Abstract
Background
It is considered that patients at risk for spontaneous fracture due to metastatic lesions should undergo surgical stabilization before fracture occurs; however, prophylactic stabilization is associated with surgical morbidity and mortality. We sought to compare pathological fracture fixation versus prophylactic stabilization of diaphyseal femoral lesions for patients with femoral metastases and assess the rate of prophylactic surgery completed in all regions of Ontario.
Methods
Using population data sets, we identified all patients who had undergone femoral stabilization, either for pathological femoral fractures or for prophylactic fixation of femoral metastases before pathological fractures, between 1992 and 1997 in Ontario. We compared the rates of survival, serious medical and surgical complications and length of stay in hospital between the 2 groups.
Results
A total of 624 patients underwent surgical stabilization for femoral metastases. The most common sites of primary metastases were the lungs (26%), breasts (16%), kidneys (6%) and prostate (6%); 46% of patients had other or multiple primary metastases. Overall, 37% of lesions were fixed prophylactically, with wide variation by region (17.6%–72.2%). Patients who underwent prophylactic stabilization had better overall survival at all postoperative time points. This held true after adjusting for age, sex, comorbidities and type of cancer (p < 0.001).
Conclusion
These data demonstrate a survival advantage with prophylactic fixation of metastatic femoral lesions combined with a relatively low perioperative risk excluding concomitant bilateral procedures. Ontario regional rates of prophylactic fixation vary enormously, with most patients not receiving prophylactic treatment.
Abstract
Contexte
On considère que les patients à risque de fracture spontanée causée par des lésions métastatiques devraient subir une stabilisation chirurgicale avant qu’il y ait fracture; il existe toutefois un lien entre la stabilisation prophylactique et la morbidité et la mortalité chirurgicales. Nous avons cherché à comparer la réduction de la fracture pathologique à la stabilisation prophylactique de lésions de la diaphyse du fémur chez les patients atteints de métastases au fémur et à évaluer le taux d’interventions chirurgicales prophylactiques pratiquées dans toutes les régions de l’Ontario.
Méthodes
À partir d’ensembles de données démographiques, nous avons identifié tous les patients qui avaient subi une stabilisation du fémur, soit en raison de fractures pathologiques, soit pour la réduction prophylactique de métastases au fémur avant la survenue d’une fracture pathologique, entre 1992 et 1997, en Ontario. Nous avons comparé les taux de survie, les complications médicales et chirurgicales graves et la durée du séjour à l’hôpital entre les 2 groupes.
Résultats
Au total, 624 patients ont subi une stabilisation chirurgicale pour métastases au fémur. Les sites les plus courants de métastases primitives étaient les poumons (26 %), les seins (16 %), les reins (6 %) et la prostate (6 %); 46 % des patients avaient d’autres métastases ou des métastases primitives multiples. Dans l’ensemble, 37 % des lésions ont été réduites de façon prophylactique et la variation a été importante selon la région (17,6 %–72,2 %). Les patients qui ont subi une stabilisation prophylactique présentaient un meilleur taux de survie générale à tous les points dans le temps après l’intervention. Le résultat est demeuré valable même après correction en fonction de l’âge, du sexe, de comorbidités et du type de cancer (p < 0,001).
Conclusion
Ces données démontrent que la réduction prophylactique de lésions fémorales métastatiques présente un avantage pour la survie et un risque périopératoire relativement faible, sauf dans le cas des interventions bilatérales concomitantes. Les taux régionaux de réduction prophylactique varient énormément en Ontario : la plupart des patients ne reçoivent pas de traitement prophylactique.
