Abstract
Despite the fact that distal radial fracture is the commonest fracture, there is a little evidence-based knowledge about the value of its classification to guide management and predict prognosis. The available classification systems are either complicated or weakly applicable in clinical practice. Older’s classification is the most reliable, but does not cover all radial fracture types. We evaluated the interobserver and intraobserver reliability of a new classification system which is a modification of Older’s classification covering all radial fracture types. Two hundred and thirty-two consecutive adult patients with acute distal radial fractures were blindly evaluated according to the new classification by three orthopedic surgeons twice with 1-year interval. The interobserver reliability was measured using the Fleiss kappa coefficient, and the intraobserver reliability was measured using the Cohen’s kappa coefficient. The new classification showed fair to substantial interobserver and intraobserver reliability, i.e., results comparable to the reliability of commonly used classification systems. The reliability was better for younger patients and when evaluation was carried out by hand-surgery-interested orthopedic surgeons. The new classification system is simple, covers all radial fracture types, and has an acceptable reliability. Further studies are needed to judge its ability to direct management and predict prognosis.
Keywords: Reliability, Classification, Distal radial fractures, Kappa
Introduction
Distal radius fracture (DRF) is the most common fracture encountered in clinical practice [22]. The management of DRF is still controversial and may be influenced by the initial fracture classification [8]. Despite the fact that numerous classification systems have been proposed, e.g., Frykman, Mayo, Melone, and AO, the evaluation of interobserver and intraobserver reliability of these systems has shown unsatisfactory results (Table 1). However, high interobserver agreement and intraobserver reproducibility were found by Andersen et al. [1] when Older’s classification (Table 2) was used to evaluate the need of reduction and to choose the initial treatment. Furthermore, Solgaard [20, 21] found that this classification was of prognostic significance, as it could predict the risk of fracture re-displacement. We believe that Older’s classification can be improved in order to cover more patterns of distal radial fractures. In Older’s classification, several different parameters such as the length of the radial styloid, the dorsal angulation, and the comminution of the dorsal cortex are measured. However, there is an overlap between the measurements and groups, and this could cause confusion and compromise inter- and intraobserver reliability. Furthermore, Older’s classification does not take into consideration comminution of the volar cortex. Although unproven yet, we believe that the volar cortex and comminution of it is of uttermost importance for fracture stability and choice of treatment, as it behaves as the calcar of the distal radius [6, 17].
Table 1.
Examples of studies tested different classification systems of DRF.
| Study | Classification systems tested | No. of patients | No. of observers | Reliability | |
|---|---|---|---|---|---|
| Interobserver | Intraobserver | ||||
| Andersson et al. 1996 [2] | Frykman | 55 | 4 | Fair | Fair–moderate |
| Melone | Fair | Fair–moderate | |||
| Mayo | Moderate | Fair–moderate | |||
| AO | Fair | Fair | |||
| Flinkkilä et al. 1998[7] | AO | 30 | 5 | Poor–fair | Not tested |
| Illarramendi et al. 1998 [9] | Frykman | 200 | 3 | Moderate | Substantial |
| AO | Fair | Moderate | |||
| Filho et al. 2004 [5] | Frykman | 40 | Fair | Moderate | |
| AO | Poor | Fair | |||
| Universal | Fair | Moderate | |||
| Jin et al. 2007 [10] | AO | 43 | 3 | Fair–moderate | Fair–moderate |
| Frykman | Fair–moderate | Moderate | |||
| Cooney | Fair–moderate | Moderate–substantial | |||
Table 2.
Older’s [18] classification of distal radial fractures.
| Type I: Non-displaced, length of radial styloid ≥7 mm, dorsal angulation ≤5°. |
| Type II: Displaced with minimal comminution of dorsal radius, length of radial styloid <7 mm and ≥1 mm, dorsal angulation >5°. |
| Type III: Displaced with slight dorsal comminution, length of radial styloid ≤4, dorsal angulation >5°. |
| Type IV: Comminution of distal radius (including the dorsal part), often with intraarticular involvement. Length of radial styloid usually negative, dorsal angulation >5°. |
The purpose of this study was to evaluate the interobserver and intraobserver reliability of a new classification system which was developed by one of the authors (GB). The new classification represents a modification of Older’s classification evaluating fracture stability. The main parameters evaluated were the degree of comminution of the dorsal and volar cortices of the distal radius as well as the involvement of radio-carpal articular surface.
