the hospital at the moment. Some engineering students work together with medical doctors in our department at the hospital. In other fields of medicine such as molecular medicine, however, specialists for informatics come from school of engineering or physics. In summary, in eastern Asia, there is no strict boundary between specialties originated from Meister system and they seem to have less difficulty to collaborate in clinical medicine. Nevertheless it is not ideal because this is not intended systematized interdisciplinary collaboration.
Even in medicine or in informatics, there are no specialists in all fields, and therefore we need teamwork collaboration between medical doctors and specialists for the informatics field and others in various fields if necessary. There are a few people who are familiar with both fields because of graduation from both medical school and faculty of engineering or physics. However they are rare cases and even if one knows well in both fields, he cannot surpass two specialists who collaborate well unless he is a real genius. There is a proverb in Japan that god gives us only one talent. According to this proverb and taking into account of the very small numbers of geniuses in the world, good and successful collaboration of specialists of different disciplines will be more practical than to find a genius. One of the purposes of multidisciplinary education is understanding one's colleagues' work as well as knowing the position of one's specialty comprehensively in the beginning of one's education. It is also important to learn about laws and ethics in the fields as general matters in this education. Thus I believe most importantly that a key to success to collaborate in information and medicine is mutual respectability and generosity to their colleagues in different discipline. This spirit will be cultivated in early interdisciplinary education that Kuhn proposed.
15. Strategic Thinking Is Needed, Cost when the Research Results Are Transferred to Practice Is an Issue to Be Addressed (by Gio Wiederhold)
The article by Kuhn et al. [1] is impressive in its comprehensiveness. It also is frightening. The number of problems that require research, the multi-disciplinary cooperations needed to be successful in the interaction of informatics and medicine, the difficulties of demonstrating effectiveness, and the barriers to beneficial implementations are shown to be massive. While there may indeed be an urgent need to transfer research results to practice, strategic thinking is needed as well, as has been shown in simpler settings [100]. Cost is one issue to be addressed. We expected in the past ratios of research projects efforts to practical implementation to integration into practice of 1 : 7 : 25 [101], and little has been changed to improve this ratio. Medical informatics will have to depend on progress in software engineering to create usable software. We expect that new initiatives cited, as service-oriented architectures, will improve software development, but an early reliance on a technology that is not yet mature is currently frustrating efforts at the US Veterans Health Administration systems to update their medical record system (VistA) [102]. It is purely a coincidence, but also an illustration, that other Vistas are encountering development and acceptance problems as well [103]. Medical informatics cannot supplant computer software engineering (SWE) efforts but must take care in understanding when and what to exploit as part of biomedical engineering (BME).
The total cost of software-based solutions in any setting has to be budgeted properly. Computer science education serves us poorly there. Software maintenance costs run at about 15% of prior software investment costs and are due primarily to keep the software up-to-date as the external world changes around us [104]. These maintenance costs over time exceed initial development costs, and after some further time, exceed the benefits that software provides. This fact is the major reason for closing down apparently successful medical informatics projects, often surprising and frustrating the participants. Unfortunately, we do not teach our SWE students how to plan for these costs, nor do we teach them how to assess the potential economic benefits of the software [105].
Replicating successful local systems has been difficult in the past and remains hard. Early systems were tied to obsolescing technology, but more recent systems, as seen at Vanderbilt and the Palo Alto Medical Foundation have not spawned successors either [106]. There is more involved than technology, leadership is certainly one issue.