Cancer will develop in 40% of the population during their lifetime, and skeletal metastases will develop in 80% of people with cancer. The femur represents one of the most frequently involved sites.1
It is generally considered good practice that patients at risk for spontaneous fracture due to metastatic lesions undergo surgical stabilization before fracture occurs.2 However, controversy exists as prophylactic surgery requires identification and effective surveillance of metastatic lesions. Proper surveillance is problematic as currently no single criterion exists that is both highly specific and sensitive to identify patients who will fracture. Prophylactic stabilization is associated with surgical morbidity and mortality including potential complications caused by raised intramedullary pressure and fat embolization.3 Intramedullary pressures are probably higher with prophylactic nailing versus nailing of a fractured femur, as the intact cortex does not allow escape of intramedullary contents. Venting has been suggested as a technique to reduce intramedullary pressure during prophylactic nailing,4,5 although it is inconsistently used clinically.6
There is little information comparing prophylactic stabilization of a femoral lesion versus fixation of a completed fracture. Similar surgical complications and patient function for both groups were reported in a review of 22 patients, although survival at 3 years was better with prophylactic stabilization.7 Another review of 182 patients noted less surgical morbidity, better patient function and lower 1- and 2-year mortality rates following prophylactic stabilization.2 No large population cohort studies on this topic have been reported. Furthermore, the relative frequency of prophylactic fixation versus treatment of a completed fracture in the population is unknown. For a pathological lesion to be treated prophylactically, appropriate surveillance by health care providers is necessary. Evidence of inadequate or inconsistent surveillance within a region would represent an important opportunity to improve the outcome of individuals living with bone metastases, if prophylactic fixation is indicated.
Methods
Using the Canadian Institute for Health Information (CIHI) and Ontario Health Insurance Plan (OHIP) population data sets, we identified all patients who had undergone fracture fixation and prophylactic stabilization for diaphyseal femoral metastatic lesions from April 1992 to March 1998 in Ontario. The OHIP database contains a unique identifier and demographic information for each patient as well as codes for each procedure billed, and CIHI collects information regarding inpatient and day surgery discharges including the International Classification of Diseases, ninth revision (ICD-9) diagnostic codes and the Canadian Classification of Procedures codes. We used CIHI codes to identify the patients who had undergone prophylactic stabilization of the femoral shaft versus those who were treated for pathologic fracture. We also used this data set to document serious medical and surgical complications such as stroke, myocardial infarction, infection and deep vein thrombosis (DVT) as well as length of stay in hospital. We linked records from the OHIP database to the CIHI database using patient health numbers and demographic information. We assessed comorbidity using the modified Charlson–Deyo classification.8 We excluded cancer as this applied to all patients; we were interested in determining additional comorbidities. We used the Ontario mortality file to capture information on patient survival.
Statistical analysis
We used standard descriptive statistics to assess the study population, complication rates and survival. We fitted a multivariate Cox proportional hazards model to determine the significance of demographic factors, tumour type and indication for fixation (prophylactic or fracture) as determinants of survival. Cox regression is appropriate for time-dependant continuous outcomes that cannot be modelled using simple linear regression.9
We compared practice patterns among 16 district health councils (DHCs) across the province of Ontario. For this analysis, we assigned each resident of Ontario to a DHC based on their home addresses, as determined by the first 3 digits of their postal codes. Rather than computing overall population rates for both types of these relatively rare surgeries, we evaluated the ratio of prophylactic stabilization to fracture fixation in each region. We quantified overall regional variation using the extremal quotient (the ratio of the highest rate relative to the lowest rate of prophylactic fixation). We used z scores to test for significant deviation of individual DHC proportions of prophylactic fixation from the mean provincial rate.
Results
Demographics
A total of 624 patients underwent surgical treatment for diaphyseal femoral metastatic lesions during the study period. We excluded 66 patients because they underwent femoral reconstruction by prosthetic means other than fracture fixation (i.e., long-stem total hip replacement), leaving 558 patients for review. Seven patients underwent a combination of fracture fixation and contralateral prophylactic fixation during a single admission. We excluded these patients from analyses comparing fracture stabilization and prophylactic fixation. Eight patients were treated for bilateral pathologic fractures, and 3 received bilateral prophylactic stabilization surgery during a single admission.
In 46% of patients, the diagnosis of the tumour was coded as unknown or as a combination of multiple primary sites. Lung and breast metastases were the most common known tumour types (Table 1). Patients presenting with fractures stayed in hospital an average of 5 days longer than those undergoing prophylactic stabilization (Table 1, p = 0.006).
Table 1.
