INTRODUCTION
Today there are remarkable opportunities for those seeking a career in urologic oncology. The revolution in molecular biology and advances in sophisticated technology will permanently change the way we care for patients with genitourinary malignancies. Minimally invasive surgical approaches are being developed for almost all urologic cancers, and image-guided intervention is providing an innovative option for treatment of very early cancers. The ability to characterize these cancers with modern imaging tools including magnetic resonance imaging and spectroscopy, dynamic PET scanning, and PET-CT fusion promises real improvements in preoperative staging and surgical planning. Genomic and proteomic analyses provide new insights into the biologic potential and growth control mechanisms of these tumors. Modern clinical evaluative science “outcomes research” provides new objective tools for assessing results. Patient-completed questionnaires and standardized assessment of individual patient preferences have helped us understand survivorship issues of urologic oncology patients, including long-term effects of treatment and quality of life. Medical informatics provides new tools such as nomograms to calculate risks for the individual patient. By embracing such developments, urologic oncologists can achieve better results by providing risk-adjusted therapy: treatment tailored to the particular characteristics of the cancer in each individual patient, an approach designed to maximize longevity with the least risk to quality of life.
Surgical excellence remains critically important in the field of urologic oncology. The development of modern chemotherapy for germ cell tumors did not eliminate the need for surgery, but challenged surgeons to learn to operate on highly complex tumors while reducing the burden of surgical morbidity. Similarily, chemotherapy for bladder cancer has expanded the role of surgery, with resection of previously inoperable cancer now common. Future leaders in urologic oncology must be highly skilled surgeons capable of open, free-hand, and robotic-assisted laparoscopic techniques and image-guided therapy, and also be scholars, well versed in the nuances of modern diagnostic and staging procedures, fully appreciative of the benefits and limitations of systemic therapy (chemotherapy, immunological, and biologic therapy) and radiation therapy.
Complete training requires equally intensive exposure to research, either in the basic sciences, translational research, or clinical trials. This will prepare future urologists to explore hypotheses about urological malignancies in an effort to improve patient care.
SOCIETY OF UROLOGIC ONCOLOGY
The Society of Urologic Oncology (SUO) was founded in 1984, and currently there are 16 academic centers that offer SUO-approved fellowships for urologic oncology (Table 1). According to the SUO membership details, essential requirements of the urologic oncologist includes expertise in multidisciplinary care, ability to perform and understand the limitations of complex tumor resections, extensive knowledge of urinary tract diversion, a clear understanding of the biology and scientific methodology of urologic malignancies, and ability to collaborate in translational research.1 Detailed essential requirements for the urologic oncologist are further demonstrated in Table 2.1 Active membership in the SUO is limited to physicians who devote >75% of their total professional effort to the field of urologic cancer, have published oncologic papers in national medical journals, are board certified by the American Urological Association or respective equivalent in their country of origin, have at least 2 years of oncologic experience following formal urologic training, and have performed at least 50 urologic oncology operative procedures during the previous year (documentation required).
Table 1.
