Abstract
Objectives. We conducted a health impact assessment to quantify the potential impact of a state menu-labeling law on population weight gain in Los Angeles County, California.
Methods. We utilized published and unpublished data to model consumer response to point-of-purchase calorie postings at large chain restaurants in Los Angeles County. We conducted sensitivity analyses to account for uncertainty in consumer response and in the total annual revenue, market share, and average meal price of large chain restaurants in the county.
Results. Assuming that 10% of the restaurant patrons would order reduced-calorie meals in response to calorie postings, resulting in an average reduction of 100 calories per meal, we estimated that menu labeling would avert 40.6% of the 6.75 million pound average annual weight gain in the county population aged 5 years and older. Substantially larger impacts would be realized if higher percentages of patrons ordered reduced-calorie meals or if average per-meal calorie reductions increased.
Conclusions. Our findings suggest that mandated menu labeling could have a sizable salutary impact on the obesity epidemic, even with only modest changes in consumer behavior.
During the past several decades, increased consumption of calorie-dense foods outside the home,1–4 “supersizing” of food and beverage portions at large chain restaurants,5,6 and an underestimation of caloric content by restaurant patrons7,8 have contributed to the increase in the prevalence of obesity in the United States. Not surprisingly, during this same time period, obesity-related health conditions,9,10 including diabetes, hypertension, fatty liver, sleep apnea, arthritis, and depression, and restaurant expenditures ($400 billion annually by consumers11) have paralleled the trajectory of the obesity epidemic. These factors and others have made the failure to disclose nutrition content at the point of purchase a growing and significant public health concern. Whereas the Nutrition Labeling and Education Act of 1990 increased the availability of nutrition information on packaged foods, prepared foods at the point of purchase are exempt from such disclosures. At present, most fast-food and sit-down chain restaurants typically disclose nutrition information only upon request, via the Internet, or in a manner not readily visible to individuals placing their food orders on site (e.g., small-print table inserts, table tents, or brochures).11
Laws mandating the provision of calorie information at the point of purchase in large chain restaurants have garnered growing public and legislative support as a potential strategy for addressing the obesity epidemic.12,13 This interest is reflected in the recent passage of menu-labeling ordinances in some jurisdictions, including New York City, New York; San Francisco, California; Multnomah County, Oregon; and King County, Washington. In California, Senate Bill (SB) 1420,14 introduced and passed in 2008, has received considerable national attention as it awaits implementation. When implemented, SB 1420 would require all restaurant chains across the state with 20 or more facilities to post calorie information next to each item on their menus and menu boards. An earlier version of the bill included restaurant chains with 15 or more facilities in the state, and required, in addition to the calorie information, the provision of information on saturated fat, sugar, and sodium content on menus (but not on menu boards).
Despite this increased interest and legislative action, no published studies have sought to quantify the potential impact of menu labeling on the obesity epidemic. To address this gap, we conducted a health impact assessment of menu labeling, as specified in the original version of SB 1420, on population weight gain in Los Angeles County. Los Angeles County is the largest county in the United States, home to more than 10 million residents.
METHODS
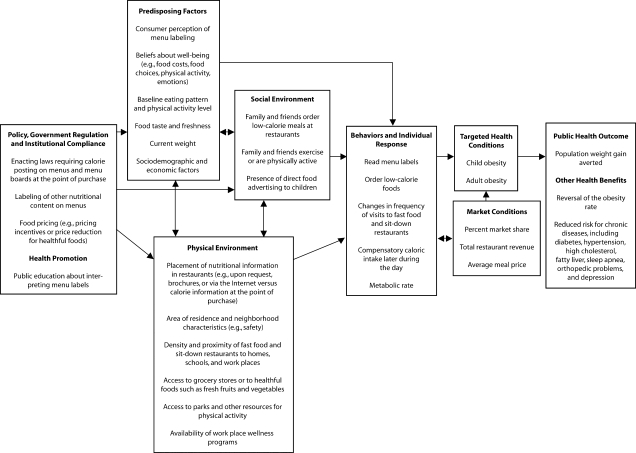
Guided by a logic framework that considered a range of complex pathways and causal interactions between menu labeling and health (Figure 1), we developed a health impact assessment approach, which draws from multiple data sources.15–18 With the health impact assessment, we aimed to, sequentially: (1) quantify the obesity epidemic in Los Angeles County, (2) model the impact of menu labeling on this epidemic by using reasonable estimates for the county's obesity burden and plausible assumptions about consumer response to calorie postings at the point of purchase, and (3) evaluate the robustness of the assessment's findings by conducting sensitivity analyses to account for the uncertainty in consumer response and in several of the market variables used in the simulation model, including the total annual revenue, market share, and average meal price of large chain restaurants in the county.