Unadjusted comparison of demographics, morbidity and mortality among patients treated with prophylactic stabilization versus fracture fixation*
| Characteristic | Fracture fixation | Prophylactic fixation | p value |
|---|---|---|---|
| No. patients† | 350 | 201 | |
| Primary cancer type, % | 0.10 | ||
| Lung | 23.1 | 31.3 | |
| Breast | 17.1 | 13.4 | |
| Kidney | 5.1 | 7.5 | |
| Prostate | 7.4 | 4.5 | |
| Other (multiple) | 47.1 | 43.3 | |
| Age, mean (range) yr | 66.8 (14.8–91.9) | 64.8 (15.0–91.8) | 0.06 |
| Comorbidity, % > 1 | 22.0 | 15.9 | 0.08 |
| Female sex, % | 64.3 | 59.2 | 0.24 |
| Length of stay in hospital, d | 24.3 (1 – 155) | 19.3 (1–105) | 0.006 |
| Surgical/medical complication, % | 10.9 | 8.0 | 0.27 |
| Infection, % | 0.6‡ | 0.0 | 0.28 |
| DVT within 3 mo, % | 6.0 | 3.0 | 0.12 |
| Urinary tract infection, % | 4.6 | 4.5 | 0.96 |
| Died, % | |||
| During surgery | 0.6‡ | 1.0‡ | 0.57 |
| Admission | 20.0 | 9.0 | 0.001 |
| 3 months | 28.3 | 13.9 | 0.000 |
DVT = deep vein thrombosis.
We made statistical comparisons between the 2 groups using the Student t test for continuous variables or the χ2 test for categorical variables (with continuity correction). We used the Fisher exact test when 1 or more cells had fewer than 5 expected counts.
Seven patients who underwent both fracture fixation and prophylactic stabilization of the opposite femur are not included in this table (see Table 2).
Two cases.
Morbidity and mortality
Death during surgery was a rare event, except in patients undergoing bilateral procedures. Overall, 5 patients out of 558 (0.7%) died during surgery, with most deaths occurring in patients undergoing bilateral procedures (Table 2). In total, 3 of 18 patients who underwent simultaneous bilateral procedures died intraoperatively (16.7%). This included 2 of 8 patients (25%) who presented with bilateral femur fractures and 1 of 7 patients (14.3%) undergoing a combination of prophylactic stabilization and fracture fixation. Three patients who had bilateral prophylactic femoral fixation survived the operation. Information on the type of procedure, implants and anesthetic employed was not available in the population data sets.
Table 2.
Unadjusted comparison of demographics, morbidity and mortality following stabilization for bilateral femoral lesions*
| Characteristic | Unilateral, %† | Bilateral, no. (%)† | p value | ||
|---|---|---|---|---|---|
| Fracture | Prophylactic treatment | Combination treatment | |||
| No. patients | 540 | 8 | 3 | 7 | |
| Primary cancer type | 0.54 | ||||
| Lung | 26.5 | 1 (12.5) | 3 (42.9) | ||
| Breast | 15.6 | 3 (37.5) | 1 (14.3) | ||
| Kidney | 6.1 | ||||
| Prostate | 6.3 | 1 (33.3) | |||
| Other (multiple) | 45.6 | 4 (50.0) | 2 (66.7) | 3 (42.9) | |
| Age, mean, yr | 66.1 | 65.8 | 67.5 | 60.8 | 0.71 |
| Comorbidity, % > 1 | 19.6 | 1 (12.5) | 2 (66.7) | 2 (28.6) | 0.19 |
| Female sex | 62.2 | 6 (75.0) | 2 (66.7) | 5 (71.4) | 0.85 |
| Length of stay in hospital, mean, d | 22.3 | 31.4 | 39.7 | 15.6 | 0.22 |
| Complications | 9.8 | — | 1 (33.3) | 1 (14.3) | 0.41 |
| Infection, no. (%) | 2 (0.4) | — | — | — | 1.00 |
| DVT within 3 mo | 5 | — | — | — | 0.81 |
| UTI on admission | 4.6 | — | — | — | 0.83 |
| Died | |||||
| During surgery | 2 (0.4) | 2 (25.0) | — | 1 (14.3) | < 0.001 |
| Admission | 15.7 | 3 (37.5) | — | 2 (28.6) | 0.25 |
| 3 months | 22.8 | 4 (50.0) | — | 3 (42.9) | 0.13 |
DVT = deep vein thrombosis; UTI = urinary tract infection.