Society of Urologic Oncology approved fellowships and contact information
| Approved Program | Location | Program Director | Contact Information |
|---|---|---|---|
| Duke University | Durham, NC | Judd W. Moul, MD | (919) 684-5057 judd.moul@duke.edu |
| Mayo Clinic | Rochester, MN | Bradley C. Leibovich, MD | (507) 284-3981 leibovich.bradley@mayo.edu |
| MD Anderson Cancer Center | Houston, TX | Ashish M. Kamat, MD | (713) 792-3250 akamat@mdanderson.org |
| Memorial Sloan-Kettering Cancer Center | New York, NY | Joel Sheinfeld, MD | (212) 639-2593 sheinfej@mskcc.org |
| National Cancer Institute | Bethesda, MD | W. Marston Linehan, MD | (301) 496-6353 linehanm@mail.nih.gov |
| University of California-Los Angeles | Los Angeles, CA | Arie Belldegrun, MD | (310) 206-1434 abelldegrun@mednet.ucla.edu |
| University of California-San Francisco | San Francisco, CA | Christopher Kane, MD | (415) 885-3660 ckane@urol.ucsf.edu |
| University of Chicago | Chicago, IL | Gary Steinberg, MD | (773) 702-3080 gsteinbe@surgery.bsd.uchicago.edu |
| University of Indiana | Indiana, IN | Michael Koch, MD | (317) 274-7338 miokoch@iupui.edu |
| University of Miami | Miami, FL | Mark S. Soloway, MD | (305) 243-6596 msoloway@maimi.edu |
| University of Michigan | Ann Arbor, MI | David P. Wood Jr., MD | (734) 763-9269 davwood@umich.edu |
| University of Texas Health Science Center | San Antonio, TX | Ian M. Thompson, MD | (210) 567-5644 thompsoni@uthscsa.edu |
| University of Toronto | Ontario, Canada | Laurence Klotz, MD | (416) 480-4673 Laurence.klotz@sunnybrook.ca |
| University of Washington | Seattle, WA | Paul H. Lange, MD | (206) 543-3918 lange@u.washington.edu |
| University of Western Ontario | Ontario, Canada | Joseph Chin, MD | (519) 685-8451 jchin@lhsc.on.ca |
| Vanderbilt University | Nashville, TN | Joseph A. Smith Jr., MD | (615) 343-5604 joseph.smith@vanderbilt.edu |
Table 2.
Essential requirements for a fellowship trained urologic oncologic surgeon
|
The goal of advanced training in urologic oncology is to enhance knowledge and skills beyond the expertise obtained during a urology residency program. The urologic oncology program must be associated with an ACGME accredited urologic training program or an NCI designated cancer center. Admission to a SUO program requires completion of an ACGME accredited urologic training program or an appropriate foreign program. The minimum duration of fellowship training is 24 months, with a minimum of 12 months of clinical exposure and 12 months of research. Applicants who have completed post-doctoral research in urologic oncology under the auspices of governing bodies, such as the NIH, can prospectively apply to have their 12 month research requirement waived.
Most SUO programs are between 2 and 3 years, although longer protected time in a research lab can usually be arranged for applicants desiring a career with a strong basic science component. All programs are required to provide a structured educational experience at an advanced level to ensure that trainees acquire the knowledge and skills necessary to obtained expertise beyond that acquired in residency.1 Access to dedicated individuals in medical oncology, radiation oncology, pathology, and radiology who have expertise in urologic malignancies is an additional requirement for the trainees. Programs must provide structured clinical opportunities for trainees to develop advanced skills in urologic surgery including exposure to laparoscopic approaches to urologic tumors. Each fellow should be involved (either as surgeon or first assistant) in at least 100 major surgical procedures for the treatment of urologic cancers.1 Additionally, an active research component is required with meaningful supervised research. If basic science laboratory training is offered, the necessary facilities must be available under the supervision of a mentor who has demonstrated a national reputation in basic science research evidenced by national grant support, publications in peer-reviewed journals, and membership in prestigious societies. As an example of one of the SUO-approved fellowships, the following section describes the fellowship experience at Memorial Sloan Kettering Cancer Center (MSKCC).
THE MEMORIAL SLOAN KETTERING EXPERIENCE
Memorial Sloan-Kettering’s tradition of care began more than a century ago in 1884. In 1960, Memorial Hospital (known for treatment of cancer and allied diseases) joined with the Sloan-Kettering Institute (known for innovative basic science research) to form the Memorial Sloan-Kettering Cancer Center (MSKCC). Located on the upper east side of Manhattan, the collaboration between scientists and physicians provides a unique strength, assuring that new research findings are appropriately and rapidly transferred from the laboratory directly to patient care.