The hard issues of economics are cited in the beginning and the end of the paper, but do not pervade the discussions. The growth of IT spending at 12% year is taken as indication of importance, but is also a rate which is unsustainable in relation to national expenses in any country, especially as the support base of working taxable individuals decreases [1, Sec. 2 and Sec. 3.4.1]. At the same time the industrial tax base is diminishing, as companies find ways to move their intellectual property and the profits derived from that IP to tax havens with no or small health care costs [107]. Given the high cost of implementation, it is important to focus on large and costly populations where actual cost reductions are possible, an issue not always covered by cost-effectiveness arguments. Some disease-based categories are well recognized now, as diabetes. However most diabetics present multiple problems, are seen in diverse settings, and their records at each site tend to be incomplete. For information integration there is a benefit in that members of that patient group tend to travel less, so that local and regional integration can proceed before national and global record integration is achieved, and economic benefits can be realized as well as improved care [108]. The same pattern holds for many of the elderly population, who require a substantial fraction of our health care services. Cost-effectiveness is stressed in the paper, but transfer to practice requires a cost-benefit as well. That benefits are hard to demonstrate is recognized in the paper, but must be sought.
Moving to the opposite direction, personalized diagnoses and therapies, is an extremely attractive goal. But given financial constraints, systems to bring research results will require very careful strategies. How does one conduct clinical trials to determine efficacy of personalized care protocols? Presenting findings to clinicians will require innovation. Phrasing findings in terms of statistical evidence based on similar populations, as done now for medical versus surgical treatment choices conveys little insight or trust. Can the findings be conveyed using a “mechanistic” metabolic model, showing affected pathways[1, Sect. 3.1.3]? How can we present patient-specific information from probes [1, Sect. 3.2.1]? And how should patients be informed of conditions for which no known intervention exists? In general unfettered access to the patients' own medical information has been shown to be beneficial, but customization has been recommended as well [109]. Any approach supporting personalized treatment decisions requires novel software, incorporating experience from many disciplines. Such software will require regular updating, since our knowledge is bound to change for many years to come. How will software be maintained when personalized experience differs? Who will maintain the software at a reasonable cost?
Cooperative approaches are recommended in Section 3. Bureaucrats indeed feel safer when topics and funding can be constrained to recognized disciplines. Only if scientists and the public experience benefits will existing regulations and legal frameworks that limit interdisciplinary work be removed [1, Sec. 3.3.2]. Practical and beneficial examples will be important. Figure 2 only links abstract concepts; lessons learned from actual projects are needed as well. The gap between the “bench” and “bedside' communities is recognized. Social expectations limit collaboration as well. There is a serious, but largely unrecognized gap between the mathematically-based disciplines, where proofs, once validated, should stand forever, and the biological disciplines, where experiments have to be repeated to cover ever more of the variations that the living world presents. Scientists have at times disparaged scientific approaches used by others as being either naïve or imprecise. Engendering sympathy to the problems that both communities face in their research is a prerequisite to achieve cooperation at the individual level, creating a model that can then move up the organizational ladders. My personal sense is that directives imposed from above, mandating cooperation, do not create effective long-term collaborations.
One barrier, recognized in the paper, to transition of research to practice are privacy concerns [110]. Expecting guaranteed methods for securing privacy is too much to ask for [1, Sec. 3.3.1]. Approaches as k-anonymity, while already problematic, assume that there is no external information that can be exploited by an intruder. Lack of trust and the resulting rules will continue to hinder beneficial applications of health care information systems [Ness]. Involuntary adoption of EHR, as implied here, will cause politicians and the administrating bureaucrats to mandate approaches to privacy protection that are based on worst case scenarios, and give little choice to the patients. Questions posed in motivating surveys often reveal a bias by the questioner. How questions are phrased makes a great deal of difference, i.e. asking “Are you concerned about others accessing your private medical records?” will elicit a different response than“Are you willing to share information from your medical records so that others with similar problems can benefit?”. Some indication about patients' attitudes about privacy will be gleaned from the acceptance of web-based voluntary personal medical data systems, as Dossia, Google Health, and MS Healthvault. While all of these promise privacy, individual with deep concerns are sure not to participate. The immediate reason not to join is of course that with few participating health care providers the benefits of entering data and links are minimal.