Material and Methods
Patients
The antero-posterior and lateral plain radiographs of 232 consecutive DRF in adults (growth plates fused) during January to December 2002 seeking treatment at Östersunds Hospital, Sweden were evaluated. No patients were excluded. We have analyzed the patients in two ways. Firstly, as one group to study the reliability in the whole cohort. Secondly, due to the etiological differences among different age groups found by others [12, 15], our patients were divided into two groups: the first group (the elderly group, 155 patients) included men older than 59 years and women older than 49 years. Distal radial fractures in this age group were operationally considered osteoporotic [12, 15]. The second group (the young group, 77 patients) included the remaining patients. The most common type of DRF in this group is high energy trauma [15].
Presentation of the New Classification
Distal radial fractures are classified according to the new classification system into:
extraarticular DRF with no cortical (metaphyseal) comminution;
extraarticular DRF with comminution of the dorsal cortex;
intraarticular (radio-carpal joint) DRF with or without metaphyseal comminution (completely articular fractures as in AO classification type C);
DRF with comminution of the volar cortex regardless of other coexisting fracture lines;
DRF which cannot be classified according to the above types such as intraarticular fractures without metaphyseal comminution (partially articular fractures), e.g., carpal fracture-dislocation, Barton fractures and Chauffeur fractures.
The difference between Buttazzoni 1 and 2 is only the comminution of the dorsal cortex. Thereafter, the classification is hierarchal, i.e., if the fracture is intraarticular, it will be classified as Buttazzoni 3 regardless of dorsal metaphyseal comminution. Likewise, if the fracture has comminution of the volar cortex, it will be classified as Buttazzoni 4 regardless of both dorsal comminution and if it is intraarticular (Fig. 1a–e).
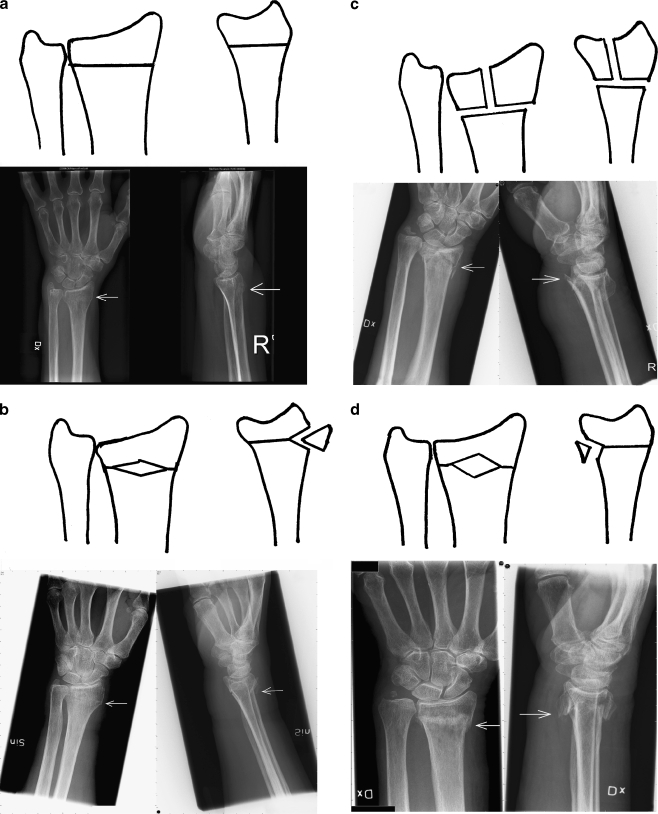
Figure 1.
a Buttazzoni 1 DRF. Extraarticular with no cortical comminution. b Buttazzoni 2 DRF. Extraarticular with dorsal cortical comminution. c Buttazzoni 3 DRF. Intraarticular fracture with metaphyseal involvement. d Buttazzoni 4 DRF. Extraarticular with volar cortical comminution. e Buttazzoni 0 DRF. Fractures not classified elsewhere according to the new system belong to this type, e.g., partially articular fractures without metaphyseal involvement. Volar Barton is shown on the right and Chauffeur on the left.