FIGURE 1.
Logic framework for the health impact assessment of menu labeling.
Quantifying the Magnitude of the Obesity Epidemic
Adult population weight gain.
We used data from the 1997 and 2005 Los Angeles County Health Surveys to quantify the obesity epidemic among adults 18 years and older in Los Angeles County. The 2 random-digit-dialing telephone surveys collected health data, including self-reported height and weight, on a random sample of 8004 and 8648 adults, respectively, through a structured telephone interview. The response rates were 52% and 47%, respectively. The survey team weighted the data to reflect the demographic characteristics of the county's adult population by using census-based population estimates. Methods of data collection for the Los Angeles County Health Surveys have been described elsewhere.19
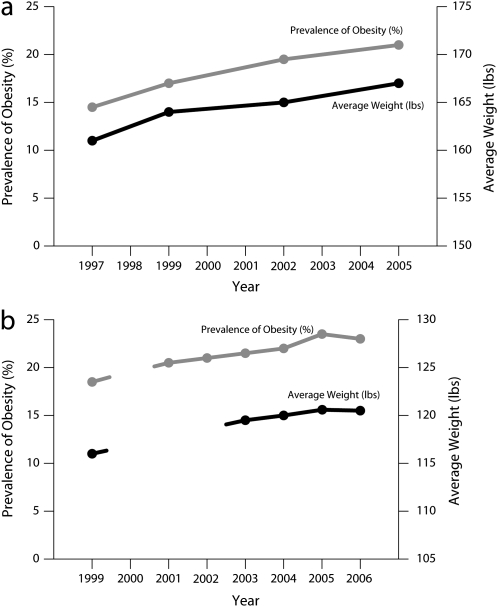
We estimated the magnitude of the obesity epidemic among adults by examining the increasing prevalence of adult obesity in Los Angeles County from 1997 to 2005. For the purpose of our analysis, we defined adult obesity as a body mass index (BMI; weight in kilograms divided by height in meters squared) of 30.0 kg/m2 or greater.20 We compared this trend to the observed increase in the mean (average) weight of an adult in the county population during the same time period; the average adult height did not change during this time interval. 21 From 1997 to 2005, the percentage of obese adults in the county increased from 14.3% to 20.9%; this parallels the average weight gain of an adult in the county during the same time interval, which increased from 160.9 lbs to 166.8 lbs (Figure 2a). On the basis of these estimates, we calculated the total adult population weight gain associated with the obesity epidemic by subtracting the average weight of an adult in 1997 from the average weight in 2005 and multiplying the difference by the number of adults in the county population in 2005. To determine the average annual population weight gain in this population, we divided the estimate for the total adult population weight gain by 8 (the number of years in the time interval).
FIGURE 2.
Prevalence of obesity and average weight among (a) adults (1997–2005) and (b) 5th-, 7th-, and 9th-graders in public schools (1999–2006): Los Angeles County, CA.
Note. Data on students' weights were not collected by the California Department of Education Physical Fitness Testing Program in 2000; data on students' weights were not available for 2001 and 2002.
Child population weight gain.