In conclusion, even Norbert Wiener, cited in [1, Sect.2], will probably agree that we don't have the capability to move most of our research results into practice, and not only because of economic constraints. Our genetic and environmental history, even if it could be fully captured, does not fully determine who we are. For instance, what our brains do with all the inputs is yet quite un-known, and randomness remains [111]. Research is required to open up possibilities. On the horizon are systems that help the clinicians and the patients to interact effectively, to which research into the issues listed in this paper will contribute.
References
- 1.Kuhn KA, Knoll A, Mewes HW, Schwaiger M, et al. Informatics and medicine: from molecules to populations. Methods Inf Med. 2008;47:283–295. [PubMed] [Google Scholar]
- 2.Kuhn TS. The Structure of Scientific Revolutions. Univ of Chicago Press; Chicago: 1962. [Google Scholar]
- 3.Hartwell LH, Hopfield JJ, Leibler S, Murray AW. From molecular to modular cell biology. Nature. 1999;402(6761 Suppl):C47–52. doi: 10.1038/35011540. [DOI] [PubMed] [Google Scholar]
- 4.Butte AJ, Chen R. Finding disease-related genomic experiments within an international repository: first steps in translational bioinformatics. AMIA Annu SympProc. 2006:106–110. [PMC free article] [PubMed] [Google Scholar]
- 5.Blois MS. Medicine and the nature of vertical reasoning. N Engl J Med. 1988;318:847–851. doi: 10.1056/NEJM198803313181309. [DOI] [PubMed] [Google Scholar]
- 6.Tsafnat G. The Field Representation Language. J Biomed Inform. 2008;40:46–57. doi: 10.1016/j.jbi.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Coiera E. Guide to Health Informatics. 2nd Edition Hodder Arnold; London: 2003. [Google Scholar]
- 8.Berg M, Langenberg C, v d Berg I, Kwakkernaat J. Considerations for sociotechnical design: experiences with an electronic patient record in a clinical context. Int J Med Inform. 1998;52:243–251. doi: 10.1016/s1386-5056(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 9.Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–286. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Latour BWS, Salk J. Laboratory Life: The Construction of Scientific Facts. Princeton University Press; Princeton, NJ: 1986. [Google Scholar]
- 11.Ash JS, Anderson NR, Tarczy-Hornoch P. People and Organizational Issues in Research Systems Implementation. J Am Med Inform Assoc. 2008;15:283–289. doi: 10.1197/jamia.M2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trist EL. The evolution of sociotechnical systems as a conceptual framework and as an action research program. In: Van de Ven AH, Joyce WF, editors. Perspectives on organization design and behavior. John Wiley, Wiley-Inter-science; New York: 1981. pp. 19–75. [Google Scholar]
- 13.Coiera E. Getting technical about socio-technical systems science. Int J Med Inform. 2007;76:S98–S103. doi: 10.1016/j.ijmedinf.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Stephens J. Retelling stories, framing culture: traditional story and metanarratives in children's literature. Routledge Publ.; New York: 1998. [Google Scholar]
- 15.Lindemann Nelson H. Damaged identities, narrative repair. Cornell Univ. Press; Ithaca, NY: 2001. [Google Scholar]
- 16.Roesler C. The self in cyberspace. Identity formation in postmodern societies and Jung's Self as an objective psyche. J Anal Psychol. 2008;53:421–436. doi: 10.1111/j.1468-5922.2008.00735.x. [DOI] [PubMed] [Google Scholar]
- 17.Arnett JJ. The psychology of globalization. American Psychologist. 2002;57:774–783. doi: 10.1037/0003-066X.57.10.774. [DOI] [PubMed] [Google Scholar]
