Abstract
Implants available for distal radius fracture fixation include dorsal nonlocked plating (DNLP), volar locked plating (VLP), radial–ulnar dual-column locked plating (DCPs), and locked intramedullary fixation (IMN). This study examines the biomechanical properties of these four different fixation constructs. In 28 fresh-frozen radii, a wedge osteotomy was performed, creating an unstable fracture model and the four fixation constructs employed (DNLP, VLP, DCPs, and IMN). Dorsal bending loads were applied and bending stiffness, load to yield 5 mm displacement, and ultimate failure were measured. Bending stiffness for VLP (16.7 N/mm) was significantly higher than for DNLP (6.8 N/mm), while IMN (12.6 N/mm) and DCPs (11.8 N/mm) were similar. Ultimate load to failure occurred at 278.2 N for the VLP, 245.7 N for the IMN, and 52.0 N for the DNLP. The VLP was significantly stronger than the DNLP and DCPs, and the IMN and DCPs were stronger than the DNLP. The VLP has higher average bending stiffness, ultimate bending strength, and resistance to 5 mm displacement than the other constructs and significantly higher ultimate bending strength than the DCPs and DNLP. There was no statistically significant difference between the VLP and IMN. VLP and IMN fixation of distal radius fractures can achieve comparable stability.
Keywords: Distal radius, Fracture, Wrist, Biomechanical, Fixation, Intramedullary, Nail, Locked plate, Dual plates, Dorsal plate, Wrist trauma, Wrist fracture fixation, Distal radius fracture fixation
Introduction
There are currently a multitude of fixation constructs available for stabilizing distal radius fractures. There have been several studies analyzing the biomechanical properties of a variety of these different implants [1, 4, 5, 8–11, 13, 14, 19, 20]. Volar locked plating has had an increase in popularity in the last several years [11]. By virtue of the success of this technique, the percentage of distal radius fractures that are now treated with open reduction and internal fixation has risen. Dorsal plating has become less popular, but newer constructs have been made lower profile to minimize soft-tissue complications, and recent reports have shown improved clinical success with this technique [7]. Dual-column fixation has been shown to have improved rigidity compared to dorsal plating and also has had demonstrated clinical success [6, 14]. Recently, intramedullary fixation of distal radius fractures has been described to have acceptable clinical outcomes [2, 18]. There has been a biomechanical assessment of the hybrid Dorsal Nail Plate™ (DNP; Hand Innovations, Miami, FL, USA) in comparison to volar locking plates [11]. However, there are no studies comparing a completely intramedullary device to the other more well-known constructs. The purpose of this study is to examine the biomechanical properties of typical examples of these four different implant types in stabilizing an unstable extra-articular distal radius fracture model.
Materials and Methods
Twenty-eight fresh frozen cadaver specimens were used. The radii were disarticulated from the wrist and distal radial–ulnar joint (DRUJ), stripped of all soft tissue, and osteotomized at the bicipital tuberosity proximally. All specimens were radiographed prior to testing to rule out bony pathology. An osteotomy model was chosen to simulate dorsal comminution. Extra-articular osteotomies were created 12 mm from the lunate facet, and a trapezoidal wedge of bone (7 mm dorsally and 3 mm volarly) was removed to allow no bony contact between the proximal and distal fragments. Osteotomies were always made proximal to the DRUJ. Monte Carlo randomization was used to create four testing groups, each with a different fixation construct. There were seven specimens per group, and the four constructs tested were: (1) a volar locked plate (VLP), using the Distal Volar Radius™(DVR) Plate (Hand Innovations); (2) a dorsal nonlocked plate (DNLP), using the Lo-Con-T™ stainless steel dorsal nonlocking plate (Wright Medical Technology, Arlington, TN, USA); (3) a construct with two dual-column plates (DCPs), using radial and ulnar dual-column 2.4 mm titanium locked plates (Synthes USA, West Chester, PA, USA); and (4) an intramedullary nail (IMN), using the Micronail™ intramedullary device (Wright Medical Technology).