We quantified the obesity epidemic among children aged 5 to 17 years in Los Angeles County by using similar methods as described for the adult population. We calculated the total and average annual population weight gain for children aged 5 to 17 years by using the 1999 and 2006 data from the California Department of Education Physical Fitness Testing Program.22 This state program requires fitness testing each year, including measured height and weight, of all 5th-, 7th-, and 9th-grade students enrolled in public schools; the program, however, does not specifically follow each student over time. We used these height and weight measurements to calculate age- and gender-specific BMIs based on standard growth charts from the Centers for Disease Control and Prevention (CDC).23 We considered the children obese if their estimated BMI exceeded the 95th percentile of their age and gender group's BMI. Where appropriate, we excluded biologically implausible BMI values by using a CDC algorithm.23
Our analysis was limited to data collected on students who were enrolled in Los Angeles County public schools who had complete data for height, weight, age, and gender and who had biologically plausible BMI values. On the basis of these inclusion criteria, we used data on 173 315 students from the 1999 database and 333 649 students from the 2006 database to compute the estimates. We adjusted the estimates by grade level because the 1999 database included a higher percentage of 5th graders (41%) and a lower percentage of 9th graders (26%) compared with the 2006 database (36% and 31%, respectively). This difference reflected the fact that high schools were slower in starting the program than were elementary and middle schools. The program was initiated in 1999.22
In calculating the total population weight gain for children, we assumed that the weight gain was similar for all school-aged children aged 5 to 17 years. This assumption is supported by county trends in child obesity and average student weight gain; they were similar from 1999 to 2006 (Figure 2b). Likewise, trends across the 3 grade levels were similar. Children younger than 5 years were excluded from the analysis because reliable population data on recent weight gain for this age group were not available. For students enrolled in private schools, BMI data were also not available (11.5% of all school enrollments in Los Angeles County in 2005 were in private schools) and for students who dropped out of school (average 1-year dropout rate was 4.0% from 1999 to 200624). Collectively, these 2 groups represent a relatively small proportion of all school-eligible children in Los Angeles County—i.e., less than 220 000 out of more than 1.7 million students.
Modeling the Impact of Menu Labeling on Population Weight Gain
The health impact assessment utilized a simulation model25 to examine the potential impact of menu labeling on population weight gain. We included estimates of total annual revenue, market share, and average meal price of large chain restaurants in the model to approximate the total number of meals served annually in Los Angeles County. We used published and unpublished data to extrapolate the percentage of restaurant patrons who would order reduced-calorie meals, and the average per-meal calorie reduction as a result of menu labeling.26,27 We used these estimates to calculate the annual populationwide reduction in caloric intake attributable to menu labeling. To convert the reduced caloric intake to pounds of weight gain averted, we used a conversion factor of 3500 calories per pound.28 We calculated the key outcome measure—the percentage of population weight gain averted because of menu labeling—by dividing the pounds of weight gain averted by the average annual population weight gain.
The simulation model considered the following consumer response scenario (base case): that 10% of the restaurant patrons would order reduced-calorie meals and that these patrons would reduce their order by an average of 100 calories in response to the calorie postings on menus and menu boards at large chain restaurants with 15 or more facilities in the state. This scenario was based on data from 2 recently published studies examining the influence of point-of-purchase nutritional information on consumer food choices.26,27 In the first study, a statewide mailed survey and intervention, Burton et al.26 found that consumers were typically unaware of the high levels of calories, fat, and sodium commonly found in restaurant foods and that when they were provided nutritional information at the point of purchase, approximately 10% decreased their selection of higher-calorie food items. In the second study, Bassett et al.27 found that at Subway restaurants in which calorie information was posted at the point of purchase, 11.8% of the patrons reported that they saw this information and that it had an effect on their purchases; these individuals purchased 99 fewer calories than did those who saw the information but reported that calorie information had no effect on their purchase choices.