- 18.Harter LM, Japp PM, Beck CS. Narratives, health, and healing: communication theory, research, and practice. Routledge Publ.; New York: 2005. [Google Scholar]
- 19.Wald HS, Dube CE, Anthony DC. Untangling the Web - the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns. 2007;68:218–224. doi: 10.1016/j.pec.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 20.Demiris G. The diffusion of virtual communities in health care: concepts and challenges. Patient Educ Couns. 2006;62:178–188. doi: 10.1016/j.pec.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Greenhalgh T, Hurwitz B. Narrative based medicine: why study narrative? BMJ. 1999;318:48–504. doi: 10.1136/bmj.318.7175.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunter KM. The narratrive structure of medical knowledge. Princeton University Press; Princeton, NJ: 1991. Doctors' stories. [Google Scholar]
- 23.Sackett DL, Rosenberg WC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas P. General medical practitioners need to be aware of the theories on which our work depend. Ann Fam Med. 2006;4:450–454. doi: 10.1370/afm.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Revere D, Turner AM, Madhavan A, Rambo N, Bugni PF, Kimball A, Fuller SS. Understanding the information needs of public health practitioners: a literature review to inform design of an interactive digital knowledge management system. J Biomed Inform. 2007;40:410–421. doi: 10.1016/j.jbi.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Le Beux P, Fieschi M. Virtual biomedical universities and e-learning. Int J Med Inform. 2007;76:331–335. doi: 10.1016/S1386-5056(07)00060-3. [DOI] [PubMed] [Google Scholar]
- 27.Hiatt R, Samet J, Ness RB, for the American College of Epidemiology Policy Committee The role of the epidemiologist in clinical and translational science. Ann Epidemiol. 2006;16:409–410. doi: 10.1016/j.annepidem.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Zerhouni EA. Translational and clinical science - time for a new vision. N Engl J Med. 2005;353:1621–1623. doi: 10.1056/NEJMsb053723. [DOI] [PubMed] [Google Scholar]
- 29.van Mulligen EM, Cases M, Hettne K, et al. Training multidisciplinary biomedical informatics students: three years of experience. J Am Med Inform Assoc. 2008;15:246–254. doi: 10.1197/jamia.M2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Academy of Sciences . Facilitating Interdisciplinary Research. The National Academic Press; Washington, DC: 2005. [Google Scholar]
- 31.Aboelela SW, Larson E, Bakken S, et al. Defining interdisciplinary research: conclusions from a critical review of the literature. Health Serv Res. 2007;42:329–346. doi: 10.1111/j.1475-6773.2006.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rhoten D. Interdisciplinary Research: Trend or Transition. Items and Issues. 2004;5(1-2):6–11. [Google Scholar]
- 33.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity and transdisciplinarity in health research, services, education and policy: 1. Definitions, objectives, and evidence of effectiveness. Clin Invest Med. 2006;29:351–364. [PubMed] [Google Scholar]
- 34.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity, and transdisciplinarity in health research, services, education and policy: 2. Promotors, barriers, and strategies of enhancement. Clin Invest Med. 2007;30:E224–232. doi: 10.25011/cim.v30i6.2950. [DOI] [PubMed] [Google Scholar]