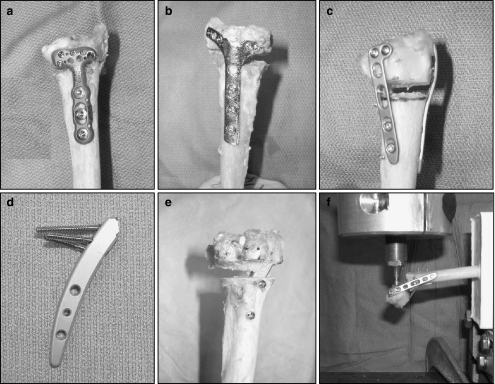
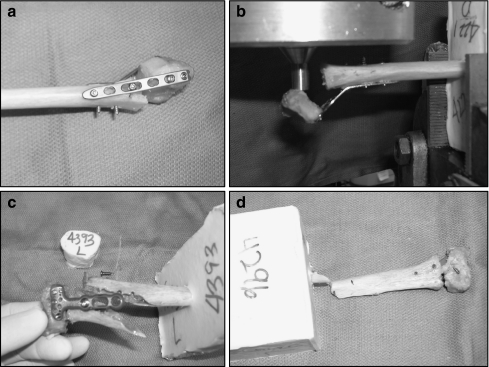
The implants were inserted in the following manner (Fig. 1). The VLP was fixed to the volar shaft with three bicortical screws and fixed distally with four locked screws: two in the distal row (one in the central hole and one in lunate facet) and two in the proximal row (one in the most radial hole and one in the most ulnar hole). The more central ulnar screws were used distally as the load cell actuator was applied at the lunate facet. The DNLP was placed dorsally and then fixed with three bicortical screws in the shaft and four nonlocking screws placed in the distal fragment. The dual-column plates were from the 2.4-mm locking distal radial plate set. The configuration used was a radial styloid plate placed straight radial with two bicortical nonlocking screws in the shaft and two locking screws in the distal fragment; combined with an L-shaped plate placed dorsal-ulnarly with two nonlocked screws in the shaft and two locked screws place in the articular segment. The IMN was placed through the radial styloid and had two nonlocked screws placed in the shaft through the attached jig and three locking screws placed in the distal fragment. The goal was to make the number of screws placed in the distal fragment identical (four) in all constructs, when possible, thus making the constructs more comparable. The Micronail has only three screw holes available distally.
Figure 1.
Fixation constructs. a Volar locked plate: Distal Volar Radius™ Plate (Hand Innovations). The DVR plate was fixed to the volar shaft with three bicortical screws and fixed distally with four locked screws: two in the distal row and two in the proximal row. b Dorsal nonlocked plate: Lo-Con-T™ stainless steel dorsal nonlocking plate (Wright Medical Technology). The Lo-Con-T plate was placed dorsally and then fixed with three bicortical screws in the shaft and four nonlocking screws placed in the distal fragment. c Dual-column plates: radial and ulnar dual-column 2.4 mm titanium locked plates (Synthes USA). A radial styloid plate was placed straight radial with two bicortical nonlocking screws in the shaft and two locking screws in the distal fragment, and an L-plate was placed dorsal-ulnarly with two nonlocked screws in the shaft and two locked screws in the articular segment. d Intramedullary nail: Micronail™ intramedullary device (Wright Medical Technology). The distal three screws are locked into the nail. e The intramedullary nail was placed through the radial styloid into the proximal shaft. The nail is seen traversing the defect, and the heads of the two proximal nonlocked screws are seen resting on the dorsal radial shaft. f Dorsal bending load. The load was applied to construct until obvious failure. Note that the load cell actuator is applied to the volar lip of the radius only and not the implant.
The constructs were potted in a poly-methyl-methacrylate (PMMA) block by placing the proximal shaft in the potting material to create a constant distance of 10 cm from the potting material to the distal articular surface. The block was mounted with a fixed vise-clamp on a materials testing machine (MTS, Eden Prairie, MN, USA). An initial preload was performed to remove any creep from the system. A small bending load of 10 N was applied to remove creep from the system in the bending plane. Definitive dorsal bending loads were then applied by having the MTS actuator apply a progressive force to the distal volar lip of the radius. It was ensured that all specimens were not loaded directly on the metal plates or rods but only on the bone. This progressive load was delivered and bending stiffness calculated from the slope of the load deformation curves in the linear region.