The specialty of urologic oncology in the United States began at MSKCC under the leadership of Dr. Willet Whitmore, Jr. Through his keen understanding of biology and natural history of genitourinary cancers, and his remarkable teaching ability, Dr. Whitmore attracted many of the leading young urologists to train as fellows. MSKCC has the oldest and most well-established fellowship in urologic oncology in the world. Currently, 4 to 6 graduating residents begin fellowship training in urologic oncology that is comprised of 18 months of clinical urologic oncology, including laparoscopic and robotic urologic cancer surgery and 12 months in basic or translational research. For fellows interested in a career in academic research, opportunities for 18–24 months of research in one of the many areas of clinical and laboratory research within MSKCC or at the neighboring institutions of Cornell University and Rockefeller University are readily available. Critical elements that we believe are essential for comprehensive training of the urologic oncology surgeon are detailed in Table 3.
Table 3.
Essential elements in a fellowship program for comprehensive training of future uro-oncology surgeons
|
Program Description
The goal of the MSKCC Urologic Oncology Fellowship Program remains the same today as when it was initiated by Dr. Whitmore: to produce for the nation a larger cadre of superbly trained clinical scientists who will become leaders in academic urologic oncology and be highly qualified to promote improvements in medical care made possible by the developments in modern biomedical science in order to reduce the incidence, morbidity, and mortality of cancer.2 The Urology Service at MSKCC currently has 17 faculty members including experts in medical informatics, urodynamics, reconstructive surgery, erectile dysfunction, tumor markers, and laparoscopic surgery.
A multidisciplinary approach to oncology represents the hallmark of the MSKCC program.3 As demonstrated in Figure 1, at the center of the MSKCC program are multidisciplinary organ working groups. These disease management teams include specific cancer sites (prostate, testis, bladder, and kidney) and are comprised of urologic surgeons, medical oncologists, radiation oncologists, pathologists, radiologists, and basic laboratory researchers. Working in these disease management teams, fellows have an opportunity to participate in the development of multidisciplinary management plans for patients as well as design and pursue research opportunities including clinical trials. The CAISIS database is a powerful computer network that is prospectively maintained and directed by research assistants and biostatisticians. The CAISIS database is utilized by each disease management team that facilitates basic, clinical, and translational research, and ultimately guides and supports the rational for effective clinical trials. Additionally, these multidisciplinary disease management teams facilitate the rapid translation of basic research into the clinical setting.
Figure 1.
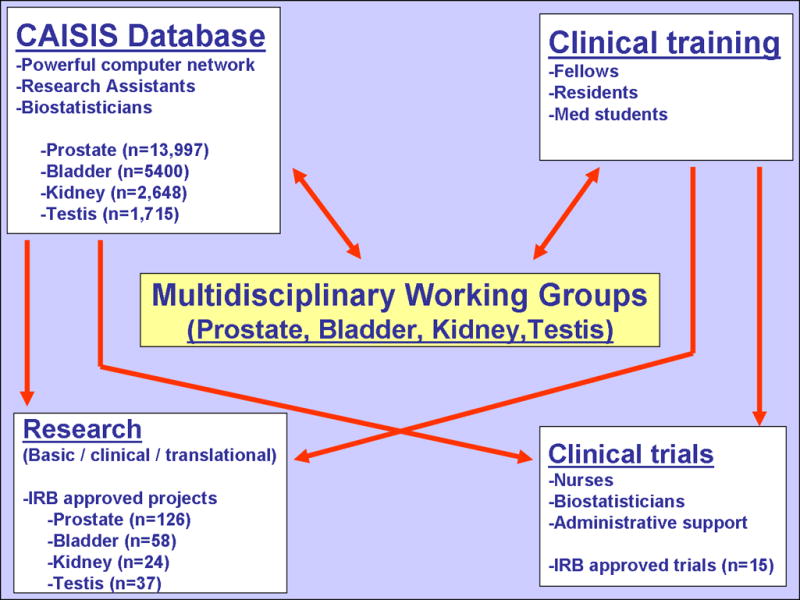
Multi-disciplinary approach to patient care and research at MSKCC
Clinical Experience
The clinical program is designed to provide the fellow with a practical knowledge of the most up-to-date methods of diagnosing and treating urologic cancers. The aim is to develop familiarity with and stimulate interest in clinical and laboratory studies designed to advance knowledge in the field. The responsibilities for clinical care are shared by the faculty, fellows, residents, medical students, and physician assistants. Fellows are directly involved in the management of patients with urologic malignancies or patients with urologic problems arising from or coincident with the treatment of neoplasms outside the urinary tract. This includes pre-and postoperative patient care as well as rotations in medical oncology, radiation oncology, and gynecologic oncology. The volume and nature of the clinical experience is such that the fellow has an opportunity to participate in the management of patients with all types and stages of urologic cancer.