We made statistical comparisons between the 2 groups using the Student t test for continuous variables or the χ2 test for categorical variables (with continuity correction). We used the Fisher exact test when 1 or more cells had fewer than 5 expected counts.
Unless otherwise indicated.
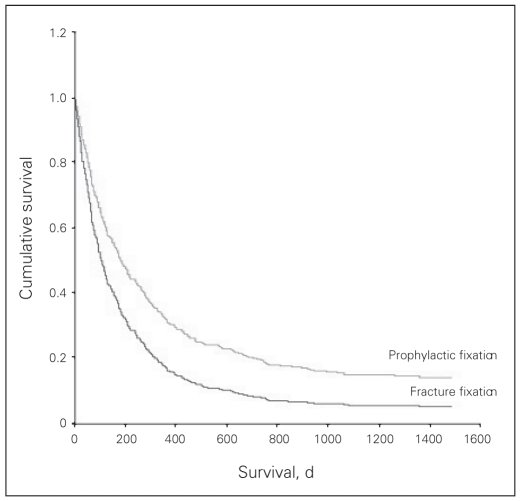
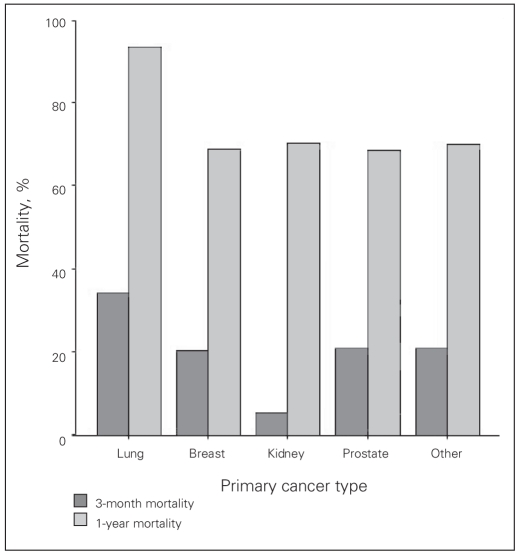
Mortality was higher at all postoperative intervals following fracture fixation versus prophylactic stabilization (Table 1). Even after adjusting for age, sex, comorbidity and type of cancer, patients treated for fracture were 1.5 times more likely to die during the follow-up period (odds ratio [OR] 1.48, 95% confidence interval (CI) 1.23–1.79) than those treated prophylactically (Fig. 1). Survival differed by type of cancer (Fig. 2); however, after adjusting for patient demographics, only lung cancer had a significantly worse survival rate than all other cancers (Table 3). One year after surgery, 76% of patients overall and 94% of those with primary lung metastases had died. Besides death, the postoperative complication rate was similar for fracture fixation versus prophylactic stabilization (Table 1).
Fig. 1.
Adjusted rate of survival following prophylactic stabilization versus fracture fixation for femoral metastases. We adjusted the survival comparison between prophylactic stabilization and fixation after fracture has occurred for patient age, sex, comorbidity and type of cancer. We computed the adjusted survival curves using Cox regression. The difference in survival is statistically significant (p < 0.001).
Fig. 2.
Unadjusted survival following treatment for femoral metastases. Raw 3-month and 1-year survival rates by tumour type are shown. Note that only lung cancer differs significantly from all other tumour types with respect to survival (p < 0.001).
Table 3.
Adjusted death rates among patients treated with prophylactic stabilization versus fracture fixation*
| Variable | p value | OR (95% CI) |
|---|---|---|
| Age per year | 0.10 | 1.006 (0.999–1.014) |
| Sex, female v. male | 0.049 | 1.242 (1.001–1.541) |
| Primary cancer type | ||
| Lung v. other | < 0.001 | 2.139 (1.702–2.687) |
| Breast v. other | 0.85 | 0.974 (0.743–1.277) |
| Kidney v. other | 0.84 | 0.959 (0.647–1.422) |
| Prostate v. other | 0.08 | 0.685 (0.447–1.050) |
| Type of surgery | ||
| Fracture fixation v. prophylactic | < 0.001 | 1.478 (1.225–1.785) |
CI = confidence interval; OR = odds ratio.