We assumed in the model that restaurant patrons who ordered reduced-calorie meals would not increase their food or beverage intake at other times during the day. This assumption is supported by recent research suggesting that small decrements in caloric intake of the magnitude used in this health impact assessment are not associated with a compensatory increase in caloric intake later in the day or over a period of several days.29 We also assumed that persons who ordered reduced- calorie meals would not alter their physical activity level and that the resting metabolic rate of these individuals would not change significantly as a result of the small caloric reduction anticipated from consumer access to calorie information on menus and menu boards at the point of purchase.
Sensitivity Analyses
Because of the uncertainty in consumer response to calorie postings, and in several of the market variables used in the simulation model, we conducted several sensitivity analyses by using a range of plausible consumer-response scenarios and estimates for the total annual revenue, market share, and average meal price of large chain restaurants in the county.30 We examined the effects of varying these scenarios and estimates on the key outcome (“population weight gain averted”) used in the model.
RESULTS
Among those 5 years and older, the average annual population weight gain associated with the recent obesity epidemic in the county was 6.75 million pounds (Table 1). This estimate was based on an average annual population weight gain of 5.5 million pounds among adults 18 years and older from 1997 to 2005, and an average annual population weight gain of 1.25 million pounds among children aged 5 to 17 years from 1999 to 2006.
TABLE 1.
Stepwises Simulation Model (Base Case) and Data Sources and Methods for Quantifying the Impact of Menu Labeling on Population Weight Gain: Los Angeles County, CA, 1997–2006
| Variable | Estimate | Data Source or Method of Calculation |
| 1. Total annual restaurant revenue, Los Angeles County | $14 600 000 000 | Projected restaurant sales for 2007 in California as reported by the National Restaurant Association.31 |
| County revenue estimated by multiplying the California sales estimate by 0.27, the proportion of the state's population in Los Angeles County (data source: California Department of Finance32). | ||
| 2. Large chain restaurant market share—15 or more facilities in California | 51% | Extrapolated information from the NPD Group, 2005; cited in the US District Court Declaration of Thomas R. Frieden, Commissioner of the New York City Department of Health and Mental Hygiene, July 5, 2007.33(p31) |
| 3. Large chain restaurant revenue, Los Angeles County | $7 446 000 000 | Calculated by multiplying the estimates in variables 1 and 2. |
| 4. Average price per meal in large chain restaurants (includes fast-food and sit-down restaurants) | $7.48 | Based on national meal price estimates in 1992,30 adjusted for inflation by using a factor of 2.58% per year to simulate compounded growth derived from the Consumer Price Index.34 |
| 5. Annual number of meals served in large chain restaurants, Los Angeles County | 995 454 545 | Calculated by dividing the estimate in variable 3 by the estimate in variable 4. |
| 6. Annual number of meals served, ages 0–4 y | 36 500 000 | Estimate derived from the 2005 Los Angeles County Health Survey data. |
| 7. Annual number of meals served, ages 5 y and older | 958 954 545 | Calculated by subtracting the estimate in variable 6 from the estimate in variable 5. |
| 8. Percentage of large-chain-restaurant patrons who select reduced-calorie meals as a result of menu labeling | 10% | Extrapolated from data published by Burton et al.26 |
| 9. Annual number of reduced-calorie meals | 95 895 455 | Calculated by multiplying the estimates in variables 7 and 8. |
| 10. Average amount of calorie reduction per meal | 100 | Data from Bassett et al.27 |
| 11. Total annual number of reduced calories attributable to menu labeling | 9 589 545 455 | Calculated by multiplying the estimates in variables 9 and 10. |
| 12. Calories per pound of weight | 3 500 | Duyff28 |
| 13. Total annual pounds of weight loss attributable to menu labeling | 2 739 870 | Calculated by dividing the estimate in variable 11 by the estimate in variable 12. |
| 14. Average annual population weight gain, ages 18 y and older, lbs | 5 500 000 | Calculated by using data from the 1997 and 2005 Los Angeles County Health Surveys. |
| 15. Average annual population weight gain, ages 5–17 y, lbs | 1 250 000 | Calculated by using data from the 1999 and 2006 California Department of Education Physical Fitness Testing Program.22 |
| 16. Average annual population weight gain, ages 5 y and older, lbs | 6 750 000 | Calculated as the sum of the estimates in variables 14 and 15. |
| 17. Percentage of population weight gain averted because of menu labeling | 40.6% | Calculated by dividing the estimate in variable 13 by the estimate in variable 16. |
As indicated in Table 1, if menu labeling resulted in 10% of large-chain-restaurant patrons ordering reduced-calorie meals with an average reduction of 100 calories per meal, a total of 40.6% of the 6.75 million pound average annual weight gain in the county population 5 years and older would be averted.