In the past year, nearly 5,000 new patients were evaluated by the Urology Service (Figure 1). Surgical volume has steadily increased with 119 retroperitoneal lymph node dissections, 222 radical cystectomies, 117 radical and 161 partial nephrectomies, and 715 radical prostatectomies were performed at MSKCC in 2006 alone (Figure 2).2 In total, nearly 3,000 major or minor operations are performed yearly by the Urology Service at MSKCC.
Figure 2.
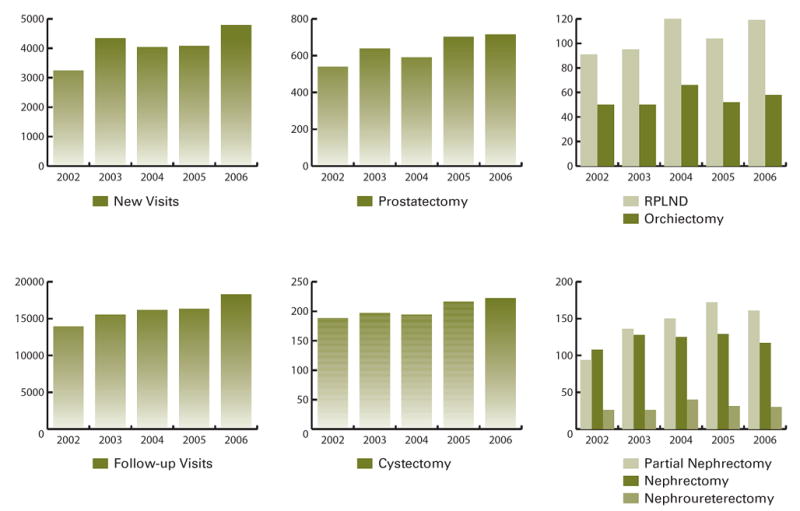
Volume of patients and surgical procedures at MSKCC by year
Laparoscopic and Minimally Invasive Surgery Program
Laparoscopic and Minimally Invasive Surgery are being adapted to surgical care in general and applied to the specialty of urologic oncology as a result of improvements in instrumentation and increasing experience. There are currently 7 surgeons at MSKCC who specialize and perform laparoscopic and robotic-assisted surgery. The training program in laparoscopy and robotic-assisted surgery encompasses major procedures in the field that involve upper- and lower-tract organ systems, including adrenalectomy, partial and radical nephrectomy, nephroureterectomy, prostatectomy, and reconstructive procedures for the female pelvic floor. Future multidisciplinary programs currently under development include image-guided percutaneous and laparoscopic procedures for cryoablation, functional tumor imaging with image-guided biopsy and treatment, and lymphatic staging and mapping studies. Fellows are involved on multiple levels through a graduated, continuous experience throughout their training, which is designed to provide a sound foundation for the subsequent progress toward mastery of advanced laparoscopic and robotic-assisted techniques.