We computed the risk of death given the presence of each variable using Cox regression. We adjusted each variable for the presence of all others. Cox regression is appropriate for evaluating and adjusting for the effect of multiple factors (analogous to multiple regressions) when the outcome involves censored data such as survival.
The overall rate of DVT was 4.9% within 3 months of surgery. However, patients with metastases from the prostate had a rate of DVT of 11% (Table 4). After adjusting for age, sex and comorbidity, the calculated risk of DVT was 4 times higher for prostatic femoral metastases than other tumour types (OR 4.0, 95% CI 1.01–16.0).
Table 4.
Unadjusted rate of deep vein thrombosis by tumour type
| Tumour type | DVT rate, % |
|---|---|
| Lung | 4.2 |
| Breast | 2.3 |
| Kidney | 3.0 |
| Prostate | 11.4* |
| Other (multiple) | 5.6 |
| Overall mean rate | 4.9 |
DVT = deep vein thrombosis.
Significantly different from the overall mean DVT rate (p = 0.043).
Regional variation
The opportunity for prophylactic stabilization was missed in more than 60% of patients who consequently required treatment for fracture. There was wide variation among regions in the percentage of missed prophylactic fixation (28%–82%; extremal quotient = 4.1). Five regions differed significantly from the overall provincial mean proportion of patients who were prophylactically stabilized (Table 5).
Table 5.
Regional variation in prophylactic fixation in the different district health councils in Ontario
| DHC | Proportion of prophylactic fixation, % |
|---|---|
| Algoma | 36.0 |
| Champlain | 35.0 |
| Durham | 31.3 |
| Essex | 44.7 |
| Grand-River | 17.6* |
| Grey Bruce | 72.2† |
| Halton-Peel | 40.0 |
| Hamilton | 31.4 |
| Toronto | 29.8 |
| Muskoka | 28.6 |
| Niagara | 30.0 |
| Northwestern | 57.1* |
| Kingston, Quinte | 54.2* |
| Simcoe-York | 34.0 |
| Thames | 54.8* |
| Waterloo | 37.9 |
| Overall mean | 39.67 |
| SD | 13.76 |
DHC = district health council; SD = standard deviation.
More than 1 standard deviation from the overall mean proportion receiving prophylactic stabilization across the entire province. Regions that differ significantly from the provincial mean are set in boldface.
More than 2 standard deviations from the overall mean proportion receiving prophylactic stabilization across the entire province.
Discussion
Our study demonstrates improved survival with prophylactic stabilization of femoral metastases versus pathological fracture fixation, even after adjusting for patient factors and tumour type. Most patients in Ontario with femoral metastases fail to undergo prophylactic stabilization, with wide variation across the province.
A clinical review of 182 patients found that prophylactic stabilization of femoral metastases versus fracture fixation was associated with less blood loss, shorter stay in hospital and better patient function.2 Survival at 1 and 2 years was about 10% better in patients who underwent prophylactic fixation than those with complete fractures.2 Ampil and Sadasivan7 also noted improved survival at 3 years for patients who received prophylactic fixation versus those with complete fractures, although they did not demonstrate any significant difference in surgical complications or patient function. The reason for the improved survival with prophylactic fixation versus treatment after fracture is unknown. It is possible that patients who underwent prophylactic fixation had less extensive local and systemic disease and would thus be expected to survive longer, independent of the prophylactic treatment. It is also possible that a fractured femur is independently associated with an increased risk of mortality and that prophylactic treatment is directly responsible for the improved survival. We would consider that the physiologic insult of both a fracture and subsequent repair would be greater than that of prophylactic fixation alone. This hypothesis is supported by survival curves, which show an early drop in survival following fracture that gradually begins to parallel the group receiving prophylactic stabilization.2 This finding may be related to the ability to effectively mobilize and rehabilitate patients who undergo prophylactic fixation versus the greater difficulty of mobilizing patients with fractures. This is compounded by the influence of immobility on a patient’s general medical condition. Patients with fractures, on average, required an additional 5 days in hospital. This is most likely related to slower mobilization, postoperative complications and, potentially, delayed surgery. The significantly increased mortality rate in patients with lung cancer is consistent with the aggressiveness of the cancer and available treatments for lung cancer versus other types of cancers during the study period.