Evaluation of Radiographs According to the New Classification
To assess the interobserver reliability, evaluation of radiographs was performed by three orthopedic surgeons: observer 1 had developed the classification system. Observer 2 was a hand-surgery-interested orthopedic surgeon with limited previous experience of this classification system and, observer 3 was a general orthopedic surgeon with limited experience of this classification system. The content of the new classification was made available for the observers during the assessment, but no other information was given. All the observers were blinded to each other’s results. The observers reclassified the fractures 1 year after the first assessment, unaware of previous classification.
Statistical Analysis
Assessment of intraobserver reliability was accomplished by the use of Cohen’s kappa coefficient, and assessment of interobserver reliability between the three observers at a time was accomplished by the use of Fleiss kappa (Table 3) as proposed by Landis and Koch [13]. The kappa value ranges from −1.0 (complete disagreement) through 0.0 (chance agreement) to 1.0 (complete agreement).
Table 3.
Landis and Koch interpretation of kappa values.
| Κ | Interpretation |
|---|---|
| <0 | No agreement |
| 0.0–0.20 | Slight agreement |
| 0.21–0.40 | Fair agreement |
| 0.41–0.60 | Moderate agreement |
| 0.61–0.80 | Substantial agreement |
| 0.81–1.00 | Almost perfect agreement |
Results
Interobserver Reliability
The Fleiss kappa value for the whole group regardless of the age of the patient was 0.47 (moderate). When separated, the Fleiss kappa was 0.42 (moderate) for the elderly group and 0.54 (moderate) for the young group.
Intraobserver Reliability
The mean kappa values for intraobserver reproducibility for observer 1 was 0.52 (moderate) for the whole group, 0.45 (moderate) for the elderly group, and 0.62 (substantial) for the young group. For observer 2, the mean kappa values was 0.61 (substantial) for the whole group, 0.57 (moderate) for the elderly group, and 0.68 (substantial) for the young group. For observer 3, the mean kappa values was 0.29 (fair) for the whole group, 0.28 (fair) for the elderly group, and 0.30 (fair) for the young group.
The mean kappa values for interobserver and intraobserver reliability among observers are shown in Tables 4 and 5.
Table 4.
Interobserver reliability of the classification using the Fleiss kappa.
| Interobserver reliability | The entire cohort | The young group | The elderly group |
|---|---|---|---|
| Observers 1, 2, 3 | 0.47 (moderate) | 0.54 (moderate) | 0.42 (moderate) |
Table 5.
Intraobserver reproducibility of the classification using the Cohen kappa.
| Intraobserver reproducibility | The entire cohort | The young group | The elderly group |
|---|---|---|---|
| Observer 1 | 0.52 (moderate) | 0.62 (substantial) | 0.45 (moderate) |
| Observer 2 | 0.61 (substantial) | 0.68 (substantial) | 0.57 (moderate) |
| Observer 3 | 0.29 (fair) | 0.30 (fair) | 0.28 (fair) |
Discussion
The use of fracture classification systems is quite common in clinical practice and aims to gain insight into the mechanism, management plan, and prognosis of a given fracture. Furthermore, a common language among clinicians is created to communicate and compare results published in different studies.
The classification system should be simple, reliable, clinically relevant, and all-inclusive and with as few subtypes as possible. Audigé et al. [3] and Slongo et al. [19] stated that any classification system should be evaluated among observers at different stages of experience to assess its reliability and accuracy. Thereafter, its use can be validated for assessing treatment options and outcomes.
Many studies have shown that comminution of the dorsal cortex is of prognostic significance for stability of a reduced DRF [17, 18, 21]. Intraarticularity in the radiocarpal joint is a prognostic factor in itself for posttraumatic arthrosis [11], but also for instability and other intraarticular pathology. This is true for fractures in young subjects, but not investigated in the elderly. The rationale for adding comminution of the volar cortex is that there is evidence suggesting that this factor itself adds to the instability of the fracture [6]. The distal joint surface of the radius is centered over the distal projection of the volar cortex, not over the center of the shaft. On a lateral view, a line drawn over and parallel to the volar cortex of the radial shaft will cross through the middle of the joint and pin the radial styloid. This line is normally called the “volar line of Lewis”. The fact that the volar cortex is thicker than the dorsal cortex [6] implicates that most of the load over the radiocarpal joint passes through the volar cortex if the joint is anatomically placed. Consequently, if a radius fracture is anatomically reduced, the load applied over the joint while exercising finger motion will be transmitted through the volar cortex. As classifications of DRF until now have not addressed this problem, very little has been written on the matter. Our theory is that comminution of the volar cortex (which is considered as the calcar of the wrist) is as relevant as comminution of the calcar of the proximal femur.