Based on varying the model assumptions about consumer response, substantially larger impacts would be realized if higher percentages of restaurant patrons ordered reduced-calorie meals or if the magnitude of the average per-meal calorie reduction was increased (Table 2). If the percentage of patrons who would purchase reduced-calorie meals were increased to 20%, for example, 81.2% of the population weight gain would be averted over the course of a year, even if the average per-meal calorie reduction remained unchanged at 100 calories. If the average per-meal calorie reduction increased to 125 calories among the 20% of patrons who ordered reduced-calorie meals, the population weight gain averted would reach 101.5%, indicating an approximate leveling and perhaps the beginning of a potential reversal of the obesity epidemic as measured by population weight gain. Further increases in either the percentage of patrons ordering reduced-calorie meals or in the average per-meal calorie reduction would result in a net population weight loss (i.e., > 100% population weight gain averted), suggesting a reversal of the obesity epidemic. Other sensitivity analyses suggest that our findings are relatively insensitive to such factors as variations in the estimates for total annual revenue, market share, and average meal price of large chain restaurants in Los Angeles County (Table 3).
TABLE 2.
Effects of Varying Consumer Responses to Calorie Postings at the Point of Purchase on Population Weight Gain Averted: Los Angeles County, CA, 1997–2006
| Percentage of Patrons Who Would Purchase a Lower-Calorie Meal |
|||||
| Average Amount of Calorie Reduction Per Meal | 10%: Population Weight Gain Averted, % | 20%: Population Weight Gain Averted, % | 30%: Population Weight Gain Averted, % | 40%: Population Weight Gain Averted, % | 50%: Population Weight Gain Averted, % |
| 25 | 10.1 | 20.3 | 30.4 | 40.6 | 50.7 |
| 50 | 20.3 | 40.6 | 60.9 | 81.2 | 101.5 |
| 75 | 30.4 | 60.9 | 91.3 | 121.8 | 152.2 |
| 100a | 40.6 | 81.2 | 121.8 | 162.4 | 203.0 |
| 125 | 50.7 | 101.5 | 152.2 | 203.3 | 253.7 |
| 150 | 60.9 | 121.8 | 182.7 | 243.5 | 304.4 |
| 175 | 71.0 | 142.1 | 213.1 | 284.1 | 355.2 |
| 200 | 81.2 | 162.4 | 243.5 | 324.7 | 405.9 |
Note. Percentages that are greater than 100% represent net population weight loss, suggesting a potential reversal of the obesity epidemic.
The base case in the simulation model.
TABLE 3.
Effects of Varying Total Annual Revenue, Market Share, and Average Meal Price of Large Chain Restaurants on the Percentage of Population Weight Gain Averted: Los Angeles County, CA, 1997–2006
| Population Weight Gain Averted, % | |
| Total annual restaurant revenue,a billions $ | |
| 15.6 | 43.5 |
| 14.6b | 40.6 |
| 13.6 | 37.7 |
| Large chain restaurant market share,c % | |
| 56 | 44.7 |
| 51b | 40.6 |
| 46 | 36.5 |
| Average meal price at large chain restaurants,d $ | |
| 8.48 | 35.6 |
| 7.48b | 40.9 |
| 6.48 | 47.1 |
Note. The 3 sensitivity analyses were based on the 10% or 100 calories consumer response scenario (base case) presented in the simulation model (Table 1). In the analysis of each variable, the values of the other 2 variables were held constant by using the same values from the base case.