The identically directed load was continued until obvious failure was demonstrated. At this point and from obvious deflection points in the load curves, the ultimate load to failure was recorded. The force required to displace the dorsal fragment 5 mm was also recorded for each specimen. A distance of 5 mm was selected as this typically would be regarded as unacceptable displacement. The specimens were then examined, and the mode of failure was determined.
Statistical Methods
Data from experiments were analyzed across all treatment conditions by a one-way analysis of variance followed by Holm–Sidak post hoc multiple comparisons. p values less than 0.05 were considered statistically significant for all tests.
Results
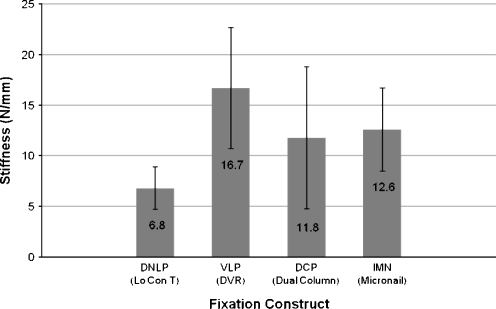
The results for bending rigidity of the constructs showed that the VLP had the highest stiffness at 16.7 N/mm and the DNLP had the lowest at 6.8 N/mm. The IMN and DCPs were similar at 12.6 and 11.8 N/mm, respectively. The VLP was significantly more rigid than the DNLP (p = 0.003). There was no other significant difference between the other constructs in bending rigidity.
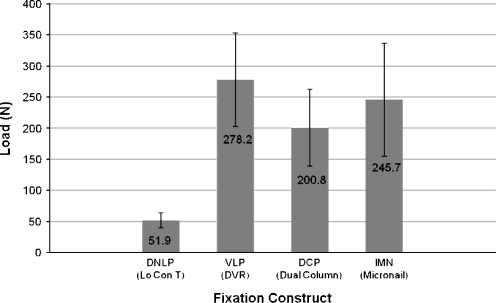
Ultimate load to failure demonstrated that the VLP had the highest value at 278.2 N, and the DNLP had the lowest at 52.0 N. The IMN construct failed at 245.7 N and the DCPs measured at 200.8 N. Significantly higher ultimate load to failure was seen in the VLP as compared to the DNLP (p < 0.001) and DCP (p = 0.05) but not to the IMN (p = 0.41). The IMN (p < 0.001) and the DCP (p = 0.001) had significantly higher ultimate load to failure as compared to the DNLP (Figs. 2 and 3).
Figure 2.
Bending stiffness. The VLP (DVR plate) was significantly more rigid than the DNLP (Lo-Con plate); p = 0.003. There was no other significant difference between the other constructs in bending rigidity.
Figure 3.
Ultimate load to failure (ULF). ULF testing demonstrated that the VLP (DVR plate) had the highest value and was significantly higher than the DNLP (Lo-Con-T) and DCPs (dual-column plates), but not the IMN (Micronail). The Micronail and the Synthes constructs demonstrated significantly higher ULF as compared to the Lo-Con plate.
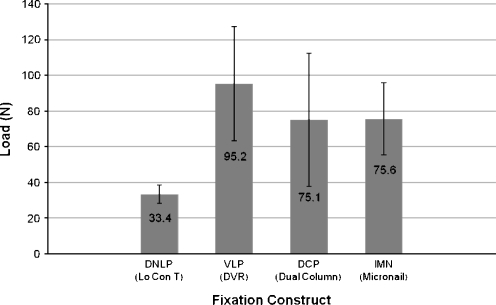
Load measured at 5 mm of displacement was found to be highest in the VLP at 95.2 N, followed by the IMN at 75.6 N, the DCP at 75.1 N, and the DNLP at 33.8 N (Table 1, Fig. 4). Significance testing showed that the VLP (p < 0.001), the IMN (p = 0.013), and the DCP (p = 0.014) withstood higher loads at 5 mm of dorsal displacement than the DNLP.
Table 1.