To help facilitate the fellow’s role, dry laboratory facilities, laparoscopic simulators, perfused-organ models, and remote-controlled manipulators are being planned with expected implementation over the next 18 months.2 Additionally, future program expansion will include state-of-the-art facilities with a live animal vivarium to allow for the critical evaluation of current laparoscopic and image guided therapeutics as they apply to surgical outcome.2 The minimally invasive surgical program collaborates with bio-engineering in instrument and biomaterial development for training, diagnosis, and therapeutics in urologic oncology. Once the program expansion is implemented, fellows will have an opportunity to play a role in the critical steps of trial design as well as participate in performing percutaneous image-guided procedures.
Research Experience
Urology Service faculty at MSKCC are involved in many areas of research related to oncology, including MIS, medical informatics and outcomes research, pathology, radiology, clinical trials, or one of the many research laboratories at MSKCC, Weill Medical College of Cornell University, or Rockefeller University. Many fellows have successfully competed for individual funding for their research experience through the American Urological Association Foundation Research Fellowships and the American Cancer Society Fellowships. This is accomplished by working closely with interested candidates to prepare competitive applications. The Urology Service also sponsors research fellowships through the NCI T32 training grant and the Career Development Program of the SPORE in prostate cancer.
Sloan-Kettering Institute (SKI) has a professional staff of over 200 faculty. At SKI, all approaches, from the most basic and theoretical to the most pragmatic and applied, are utilized in advancing biological knowledge and discovering or improving means for the detection, diagnosis, treatment, and prevention of cancer. The research programs of SKI now occupy about half a million square feet in four buildings including the new 23-story Zuckerman Research Center, which is uniquely designed to foster interaction and collaboration among researchers from different disciplines. Within MSKCC, 31 core facilities such as the human Tissue Procurement and Tissue Bank, Immunohistochemistry Laboratory, Nuclear Magnetic Resonance Analytical Facility, radiation Biophysics Facility, and the Monoclonal Antibody Production Facility support basic and clinical research.
MSKCC has made a major commitment to translation research through the initiation of the Human Oncology and Pathogenesis Program with long-term goals to discover and develop novel approaches to detection, diagnosis, treatment, and prevention of cancer. Additional areas for focused research include characterization of molecular alterations in human cancers, evaluation of tumor suppressors in human carcinogenesis and leukemogenesis, epidemiology and the study of outcomes and quality of care using population based data, immunology and manipulation of the immune response in cancer, gene therapy, tumor markers, imaging techniques, erectile dysfunction and cellular mechanisms of peyronie’s disease.
Didactic Education
In addition to patient care and clinical research, the Urology Service has a formal program for education in urologic oncology.3 The training experience is enhanced by a didactics course in urologic oncology, a course in biostatistics, weekly grand rounds that focus on integrating a multidisciplinary approach to oncology along with weekly research conferences. The didactic lecture series is detailed in Table 4. The goal of the educational program is to provide a broad view of all aspects of genitourinary cancer, and a complete familiarity with all diagnostic and therapeutic approaches. Rotations on medical oncology are supplemented by formal lectures on systemic therapy. Similarly, radiation oncologists lecture on external beam and brachytherapy strategies to supplement the clinical experience in radiation oncology.
Table 4.