In Los Angeles County. Business volume = $14.6 billion ±$1 billion.
Base case in the simulation model.
Market share = 51% ±5 percentage points.
Average meal price = $7.48 ±$1.00.
DISCUSSION
Findings from this health impact assessment suggest that mandated menu labeling at fast food and other large chain restaurants could reduce population weight gain, even with only modest changes in consumer behavior. In addition, our simulation model suggests that the impact on population weight gain could be greatly enhanced if community education efforts,35 pricing incentives,36 restrictions on advertising to children,37 or other strategies33,37 were undertaken to increase the degree to which restaurant patrons use the posted information to select reduced-calorie meals. Several strategies such as pricing incentives or price reductions for healthful foods have been shown to change individual purchasing patterns of targeted foods in work site and school cafeteria settings.36 Other strategies such as community education to improve nutrition knowledge have also been shown to improve diet quality in small degrees and among particular age groups, including the elderly.35 Collectively, these strategies could lead to a greater demand for more-healthful foods and provide the restaurant industry with a stronger incentive to reformulate their menus with lower-calorie foods and smaller portion sizes.13 Most experts agreed that because consumers make decisions about what they eat on the basis of a number of factors, a combination of community strategies and policy interventions will be required to improve food choices among diverse population groups.13,35,36
Limitations
A limitation of the present health impact assessment is that we were unable to assess the effect of menu labeling on the obesity epidemic directly (i.e., its impact on the rising rate of obesity), but rather, estimated the effect by using population weight gain averted as an alternative measure. Although our analysis demonstrated that the recent trends in the obesity rate and the average body weight gain were similar, we cannot be certain that the impact of menu labeling would be identical across the 2 measures. For example, if obese restaurant patrons were more likely than were nonobese patrons to order reduced-calorie meals, the impact of menu labeling on the obesity rate could be greater than what we reported for the population weight gain averted. Alternatively, if nonobese restaurant patrons were more likely to order reduced-calorie meals than were obese patrons, the impact on the obesity rate could be less than what we reported.
In addition, the health impact assessment assumed that the obesity rate will continue to increase in the future. Recent data released by the Centers for Disease Control and Prevention suggest that this may not be the case. The prevalence of high BMI values among children and adults showed no significant changes between 2003 to 2004 and 2005 to 2006.38,39 Further research is needed to clarify and verify these factors and other effects of menu labeling on the obesity rate.
This health impact assessment was further limited by the lack of county-specific data on total annual revenue, market share, and average meal price of large chain restaurants; these estimates were extrapolated from national data. However, sensitivity analyses conducted on these key market variables suggest that our findings were relatively insensitive to variations in these estimates. Thus, any small to modest error in the variable estimates are unlikely to have led to major errors in our findings. Additionally, reanalysis of our data suggests that the impact of California's menu-labeling legislation (SB 1420) would not be diminished significantly by changes made in the final draft of the bill—i.e., from requiring calorie postings in all restaurants with 15 or more facilities to include only restaurants with 20 or more facilities in the state); this change in the requirement would only reduce the magnitude of the impact by approximately 3%, from 40.6% to 37.3% population weight gain averted.
Finally, there were only limited data available to us on the degree to which menu labeling would influence the menu item selections or purchasing intentions of restaurant patrons. For this reason, the health impact assessment provided a plausible range of estimates on the impact of menu labeling on population weight gain, assuming varying levels of change in consumer behavior that could be easily achieved. For example, based on a composite of calorie information from 3 fast-food restaurant chains, changing from a double meat patty to a single meat patty hamburger would save 244 calories, from a large to a medium order of french fries would save 163 calories, or from a large to medium soft drink would save 95 calories. Emerging evidence in the literature suggests that these modest changes are feasible. In a study of restaurant patrons, Bassett et al.27 found that among patrons of Subway restaurants, those who saw calorie information posted prominently were more likely to purchase meals with fewer calories (on average, 52 fewer calories) than those who did not see similar calorie information.