Summary table.
| Lo-Con-T | DVR | Dual column | Micronail | |
|---|---|---|---|---|
| Bending stiffnessa (N/mm) | 6.8 | 16.7 | 11.8 | 12.6 |
| Ultimate load to failurea (N) | 52.0 | 278.2 | 200.8 | 245.7 |
| Load at 5 mm displacementa (N) | 33.8 | 95.2 | 75.1 | 75.6 |
This table summarizes the results of the four constructs tested with respect to bending stiffness, ultimate load to failure, and load needed to create 5 mm of displacement
aAverage
Figure 4.
Load to create 5 mm displacement. The VLP (DVR) construct required the highest load to displace 5 mm. Significance testing showed that the VLP (DVR), IMN (Micronail) and DCPs constructs all withstood significantly higher loads than the DNLP (Lo-Con-T).
At construct failure (Fig. 5), the mechanism observed showed both the DCPs and DNLP to consistently fail by bending of the plates at the osteotomy gap in all cases. The DNLP had no screw loosening, but the plate always bent at the osteotomy site within the vertical limb of the plate. Regarding the DCP, the dorsal–ulnar plate consistently bent at its midportion, while the radial styloid plate screws loosened or pulled out proximally in three cases and distally in three. The VLP was found to bend at the T-junction in one case, had screw pull-out distally in one case, proximally in another, and had fracture proximally through the shaft screw holes in three cases. The IMN specimens failed proximal to the construct in all cases. The bone fractured at the PMMA block–bone junction in three cases and through the shaft screw holes in the other three. In no cases was there screw pull-out or loosening distally.
Figure 5.
Modes of failure. a Dual-column plating method of failure. Failure of the Synthes plates (DCPs) shows consistent bending of the dorsal-ulnar plate at the osteotomy gap. Note the loosening of the most proximal and pull-out of the distal shaft screws in the radial styloid plate. b Dorsal nonlocked plate method of failure. The dorsally directed load on the distal fragment caused all Lo-Con-T constructs to fail via dorsal plate bending at the osteotomy site, with no screw loosening. c Volar locked plate method of failure. This DVR specimen resulted in fracture of the proximal bone along the shaft screw holes. No distal screw pull-out or loosening is seen. d Intramedullary nail method of failure. Failure of this IMN stabilized radius occurred proximally near the bone–PMMA block junction. The distal radial fragment is still well aligned with no screw pullout.
Discussion
There are several options for fixation of unstable extra-articular distal radius fractures, including external fixation, volar, dorsal, or column plating and intramedullary nail fixation. Dorsal plating has the advantage of providing a biomechanical buttress for dorsally unstable fractures as well as allowing visualization of the articular surface if needed. Biomechanical evaluations have been done to demonstrate appropriate stiffness and strength of various dorsal plating systems. Genesway et al. [5] reported superior results when fresh cadaver specimens were tested using a dorsal blade plate versus the nonlocked dorsal T plate in resisting axial load. This data is consistent with the current thinking that locked plating provides improved rigidity in cancellous bone as found in the distal radius.
Peine et al. [14] compared dual-column titanium plates, the AO π plate, and a 3.5-mm titanium nonlocked T plate system. The dual plating construct included a 2.0-mm dorsoulnar T plate beneath the fourth dorsal compartment and a dorsoradial 2.0 mm dynamic compression plate beneath the second dorsal compartment, with plates lying approximately 60° to each other. Four-point bending followed by dorsal, radial, and ulnar bending forces were placed on the dorsally unstable cadaver models. The dual plating was significantly stiffer than the other two constructs in all bending planes. This construct is similar to the dual-column plates we used in our investigation, except that these screws were not locked to the plate distally as in the current 2.4-mm system.