Given the apparent benefits of prophylactic stabilization for femoral metastases,2,7,10–12 it would seem appropriate to follow patients with metastatic disease of the femur and to intervene early for impending pathological fracture. How this surveillance should be carried out, how frequently various imaging studies should be performed and what criteria should be used to mandate prophylactic surgery is less clear.2,13–16 Recent work using quantitative computed tomography has shown some promising results, which in the future may allow a more sensitive means of predicting which patients are at higher risk of fracturing.17–20 Those who do not favour prophylactic fixation hope to avoid potential complications of surgery until surgery is absolutely necessary. There is also a perceived improved cost–benefit ratio if one operates only on patients who go on to experience fractures. However, this doesn’t take into consideration a survival advantage and the potential shorter hospital stay with prophylactic fixation. More data are necessary to investigate potential additional benefits of prophylactic fixation. Quality of life data such as pain levels, functional ability and patient satisfaction could further help to determine the utility of prophylactic treatment. Prophylactic fixation must be analyzed from a risk–benefit perspective taking into consideration the probability of fracture, pain relief, mobility and general quality of life against the risks of surgery tempered by the patients’ comorbidities and life expectancy.
We found significantly decreased survival among patients requiring bilateral procedures. Despite the relatively large number of patients within the study, only 18 patients (3.2%) underwent bilateral procedures. This higher mortality rate can be associated with the larger surgical insult incurred from bilateral procedures. In addition, this subset of patients would likely have more extensive local and systemic involvement indicative of a more vulnerable medical state. Patients with bilateral fractures have little option but to have stabilization procedures. Unfortunately, these patients had the highest mortality rate in our study (25%). However, there were no early deaths in our limited sample of 3 patients who had bilateral prophylactic procedures. In patients with a pathologic fracture and a contralateral metastatic lesion, we observed a high intraoperative mortality rate (14%). In light of our data, consideration to defer prophylactic fixation of a contralateral lesion to a fracture may be reasonable given this potential decrease in survival. Femoral venting may also play some role in reducing mortality in these patients. However, given the small numbers of patients undergoing bilateral procedures in our study, an individualized approach to each patient is prudent.
Prophylactic stabilization of femoral metastases can be associated with intraoperative complications, including pulmonary embolism, which is thought to be due to raised intramedullary pressures during nailing.3,12,21–23 Whereas pressures increase during all femoral nailings, the increase is greater when the femoral cortex is intact (e.g., during prophylactic femoral nailing).4,5 Venting of the femoral canal has been shown to significantly lower intramedullary pressure during femoral nailing in vitro.5 In vivo, venting has also been shown to decrease intramedullary pressures although the pressure may still be high enough to produce emboli.4 We noted a 1% intraoperative death rate for prophylactic femoral nailing (2 deaths in 201 patients), which was similar to the death rate of 0.6% for fracture fixation (2 deaths in 350 patients). Information regarding the use of venting was not available in the population data set that we used; however, it appears that most surgeons in Ontario do not routinely use venting in practice.6
Proximal DVT has been reported in more than 14% of cancer patients using routine Doppler ultrasonography,24 which is considerably higher than our finding of an overall 4.9% rate of DVT. Lin and colleagues24 found no difference in DVT rate by tumour type, in contrast to the marked difference in DVT rate that we noted for prostate metastasis versus other types of cancer. The population data set used for this study does not contain any information regarding DVT surveillance or prophylaxis. Moreover, the only DVTs we identified were those that resulted in hospital inpatient treatment for DVT within 3 months of surgery. Given the lack of surveillance and the possibility that some patients were treated as outpatients, our numbers should be considered an underestimate. In addition, our study population is a subset of patients who received surgery for fracture or pending fracture. It is quite possible that patients who require surgery for fracture or prophylaxis represent a subset of patients with a different risk for DVT. Their general well-being, coagulation profiles and mobility at the time of surgery could conceivably differ based on the type of cancer. Patients with prostate metastases suffer from blastic metastases and often have quite extensive disease when fractures occur. Our data likely capture patients with this extensive disease, possibly explaining the high DVT rate found in our study. Nonetheless, the reason for differing DVT rates for prostate cancer in our study cannot be completely explained from the data collected.