Conclusions
Our findings suggest that, even with modest changes in consumer behavior as a response to calorie postings at the point of purchase, the impact of menu labeling on population weight gain could be substantial, favoring legislative strategies such as SB 1420 in California for combating the obesity epidemic.
Acknowledgments
The authors would like to thank D. Mike Jackson, Rachel Tyree, Amy Lightstone, and Margaret Shih for their contributions to the article.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Kant AK, Graubard BI. Eating out in America, 1987–2000: trends and nutritional correlates. Prev Med 2004;38:243–249 [DOI] [PubMed] [Google Scholar]
- 2.Bowman SA, Vinyard BT. Fast food consumption of US adults: impact on energy and nutrient intakes and overweight status. J Am Coll Nutr 2004;23:163–168 [DOI] [PubMed] [Google Scholar]
- 3.Nielsen SJ, Siega-Riz AM, Popkin BM. Trends in energy intake in US between 1977 and 1996: similar shifts seen across age groups. Obes Res 2002;10:370–378 [DOI] [PubMed] [Google Scholar]
- 4.St-Onge MP, Keller KL, Heymsfield SB. Changes in childhood food consumption patterns: a cause for concern in light of increasing body weights. Am J Clin Nutr 2003;78:1068–1073 [DOI] [PubMed] [Google Scholar]
- 5.McCrory MA, Fuss PJ, Hays NP, Vinken AG, Greenberg AS, Roberts SB. Overeating in America: association between restaurant food consumption and body fatness in healthy adult men and women ages 19 to 80. Obes Res 1999;7:564–571 [DOI] [PubMed] [Google Scholar]
- 6.Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health 2002;92:246–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Backstrand J, Wootan MG, Young LR, Hurley J. Fat Chance Washington, DC: Center for Science in the Public Interest; 1997 [Google Scholar]
- 8.Variyam JN, Golan E. New health information is reshaping food choices. Econ Res Serv Food Rev 2002;25(1):13–18 [Google Scholar]
- 9.Sugarman SB, Foerster SB, Adkins SE, Carman JS, Hooker SP. The Economic Costs of Physical Inactivity, Obesity, and Overweight in California Adults: Health Care, Workers' Compensation, and Lost Productivity. Sacramento: California Dept of Health Services, Cancer Prevention and Nutrition Section; 2005 [Google Scholar]
- 10.Thorpe KE, Florence CS, Howard DH, Joski P. The impact of obesity on rising medical spending. Health Aff (Millwood) 2004;(suppl Web exclusives):W480–W486 [DOI] [PubMed] [Google Scholar]
- 11.Keystone Forum on Away-From-Home Foods Opportunities for Preventing Weight Gain and Obesity Washington, DC: Keystone Center; 2006 [Google Scholar]
- 12.Wootan MG, Osborn M. Availability of nutrition information from chain restaurants in the United States. Am J Prev Med 2006;30:266–268 [DOI] [PubMed] [Google Scholar]
- 13.Berman M, Lavizzo-Mourey R. Obesity prevention in the information age. Caloric information at the point of purchase. JAMA 2008;300:433–435 [DOI] [PubMed] [Google Scholar]
- 14. CA Senate Bill 1420. Introduced by Senators Padilla and Migden on February 21, 2008; amended in the Assembly on August 8 and 22, 2008; amended in the Senate on May 13, 2008. Available at: http://www.leginfo.ca.gov. Accessed May 1, 2008.