- 35.Choi BC, Pak AW. Multidisciplinarity, interdisciplinarity, and transdisciplinarity in health research, services, education and policy: 3. Discipline, inter-discipline distance, and selection of discipline. Clin Invest Med. 2008;31:E41–48. doi: 10.25011/cim.v31i1.3140. [DOI] [PubMed] [Google Scholar]
- 36.Martin-Sanchez F, Iakovidis I, Nørager S, et al. Synergy between medical informatics and bioinformatics: facilitating genomic medicine for future health care. J Biomed Inform. 2004;37:30–42. doi: 10.1016/j.jbi.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 37.Maojo V, Kulikowski C. Medical informatics and bioinformatics: integration or evolution through scientific crises? Methods Inf Med. 2006;45:474–482. [PubMed] [Google Scholar]
- 38.Kulikowski CA. The micro-macro spectrum of medical informatics challenges: from molecular medicine to transforming health care in a globalizing society. Methods Inf Med. 2002;41:20–24. [PubMed] [Google Scholar]
- 39.Maojo V, Martin-Sanchez F. Bioinformatics: towards new directions for public health. Methods Inf Med. 2004;43:208–214. [PubMed] [Google Scholar]
- 40.Lynch J. It's not easy being interdisciplinary. Int J Epidemiol. 2006;35:1119–1122. doi: 10.1093/ije/dyl200. [DOI] [PubMed] [Google Scholar]
- 41.Smith JA, Carey GE. What is the role of an inter-disciplinary researcher? Int J Epidemiol. 2007;36:690. doi: 10.1093/ije/dym106. [DOI] [PubMed] [Google Scholar]
- 42.Payton A, Zoback M. Crossing boundaries, hitting barriers: interdisciplinary research may be lauded, but it's not yet rewarded. Nature. 2007;445:950. [Google Scholar]
- 43.Carey G, Smith J. Jack of all-trades, master of none: postgraduate perspectives of interdisciplinary health research in Australia. BMC Health Services Res. 2007;7:1–15. doi: 10.1186/1472-6963-7-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lehmann CU, Altuwaijri MM, Li YC, Ball MJ, Haux R. Translational research in medical informatics or from theory to practice. A call for an applied informatics journal. Methods Inf Med. 2008;47:1–3. [PubMed] [Google Scholar]
- 45.Dhansay MA. The need for context-specific nutrition and health policies and interventions: the reality of disparities in socio-economic, health and nutritional status. S Afr J Clin Nutr. 2006;19:142–145. [Google Scholar]
- 46.Séguin B, Hardy B-J, Singer PA, Daar AS. Genomic medicine and developing countries: creating a room of their own. Nat Rev Genet. 2008;9:487–493. doi: 10.1038/nrg2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Séguin B, Hardy B, Singer PA, Daar AS. Bidil: recontextualizing the race debate. Pharmacogenomics J. 2008;8:169–173. doi: 10.1038/sj.tpj.6500489. [DOI] [PubMed] [Google Scholar]
- 48.Eriksson N, Pachter L, Mitsuya Y, et al. Viral population estimation using pyrosequencing. PLoS Comput Biol. 2008;4:e1000074. doi: 10.1371/journal.pcbi.1000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lengauer T, Sander O, Sierra S, et al. Bioinformatics prediction of HIV coreceptor usage. Nat Biotechnol. 2007;25:1407–1410. doi: 10.1038/nbt1371. [DOI] [PubMed] [Google Scholar]
- 50.Rocco MC. Science and technology integration for increased human potential and societal outcomes. Ann N Y Acad Sci. 2004;1013:1–16. doi: 10.1196/annals.1305.001. [DOI] [PubMed] [Google Scholar]
- 51.Hunter PJ, Crampin EJ, Nielsen PM. Bioinformatics, multiscale modeling and the IUPS physiome project. Brief Bioinform. 2008;9:333–343. doi: 10.1093/bib/bbn024. [DOI] [PubMed] [Google Scholar]
- 52.Anderson C. The end of theory: the data deluge makes the scientific method obsolete. Wired Magazine 23.06.2008, http://www.wired.com/science/discoveries/magazine/16-07/pb_theory. Last accessed July 10, 2008.