Volar plating is advantageous because it theoretically avoids the soft-tissue complications associated with dorsal plating. The volar surface may also be easier to align with a plate, since it is a smoother, flatter surface and has thicker cortical bone than the dorsal surface. Koh et al. [8] tested 48 cadaver specimens using two different osteotomy models. Axial loading was done before, after, and between several sets of cyclical loading. Ten different constructs were tested using variations of five volar plating systems: Richards (Smith and Nephew) small stainless steel T plate, stainless steel and titanium Synthes volar locking plates, Synthes small fragment locking compression plate, Avanta large and small volar plates, and the DVR plate with single and double distal rows. All constructs withstood cyclical loading, and there was no significant difference among constructs in ultimate load to failure. The Richards T plate had the highest stiffness and the Synthes titanium plate, the lowest. The locked pegs and screws in the DVR and Synthes plate groups resisted distal fragment hardware pullout, while the other constructs exhibited frank pullout or toggling within the distal screw holes. In this model of axial loading, we again see that locked plating was shown to be advantageous over nonlocked constructs.
Liporace et al. [10] and Chen et al. [4] both assessed biomechanical differences between the Synthes distal radius volar locking plate and Hand Innovations DVR plate. While the loading parameters varied, both authors concluded that there was no statistical difference between the two constructs. In each of these papers, the load was applied axially, and the earlier version of the DVR plate was used. Thus, in axial loading, it appears that locked plating has advantages by minimizing hardware failure, but the type of volar locked plate is not critical.
There have also been several studies which have compared dorsal and volar constructs [1, 9, 13, 19, 20]. However, these studies have varying loading parameters, and their results reach different conclusions that support either dorsal [1, 19, 20] or volar [9, 13] fixation as superior. From these studies, it seems that no definitive statement can be made as to which is the biomechanically superior construct. However, it appears that the various types of constructs would provide adequate stability to allow early physiologic wrist and finger motion and have proven successful in clinical practice [3, 7, 12, 14–17, 21].
Intramedullary stabilization combined with locked screw fixation of distal radius fractures is a relatively new technique. The Hand Innovations Dorsal Nail Plate™ combines a proximal intramedullary component with a more distal dorsal (extramedullary) locked plate. McCall et al. [11] compared its strength to that of the DVR™ and the locking compression plate (LCP) using a dorsally unstable synthetic model. While the LCP was less stiff than the DVR and exhibited more displacement at yield than the DNP and DVR, all three constructs had similar yield strength. However, to our knowledge, ours is the first comparative biomechanical study of a completely intramedullary implant. Our data demonstrate that a locked intramedullary (IM) implant has statistically comparable biomechanical properties to volar locked plating and dual-column plating and superior characteristics to dorsal unlocked plates. With its ultimate load to failure of 245 N, it would be expected that this IM implant could withstand typical loads seen in early postoperative motion [13].
The DNLP (Lo-Con-T), the only nonlocked implant in our group, had significantly lower biomechanical parameters than all other implants. Also, this implant consistently failed at the osteotomy site and weakest point of the plate at the longitudinal and transverse junctions. However, even with these relatively low biomechanical properties, this plate has shown to have good clinical outcomes in recent series [7].
Surprisingly, the dual plate construct had lower stiffness and ultimate load to failure than the other single implant locked constructs. This may be because the main stabilizer to dorsal bending was the small dorsal-ulnar plate that consistently bent, while the radial plate was not in an optimal position to resist dorsal bending. Even though the screws were locked distally and bicortical in diaphyseal bone proximally, screw pullout was seen in all cases. The IM Nail and VLP have more implant metal in the central portion of the radius which may have improved their resistance to dorsal bending.
The VLP had the highest average values in all of the biomechanical properties that we tested: bending rigidity, ultimate load to failure, and force at 5 mm of displacement. Significant differences were seen in all categories compared to dual column and dorsal plating but not to intramedullary nailing. These data validate the use of volar locked plating for the use of unstable distal radius fractures with dorsal comminution. The current DVR plate has seven screw holes distally, and placement of additional screws may have further improved the biomechanical performance.
Analysis of the mode of failure showed that the VLP and IMN failed in similar fashion. The IMN had consistent failure of the bone proximal to the implant in all cases, with no screw pull-out or implant deformation. In most cases, the implant maintained acceptable alignment of the distal fragment even after bone failure proximally. The thickness of the implant and its intramedullary position likely added to the high load to failure. The VLP, which is thicker than the Synthes dual column plates and Lo-Con plates, had screw pull out in only two cases and proximal bone fracture with maintenance of distal alignment after failure in half the cases. One consideration regarding the proximal failure may be regarding the potential stress riser at the proximal end of the implant. However, since there was another stress riser certainly made by potting the radii in cement, it would be impossible to truly draw conclusions about any inherent weakness at the construct interface with the intact bone. Furthermore, failure proximal to the fracture is also a testament to the ability of the construct to actually stabilize the fracture.