- 15.Health Impact Assessment. Main Concepts Suggested Approach. Brussels, Belgium: European Centre for Health Policy, World Health Organization Regional Office for Europe; 1999. Gothenburg consensus paper. Available at: http://www.euro.who.int/document/PAE/Gothenburgpaper.pdf. Accessed March 25, 2008 [Google Scholar]
- 16.Cole BL, Fielding JE. Health impact assessment: a tool to help policy makers understand health beyond health care. Annu Rev Public Health 2007;28:393–412 [DOI] [PubMed] [Google Scholar]
- 17.Evans RG, Stoddart GL. Consuming research, producing policy? Am J Public Health 2003;93:371–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bleich S, Cutler D, Murray C, Adams A. Why is the developed world obese? Annu Rev Public Health 2008;29:273–295 [DOI] [PubMed] [Google Scholar]
- 19.Simon PA, Wold CM, Cousineau MR, Fielding JE. Meeting the data needs of a local health department: the Los Angeles County Health Survey. Am J Public Health 2001;91:1950–1952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science 2003;299:853–855 [DOI] [PubMed] [Google Scholar]
- 21.County of Los Angeles Public Health Chronic Disease and Injury Prevention Web page. Available at: http://publichealth.lacounty.gov/chronic. Accessed January 1, 2008
- 22.California Department of Education Physical Fitness Testing (PFT) program Web page. Available at: http://www.cde.ca.gov/ta/tg/pf. Accessed February 1, 2008
- 23.Centers for Disease Control and Prevention, National Center for Health Statistics Growth charts. Available at: http://www.cdc.gov/growthcharts. Accessed February 1, 2008
- 24.California Department of Education Web site. Available at: http://www.cde.ca.gov. Accessed February 24, 2008.
- 25.Monheit AC, Cantor JC, Banerjee P. Assessing Policy Options for the Non-Group Health Insurance Market: Simulation of the Impact of Modified Community Rating in the New Jersey Individual Health Coverage Program. New Brunswick, NJ: Rutgers Center for State Health Policy; 2005 [Google Scholar]
- 26.Burton S, Creyer EH, Kees J, Huggins K. Attacking the obesity epidemic: the potential health benefits of providing nutrition information in restaurants. Am J Public Health 2006;96:1669–1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bassett MT, Dumanovsky T, Huang C, et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health 2008;98:1457–1459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duyff RL. American Dietetic Association Complete Food and Nutrition Guide. Hoboken, NJ: John Wiley and Sons; 2002:36 [Google Scholar]
- 29.Levitsky DA. The non-regulation of food intake in humans: hope for reversing the epidemic of obesity. Physiol Behav 2005;86:623–632 [DOI] [PubMed] [Google Scholar]
- 30.Jekanowski MD. Causes and consequences of fast food sales growth. Away-From-Home Foods 1999;Jan–April:11–16 [Google Scholar]
- 31.National Restaurant Association Web site. Available at: http://www.restaurant.org. Accessed September 1, 2007.
- 32.California Department of Finance Web site. Available at: http://www.dof.ca.gov/research. Accessed January 1, 2008.
- 33.Frieden TR. Declaration to civil complaint No. 07 Civ 5710 (RJH): New York State Restaurant Association Against New York City Board of Health, New York City Department of Health and Mental Hygiene, and Thomas R. Frieden, in His Official Capacity as Commissioner of the New York City Department of Health and Mental Hygiene. July 5, 2007. Available at: http://www.nyc.gov/html/doh/downloads/pdf/public/calorie_TRF_declaration-02-08.pdf. Accessed May 21, 2009 [Google Scholar]
- 34.Bureau of Labor Statistics, US Department of Labor Consumer Price Index. Available at: http://www.bls.gov/cpi. Accessed June 26, 2009
- 35.Frazao E, Allshouse J. Strategies for intervention: commentary and debate. J Nutr 2003;133:844S–847S [DOI] [PubMed] [Google Scholar]
- 36.French SA. Pricing effects on food choices. J Nutr 2003;133:841S–843S [DOI] [PubMed] [Google Scholar]
- 37.Hawkes C. Regulating food marketing to young people worldwide: trends and policy drivers. Am J Public Health 2007;97:1962–1973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA 2008;299:2401–2405 [DOI] [PubMed] [Google Scholar]
- 39.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity Among Adults in the United States – No Statistically Significant Change Since 2003-2004. Hyattsville, MD: National Center for Health Statistics; 2007. NCHS data brief no. 1 [PubMed] [Google Scholar]