In this paper, as recommended by Audigé and Slongo [3, 19], we have evaluated the interobserver and intraobserver reliability of the Buttazzoni classification. The next step will be to determine if this classification has a prognostic significance and can justify clinical decision making and outcome prediction.
The classification system used in this study is fairly simple and depends on the configuration of the fracture. There are no measurements of displacement, angulation, or radial shortening in contrast to many other classifications. The only parameters to look at are: dorsal metaphyseal comminution, intraarticularity, and volar metaphyseal comminution. This could minimize disagreement between observers encountered in certain fracture patterns.
We believe that our classification system can be clinically relevant and each fracture type can be given a suggestion for a specific treatment. For example, Buttazzoni 1 fractures may be considered stable with minimal risk of further displacement, and these fractures could be treated with a brace. Buttazzoni 2 fractures are thought to be less stable due to lack of dorsal support and are best managed by closed reduction and a plaster cast, pinning or external fixation. Buttazzoni 3 fractures are treated according to the degree of intraarticular step-off and metaphyseal comminution. If the intraarticular step-off is 2 mm or more, open reduction and internal fixation is considered to restore the articular surface. We believe that Buttazzoni 4 fractures are axially unstable and have high risk of re-displacement. They can be treated with open reduction and plating since radial length cannot be held with pins nor bridging external fixation alone or in combination with pinning. William P. Cooney [4] referred to open reduction of distal radius fractures as he stated: “For Colles’-type fractures, a palmar incision may be necessary if there is a pronator quadratus interposition or if there is a palmar bone spike fracture”. Buttazzoni 0 fractures are treated according to the type and configuration of the fracture, e.g., open reduction and plating in Barton fractures.
Despite that the ideal classification should have a reliability which is the same regardless of the age of the patients, we chose to study the reliability of the Buttazzoni classification in different age groups in addition to the whole cohort. Lindau et al. [15] found that distal radial fractures in men younger than 60 and women younger than 50 represent a special group and were intraarticular in more than two thirds of the cases, displaced in 50%, and were mostly caused by severe trauma. Furthermore, they were often combined with intraarticular pathology as intercarpal ligament ruptures, triangular fibro cartilaginous complex pathology, and cartilage damage. Because of these factors, we believe that this group of patients probably has another outcome and should be looked at separately in studies to come.
The interobserver and intraobserver reliability of the classification system used in this study was comparable and in some aspects better than other classification systems (Table 1). We found that both interobserver and intraobserver reliability was better in the (young) group. This might be due to the better bone quality in this group allowing easier and more reliable evaluation of radiographs.
In accordance with the recommendation made by Audigé et al. [3], the evaluation of this classification system was made by two orthopedic surgeons with special interest in hand surgery as well as one general orthopedic surgeon. The 1-year interval between the first and second evaluation of radiographs minimized bias due to remembering some of these. The quality of the evaluated radiographs was similar to those used in everyday practice, i.e., we demanded no high-quality films or special views to make the evaluation.
The present classification system covers all common types of distal radial fractures, i.e., all inclusive despite containing no subtypes. Other classifications such as the AO classification contain numerous subtypes which give rise to confusion and unsatisfactory reliability [2, 5, 7, 9]. However, the Buttazzoni classification has some limitations. It does not take into account problems with the distal radioulnar joint or intercarpal instability which might affect the long-term outcome of DRF [14, 16].
In conclusion, the new classification system presented in this study has shown comparable characteristics to those of previously studied classification systems. Further investigations are warranted to determine its application consistency and ability to direct treatment options and predict prognosis.
References
- 1.Andersen GR, Rasmussen JB, Dahl B, Solgaard S. Older’s classification of Colles’ fractures. Good intraobserver and interobserver reproducibility in 185 cases. Acta Orthop Scand 1991;62(5):463–4. [DOI] [PubMed]
- 2.Andersen DJ, Blair WF, Steyers CM Jr, Adams BD, el-Khouri GY, Brandser EA. Classification of distal radius fractures: an analysis of interobserver reliability and intraobserver reproducibility. J Hand Surg (Am) 1996;21(4):574–82. doi:10.1016/S0363-5023(96)80006-2. [DOI] [PubMed]
- 3.Audigé L, Bhandari M, Hanson B, Kellam J. A concept for the validation of fracture classifications. J Orthop Trauma 2005;19(6):401–6. (review). [DOI] [PubMed]
- 4.Cooney WP. The wrist: diagnosis and operative treatment, vol. 1. St. Louis: Mosby; 1998. p. 330.