There are several limitations to our study. The age and pairing of the specimens was unknown. However, all images were radiographed to rule out any significant bony abnormality. All soft tissues were stripped, removing any possible inherent stability to the model. Although it would have been more physiologic to load the radius through attached wrist or finger extensor tendons, we tested a load directly on the radius. By eliminating soft-tissue contribution, we were better able to determine a clearer analysis of the biomechanical properties of the implants themselves and the implant–bone interface. A complete wedge of bone was removed which is not typical for a distal radius fracture, but our goal was to create the most unstable situation to test the limits of the implants and their fixation into the bone. Dorsal loading was used for a similar reason in order to directly stress the most vulnerable part of the dorsally unstable construct. The inclusion of axial, as well as cyclic, loading may have better mimicked the physiologic stress of postoperative range of motion.
In conclusion, this report compares the biomechanical properties of examples of four different classes of fixation for distal radius fractures: volar locked plating; dorsal unlocked plating; dual-column locked plating; and intramedullary fixation. In this cadaver model, the volar locked plate was found to have the highest average bending rigidity, ultimate load to failure, and load at 5 mm of dorsal displacement. Analysis of this data demonstrated the VLP to have statistically superior biomechanical properties to the dorsal nonlocked plate and the dual-column locked plates but not in comparison to the IMN. The IMN and DCP systems had significantly higher load to failure than the dorsal nonlocked plate. Additionally, this report is the first to provide direct comparative, biomechanical data on these four different types of fixation that all may be used for fixation of similar distal radius fractures. This study illustrates how fixation of distal radius fractures by very different methods can achieve comparable levels of stability.
References
- 1.Blythe M, Stoffel K, Jarrett P, Kuster M. Volar versus dorsal locking plates with and without radial styloid locking plates for the fixation of dorsally comminuted distal radius fractures: a biomechanical study in cadavers. J Hand Surg [Am] 2006;31 10:1587–93, PMID: 17145377. doi:10.1016/j.jhsa.2006.09.011. [DOI] [PubMed]
- 2.Brooks KR, Capo JT, Warburton M, Tan V. Internal fixation of distal radius fractures with novel intramedullary implants. Clin Orthop Relat Res 2006;445:42–50, PMID: 16505729. [DOI] [PubMed]
- 3.Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg [Am] 1998;23 2:300–7, PMID: 9556273. doi:10.1016/S0363-5023(98)80131-7. [DOI] [PubMed]
- 4.Chen L, Dai Q, Wongworawat MD. A biomechanical comparison between two volar locking plate systems for distal radius fractures. Orthopedics 2006;29 10:927–9. PMID: 17061419. [DOI] [PubMed]
- 5.Gesensway D, Putnam MD, Mente PL, Lewis JL. Design and biomechanics of a plate for the distal radius. J Hand Surg [Am] 1995;20 6:1021–7, PMID: 8583051. doi:10.1016/S0363-5023(05)80153-4. [DOI] [PubMed]
- 6.Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function.A prospective study of 73 consecutive patients. J Bone Joint Surg Br 2000;82 3:340–4, PMID: 10813166. doi:10.1302/0301-620X.82B3.10099. [DOI] [PubMed]