- 53.Mandl KD, Kohane IS. Tectonic shifts in the health information economy. New Engl J Med. 2008;358:1732–1737. doi: 10.1056/NEJMsb0800220. [DOI] [PubMed] [Google Scholar]
- 54.Berners-Lee T, Hall W, Hendler JA, O'Hara K, Shadbolt N, Weitzner DJ. A framework for web science. Foundations and Trends in Web Science. 2006;1:1–130. [Google Scholar]
- 55.Crisp N, Gawanas B, Sharp I, Task force for scaling up education and training for health workers Training the health workforce: scaling up, saving lives. The Lancet. 2008;371:689–691. doi: 10.1016/S0140-6736(08)60309-8. [DOI] [PubMed] [Google Scholar]
- 56.Anderson NR, Ash JS, Tarczy-Hornoch P. A qualitative study of the implementation of a bioinformatics tool in a biological research laboratory. Int J Med Inform. 2007;76:821–828. doi: 10.1016/j.ijmedinf.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 57.Pearson TA, Manolio TA. How to interpret a genome-wide association study. J Am Med Assoc. 2008;299:1335–1544. doi: 10.1001/jama.299.11.1335. [DOI] [PubMed] [Google Scholar]
- 58.Prüss-Üstün A, Bos R, Gore F, Bartram J. Safer water, better health: Costs, benefits and sustain-ability of interventions to protect and promote health. Geneva: WHO. 2008 [Google Scholar]
- 59.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM., Jr Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and metaanalysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 60.Morris J. BC Workshop. Wosk Center for Dialogue; Vancouver, BC: Mar 27-28, [Google Scholar]
- 61.Weed LL. New connections between medical knowledge and patient care. BMJ. 1997;315:231–235. doi: 10.1136/bmj.315.7102.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kwankam SY, Pablos-Mendez A, Kay M. eHealth. In: Unwin T, editor. ICT for Development. In press. [Google Scholar]
- 63.Carroll L. Alice's adventures in wonderland. 1865 [Google Scholar]
- 64.The IMIA Strategic Plan: Towards IMIA 2015. Available online at http://www.imia.org/strategic/index.lasso Last accessed July 10, 2008.
- 65.Murray PJ. Geissbuhler A, Kulikowski CA, editors. The IMIA strategic plan - towards IMIA 2015. IMIA Yearbook of Medical Informatics 2008. Methods Inf Med. 2008;47(Suppl 1):7–15. [PubMed] [Google Scholar]
- 66.Lorenzi NM, Murray PJ, Moura L, Goh HM, Huesing S, Martin-Sanchez F, Eisenberg F, Strachan H, The IMIA Strategic Planning Task Force Strategy in a fishbowl: An invitation to determine the shape of IMIA in 2015. Methods Inf Med. 2006;45:235–239. [PubMed] [Google Scholar]
- 67.Murray PJ, Haux R, Lorenzi NM. Let a thousand flowers bloom: Transition towards implementation of the IMIA strategic plan. Methods Inf Med. 2007;46:625–628. [PubMed] [Google Scholar]
- 68.Schmidt KF. Nanofrontiers: Visions for the future of Nanotechnology. Woodrow Wilson International Center for Scholars. Project on Emerging Nanotechnologies. 2007 [Google Scholar]
- 69.Poland CA, et al. Carbon nanotubes introduced into the abdominal cavity of mice show asbestos-like pathogenicity in a pilot study. Nature Nanotechnology. 2008;3:423–428. doi: 10.1038/nnano.2008.111. [DOI] [PubMed] [Google Scholar]
- 70.NNN - National Nanomanufacturing Network . NSF. Workshop on nanoinformatics strategies. Arlington, VA: Jun, 2007. http://128.119.56.118/~nnn01/Workshop.html. Last accessed July 10, 2008. [Google Scholar]
- 71.Martin-Sanchez F, Lopez-Alonso V, Hermosilla-Gimeno I, Lopez-Campos G. A primer in knowledge management for Nanoinformatics in Medicine. KES; Accepted as oral communication in the 12th International Conference on Knowledge-Based and Intelligent Information and Engineering Systems; Zagreb, Croatia. September 2008.2008. [Google Scholar]
- 72.Mihalas GI, Lungeanu D, Vernic C, Kigyosi A, Focsa M. Criteria for classification of medical information. In: Baud R, Fieschi M, Le Beux P, Ruch P, editors. The new navigators: from professionals to patients (Proc MIE 2003, St. Malo) IOS Press; Amsterdam: 2003. pp. 358–363. [Google Scholar]
- 73.Hafizovic S, Heer F, Ugniwenko T, Frey U, Blau A, Ziegler C, Hirlemann A CMOS-based micro-electrode array for interaction with neuronal cultures. J Neurosci Methods. 2007;164:93–106. doi: 10.1016/j.jneumeth.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 74.Information workshop in neuroinformatics. http://cordis.europa.eu/search/, (Brussels, 09.06.2000). Last accessed July 10, 2008.