- 5.de Oliveira Filho OM, Belangero WD, Teles JB. Distal radius fractures: consistency of the classifications. Rev Assoc Med Bras 2004;50(1):55–61. (Abstract, article in Portuguese). [DOI] [PubMed]
- 6.Dhillon SS, Kumar AJ, Sadaiyyappan V, Bassi RS, Shanahan D, Deshmukh SC. Anatomical study comparing the thickness of the volar and dorsal cortex of cadaveric adult distal radii using digital photography. Arch Orthop Trauma Surg 2007;127(10):975–7. doi:10.1007/s00402-007-0394-8. [DOI] [PubMed]
- 7.Flinkkilä T, Raatikainen T, Hämäläinen M. AO and Frykman’s classifications of Colles’ fracture. No prognostic value in 652 patients evaluated after 5 years. Acta Orthop Scand 1998;69(1):77–81. [DOI] [PubMed]
- 8.Handoll HH, Madhok RM. Surgical interventions for treating distal radius fractures in adults. Cochrane Database Syst Rev 2003;3:37–8. [DOI] [PubMed]
- 9.Illarramendi A, González Della Valle A, Segal E, De Carli P, Maignon G, Gallucci G. Evaluation of simplified Frykman and AO classifications of fractures of the distal radius. Assessment of interobserver and intraobserver agreement. Int Orthop 1998;22(2):111–5. doi:10.1007/s002640050220. [DOI] [PMC free article] [PubMed]
- 10.Jin WJ, Jiang LS, Shen L, Lu H, Cui YM, Zhou Q, et al. The interobserver and intraobserver reliability of the Cooney classification of distal radius fractures between experienced orthopaedic surgeons. J Hand Surg Eur 2007;32(5):509–11. doi:10.1016/j.jhse.2007.03.002. [DOI] [PubMed]
- 11.Jupiter JB, Fernandez DL, Whipple TL, Richards RR. Intra-articular fractures of the distal radius: contemporary perspectives. Instr Course Lect 1998;47:191–202. [PubMed]
- 12.Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg (Br) 1993;18(1):45–9. doi:10.1016/0266-7681(93)90195-L. [DOI] [PubMed]
- 13.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977;33(2):363–74. doi:10.2307/2529786. [DOI] [PubMed]
- 14.Lindau T, Aspenberg P. The radioulnar joint in distal radial fractures. Acta Orthop Scand 2002;73(5):579–88 (review). doi:10.1080/000164702321022884(review). [DOI] [PubMed]
- 15.Lindau TR, Aspenberg P, Arner M, Redlundh-Johnell I, Hagberg L. Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand 1999;70(2):124–8. [DOI] [PubMed]
- 16.Lindau T, Hagberg L, Adlercreutz C, Jonsson K, Aspenberg P. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res 2000;376:229–35. doi:10.1097/00003086-200007000-00031. [DOI] [PubMed]
- 17.Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Jt Surg Am 2006;88:1944–51. doi:10.2106/JBJS.D.02520. [DOI] [PubMed]
- 18.Older TM, Vernon Stabler E, Cassebaum WH. Colles fracture: evaluation and selection of therapy. J Trauma 1965;5:469–76. doi:10.1097/00005373-196507000-00004. [DOI] [PubMed]
- 19.Slongo T, Audigé L, Lutz N, Frick S, Schmittenbecher P, Hunter J, et al. Documentation of fracture severity with the AO classification of pediatric long-bone fractures. Acta Orthop 2007;78(2):247–53. doi:10.1080/17453670710013753. [DOI] [PubMed]
- 20.Solgaard S. Classification of distal radius fractures. Acta Orthop Scand 1985;56(3):249–52. [DOI] [PubMed]
- 21.Solgaard S. Early displacement of distal radial fracture. Acta Orthop Scand 1986;57:229–31. [DOI] [PubMed]
- 22.van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone 2001;29:517–22. doi:10.1016/S8756-3282(01)00614-7. [DOI] [PubMed]