The reasons for wide variation in the use of prophylactic fixation based on geographic location are difficult to ascertain. This finding may reflect regional beliefs regarding prophylactic surgery among both surgeons and other practitioners. Surveillance of metastatic lesions and referral patterns to orthopedic surgeons may differ on a regional basis. Also, local access to multidisciplinary cancer centres, specialists and operative resources could influence rates of prophylactic treatment. It is possible that the presence of integrated local cancer centres would improve recognition and surveillance of metastatic bony disease and generate consistent timely referrals to orthopedic surgeons to deal with impending fractures.
Administrative data sets such as the one used in our study are able to provide information regarding an entire population; however, the data sets lack important clinical information such as the exact type of implant, whether cement was added to the fixation construct or what type of anesthetic was given. The size of the lesion and functional status of the patients before and after surgery are also unknown.
Conclusion
We found that patients who underwent prophylactic stabilization for femoral metastases had a survival advantage over those who had fixation for pathological fracture. In addition, surgery, excluding concomitant bilateral procedures, was associated with relatively low perioperative risk. Nonetheless, we found that most patients with femoral metastatic lesions do not receive prophylactic treatment in Ontario and that there is wide variation in practice across the province. The reason for this discrepancy in service is unclear but deserves further investigation and correction. It is unknown how many of these patients saw an orthopedic surgeon before fracture.
Acknowledgements
Dr. Kreder received grant funding from the Institute for Clinical Evaluative Sciences.
Footnotes
Competing interests: None declared for Drs. Ristevski, Jenkinson, Finkelstein, Schemitsch, McKee and Kreder. Dr. Stephen has received speaker fees from Zimmer and Synthes.
Contributors: Drs. Stephen, Schemitsch, McKee and Kreder designed the study. Drs. Stephen, Finkelstein and Kreder acquired the data, which Drs. Ristevski, Jenkinson, Stephen and Kreder analyzed. Drs. Ristevski, Jenkinson, and Kreder wrote the article, which all authors reviewed and approved for publication.
References
- 1.Galasko CS. Skeletal metastases. Clin Orthop Relat Res. 1986;(210):18–30. [PubMed] [Google Scholar]
- 2.Ward WG, Holsenbeck S, Dorey FJ, et al. Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res. 2003:S230–44. doi: 10.1097/01.blo.0000093849.72468.82. [DOI] [PubMed] [Google Scholar]
- 3.Choong PF. Cardiopulmonary complications of intramedullary fixation of long bone metastases. Clin Orthop Relat Res. 2003;(415 Suppl):S245–53. doi: 10.1097/01.blo.0000093058.96273.1f. [DOI] [PubMed] [Google Scholar]
- 4.Martin R, Leighton RK, Petrie D, et al. Effect of proximal and distal venting during intramedullary nailing. Clin Orthop Relat Res. 1996;(332):80–9. doi: 10.1097/00003086-199611000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Roth SE, Rebello MM, Kreder H, et al. Pressurization of the metastatic femur during prophylactic intramedullary nail fixation. J Trauma. 2004;57:333–9. doi: 10.1097/01.ta.0000082157.29723.16. [DOI] [PubMed] [Google Scholar]
- 6.Dalgorf D, Borkhoff CM, Stephen DJ, et al. Venting during prophylactic nailing for femoral metastases: current orthopedic practice. Can J Surg. 2003;46:427–31. [PMC free article] [PubMed] [Google Scholar]