- 75.Picard RW. Affective computing. MIT Press; Cambridge Mass: 2000. [Google Scholar]
- 76. http://ecell3d.iab.keio.ac.jp. Last accessed July 10, 2008.
- 77. http://www.e-cell.org. Last accessed July 10, 2008.
- 78. http://www.physiome.org.nz. Last accessed July 10, 2008.
- 79. http://www.biomedtown.org. Last accessed July 10, 2008.
- 80.Engelbrecht R, Geissbuhler A, Lovis C, Mihalas GI, editors. Connecting Medical Informatics and Bioinformatics (Proc. MIE 2005, Geneva) IOS Press; Amsterdam: 2005. [Google Scholar]
- 81.Reichert A, Mihalas GI, Stoicu-Tivadar L, Schulz S, Engelbrecht R, editors. Integrating biomedical information: From e-Cell to e-Patient. (Proc. STC 2006, Timisoara) IOS Press; Amsterdam: 2006. [Google Scholar]
- 82.Grimshaw JM, Russel IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993;342:1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- 83.Quaglini S, Stefanelli M, Lanzola G, Caporusso V, Panzarasa S. Flexible guideline-based patient careflow systems. Artif Int Med. 2001;22:65–80. doi: 10.1016/s0933-3657(00)00100-7. [DOI] [PubMed] [Google Scholar]
- 84.Shahar Y, Young O, Shalom E, et al. A framework for a distributed, hybrid, multiple-ontology clinical-guideline library and automated guideline-support tools. J Biomed Inform. 2004;37:325–344. doi: 10.1016/j.jbi.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 85.Shalom E, Shahar Y, Taieb-Maimon M, Lunenfeld E, Bar G, Yarkoni A, Young O, Martins SB, Vaszar LT, Goldstein MK, Liel Y, Leibowitz A, Marom T, Lunenfeld E. A quantitative evaluation of a methodology for collaborative specification of clinical guidelines at multiple representation levels. J BioMed Inform. 2008 doi: 10.1016/j.jbi.2008.04.009. in press. [DOI] [PubMed] [Google Scholar]
- 86.Chen DP, Weber SC, Constantinu PS, Ferris TA, Lowe HJ, Butte AJ. Clinical arrays of laboratory measures, or “clinarrays”, built from an electronic health record enable disease subtyping by severity. Proceedings of the 2007 American Medical Informatics Fall meeting (AMIA 2007); pp. 115–199. [PMC free article] [PubMed] [Google Scholar]
- 87.Doyal L. Informed consent: moral necessity or illusion? Quality in Health Care. 2002;10(Suppl i):i29–i33. doi: 10.1136/qhc.0100029... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bowling A, Ebrahim S. Measuring patients' preferences for treatment and perceptions of risk. Quality in Health Care. 2001;10(Suppl i):i2–i8. doi: 10.1136/qhc.0100002... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Woolf SH, Chan ECH, Harris R, Sheridan SL, Braddock BH, Kaplan RM, Krist A, O'Connor AM, Tunis S. Promoting informed choice: transforming health care to dispense knowledge for decision making. Annals of Internal Medicine. 2005;143:293–300. doi: 10.7326/0003-4819-143-4-200508160-00010. [DOI] [PubMed] [Google Scholar]
- 90.Kuhn KA, Giuse DA. From hospital information systems to health information systems. Problems, challenges, perspectives. Methods Inf Med. 2001;40:275–287. [PubMed] [Google Scholar]