- 7.Kamath AF, Zurakowski D, Day CS. Low-profile dorsal plating for dorsally angulated distal radius fractures: an outcomes study. J Hand Surg [Am] 2006;31 7:1061–7, PMID: 16945704. doi:10.1016/j.jhsa.2006.05.008. [DOI] [PubMed]
- 8.Koh S, Morris RP, Patterson RM, Kearney JP, Buford WL Jr, Viegas SF. Volar fixation for dorsally angulated extra-articular fractures of the distal radius: a biomechanical study. J Hand Surg [Am] 2006;31 5:771–9, PMID: 16713841. doi:10.1016/j.jhsa.2006.02.015. [DOI] [PubMed]
- 9.Liporace FA, Gupta S, Jeong GK, Stracher M, Kummer F, Egol KA, et al. A biomechanical comparison of a dorsal 3.5-mm T-plate and a volar fixed-angle plate in a model of dorsally unstable distal radius fractures. J Orthop Trauma 2005;19 3:187–91, PMID: 15758672. doi:10.1097/00005131-200503000-00006. [DOI] [PubMed]
- 10.Liporace FA, Kubiak EN, Jeong GK, Iesaka K, Egol KA, Koval KJ. A biomechanical comparison of two volar locked plates in a dorsally unstable distal radius fracture model. J Trauma 2006;61 3:668–72, PMID: 16967005. doi:10.1097/01.ta.0000234727.51894.7d. [DOI] [PubMed]
- 11.McCall TA, Conrad B, Badman B, Wright T. Volar versus dorsal fixed-angle fixation of dorsally unstable extra-articular distal radius fractures: a biomechanic study. J Hand Surg [Am] 2007;32 6:806–12, PMID: 17606058. doi:10.1016/j.jhsa.2007.04.016. [DOI] [PubMed]
- 12.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am] 2002;27 2:205–15, PMID: 11901379. doi:10.1053/jhsu.2002.32081. [DOI] [PubMed]
- 13.Osada D, Viegas SF, Shah MA, Morris RP, Patterson RM. Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg [Am] 2003;28 1:94–104, PMID: 12563644. doi:10.1053/jhsu.2003.50016. [DOI] [PubMed]
- 14.Peine R, Rikli DA, Hoffmann R, Duda G, Regazzoni P. Comparison of three different plating techniques for the dorsum of the distal radius: a biomechanical study. J Hand Surg [Am] 2000;25 1:29–33, PMID: 10642470. doi:10.1053/jhsu.2000.jhsu025a0029. [DOI] [PubMed]
- 15.Ring D, Jupiter JB, Brennwald J, Buchler U, Hastings H 2nd. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg [Am] 1997;22 5:777–84, PMID: 9330133. doi:10.1016/S0363-5023(97)80069-X. [DOI] [PubMed]
- 16.Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg [Am] 2006;31 3:359–65, PMID: 16516728. doi:10.1016/j.jhsa.2005.10.010. [DOI] [PubMed]
- 17.Simic PM, Robison J, Gardner MJ, Gelberman RH, Weiland AJ, Boyer MI. Treatment of distal radius fractures with a low-profile dorsal plating system: an outcomes assessment. J Hand Surg [Am] 2006;31 3:382–6, PMID: 16516731. doi:10.1016/j.jhsa.2005.10.016. [DOI] [PubMed]
- 18.Tan V, Capo J, Warburton M. Distal radius fracture fixation with an intramedullary nail. Tech Hand Up Extrem Surg 2005;9 4:195–201, PMID: 16340580. doi:10.1097/01.bth.0000190818.66285.b6. [DOI] [PubMed]
- 19.Trease C, McIff T, Toby EB. Locking versus nonlocking T-plates for dorsal and volar fixation of dorsally comminuted distal radius fractures: a biomechanical study. J Hand Surg [Am] 2005;30 4:756–63, PMID: 16039369. doi:10.1016/j.jhsa.2005.04.017. [DOI] [PubMed]
- 20.Willis AA, Kutsumi K, Zobitz ME, Cooney WP 3rd. Internal fixation of dorsally displaced fractures of the distal part of the radius. A biomechanical analysis of volar plate fracture stability. J Bone Joint Surg Am 2006;88 11:2411–7, PMID: 17079398. doi:10.2106/JBJS.E.00946. [DOI] [PubMed]
- 21.Wright TW, Horodyski M, Smith DW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg [Am] 2005;30 2:289–99, Erratum in: J Hand Surg. Am. 2005 May;30. 3.: 629. PMID: 15781351. PubMed-indexed for MEDLINE. doi:10.1016/j.jhsa.2004.11.014. [DOI] [PubMed]