Formal didactic lecture series given yearly at MSKCC. Each lecture has a comprehensive updated reading list of most pertinent articles
| Bladder Cancer | Testis Cancer |
|---|---|
| 1) Overview and molecular biology of bladder cancer-Bernard H. Bochner, MD | 1) Retroperitoneal lymph node dissection- Joel Sheinfeld, MD |
| 2) Superficial cancer (Ta-CIS-T1): Natural history, diagnosis, monitoring, and staging- Harry Herr, MD | 2) Low stage non-seminomatous germ cell tumors- Joel Sheinfeld, MD |
| 3) Superficial cancer: Role of intravesical chemotherapy- Harry Herr, MD | 3) Management of seminoma- Joel Sheinfeld, MD |
| 4) Pathology of urothelial cancer- Victor Reuter, MD | 4) Pathology of germ cell tumors- Victor Reuter, MD |
| 5) Radiographic imaging of urothelial cancer- Jingbo Zhang, MD | 5) Chemotherapy for germ cell tumors- George J. Bosl, MD |
| 6) Surgical management of invasive cancer- Bernard H. Bochner, MD | 6) Management of advanced-stage- Joel Sheinfeld, MD |
| 7) Urinary tract reconstruction- Bernard H. Bochner, MD | |
| 8) Chemotherapy for urothelial tumors- Dean F. Bajorin, MD | Kidney Cancer |
| 9) Role of radiation and bladder preservation- Michael J. Zalefsky, MD and S. Machele Donat, MD | 1) Overview- Paul Russo, MD |
| 10) Management of urethral and ureteral cancers-Guido Dalbagni, MD and S. Machele Donat, MD | 2) Pathology of tumors in adults- Paul Russo, MD and Satish Tickoo, MD |
| 3) Open partial nephrectomy- Paul Russo, MD | |
| Prostate Cancer | 4) Minimally invasive surgery- Karim A. Touijer, MD |
| 1) Prostate cancer: A perspective- Peter T. Scardino, MD | 5) Advanced and metastatic tumor surgery- Paul Russo, MD |
| 2) Modern radiological imaging of prostate cancer- Hedvig Hricak, MD, PhD | 6) Medical management of metastatic disease- Robert J. Motzer, MD |
| 3) Pathology of prostate cancer- Samson Fine, MD | |
| 3) Laparoscopic radical prostatectomy- Karim A. Touijer, MD | Other Lectures |
| 4) Prevention and early detection of prostate cancer- Hans Lilja, MD, PhD and Brett Carver, MD | 1) Cancer of the penis- Paul Russo, MD |
| 5) Pelvic lymph node dissection- Bertrand Guillonneau, MD | 2) Erectile dysfunction after pelvic surgery- John P. Mulhall, MD |
| 6) Molecular biology- William Gerald, MD, PhD | 3) Genitourinary sarcoma- Paul Russo, MD |
| 7) Open radical prostatectomy- James Eastham, MD | 4) Risk management- Glenn Dopf, JD, LLM |
| 8) Brachytherapy- Michael J. Zelefsky, MD | 5) Adrenal cancerr- Pramod Sogani, MD |
| 9) External beam radiotherapy- Michael J. Zelefsky, MD | |
| 10) Pathophysiology of sexual dysfunction following radical pelvic surgery- John P. Mulhall, MD | |
| 11) Hormonal therapy and bone health- Michael J. Morris, MD | |
| 12) Chemotherapy and new experimental approaches- Howard Scher, MD |
In addition, the urologic oncology fellows participate in the NIH-sponsored Clinical Research Curriculum. This extensive course provides trainees with comprehensive, high quality, multidisciplinary didactic training in the design, conduct, ethics, and regulatory issues governing research on human subjects to prepare trainees for successful clinical research careers. The course is comprised of four modules taught by faculty from the Departments of Medicine, Psychiatry, Human Genetics, Pediatrics, Radiation, Epidemiology and Biostatistics, Anesthesiology, Neurology, and Surgery.
CONCLUSION
In this article, we present the critical elements of fellowship training for the urologic oncologist. As an example, the Memorial Sloan-Kettering Cancer Center experience is outlined in detail including the clinical experience, research curriculum, laparoscopic and minimally invasive exposure, and didactic lecture series.
References
- 1. [Accessed September 28, 2007];Society of Urologic Oncology: SUO Fellowship Programs. Available at: http://www.societyofurologiconcology.org.
- 2.Sheinfeld J, Eastham JA, Scardino PT, editors. Urology service department of surgery fellowship and educational programs. New York, NY: Memorial Sloan-Kettering Cancer Center; 2007. [Google Scholar]
- 3.Sheinfeld J. Urologic oncology- What are the challenges facing recruiting GU cancer fellowships and how might these changes affect the training of GU cancer specialists. Lecture at the Society of University Urologists Annual Meeting; 2007. [Google Scholar]