- 91.Bhave SV, Hornbaker C, Phang TL, Saba L, Lapadat R, Kechris K, Gaydos J, McGoldrick D, Dolbey A, Leach S, Soriano B, Ellington A, Ellington E, Jones K, Mangion J, Belknap JK, Williams RW, Hunter LE, Hoffman PL, Tabakoff B. The PhenoGen informatics website: tools for analyses of complex traits. BMC Genet. 2007;30:8–59. doi: 10.1186/1471-2156-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vivona S, Gardy JL, Ramachandran S, Brinkman FS, Raghava GP, Flower DR, Filippini F. Computer-aided biotechnology: from immuno-informatics to reverse vaccinology. Trends Biotechnol. 2008;26:190–200. doi: 10.1016/j.tibtech.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 93.Hawkins T, Chitale M, Kihara D. New paradigm in protein function prediction for large scale omics analysis. Mol Biosyst. 2008;4:223–231. doi: 10.1039/b718229e. [DOI] [PubMed] [Google Scholar]
- 94.Borisjuk L, Hajirezaei MR, Klukas C, Rolletschek H, Schreiber F. Integrating data from biological experiments into metabolic networks with the DBE information system. In Silico Biol. 2005;5:93–102. [PubMed] [Google Scholar]
- 95.Olsson S, Hofmann I, Brambilla PM, Jacobsson U, Kennedy P, Roca J, Schmitt KJ, Wyke A. New solutions for personalised health management: citizens' needs, healthcare changes, and market perspectives round table debate. Stud Health Technol Inform. 2004;108:305–312. [PubMed] [Google Scholar]
- 96.Ball MJ, Costin MY, Lehmann C. The personal health record: consumers banking on their health. Stud Health Technol Inform. 2008;134:35–46. [PubMed] [Google Scholar]
- 97.Ferreira A, Cruz-Correia R, Antunes L, Chadwick D. Access control: how can it improve patients' healthcare? Stud Health Technol Inform. 2007;127:65–76. [PubMed] [Google Scholar]
- 98.Hazlehurst B, Sittig DF, Stevens VJ, Smith KS, Hollis JF, Vogt TM, Winickoff JP, Glasgow R, Palen TE, Rigotti NA. Natural language processing in the electronic medical record: assessing clinician adherence to tobacco treatment guidelines. Am J Prev Med. 2005;29:434–439. doi: 10.1016/j.amepre.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 99.Post AR, Harrison JH., Jr Temporal data mining. Clin Lab Med. 2008;28(1):83–100. doi: 10.1016/j.cll.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 100.Haux R, et al. Strategic information management in hospitals. Springer; New York: 2004. [Google Scholar]
- 101.Shortliffe EH, et al. Medical informatics: Computer applications in health care and biomedicine. 1 st edition Addison-Wesley; 1990. p. 164. [Google Scholar]
- 102.Brown B. VHA eyes open-source replacement for VistA. Government HealthIT. 2006 June; [Google Scholar]
- 103.Ricadela A. Closing the door to Microsoft Vista. Business Week. 2008 March 13; [Google Scholar]
- 104.Cusumano MA. The business of software. Free Press; 2004. [Google Scholar]
- 105.Wiederhold G. What is Your Software Worth. Comm ACM. 2006;49(9):65–75. [Google Scholar]
- 106.Reid PP, et al. Building a better delivery system, a new engineering/healthcare partnership. National AcademyPress; Washinton DC: 2005. [Google Scholar]
- 107.The Economist: Places in the Sun. 2007 February 2; [Google Scholar]
- 108.Commission on Systemic Interoperability: Ending the Document Game, Connecting and Transforming Your Healthcare Through Information Technology. U.S. Government Printing Office; Washington, DC: 2005. [PubMed] [Google Scholar]
- 109.Institute of Medicine: Crossing the Quality Chasm, A New Health System for the 21 st Century. National Academy Press; Washington DC: 2001. [Google Scholar]
- 110.Ness RB. Influence of the HIPAA privacy rule on health research. JAMA. 2007;298:2164–2170. doi: 10.1001/jama.298.18.2164. [DOI] [PubMed] [Google Scholar]
- 111.Wiener N. Perspectives in cybernetics, 1964; published 1965 and in Masanti: Norbert Wiener, collected works. MIT Press; Boston, MA: 1985. pp. 360–369. [Google Scholar]