- 7.Ampil FL, Sadasivan KK. Prophylactic and therapeutic fixation of weight-bearing long bones with metastatic cancer. South Med J. 2001;94:394–6. [PubMed] [Google Scholar]
- 8.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein JA, Kreder H. Spine stats. The Cox regression analysis. Spine J. 2001;1:382. doi: 10.1016/s1529-9430(01)00140-1. [DOI] [PubMed] [Google Scholar]
- 10.Van Geffen E, Wobbes T, Veth RP, et al. Operative management of impending pathological fractures: a critical analysis of therapy. J Surg Oncol. 1997;64:190–4. doi: 10.1002/(sici)1096-9098(199703)64:3<190::aid-jso3>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 11.Edwards SA, Pandit HG, Clarke HJ. The treatment of impending and existing pathological femoral fractures using the long gamma nail. Injury. 2001;32:299–306. doi: 10.1016/s0020-1383(00)00218-7. [DOI] [PubMed] [Google Scholar]
- 12.van Doorn R, Stapert JW. Treatment of impending and actual pathological femoral fractures with the long Gamma nail in The Netherlands. Eur J Surg. 2000;166:247–54. doi: 10.1080/110241500750009366. [DOI] [PubMed] [Google Scholar]
- 13.Aaron AD. Treatment of metastatic adenocarcinoma of the pelvis and the extremities. J Bone Joint Surg Am. 1997;79:917–32. doi: 10.2106/00004623-199706000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;(249):256–64. [PubMed] [Google Scholar]
- 15.Kreder HJ. Factors affecting outcome after surgical treatment of acetabular and femoral metastatic lesions. Tech Orthop. 2004;19:38–44. [Google Scholar]
- 16.Van der Linden YM, Kroon HM, Dijkstra SP, et al. Simple radiographic parameter predicts fracturing in metastatic femoral bone lesions: results from a randomised trial. Radiother Oncol. 2003;69:21–3. doi: 10.1016/s0167-8140(03)00232-9. [DOI] [PubMed] [Google Scholar]
- 17.Lee T. Predicting failure load of the femur with simulated osteolytic defects using noninvasive imaging technique in a simplified load case. Ann Biomed Eng. 2007;35:642–50. doi: 10.1007/s10439-006-9237-y. [DOI] [PubMed] [Google Scholar]
- 18.Spruijt S, van der Linden JC, Dijkstra PD, et al. Prediciton of torsional failure in 22 cadaver femora with and without simulated subtrochanteric metastatic defects: a CT scan-based finite element analysis. Acta Orthop. 2006;77:474–81. doi: 10.1080/17453670610046424. [DOI] [PubMed] [Google Scholar]
- 19.Snyder BD, Hauser-Kara DA, Hipp JA, et al. Predicting fracture through benign skeletal lesions with quantitative computed tomography. J Bone Joint Surg Am. 2006;88:55–70. doi: 10.2106/JBJS.D.02600. [DOI] [PubMed] [Google Scholar]
- 20.Keyak JH, Kaneko TS, Skinner HB, et al. The effect of simulated metastatic lytic lesions on proximal femoral strength. Clin Orthop Relat Res. 2007;459:139–45. doi: 10.1097/BLO.0b013e3180514caa. [DOI] [PubMed] [Google Scholar]
- 21.Gibbons CE, Pope SJ, Murphy JP, et al. Femoral metastatic fractures treated with intramedullary nailing. Int Orthop. 2000;24:101–3. doi: 10.1007/s002640000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barwood SA, Wilson JL, Molnar RR, et al. The incidence of acute cardiorespiratory and vascular dysfunction following intramedullary nail fixation of femoral metastasis. Acta Orthop Scand. 2000;71:147–52. doi: 10.1080/000164700317413111. [DOI] [PubMed] [Google Scholar]
- 23.Wedin R. Surgical treatment for pathologic fracture. Acta Orthop Scand Suppl. 2001;72:2, 1–29. [PubMed] [Google Scholar]
- 24.Lin PP, Graham D, Hann LE, et al. Deep venous thrombosis after orthopedic surgery in adult cancer patients. J Surg Oncol. 1998;68:41–7. doi: 10.1002/(sici)1096-9098(199805)68:1<41::aid-jso9>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]